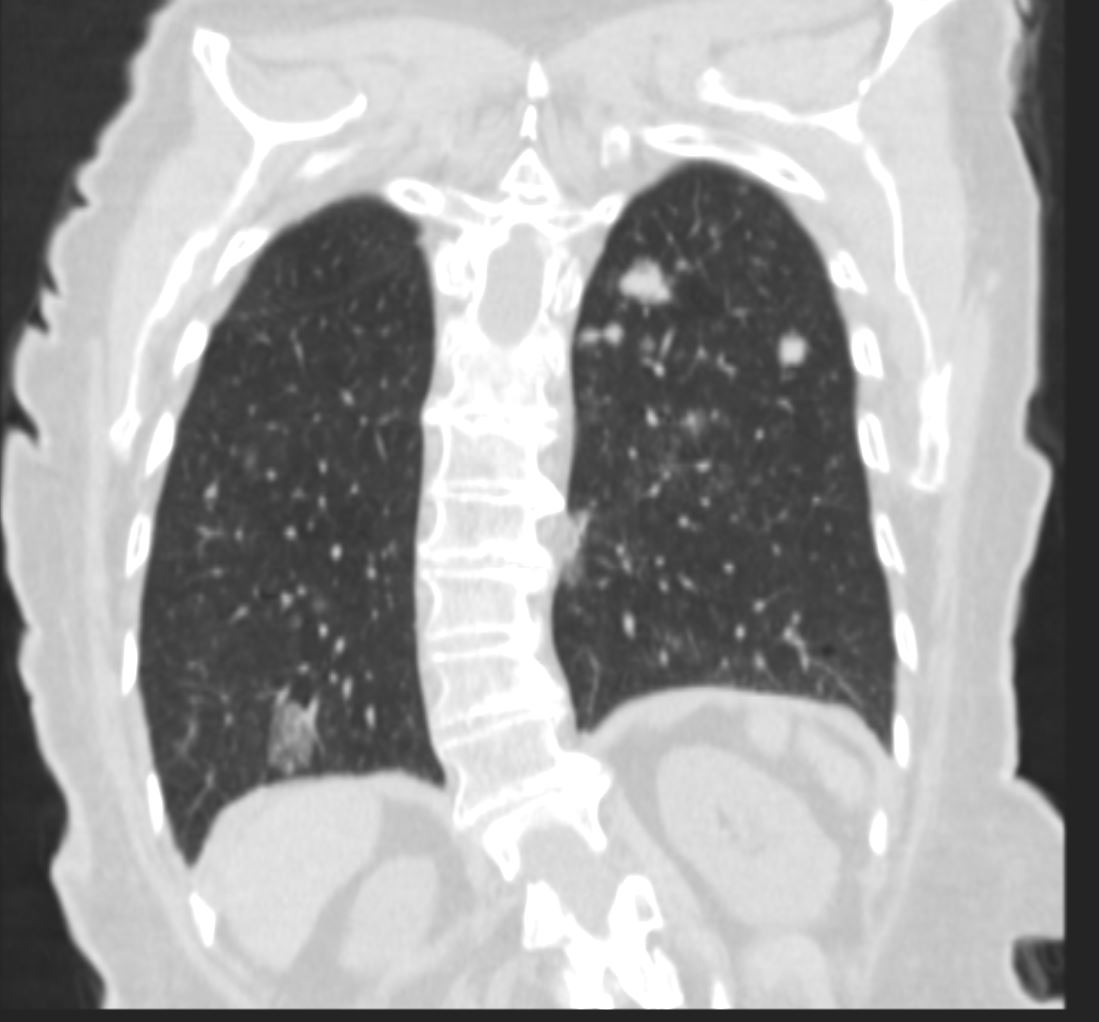
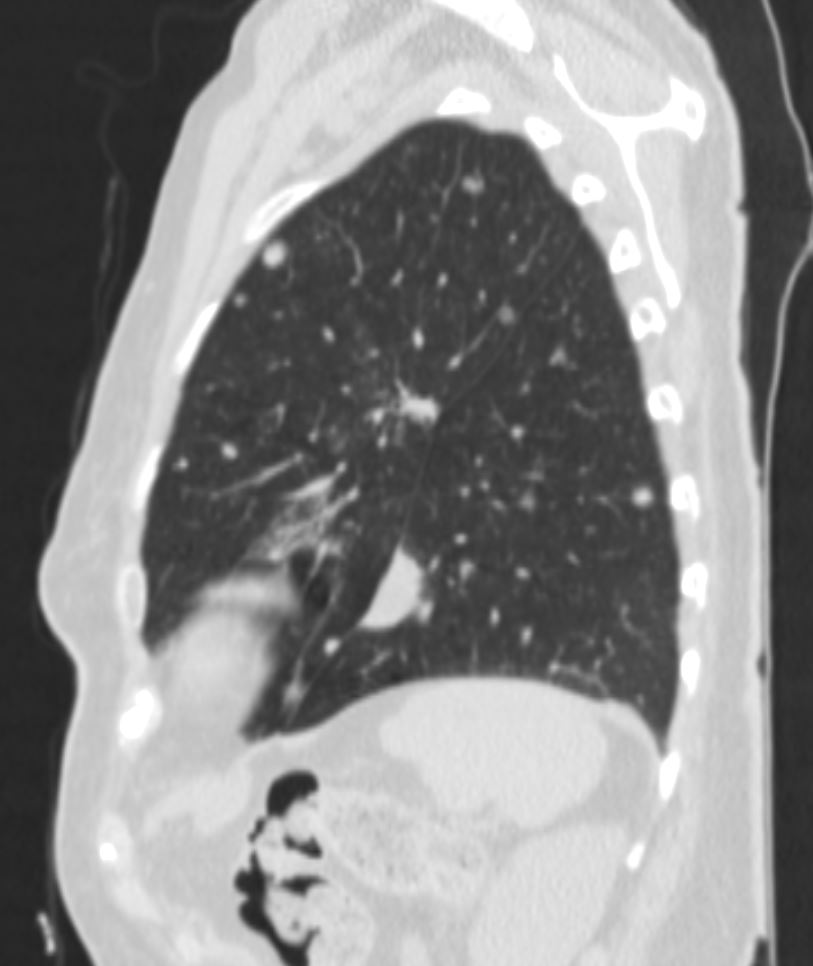
87-year-old woman with a history of localized pulmonary amyloidosis and kappa MGUS last
Echocardiogram:
Poor GLS contours
Rhythm is AF
Mildly increased wall thickness, hyperdynamic LVEF. Aortic sclerosis without stenosis, mitral annular calcification.
IVC top normal with blunted variation
Mildly Elevated pulmonary artery systolic pressures
Complete spectral Doppler velocity analysis and color Doppler were
performed.
Measurements Normal
Ao (mm): 28 (20-35)
LA (mm): 43
IVSd (mm): 11 (7-11)
LVIDd (mm): 34 < 57
LVPWd (mm): 11 (6-11)
Aortic Ascending (mm): 24
LV Mass (gm): 114.011584
LV Mass Index (gm/m2): 76.52 M: < 131
F: < 100
LV Mass Index (gm/m): 73.56 M: < 143
F: < 102
AV MV TV PV
Regurgitation: None 1+ 1+ None
Est. RA Pressure (mmHg):
Est. RV Systolic Pressure (mmHg):
Stenosis None None None
None
Wall Motion
Level Inferior Septum Anterior Septum Anterior
Base: Normal Normal Normal
Mid: Normal Normal Normal
Septum
Apex: Normal Normal
Level Anterior Lateral Inferior Lateral Inferior
Base: Normal Normal Normal
Mid: Normal Normal Normal
Lateral
Apex: Normal Normal
Left Ventricle
Size: Small
Function: Normal
Overall Function: Normal
Diastolic Function: Indeterminate
Wall Thickness: Mild
Ejection Fraction: 70 %
Right Ventricle
Size: Normal
Function: Normal
Left Atrium
Size: Markedly Enlarged
Function: Normal
Right Atrium
Size: Normal
Function: Normal
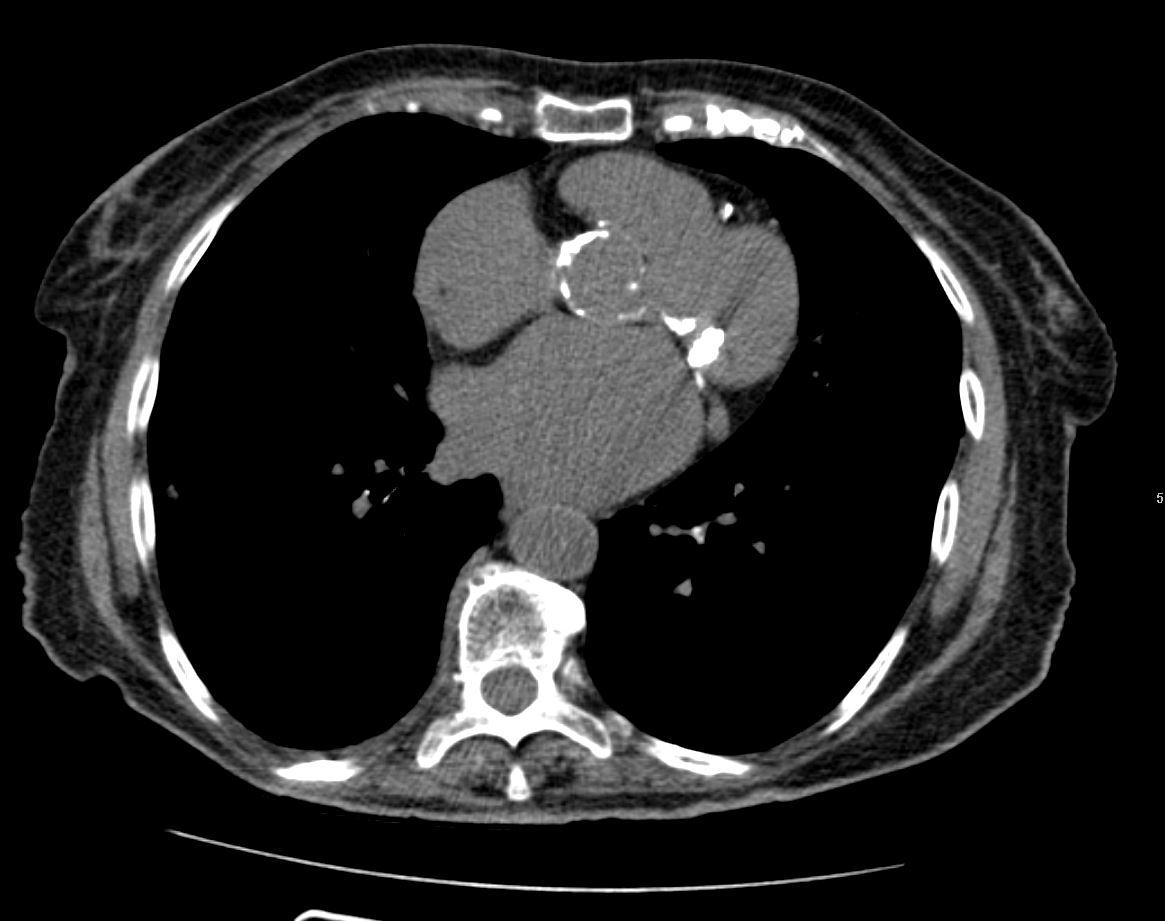
Aortic Valve
Leaflet Calcification: Moderate
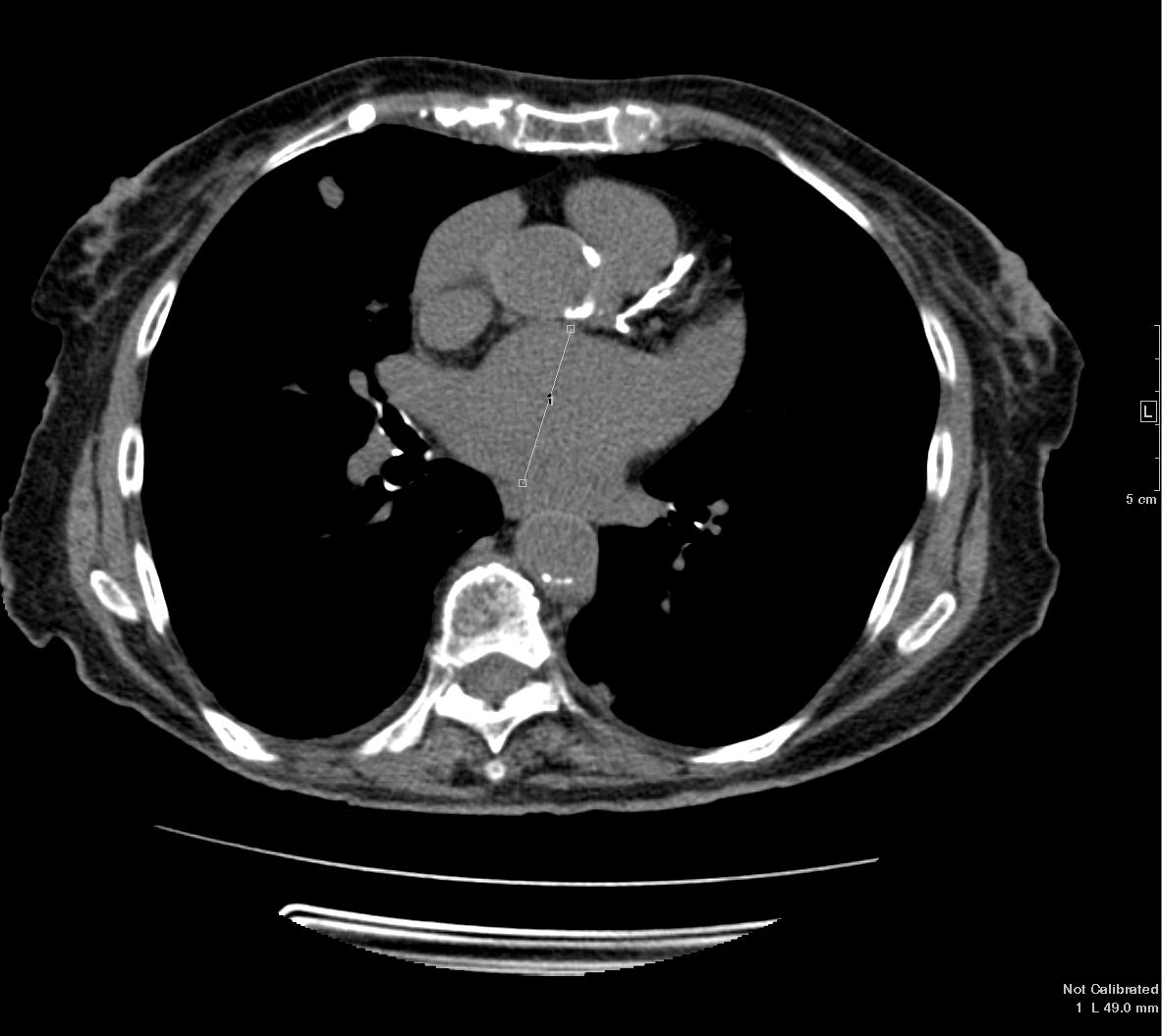
Mitral Valve
Structure: Normal
Annular Calcification: Severe
Leaflet Calcification: Mild
Calcification of Annulus and Aortic Root: yes
Tricuspid Valve
Structure: Normal
Function: Normal
Pulmonic Valve
Function: Normal
Structure: Normal
Pulmonary Artery –Normal
Pericardium
Normal: yes
Conclusions:
Rhythm is atrial fibrillation. Technically difficult study. Small LV cavity
size with mildly increased LV wall thickness, and normal global LV systolic
function. Estimated LVEF is 70%. No obvious regional LV wall motion
abnormalities. Global longitudinal strain is reduced at -12%. Normal RV size
and global RV systolic function. Severely dilated LA (LA volume indexed to
BSA is 78 mL/m^2). Normal RA size. Indeterminate diastolic function. Aortic
annular calcification is visualized. Trileaflet aortic valve with moderate
calcification with no significant AS or AR. Severe posterior mitral annular
calcification with calcified mitral leaflets. Mean gradient is 2 mm Hg at a
heart rate of 57 bpm. Mild MR. Mild to moderate TR. Normal IVC size with
blunted respirophasic variation suggestive of RA pressure of 8 mmHg.
Estimated PA systolic pressure is 40 mm Hg. No pericardial effusion.
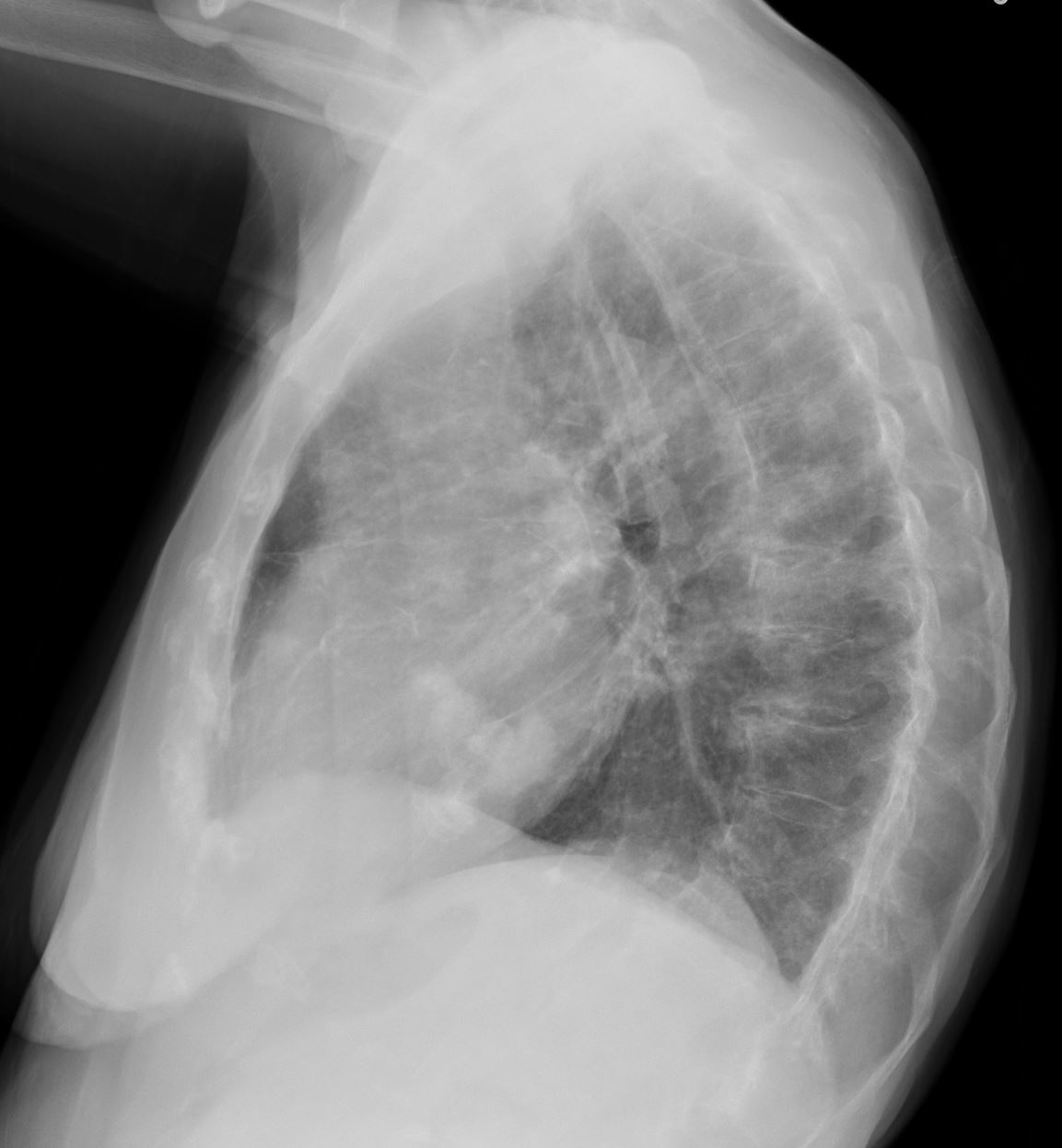
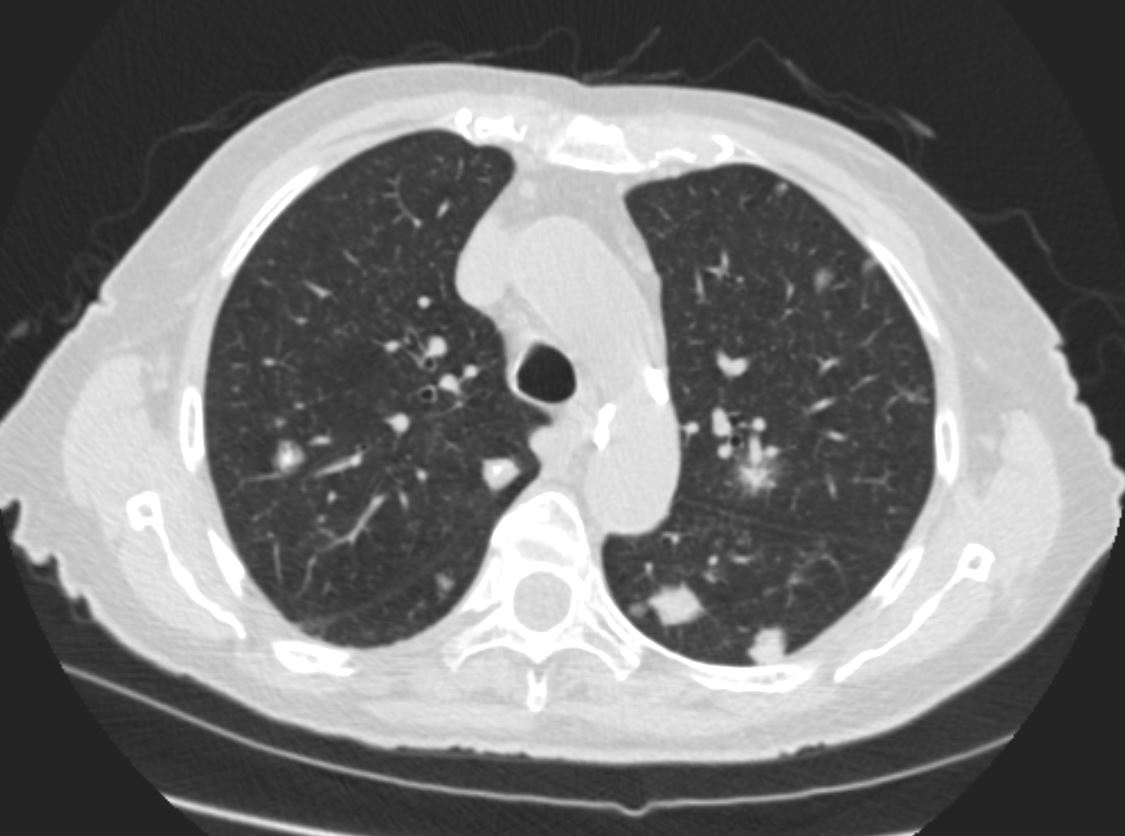
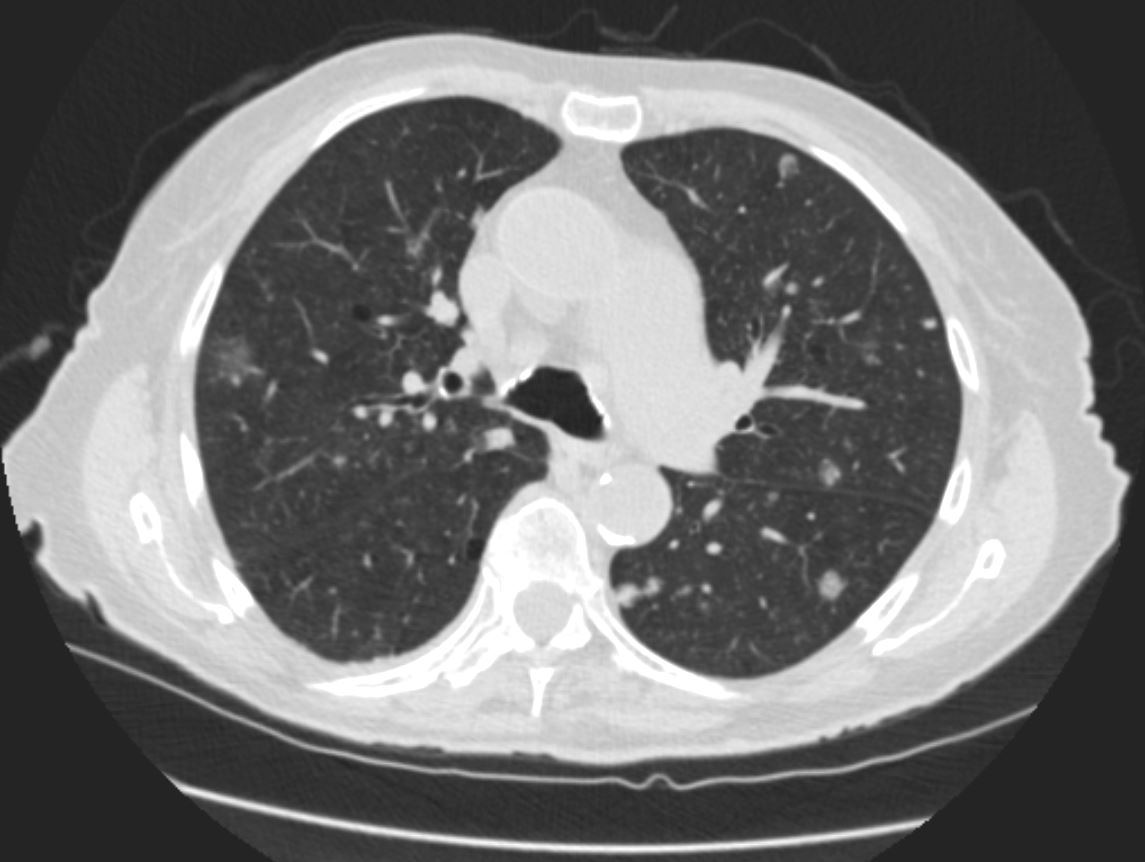
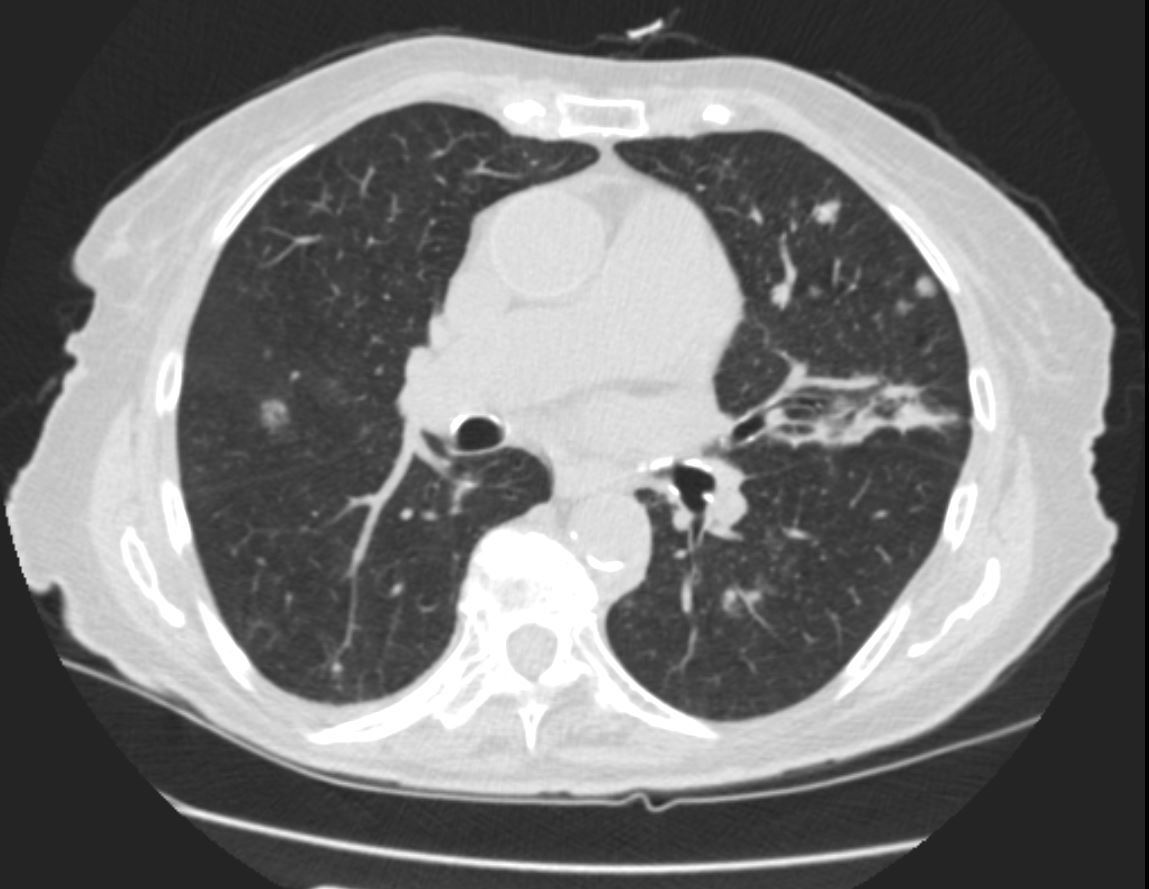
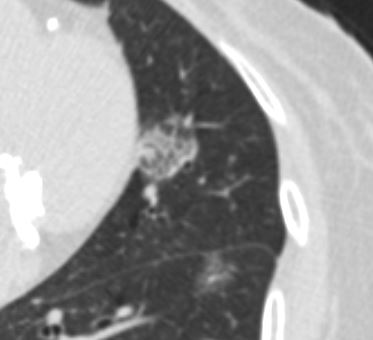
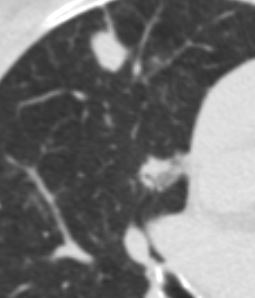
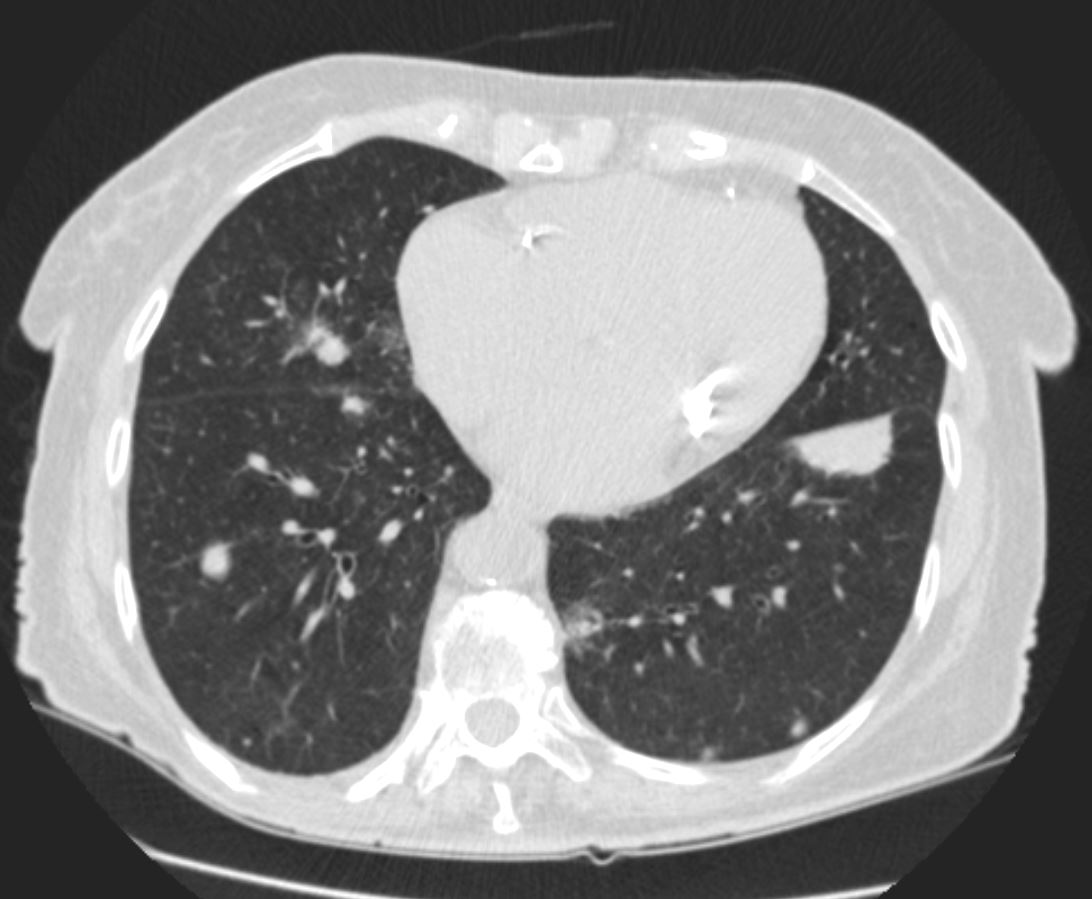
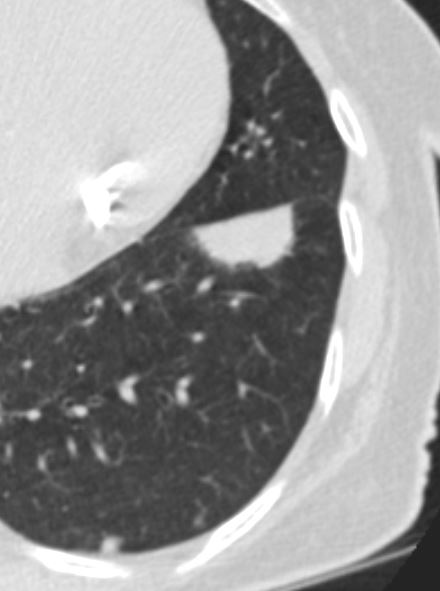
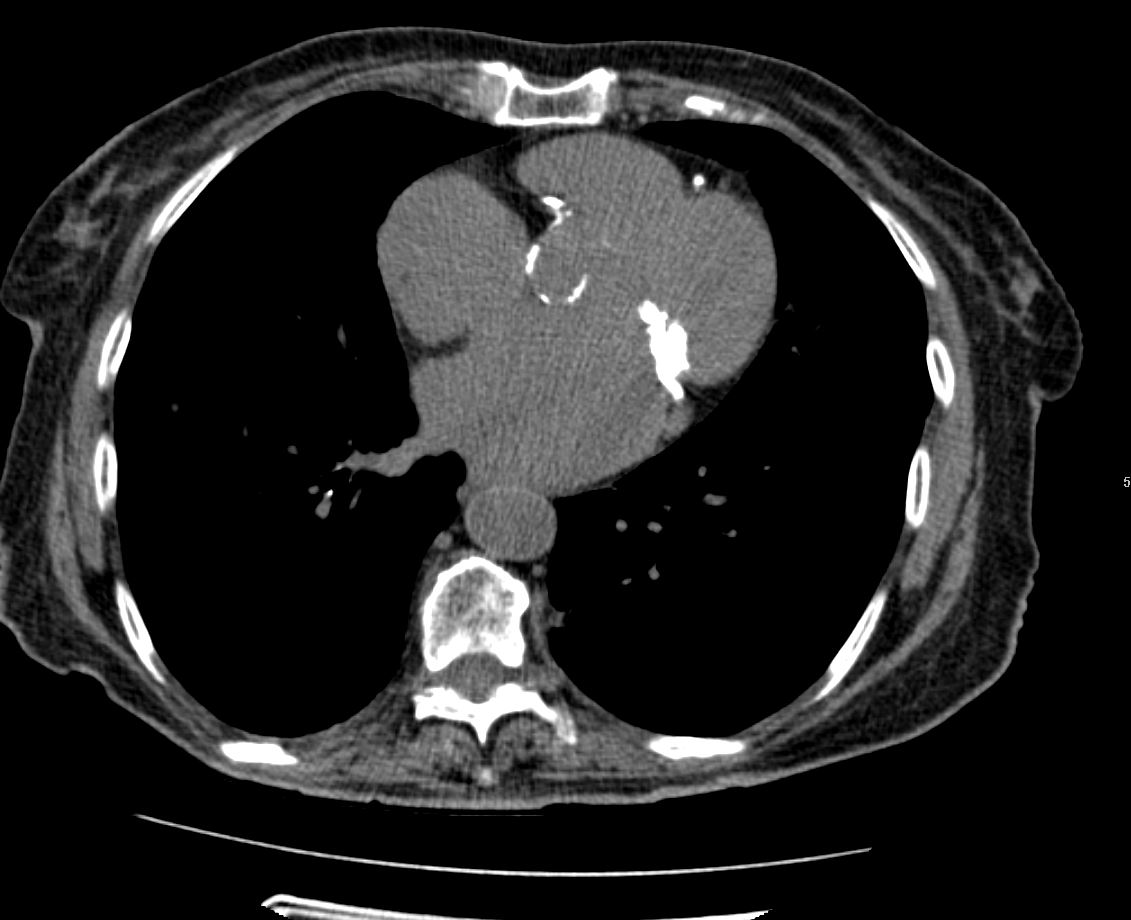
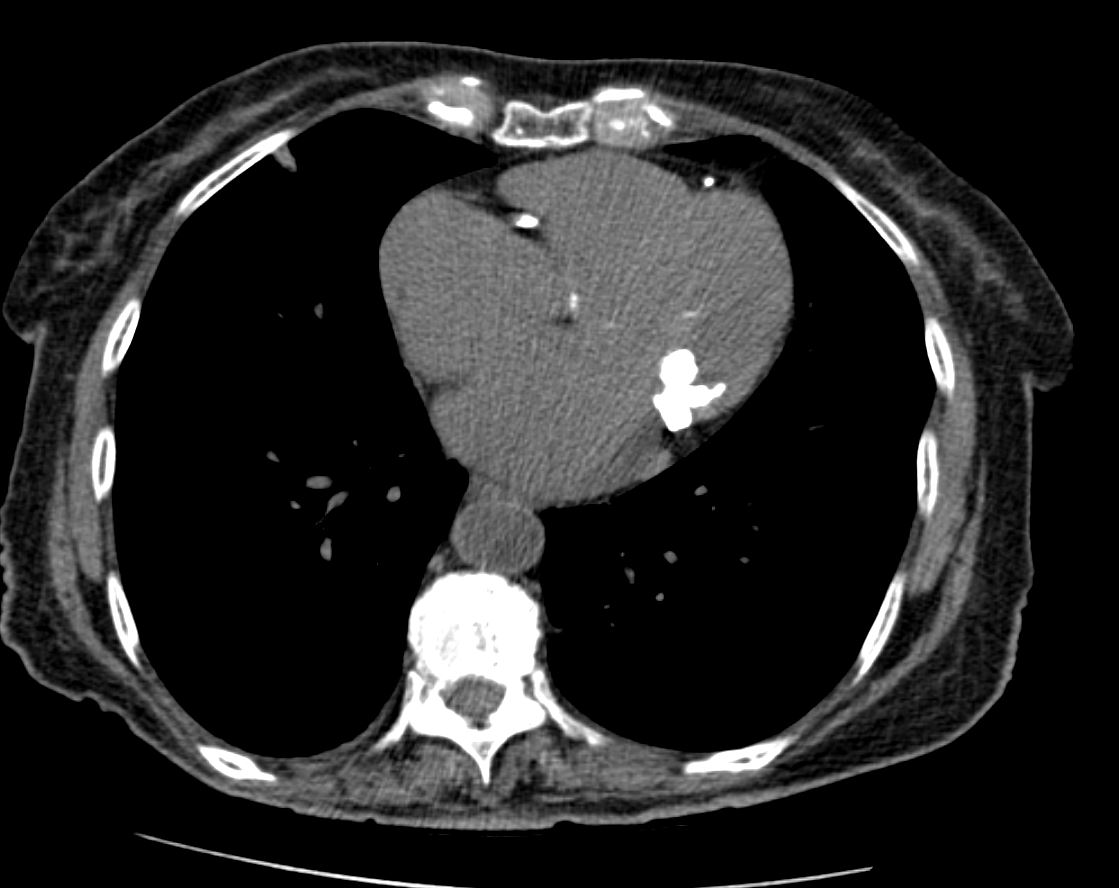
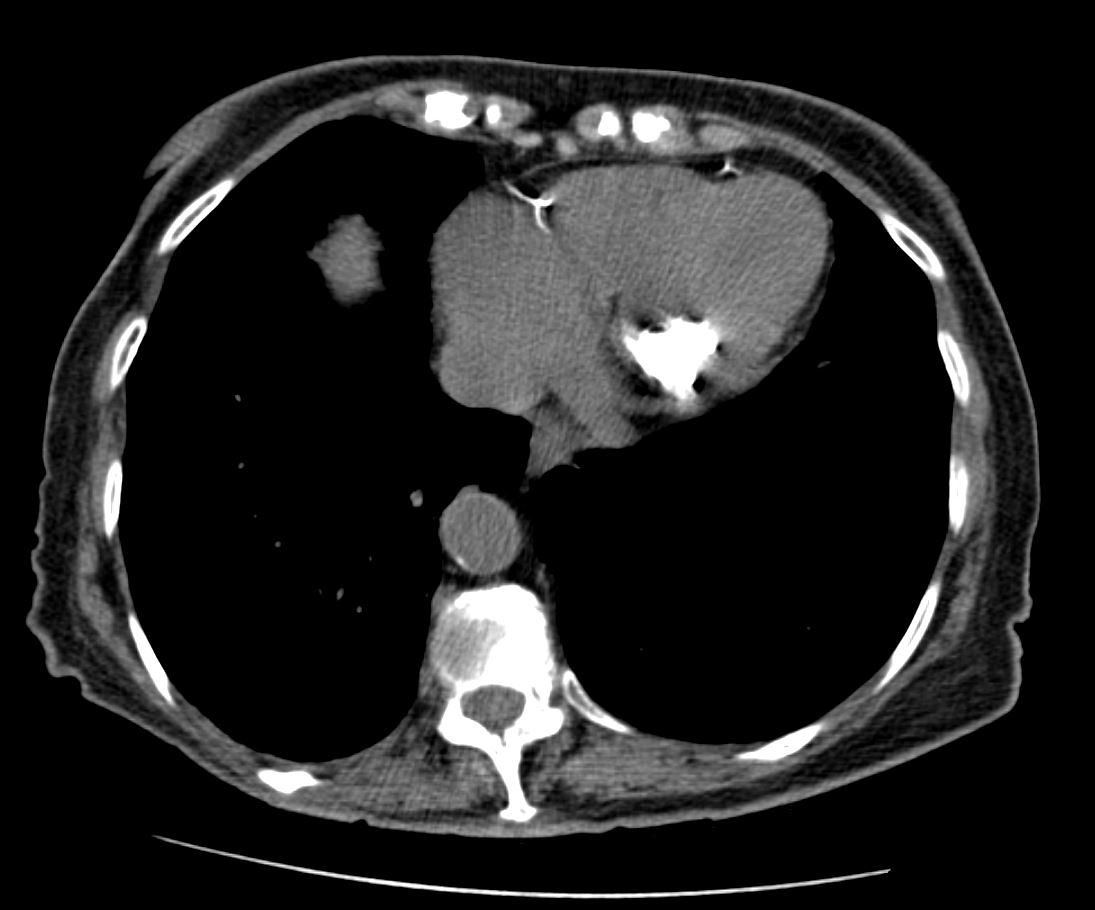
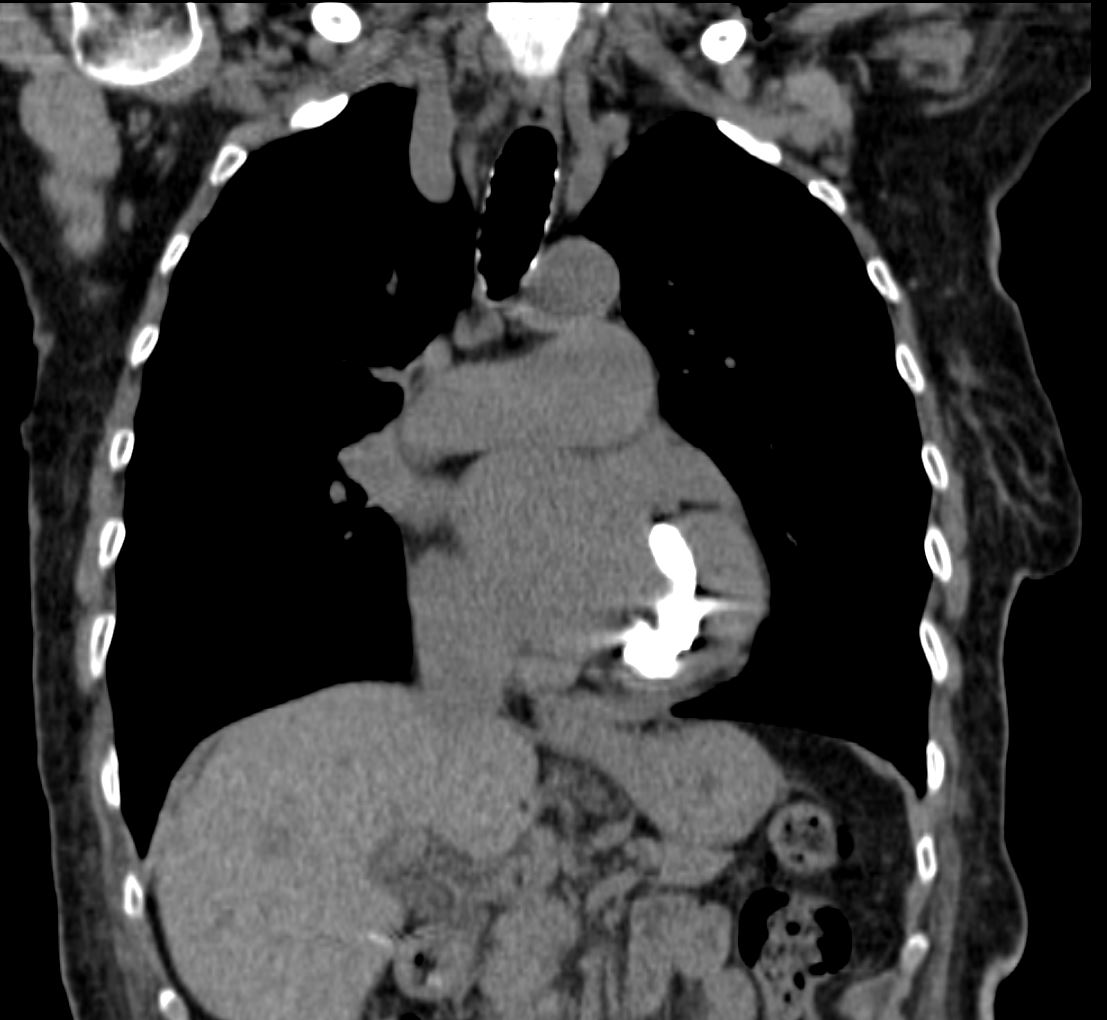
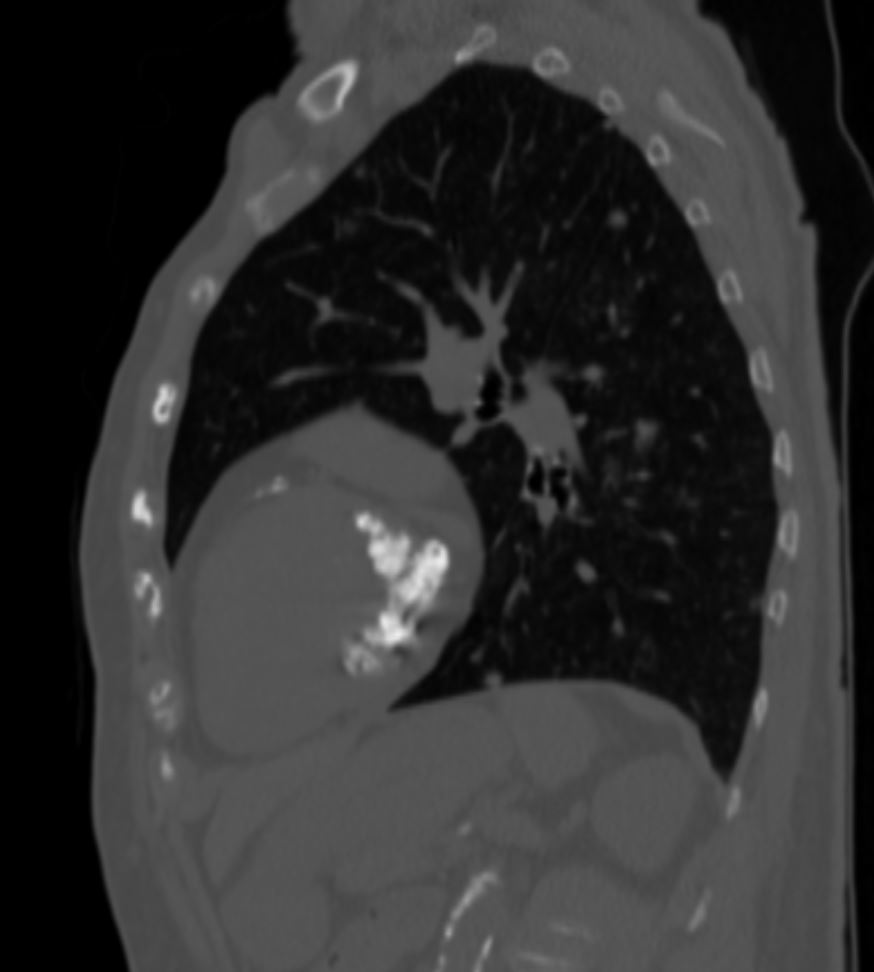
two small monoclonal peaks on IEF: a lambda LC and kappa LC. No specific therapy recommended then but yearly chest CT suggested – ?early MGUS.
PFT with low DLCO only and stable 2018-2019
AFIB controlled on BB
Dry eyes chronically related to Sjogren’s syndrome
Primary biliary cirrhosis
Hypothyroidism; post-surgical
H/O Mitral valve regurgitation
Poor GLS contours
Rhythm is AF
Mildly increased wall thickness, hyperdynamic LVEF. Aortic sclerosis without stenosis, mitral annular calcification.
MAC
Czeyda-Pommersheim F Radiographics Review