67 y.o. male prior tobacco use (20pyhx, quit 20 years ago) with PMHx of asthma/COPD (3 years prior FEV1 1.6 55% moderately severe obstructive lung disease by PFTs PFTs severe airflow limitaton w/ hyperinflation.)
# Asthma/COPD
# possible ABPA
# elev aspergillus IgE
# exertional hypoxemia
Interval events:
– abs eos 500, IgE 572 and elev IgE to Aspergillus with neg Aspergillus IgG at last visit
Echocardiogarm
sinus tachycardia with HR 101 bpm. LV cavity and wall thickness appears normal. Normal systolic function with estimated LVEF 65%. No obvious regional LV wall motion abnormalities. Diastolic function is indeterminate. RV appears dilated with thickened walls (RV wall thickness 11 mm). There is normal RV systolic function (TAPSE 2.5 cm). Atria are not well visualized. Aortic valve appears trileaflet with no AS or AR. Within the limitations of the study, there are no other significant valvular abnormalities.
Insufficient TR Doppler profile to accurately estimate PA systolic pressure. Normal IVC size and respirophasic variation, suggestive of normal RA pressure. No prior study for comparison
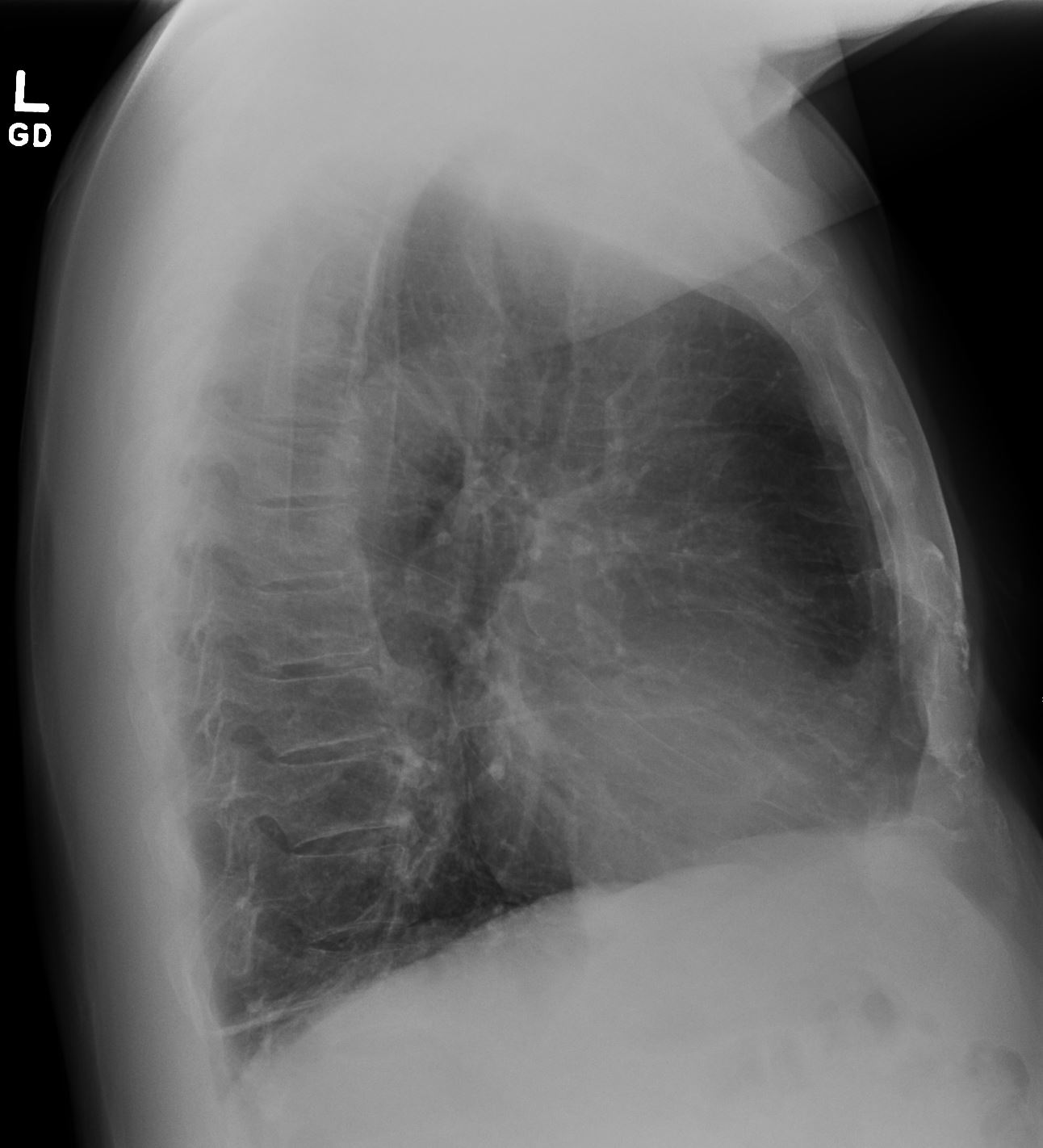
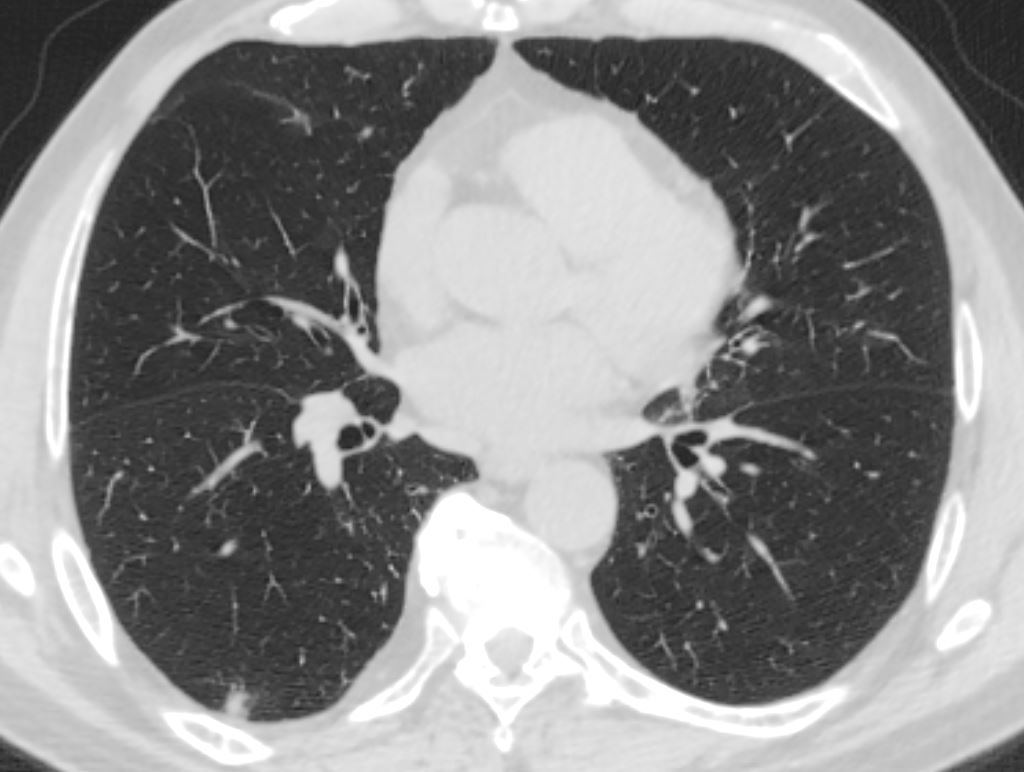
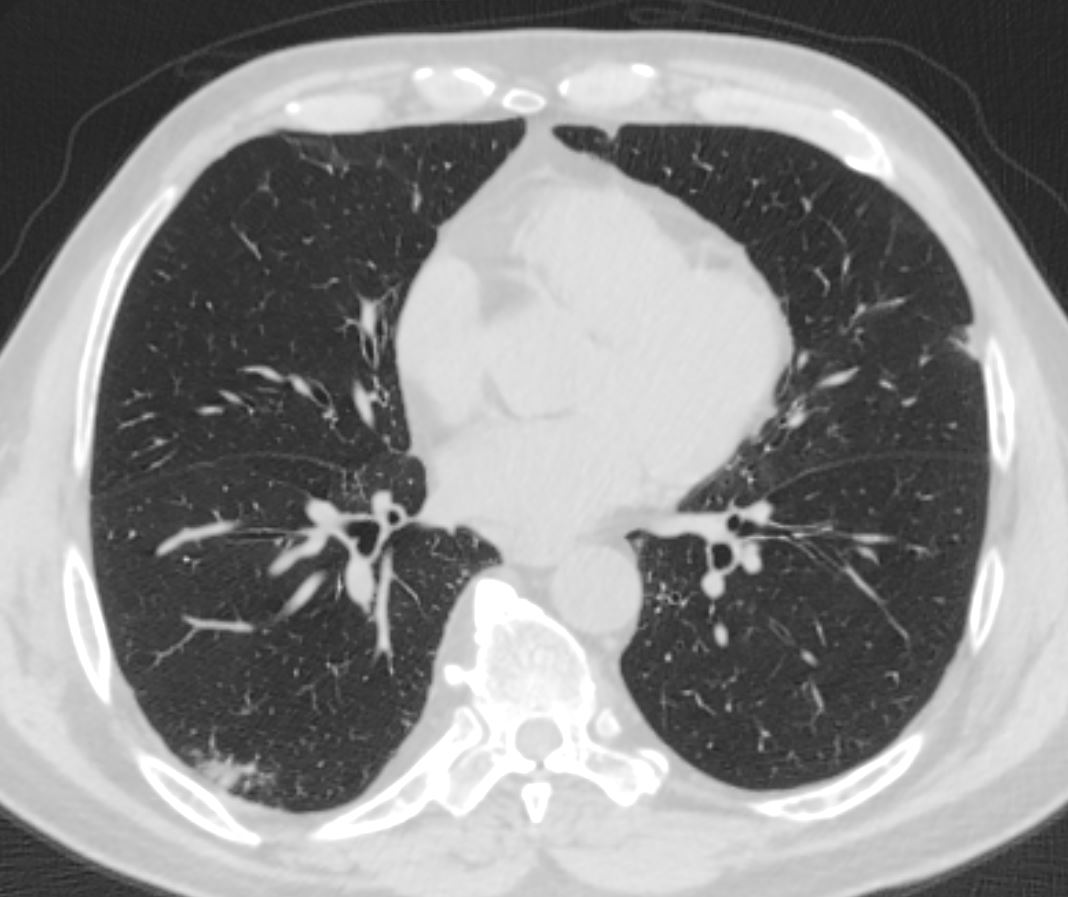
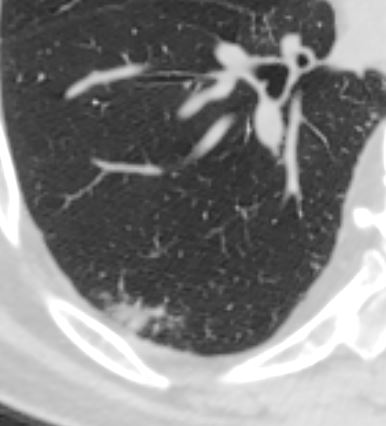
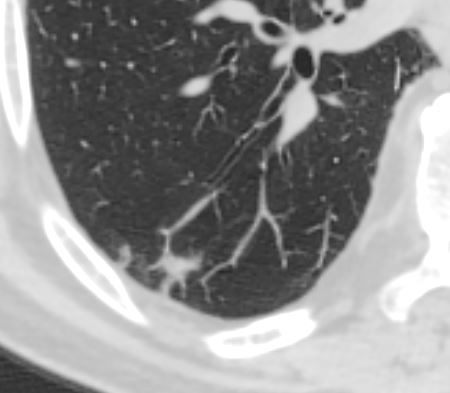
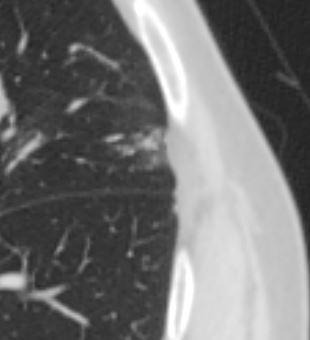
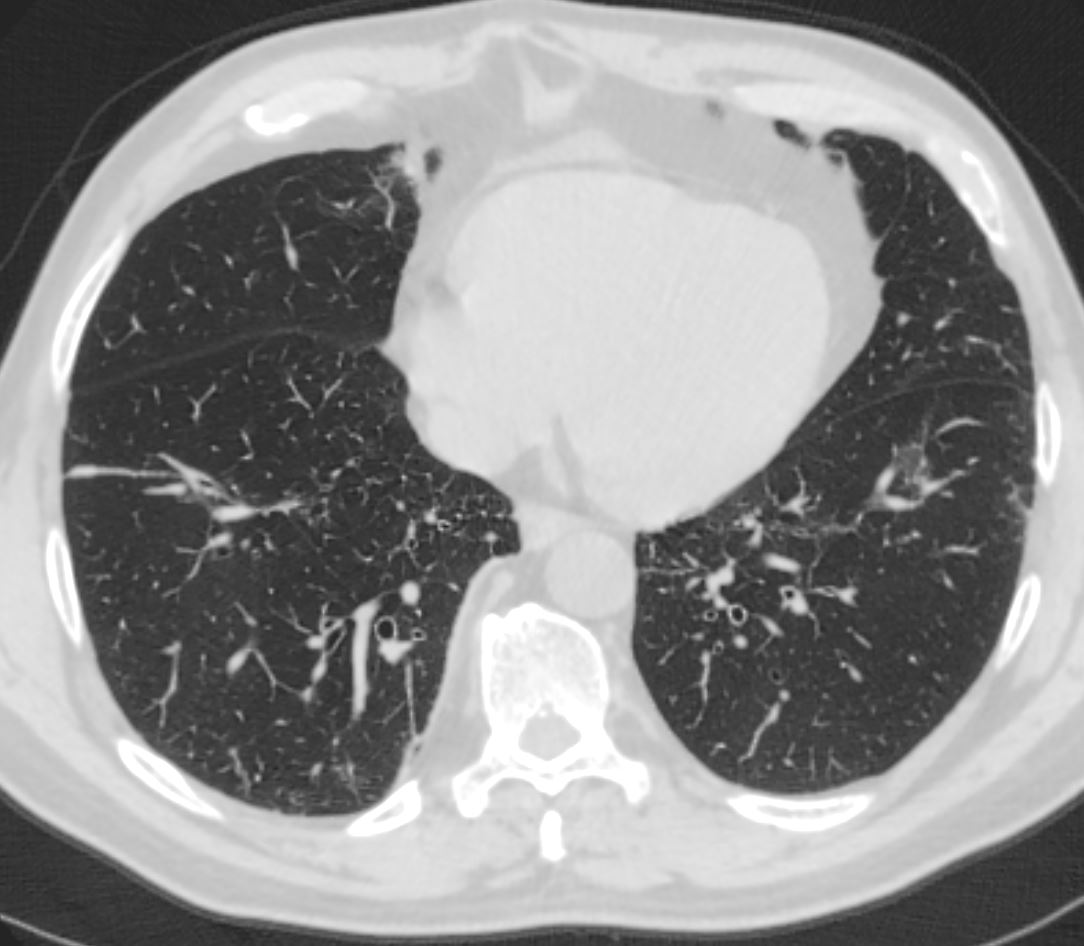
CT scan
Several confluent and ill-defined peripheral parenchymal opacities in both lungs. Given history of peripheral esinophilia/asthma, these findings aresuggestive of eosinophilic lung disease like chronic eosinophilic pneumonia
The peripheral infiltrates are small and usually more prominent in eosinophillic pneumonia The other possibility in this patient is is that the eosinophilia is caused by the asthma.