Definition
Adenocarcinoma with Lepidic Growth (aka BAC and Bronchiocarcinoma)

Histopathology
Histological sections of a group of alveoli filled with nests of malignant cells originating from and spreading along the alveolar epithelium without destroying the alveolar walls.(dark pink overlay) The cells seem to be almost hanging from the alveolar epithelium like washing from a washing line. Note groups of tall, columnar, mucin producing cells spreading along preexisting alveolar walls, which is typical of bronchioalveolar carcinoma.
Courtesy Dr Armando Fraire MD TheCommonVein.net 32828c08.8s
Partial Filling Of the Alveoli
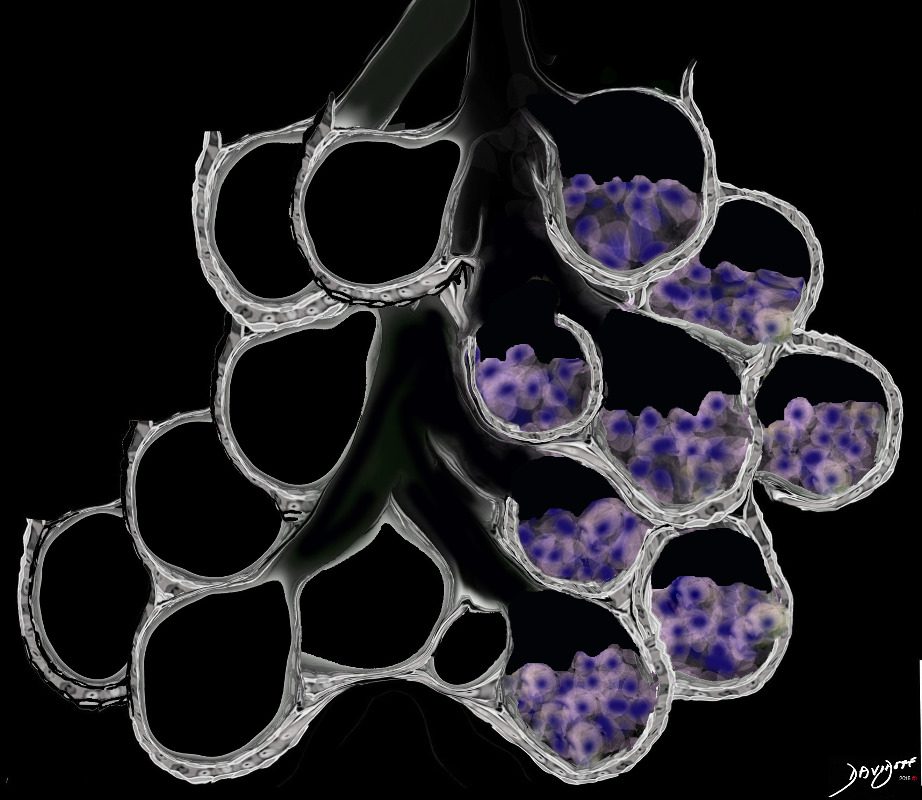
Ashley Davidoff MD TheCommonVein.net lungs-0707ad
Total Filling Of the Alveoli with Malignant Cells
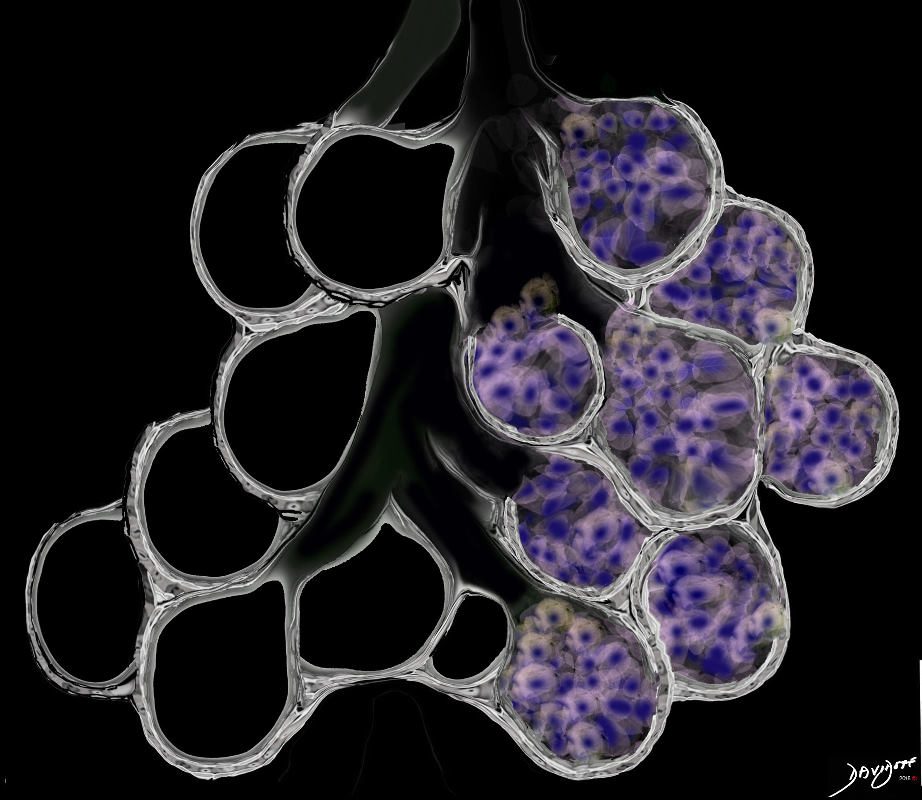
Consolidation is the replacement of air with solid material resulting in obscuration of blood vessels and airway walls The replacement may be due to cellular infiltration including inflammatory ,benign or malignant cells without or with fluid.
Ashley Davidoff MD TheCommonVein.net
lungs-0707d
Adenocarcinoma with Lepidic growth is a subtype of adenocarcinoma, accounts for about 5% of lung carcinomas but up to 20% are histologically mixed adenocarcinoma and BAC.
It has an indolent course and in its pure form, is really a carcinoma in situ, showing no invasive changes. It does have the potential to evolve into frankly malignant and invasive disease
Smoking appears to some extent be a causative link though it has a disproportionate high incidence among non smokers, women and occurs in a slightly younger population. About 30% of patients with BAC have never smoked. It also has a higher incidence in Japan.
BAC is sometimes associated with patients suffering from interstitial lung disease (eg scleroderma), and also with the uncommon entity of exogenous lipoid pneumonia. .
Structurally, it is characterized by its unique relatively slow lepidic growth, meaning it grows by scaling along the structure of the alveolus or acinus, but does not destroy the architecture. In addition in its pure form it does not invade vascular, lymphatic, or pleural elements.
When it shows invasive properties then it is defined as a mixed BAC adenocarcinoma. Raz There appears to be an evolving spectrum from benign to malignant, starting with premalignant atypical adenomatous hyperplasia, then BAC, and then into a subtype of adenocarcinoma. (Travis)
There is a mucinous form (80%) originating in the mucus secreting columnar cells, and tending to a multicentric pattern. The non mucinous form (20%) arises from the type II pneumocytes of the alveolus, is localized and has a better prognosis.
BAC appears to have characteristic heightened sensitivity to epidermal growth factor receptor tyrosine kinase inhibitors (EGFR-TKIs).
Clinically, patients in most instances are asymptomatic and many patients are identified by CT screening programs. When the disease is diffuse, bronchorrhea may occur.
The diagnosis is initially suspected radiologically presenting as a solitary ground glass opacity (GG0) (45%), as multicentric nodules (GGOs) (25%), or as a consolidation (30%). Inflammatory or infectious disease is considered in the differential diagnosis, but if the radiologic finding fail to respond to conservative therapy, BAC and its variants become more likely, and surgical biopsy is necessary.
When GGO’s are less than 2cms, they are usually pure BAC. As solid components within the GGO become more apparent, adenocarcinoma becomes more likely. When the disease is multifocal, it defines itself as IIIb or IV
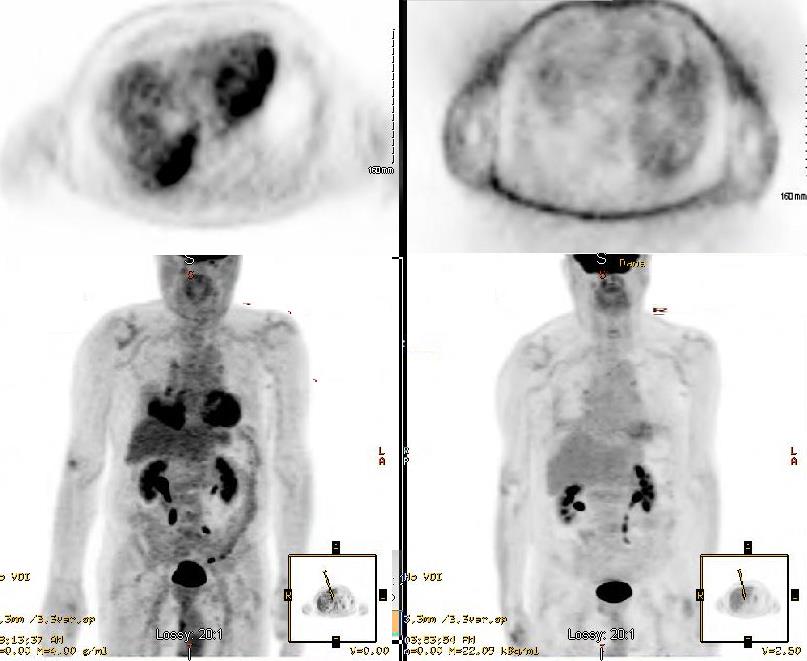
PET scanning has limited sensitivity so that only about 50% of lesions have a diagnostic SUV >2.5
The final diagnosis is made at pathology, and requires histological examination to determine invasion. Cytological aspiration is insufficient.
Treatment depends on staging. When in pure form – as an in situ disease by definition, treatment is surgical and curative. Surgery usually consists of lobar resection, and ipsilateral mediastinal lymphadenectomy. When in the mixed form 10-25% have lymph node involvement and 5% have distant metastases and therefore require additional radiation and chemotherapy.
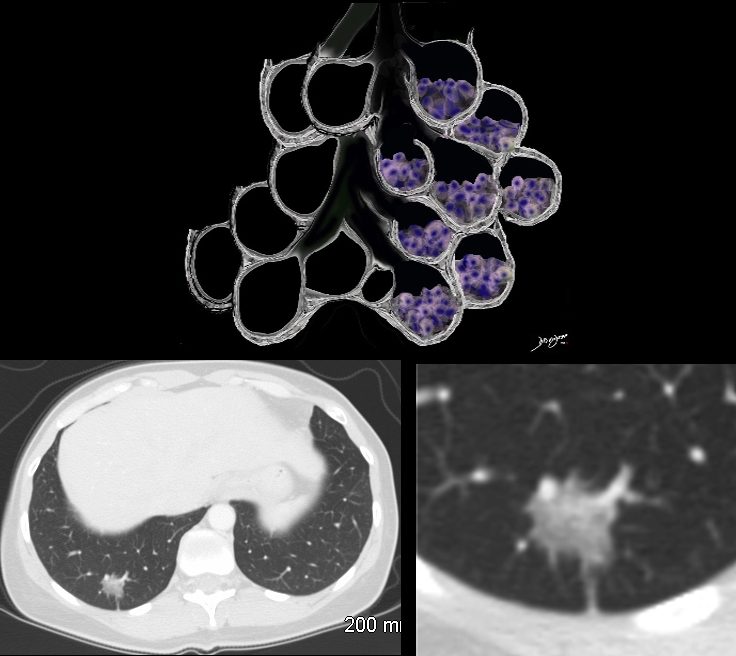
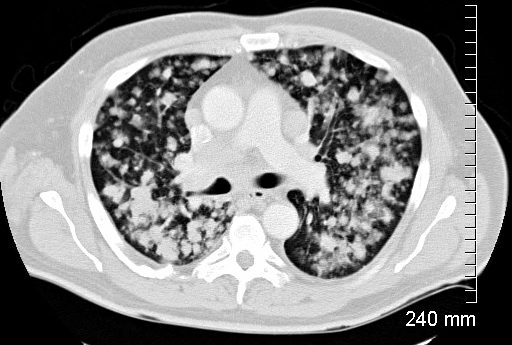
The Ground Glass Opacity (GGO) in this case is caused by partial filling of the alveolus with malignant cells Ground glass opacification may be caused by partial filling of the alveolus with cellular material resulting in partial replacement of air with solid material. The net density is gray rather than white in the situation where the alveolus is fully replaced with cells or fluid. There is blending of the black of the subtending airways and the white of the vessels with the gray density of the cellular infiltrate and hence the normal vessels are not visualized in ground glass opacities.
Ashley Davidoff MD TheCommonVein.net 134375b01

GGO in the secondary lobule reflects alveolar process and is one of the presenting appearances of unifocal or multifocal BAC. It is a slow growing in situ disease that may not change in size over two years but continued surveillance is necessary.
Courtesy Ashley Davidoff MD
TheCommonVein.net
45465b01
Ashley Davidoff
TheCommonVein.net
134372
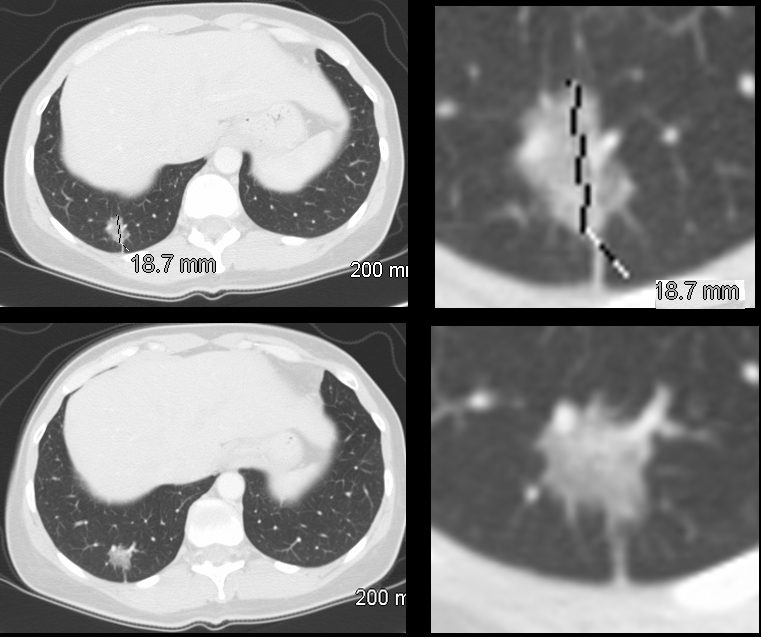
The CT is from a 51 year old male who is a smoker who shows three areas areas of ground glass opacity in the right lower lobe, two that measure close to 2cms each and a third more anterior that measures about 8mms. This case represents multicentric adenocarcinoma with lepidic growth
Courtesy Ashley Davidoff MD
TheCommonVein.net
87755.8s
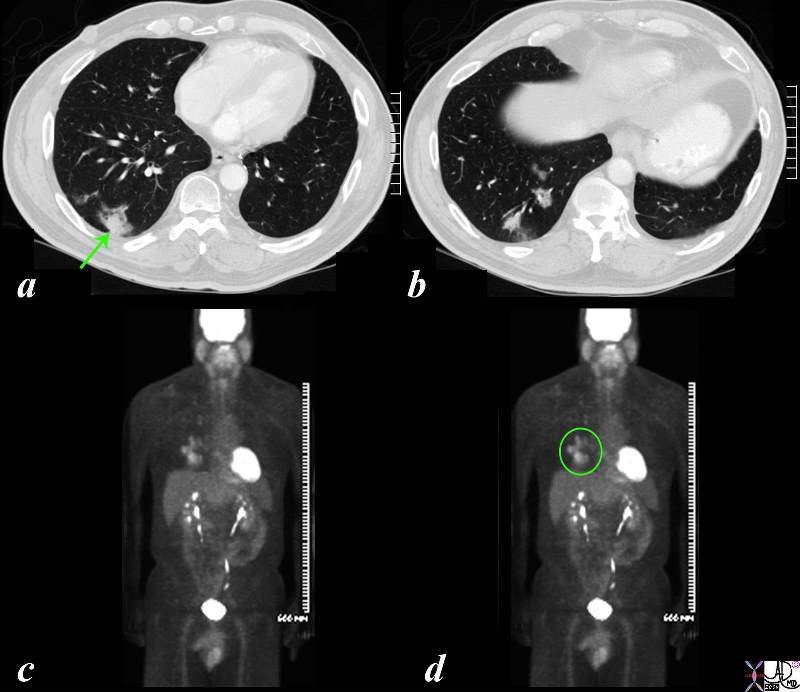
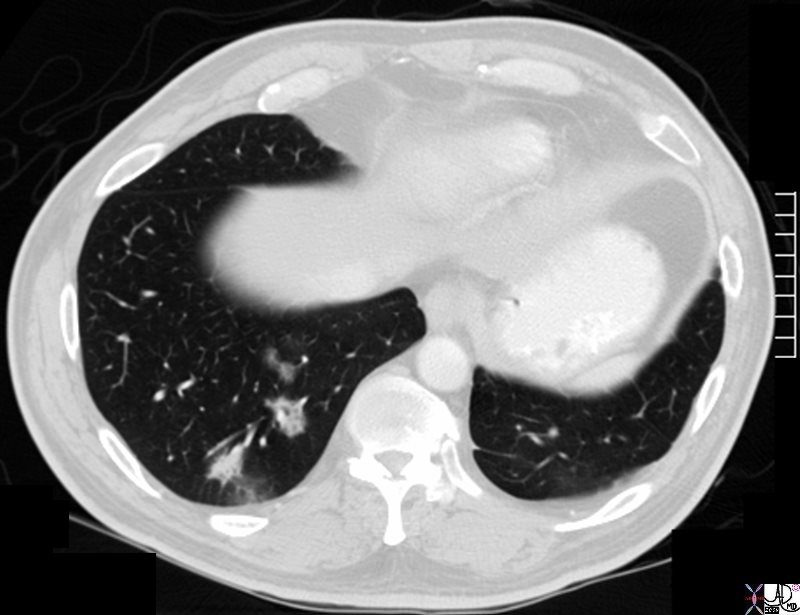
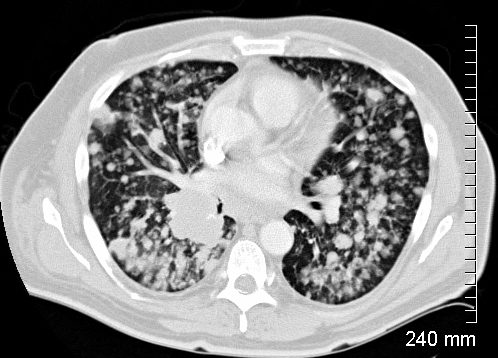
The CT is from a 51 year old male who is a smoker who shows a ground glass opacity (GGO) mixed with a solid mass (arrow in a) and multicentric BAC in a lower cut (b) characterised by three areas in the right lower lobe of partial alveolar opacification. Ground glass appearance is the result of partial opacification of the alveoli. Two of the GGOs measure close to 2cms each and the third more anterior measures about 8mms. In this instance a PET scan was positive in the area (green ring in d) It is likely that the solid component in image a represents the transformation of BAC – (really a carcinoma in situ) into adenocarcinoma.
Courtesy Ashley Davidoff MD
TheCommonVein.net
87769c02b.8s
Radiological Presentation as a Solid Nodule or Consolidation
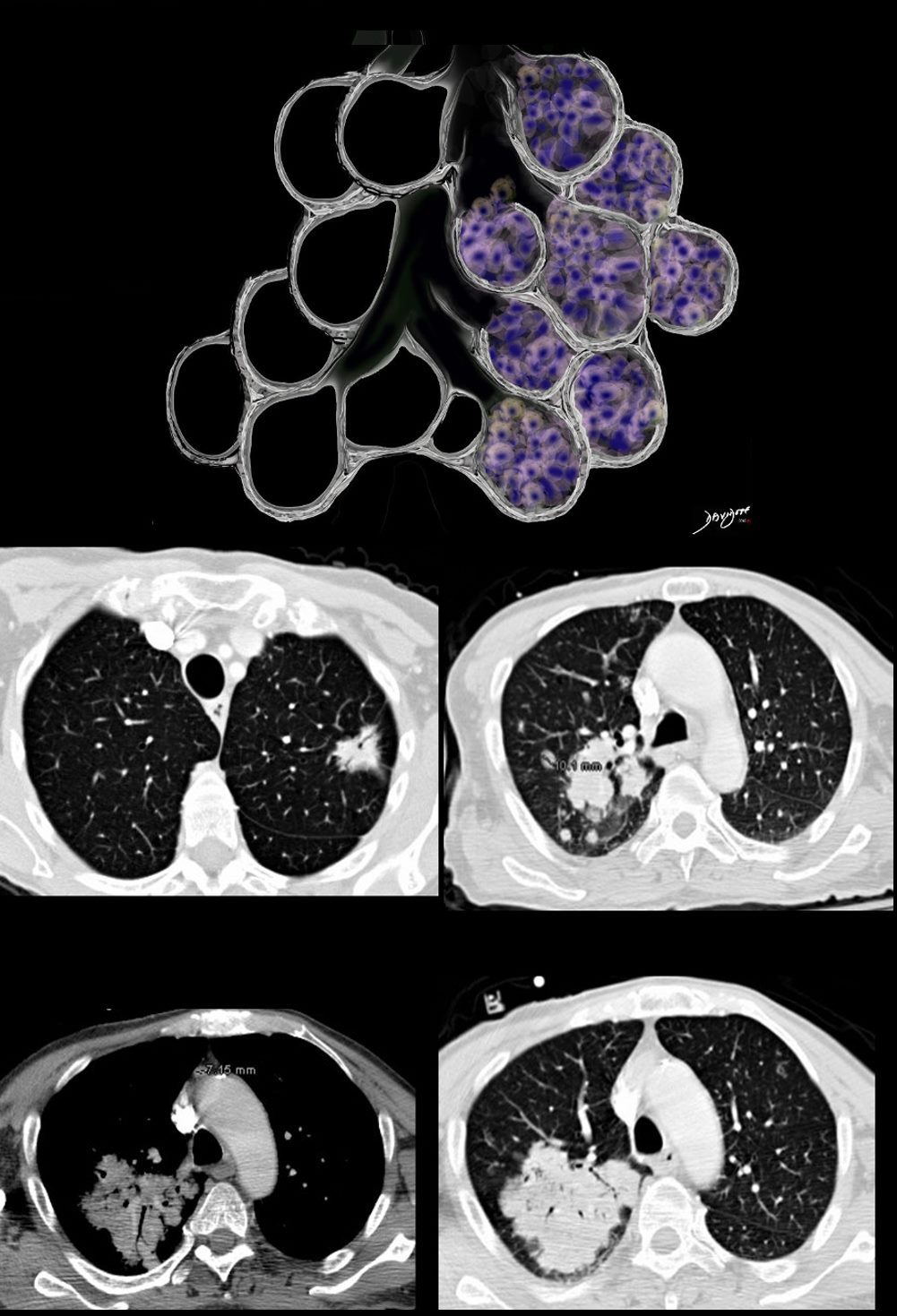
The focal nodules (middle row) and segmental consolidation in the right upper lobe (lower row) in this case is caused by total filling of the alveoli with malignant cells. This results in opacification of the alveoli and the “white” density in contrast to the “black” airways, enable the airways to be visualised as air bronchograms
Ashley Davidoff MD TheCommonVein.net 87770c01
Adenocarcinoma with Lepidic Growth Lingula Infiltrate Masquerading as a Pneumonia
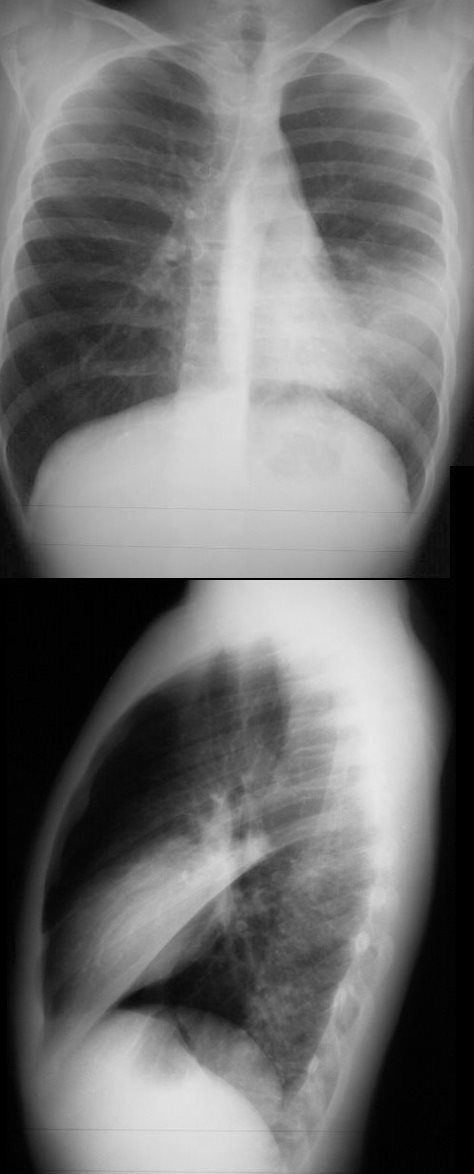
43 year old male with pneumonic consolidation of malignant origin
Ashley Davidoff MD TheCommonVein.com 31791c
Adenocarcinoma with Lepidic Growth is Characterized by Any or All of the Following Features; Multicentricity, Segmental Consolidation, Solid Round Nodules, Solid Spiculated Nodules Ground Glass Nodules, and Mixed Nodules
The Following Case Demonstrates All of the Features
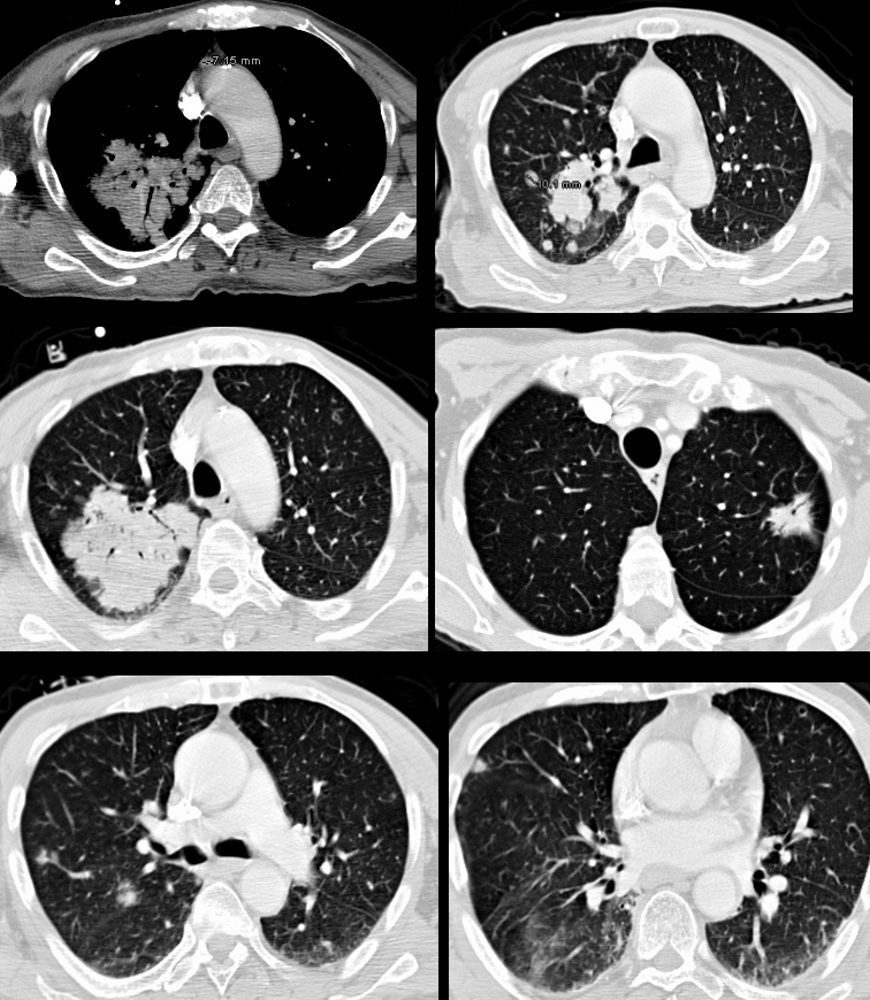
Ashley Davidoff TheCommonVein.net 87770c
Pre and Post Op Studies – 79 year old Male with Adenocarcinoma with Lepidic Growth
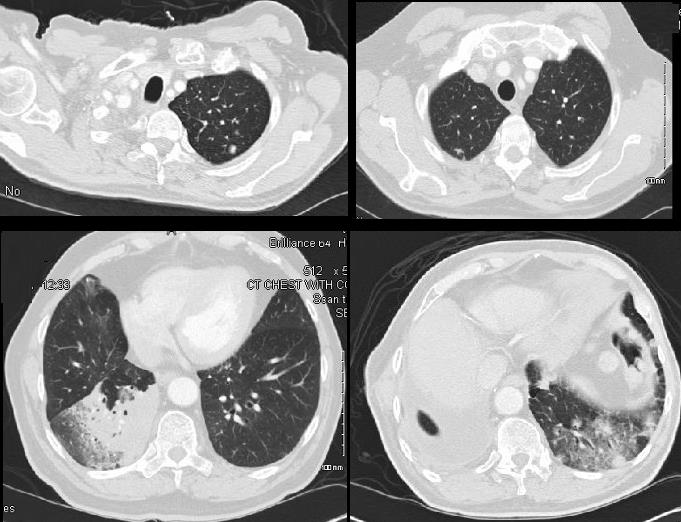
Ashley Davidoff
TheCommonVein.net
79M adenoca with lepidic growth 001
Ashley Davidoff TheCommonVein.net 79M adenoca with lepidic growth 002
Presenting with Solid Nodules

Ashley Davidoff TheCommonVein.net 134362
Adenocarcinoma with Lepidic Growth Presenting with Diffuse Nodular Disease, Ground Glass Changes Some Nodules are Centrilobular in Location
Ashley Davidoff MD TheCommonVein.net 134332
Ashley Davidoff MD
TheCommonVein.net
134334
Ashley Davidoff MD
TheCommonVein.net
134336
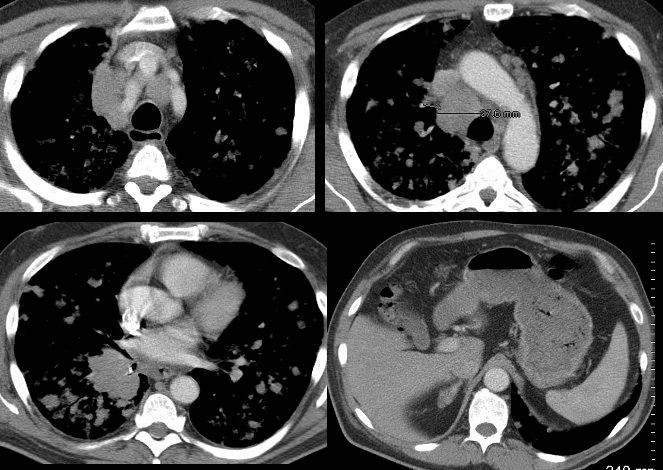
This set of 4 images shows extensive mediastinal and hilar adenopathy and a nodular right adrenal gland most likely reflecting a metastasis (bottom right image)
Ashley Davidoff MD
TheCommonVein.net
134326c
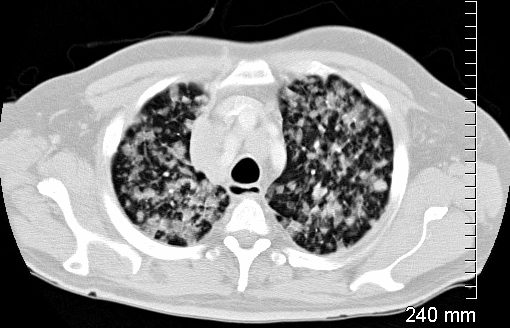
Diffuse Ground Glass Changes with Crazy Paving

shows a bilateral crazy-paving pattern and centrilobular nodules. (b) Photomicrograph (original magnification,
400; hematoxylin-eosin stain) of a specimen from open lung biopsy shows replacement of the alveolar epithelium
by epithelial neoplastic cells with abundant intracytoplasmic mucin (arrows).
Rossi, S.E et al “Crazy-Paving” Pattern at Thin-Section CT of the Lungs: RadiologicPathologic Overview Radiographics Volume 23 – Number 6, 2003
