Chronic obstructive pulmonary disease
- really consists of four anatomic lesions
- emphysema,
- small airway remodeling,
- vascular remodeling with pulmonary hypertension,
- mucus overproduction and
- chronic bronchitis
- there is airflow obstruction.
- Membranous bronchioles
- terminal bronchioles
- lined by columnar epithelial cells with cilia.
- respiratory bronchioles are
- lined by transitioning columnar to cuboidal epithelium and lead into
- alveolar ducts and alveolar spaces with
- flattened epithelium
-

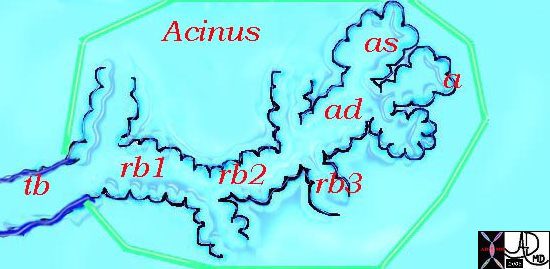
Acinus.
This diagram illustrates the acinus which consists of the respiratory bronchioles (rb 1, 2, 3) the alveolar duct (ad) the alveolar sac (as) and the alveoli. (a)
Courtesy Ashley Davidoff MD 42446b12
TheCommonVein.net
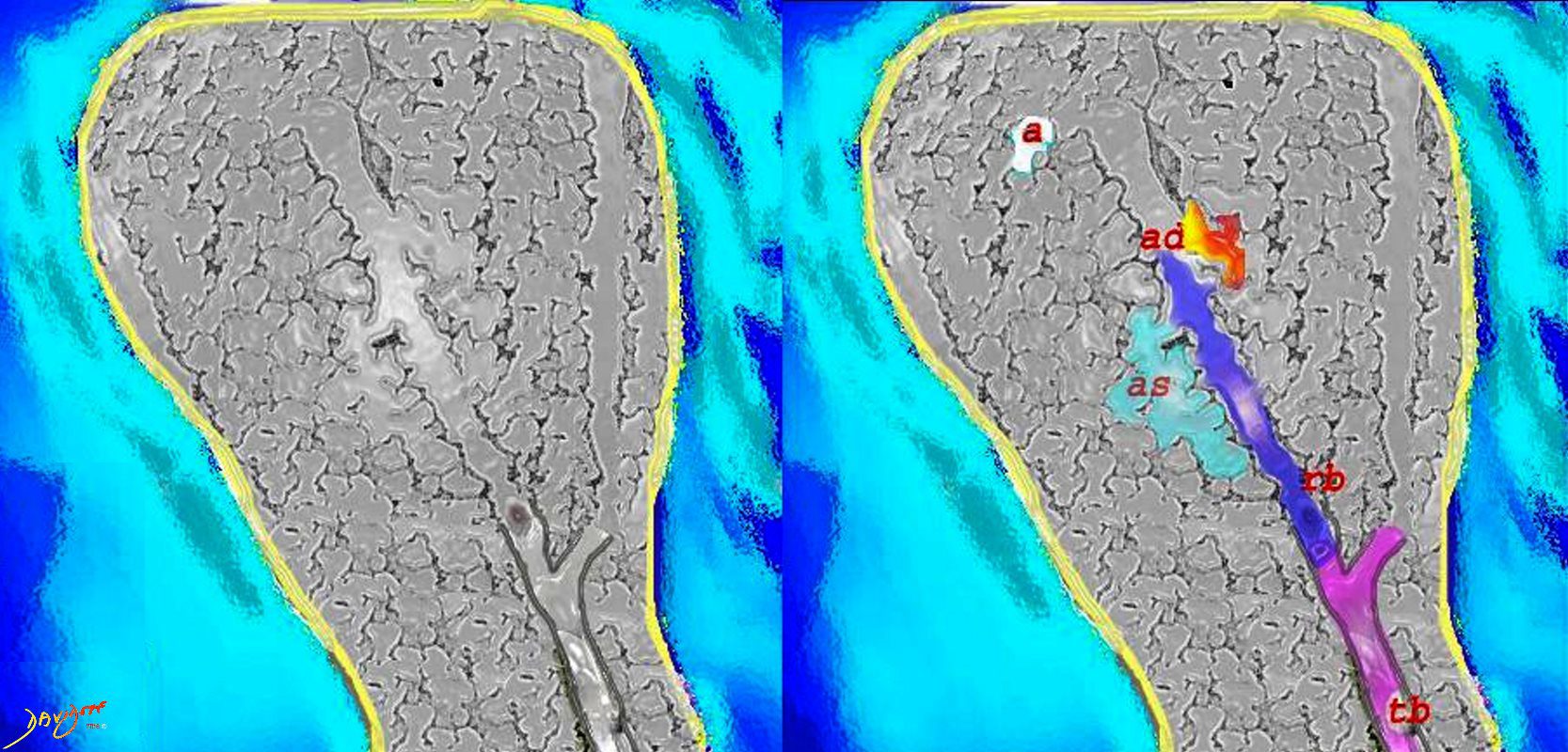
The diagram shows the structure of the airways and alveoli at the level of the secondary lobule. The terminal bronchiole (tb- pink) enters the secondary lobule and terminates in the respiratory bronchiole (rb purple) which lies in the center of the the secondary lobule (centrilobular). It gives rise to alveolar duct (ad yellow)which gives rise to the alveolar sac (as, teal blue. Finally the as terminates in the alveoli (a white)
Courtesy Ashley Davidoff MD
lungs-0028-low res -

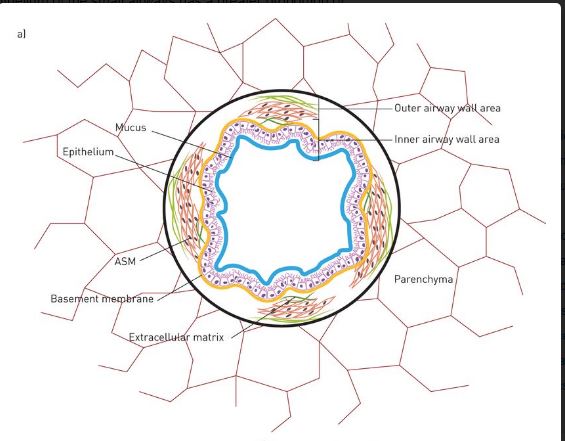
a) Schematic drawing of a cross section of a normal small airway embedded in the lung parenchyma. The different compartments and components of the airway wall are shown.
van den Bosch, W. B. et al Structure and function of small airways in asthma patients revisited European Respiratory Review 2021 30: 2001
- terminal bronchioles
-

Photomicrograph (haematoxylin & eosin stain, magnification ×20) of a) a small airway of a healthy subject Images courtesy of J.H. von der Thüsen (Dept of Pathology, Erasmus MC, University Medical Center Rotterdam, Rotterdam, The Netherlands).
van den Bosch, W. B. et al Structure and function of small airways in asthma patients revisited European Respiratory Review 2021 30: 2001
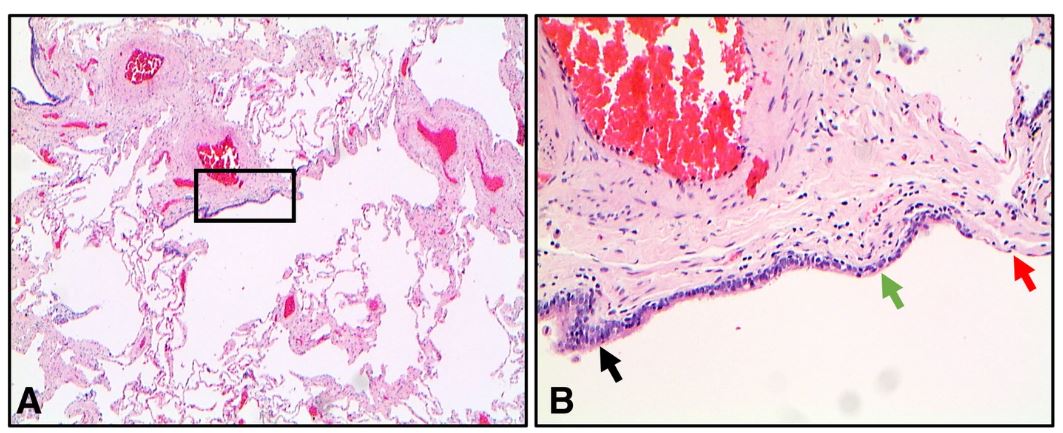
ransitioning epithelial structure in a respiratory bronchiole. a A bronchiole demonstrating transition from the columnar epithelium to cuboidal epithelium and finally to flattened alveolar epithelium (2X magnification). b An enlarged image of the inset from image A showing columnar epithelium (black arrow), cuboidal epithelium (green arrow) and flattened epithelium (red arrow) (10X magnification). Section stained with hematoxylin and eosin
Higham A et al The pathology of small airways disease in COPD: historical aspects and future directions Respiratory Research volume 20, Article number: 49 (2019)
Histopathological features of small airways disease in COPD. a A COPD bronchiole with a thickened airway wall due to fibrotic remodeling and excessive deposition of collagen bundles (blue colouration). Section stained with Masson’s Trichrome (10X magnification). b A COPD bronchiolevascular bundle whereby the bronchiole contains a large intra-luminal mucous plug (red arrow) (2X magnification). Section stained with hematoxylin and eosin. c A COPD bronchiole with increased numbers of goblet cells (greenarrows) in the epithelial lining (20X magnification). Section stained with hematoxylin and eosin. d The wall of a COPD bronchiole with increased numbers of inflammatory cells (black arrows) (20X magnification). Section stained with hematoxylin and eosin
Higham A et al The pathology of small airways disease in COPD: historical aspects and future directions Respiratory Research volume 20, Article number: 49 (2019)
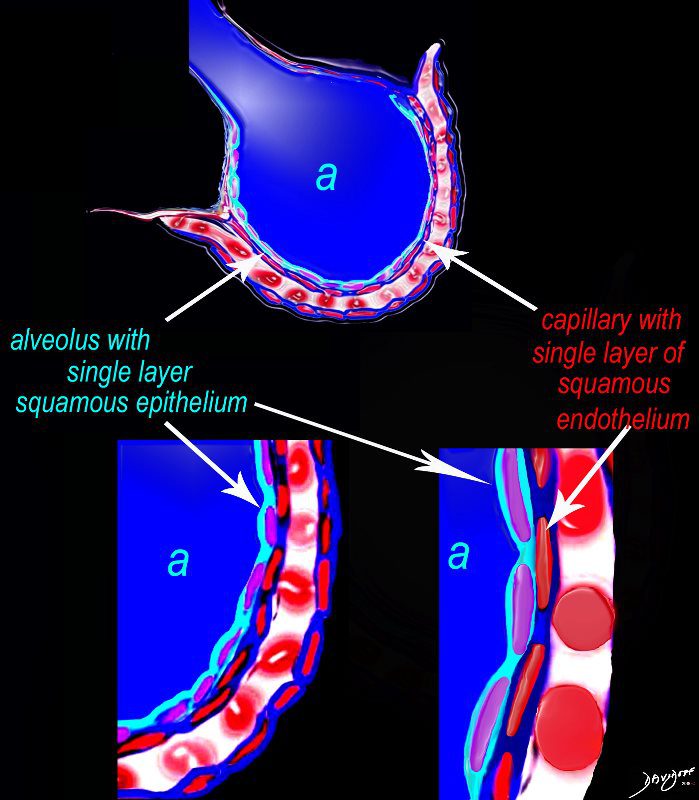
Alveolus at a Cytologic Level
The diagram shows an alveolus (a) above, lined by a single layer of squamous cells, surrounded by a capillary with red cells which is also lined by a single layer of squamous endothelial cells . The images below show progressive magnification of the alveolar wall demonstrating the two thin layer of the alveolar membrane .
Courtesy Ashley Davidoff 2019
lungs-0028-low res - Caused by smoking and exposure to pollution.
- Results in shortness of breath, breathing difficulties, coughing, more mucus produced, wheezing, exercise problems, and chest pain.
-

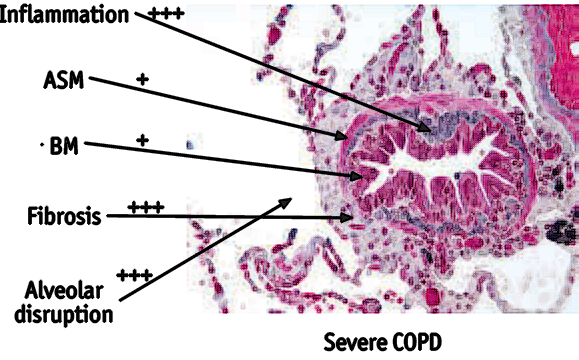
In severe COPD there is infiltration of inflammatory cells. The airway smooth muscle (ASM) layer is only hypertrophied to a minimal degree in COPD. In COPD collagen is deposited mainly around the airway (peribronchiolar fibrosis). The alveolar attachments are disrupted in COPD as a result of emphysema. Modified image courtesy of J. Hogg (iCAPTURE Centre, St Paul’s Hospital, Vancouver, BC, Canada).
Revised from an article Barnes P , Mechanisms in COPD compared with asthma Semantic Scholar - Diagnosed by observation, chest inspection, listening to respiratory sounds, chest x-ray, chest CT scan, oxygen level measurement, and pulmonary function tests.
- Treated by bronchodialtors, stopping smoking, steroids, antibiotics, low-flow oxygen, ventilation, intubation, srugery, and transplant.
Links and References
Barnes P , Mechanisms in COPD compared with asthma semantic Scholar
Higham A et al The pathology of small airways disease in COPD: historical aspects and future directions
Respiratory Research volume 20, Article number: 49 (2019)