Structure
- lower lobe predominance
- infiltration of lymphocytes and plasma cells into the
- perilymphatic
- bronchovascular bundles
- venules
- interstitium.
- perilymphatic
| CT Finding | Description |
|---|---|
| Cysts and Nodules: | Development of cysts and nodules varying in size and distribution.
hypotheses perhaps bronchiolar obstruction similar to the pathogenesis of Langerhans cysts but many other hypotheses |
| Peribronchovascular and Perilymphatic Distribution: | Clustering of lymphocytic infiltrates around bronchovascular bundles and lymphatic vessels. |
| Interstitial Thickening: | Thickening of interlobular septa and bronchovascular bundles contributing to a reticular pattern. |
| Ground-Glass Centrilobular Nodules: | Centrilobular ground-glass nodules may be present. |
| CT Finding | Description |
|---|---|
| Ground-Glass Opacities (GGOs): | Bilateral and diffuse opacities indicating partial airspace filling. |
| Interstitial Thickening: | Thickening of interlobular septa and bronchovascular bundles contributing to a reticular pattern. |
| Cysts and Nodules: | Development of cysts and nodules varying in size and distribution. |
| Ground-Glass Centrilobular Nodules: | Centrilobular ground-glass nodules may be present. |
| Pleural Effusion: | Pleural effusion is not common but mild effusion may be observed in some cases. |
Rare
- Typical onset at ages 40 – 70 years old but can occur at any age (Chest 2002;122:2150)
- Typically in patients with Sjogren’s syndrome
- lower lobe predominance
- GGO’s
- Can have MALT lymphoma
- and Amyloidosis Light chain deposition disease
- More common in women
- No association with smoking history
- Bilateral lower lobes of the lung

Lower Lobe distribution
Ashley Davidoff MD TheCommonvein.net lungs-0771
Lower Lobes Why?
- exact reason for this preference is
- not completely understood,
- One possible explanation
- lower lobes of the lungs are
- more dependent on gravity, which
- may affect the distribution of
- lymphocytes and
- other immune cells that are involved in the development of LIP.
- Gravity may cause these cells to accumulate more easily in the lower lobes, where
- blood flow and ventilation are also generally
- lower
- compared to the upper lobes.
- lymphatic drainage of the lower lobes
- less than the upper lobes, which could lead to the
- accumulation of lymphocytes in the lower lobes.
- certain infections or environmental exposures that may
- contribute to the development of LIP
- may also have a greater impact on the lower lobes of the lungs.
Disease Process
- infiltration of lymphocytes and plasma cells into the lung interstitium
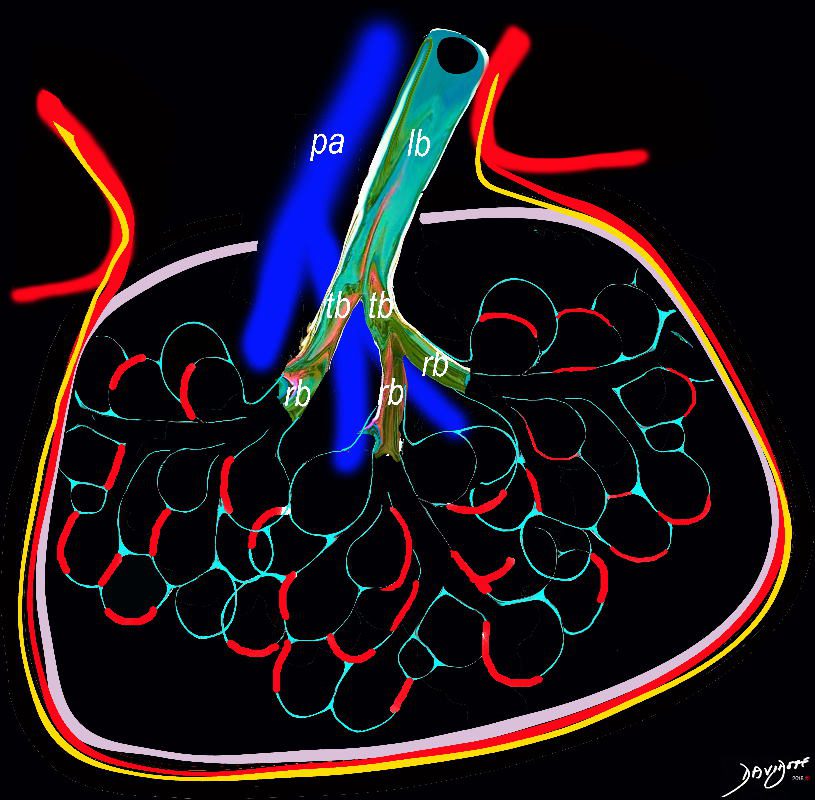
Ashley Davidoff TheCommonVein.net lungs-0736a01
- Pathogenic mechanisms of LIP are still unclear
- Has aspects of lymphoproliferative disease and lymphoid hyperplasia of polyclonal T or B cells (Chest 2002;122:2150)
- Although it may transform to lymphoma, especially MALT, the risk is lower than initially reported (Eur Respir J 2006;28:364)
- Associated with several systemic diseases and conditions
- Autoimmune (most common)
- Sjögren syndrome (SjS); 25% of LIP cases have SjS and 1% of SjS cases present with LIP
- Rheumatoid arthritis
- Systemic lupus erythematosus
- Polymyositis / dermatomyositis
- Hashimoto disease
- Hypothyroidism
- Castleman disease
- Myasthenia gravis
- Autoimmune hemolytic anemia
- Pernicious anemia
- Primary biliary cirrhosis
- Infection
- Human immunodeficiency virus (HIV)
- Epstein-Barr virus
- Human T cell lymphotropic virus type 1
- Legionella pneumonia
- Mycoplasma
- Chlamydia
- Tuberculosis
- Immunodeficiency
- Acquired immunodeficiency syndrome (AIDS); especially in children
- Monoclonal or polyclonal gammopathy
- Common variable immunodeficiency
- Idiopathic LIP accounts for 20% of cases (Eur Respir J 2006;28:364)
- Autoimmune (most common)
- Very slowly progressive respiratory symptoms
- Dyspnea on exertion
- Dry cough
- Systemic symptoms such as malaise, fever and weight loss
- Duration of the symptoms prior to diagnosis can exceed a year
- Bibasilar inspiratory crackles on chest auscultation
- Based on clinical, radiological and pathological findings (multidisciplinary diagnosis)
- No firm diagnostic criteria currently exist
- Dysproteinemia is often present
- Hypergammaglobulinemia is more common than hypogammaglobulinemia
- Restrictive pattern on pulmonary function tests
- Reduced forced vital capacity (FVC)
- Reduced diffusing capacity of the lung for carbon monoxide (DLCO)
- Chest radiography
- Bibasilar opacities with lower lobe predominance
- High resolution computed tomography (Eur J Radiol 2015;84:542, Respirology 2016;21:600)
- Ground glass opacity with / without consolidation with lower lobe predominance
- Cyst formation and thickening of bronchovascular bundle and interlobular septa are often present
- Cysts often remain even after resolution of symptoms
27 year old female with congenital HIV/AIDS and B cell Lymphoma
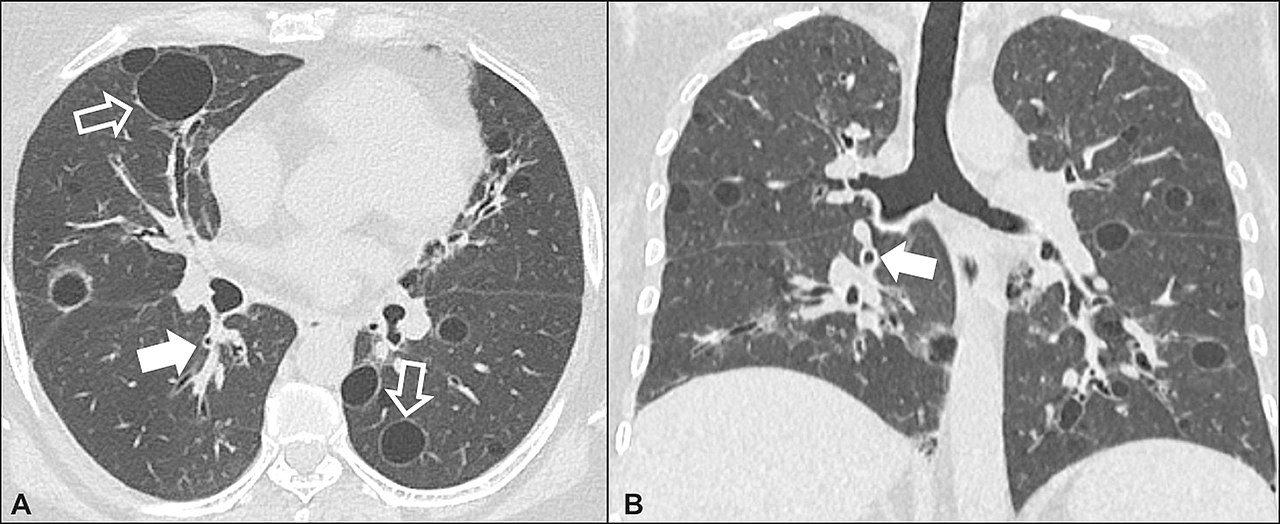
Lymphocytic interstitial pneumonia. A 62-year-old female patient with Sjögren’s syndrome. Axial high-resolution computed tomography scan of the chest (A) and coronal reformatting (B). In A, diffuse thickening of the bronchial walls (closed arrows), some ground-glass opacities and thin-walled cysts of varying sizes, with a diffuse, bilateral distribution (open arrows). In B, distribution predominantly in the lower fields.
Daniel Simões Oliveira et al
Radiologia Brasileira 51 (5): 321–327.
References and Links
Radiopaedia
Yoshikawa A, et al . Pathology Outlines.com
- TCV
-
- Usual interstitial pneumonia (UIP)
- Nonspecific interstitial pneumonia (NSIP)
- Cryptogenic organizing pneumonia (COP)
- Desquamative interstitial pneumonia (DIP)
- Respiratory bronchiolitis-interstitial lung disease (RB-ILD)
- Acute interstitial pneumonia (AIP)
- Lymphoid interstitial pneumonia (LIP)
- Idiopathic pleuroparenchymal fibroelastosis (PPFE)


