reference
https://www.youtube.com/watch?v=5wn916moUy8
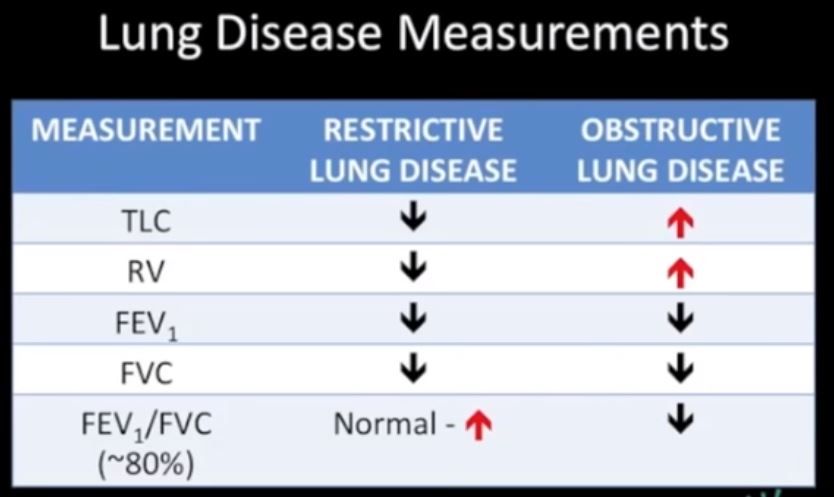
TLC Total Lung Capacity = Amt of air when lungs are maximallly filled
RV residual volume = amount of air left in the lungs after maximal expiration
FEV1 – Forced expiration after 1 second of expiration is the amount of air that comes out in 1st second of expiration
FVC Forced Vital Capacity – Is the total volume of air of air that can exhaled after after a maximal inspiration
Lung Volumes
In order to explain the process we will pretend that you are a lung function technologist for a moment. You are going to test your patient’s lung volumes, capacities and velocities. We want you to think and apply what you see on these graphs to your own situation when you are doing a CXR, and to imagine the differences between an inspiration CXR and expiration CXR. We particularly want you to see the difference in volume of air between the inspiration film and the expiration film.
So we go back to our theoretical patient undergoing lung function tests and we place a mouthpiece over her mouth and attach the tubing on the other end to a recording device called a spirometer. As our patient lies on the table breathing quietly under resting conditions we notice a simple rhythmic pattern on the spirogram. This pattern is entirely involuntary caused by the production of a signal from center of respiration located in the brain that causes the diaphragm and other muscles to contract and to expand the chest, and then as it switches off, the muscular relaxation and elastic recoil cause the chest to contract.
Tidal Volume
Courtesy of: Ashley Davidoff, M.D.
TheCommonVein.net
42529b06b01b
We reset our spirometer to get our basal conditions set between the 3 and 4 liter mark so that we have room on the graph to see what happens with forced inspiratory effort and forced expiratory effort.
For those of you who require your patient to “breath hold” for MRI and CT, we are in fact asking them to stop this involuntary breathing pattern in order to prevent chest wall and lung movement that would otherwise cause motion artifact on our images.
For our CXR we now ask our patient to take as deep a breath in as possible and we see a dramatic change on the graph.
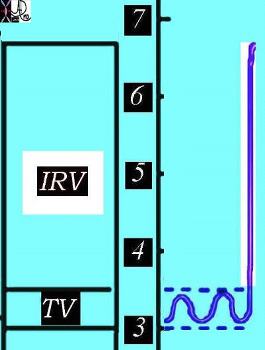
Inspiratory Reserve Volume
Courtesy of: Ashley Davidoff, M.D. TheCommonVein.net 42529b06b02
When we ask your patient to take a deep breath in we have a similar experience but the change is reflected in a CXR is a larger chest volume by more than 3 liters. The patient will muster their muscular forces to contract the diaphragm and intercostal muscles to enlarge the chest cavity and pull in air. The lung in the healthy patient will now contain about 6.7 liters of air. When our patients can take a deep breath and hold it in, the radiologists are better able to identify disease processes since the interface of air and the soft tissue of the disease is larger and therefore the disease is more easily seen.
For those of you who are ultrasound technologists you use the consequences “deep breath in” to bring the diaphragm and upper abdominal organs down, beyond the rib cage, in order to optimize your window to the upper abdomen.
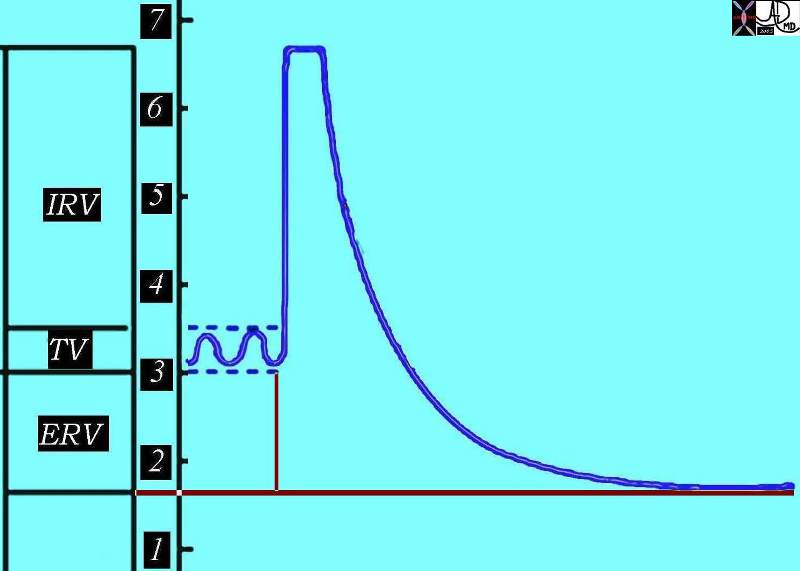
Now as the patient reaches peak inspiration we tell her to breath out as completely and rapidly as possible, and our spirometer reading does the following;
Forced Expiration
Courtesy of: Ashley Davidoff, M.D. TheCommonVein.net 42529b06aa02
The difference between the end of basal expiration and complete expiration is called the expiratory reserve volume. (ERV)
For the lung function technologist the speed with which the expiration is performed is a key issue in lung function, but for you the degree to which the patient can empty their lungs is key for a good expiration film.
At the end of this complete expiration, there is still a volume of air left in the lungs and airways, and this is called the residual volume (RV), which is the air filled space that keeps everything open after a full expiration. When we perform a CXR in expiration, we ask our patients to breathe in and then all the way out, and to hold it out, and we then expose our film. The air you see in the lungs at the end of expiration is called the residual volume. The lungs are at their smallest volume in end expiration and at this point contain about 1.5-1.7 liters in our patient. In the normal adult the RV ranges between 1.0 and 2.4 liters.
Residual volume
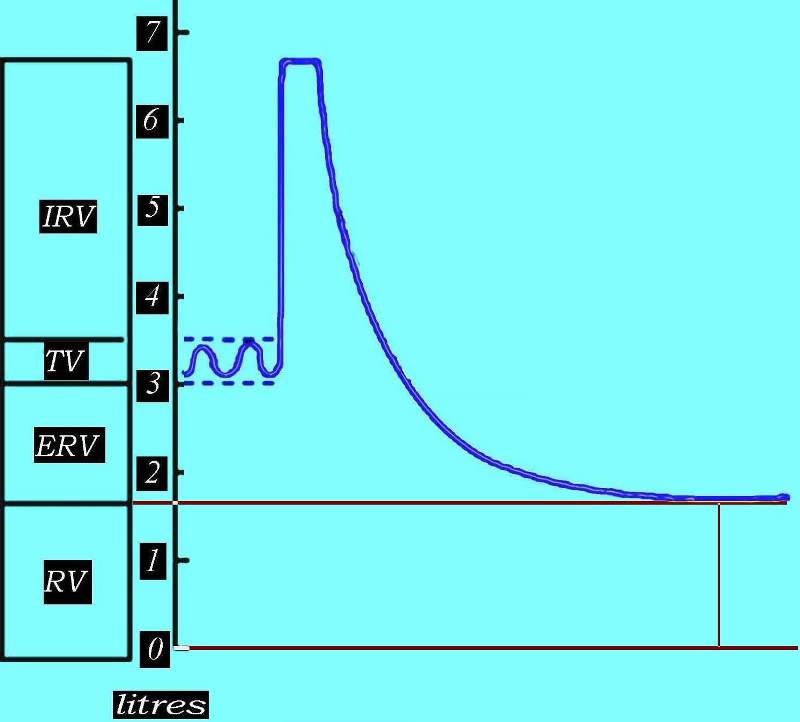
This diagram outlines the residual volume between the red lines, representing the air that is left in the airways and the alveoli after a full expiration. The air you may see on expiration CXR is the residual volume and as you can see it is about 1.8 liters in this patient.
Courtesy of: Ashley Davidoff, M.D. TheCommonVein.net
42529b06aa03
Lung Capacities
We now move on to our patient’s lung capacities, which represent a combination of the volumes we have spoken about. What do you think inspiratory capacity is? It is of course the combination of the basal inspiration which is our tidal volume of 500css combined with the inspiratory reserve volume (3.2liters) giving us a total of a 3.7 liters capacity for inspiration
Inspiratory Capacity
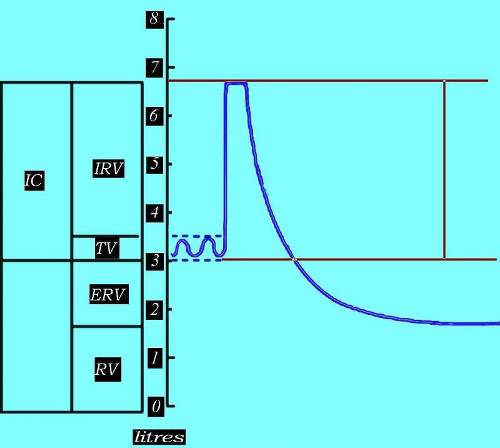
The inspiratory capacity (IC) is the total volume that the person can inspire, and is a combination of the inspiratory component of the tidal volume and the inspiratory reserve volume.
Courtesy of: Ashley Davidoff, M.D. TheCommonVein.net 2529b06aa04
Functional Reserve Capacity (FRC).
The amount of air left in the lungs after a resting expiration includes the expiratory reserve volume and the residual volume is called the functional reserve capacity (FRC).
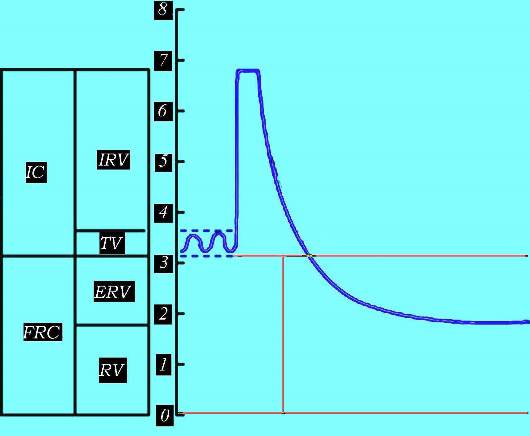
The combination of ERV and RV is called the functional residual capacity (FRC) as marked by the vertical red line
Ashley Davidoff, M.D. TheCommonVein.net 42529b06aa05d
The vital capacity (VC) is defined as is the maximum volume of air expelled after a maximum inspiration. For you, this is the difference in amount of air in the lungs between a CXR with maximum inspiration and a CXR with maximum expiration. In this patient it is about 5 liters – a large difference in volume and a large difference in the appearance of the chest, sometimes making the difference as to whether a pneumothorax is seen or not seen. Why is this so important? A small pneumothorax itself may not have any functional significance meaning the patient has no untoward effect. It does however reflect a leak, and a leak can get better or worse. In the situation in which it gets bigger it can cause a life threatening situation and so it is essential to make the diagnosis of even a small pneumothorax. Using expiration technique for the clinical question of pneumothorax is essential. .
Vital Capacity (VC)
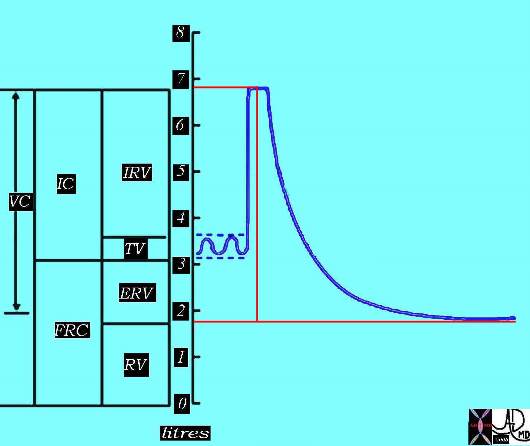
The vital capacity is the maximum volume of air expelled after a maximum inspiration. It also can be viewed as the maximum amount of air that the patient can move in and out of his or her lungs.
Courtesy of: Ashley Davidoff, M.D. TheCommonVein.net 42529b06aa06bd
Total Lung Capacity
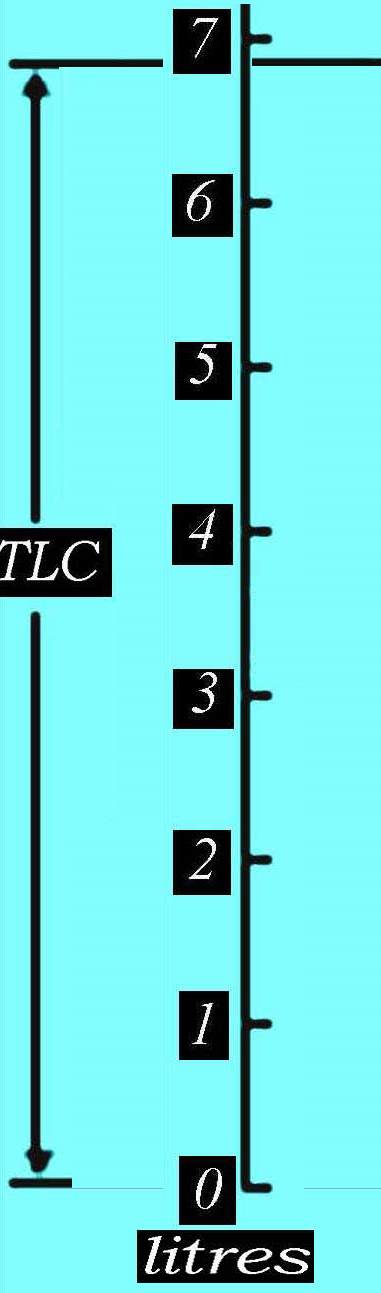
The total amount of air in the lungs after a deep inspiration is called the total lung capacity and is a combination of the vital capacity VC and the residual volume. Thus it is a combination of the maximum volume of air that the patient can move in and out of his lungs and the air that remains in the lungs after a forced expiration. In our patient it is about 6.8 liters. Courtesy of: Ashley Davidoff, M.D. TheCommonVein.net 42529b06aa
Total Lung Capacity
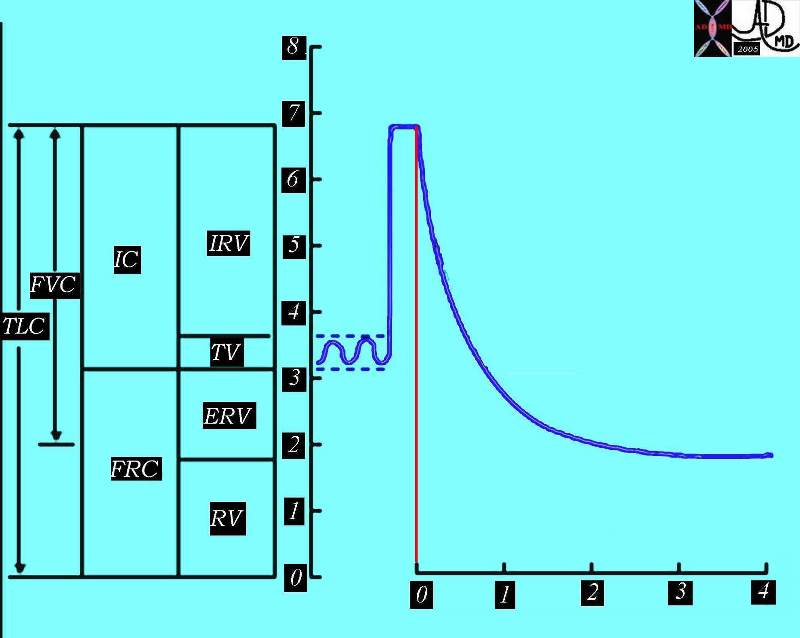
The total lung capacity (TLC) is the total amount of air in the lungs and airways after a deep inspiration. In our patient it is about 6.8 liters.
Ashley Davidoff, M.D. TheCommonVein.net 42529b06aa07
Ventilation and Perfusion
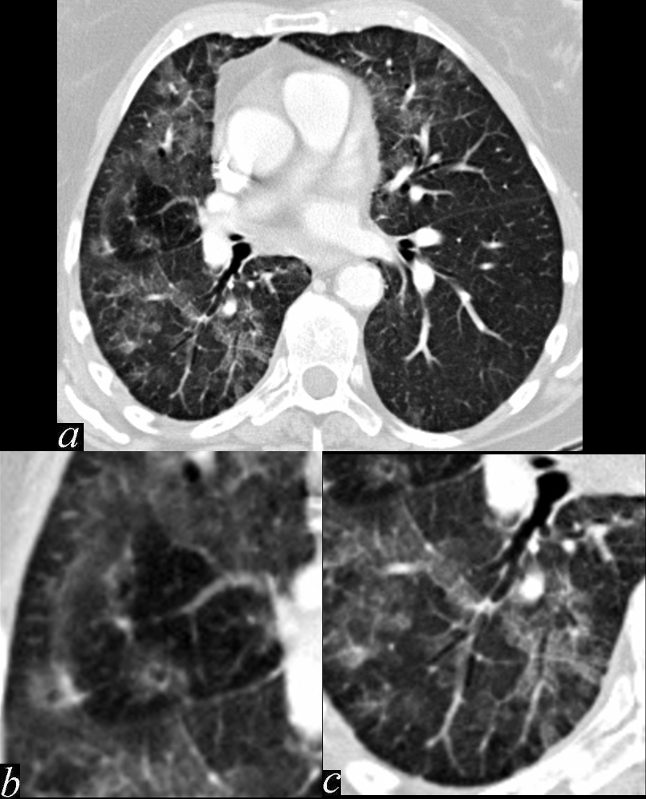
This series of images shows some subtle changes that reflect the local control of blood flow to a small segment of the right middle lobe. Note that in image a, there is a small area of increased lucency (blacker) in the right lung just lateral to the vessels of the right hilum. This region is highlighted in b. Note also that in b, the rapid diminution of the size of the blood vessel to that subsegment when compared to the size change of the vessels in the image in c. The lucent appearance of the lung suggests air trapping and the vasoconstriction reflects decreased perfusion – ie with decreased ventilation there is an associated consequent associated decrease in perfusion.
Keywords # broncho-centric inflammation lung bronchovascular bundle chest inflammation peribronchial halo air trapping mosaic perfusion ground glass changes alveolar change air bronchogram acute bronchovascular inflammation ddx allergic collagen vascular disease infection CTscan
Ashley Davidoff MD TheCommonVein.net 47170c01.800
