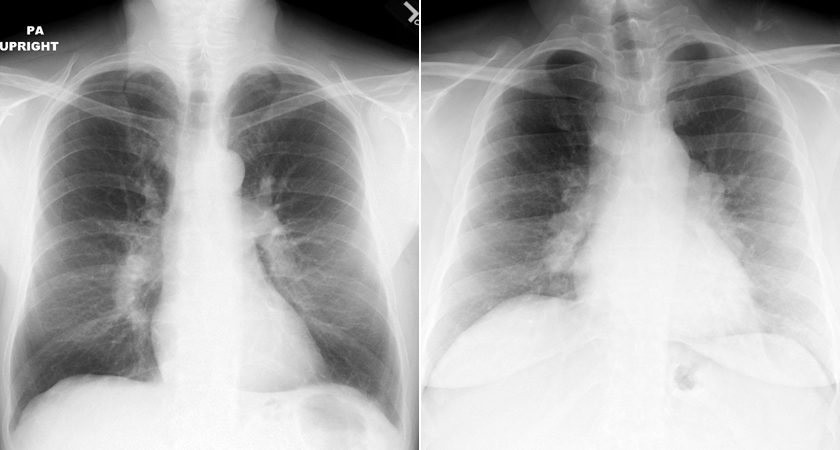
The left image shows bilateral pulmonary artery enlargement. Note the smooth contours of the arteries. The image on the right shows lumpy-bumpy opacities characteristic of hilar adenopathy
Courtesy Med Ed Virginia
Sarcoidosis

31- year-old male with stable mediastinal and hilar adenopathy, no parenchymal disease, with splenomegaly and an enlarged main pulmonary artery . The cardiac echo was normal without pulmonary hypertension
The widened carina is likely as a result of the subcarinal adenopathy
Ashley Davidoff MD

70 year old male with history of sarcoidosis presents with a cough. There upper lobe retractile reticular process associated bilateral hilar /mediastinal egg shell calcifications of the lymph nodes
Ashley Davidoff MD

70 year old male with history of sarcoidosis presents with a cough. There upper lobe retractile reticular process associated bilateral hilar /mediastinal egg shell calcifications of the lymph nodes
Ashley Davidoff MD
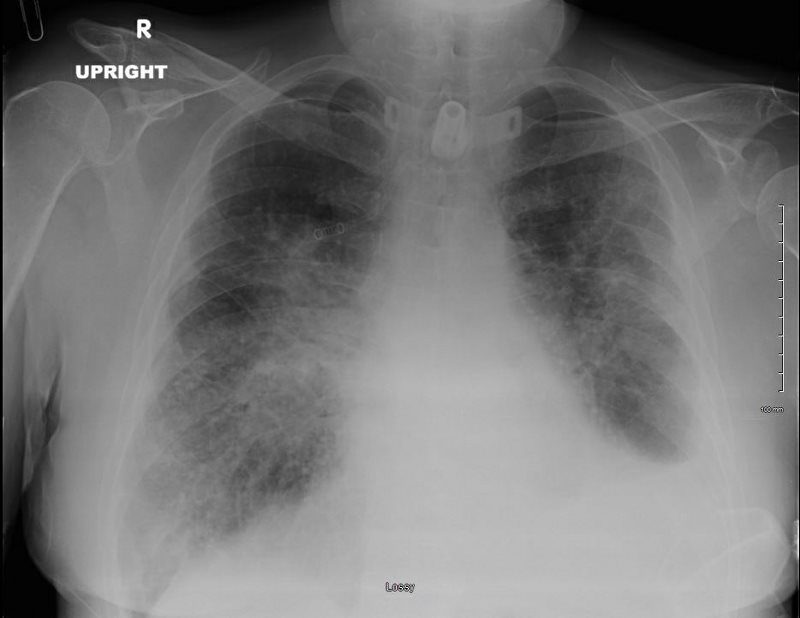
SARCOIDOSIS, STAGE IV, PTX, ENCASEMENT
50-year-old male presents with history of Stage 4 sarcoidosis acute chest pain and dyspnea
The initial CXR shows a left sided pneumothorax, diffuse nodular pattern with confluent perihilar infiltrates and a left pleural effusion
A chest tube was placed and a chest CT showed confluent fibrotic masses in the hilar regions totally surrounding the bronchovascular bundles with encasement of the middle lobe artery. In addition, multiple lymphovascular micronodules are demonstrated. The pulmonary artery measures 32.7mm indicating pulmonary hypertension.
A CXR during this admission shows re-expansion of the pneumothorax. Left lung volume is reduced.
The patient presents 2 years later, again with progressive dyspnea and chest pain and CT PA shows encasement of the airways, right middle lobe pulmonary artery and left lower pulmonary vein by the fibrotic broncho vascular masses, and non-occlusive, subacute pulmonary embolus of the LPA. There are moderate bilateral pleural effusions, calcified lymph nodes, with ongoing pulmonary hypertension with right ventricular enlargement, right atrial enlargement, tricuspid regurgitation and pulmonary hypertension. At this time the patient is intubated.
He again presents 1 month after with chest pain and dyspnea. At this time, he has a tracheostomy. The scout frontal view shows persistent encasement of the left upper lobe bronchus and significant reduction on the volume of the left lung with elevated left hemidiaphragm.
CT PA has similar findings with a large right pleural effusion and unresolved large non occlusive thrombus in the left pulmonary artery.
Ashley Davidoff MD
