2-3mms
random
centrilobular- do not touch the pleural surfaces
discrete solid
infection
aspiration
silicosis
Langerhans Cell Histiocytosis
ground glass
hypersensitivity pneumonitis
bronchiolitis
respiratory
infection (viral)
adenocarcinoma (BAC)
organizing pneumonia/NSIP
vasculitis
edema
tree in bud
TB
Atypical TB
virus
bacterial
aspiration
perilymphatic
along the bronchovascular bundle
along interlobular septa
pleural surface
fissural surface
Cause most commonly sarcoidosis
lymphangitic disease
When perilymphatic is clustered highly suspicious of sarcoidosis otherwise perilymphatic dd is silicosis
Random distribution
-
- random nodules in the vascular distribution and lymphatic
- lower lobes (that is where blood flow goes)
- solid
- well defined
- +/- feeding vessel sign
- +/- cavitation
- +/- lymphangitic appearance
- Causes
- Metastases
- renal
- melanoma
- thyroid
- testicular
- Miliary
- TB
- Fungal
-
- coccidiomycoses
- histoplasmosis
- pneumocytis
- Viral
-
- Metastases
Histoplasmosis
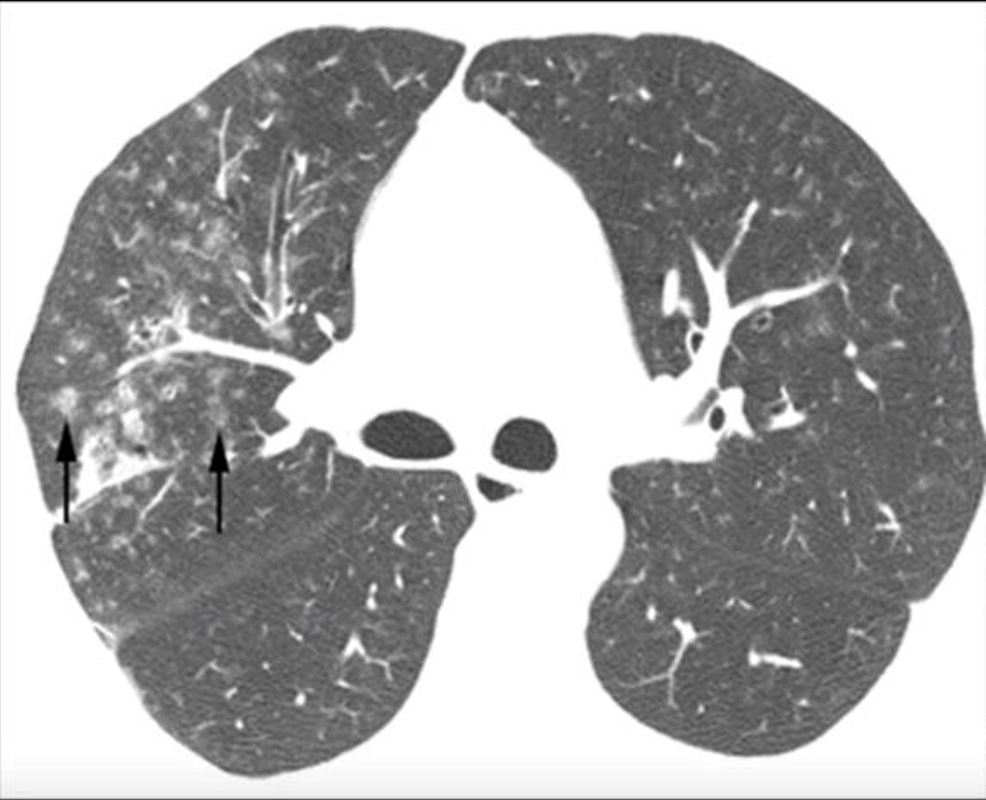
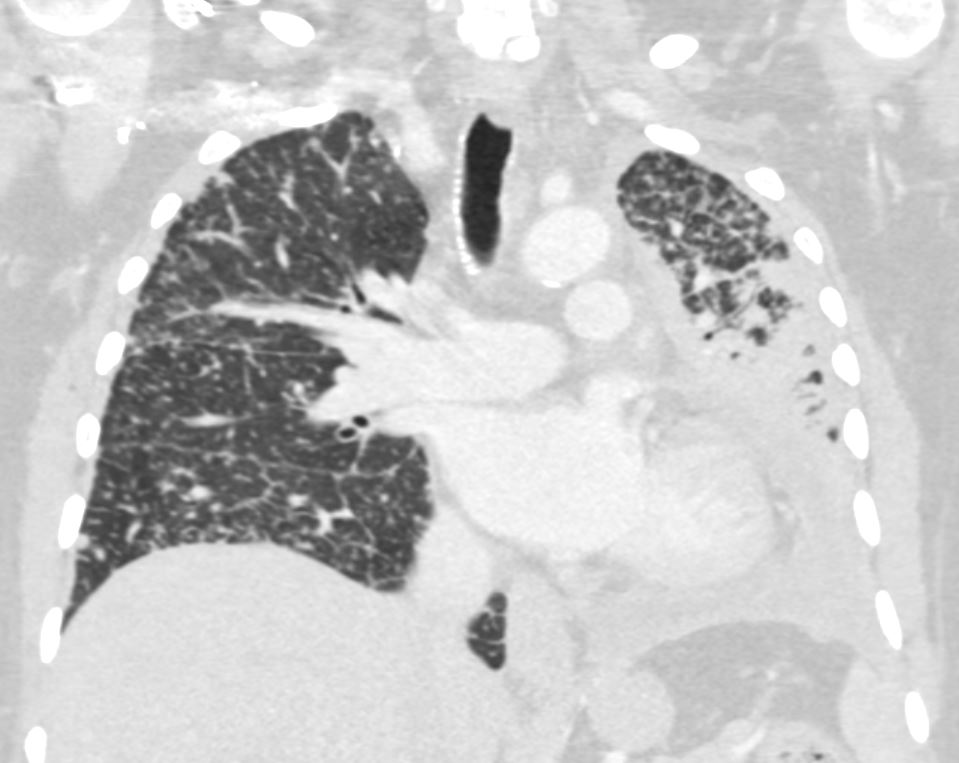
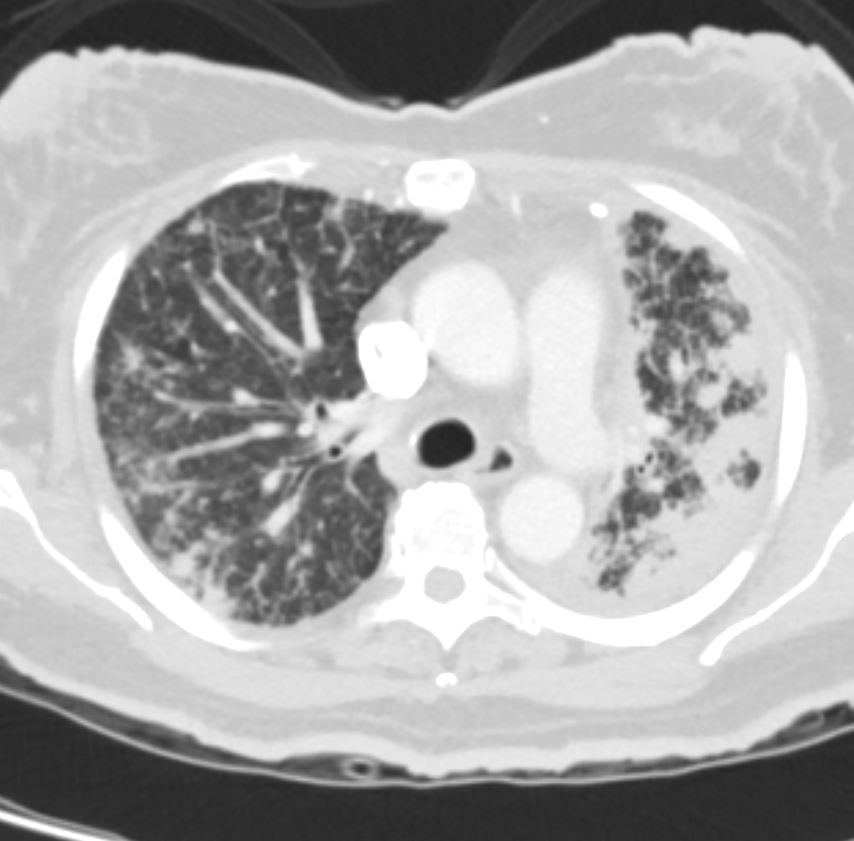
22-year-old female presents with flu like symptoms and has a normal CXR
3 weeks later a chest CT shows extensive diffuse bilateral micronodular military disease associated with mediastinal lymphadenopathy, and hepatosplenomegaly.
A week later she was admitted to the ICU with confluent pneumonic infiltrates with air bronchograms in the lower lobes.
Later that month her CXR started to improve but still showed military disease.
A CXR 9 months later shows resolution.
Ashley Davidoff MD
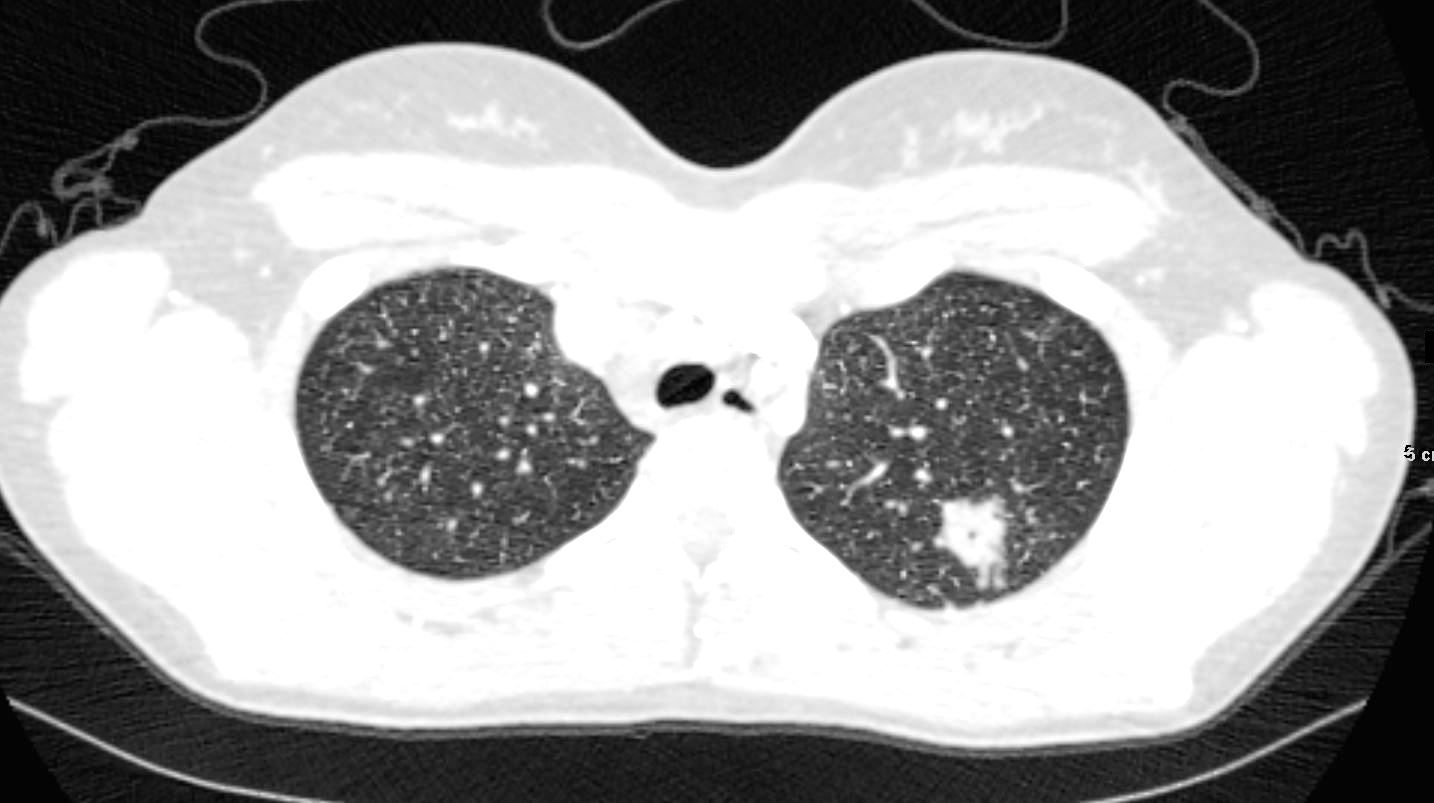
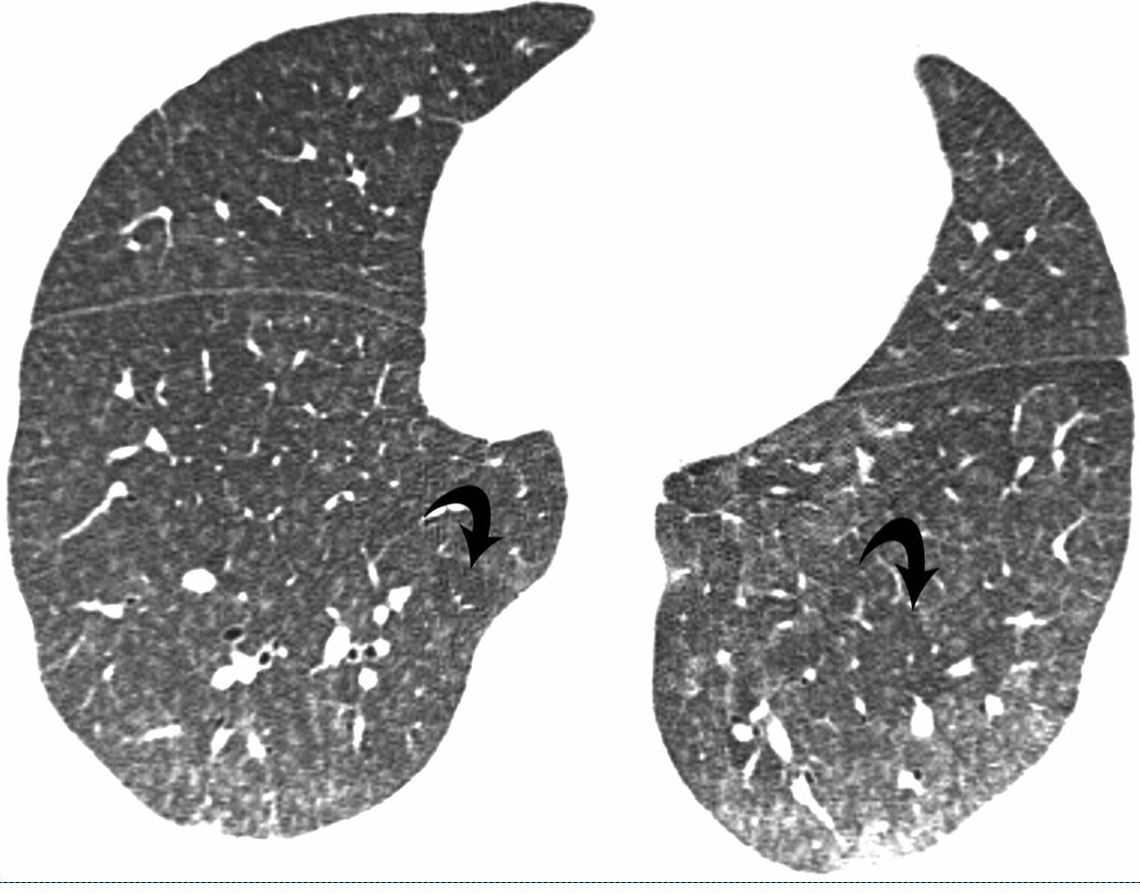
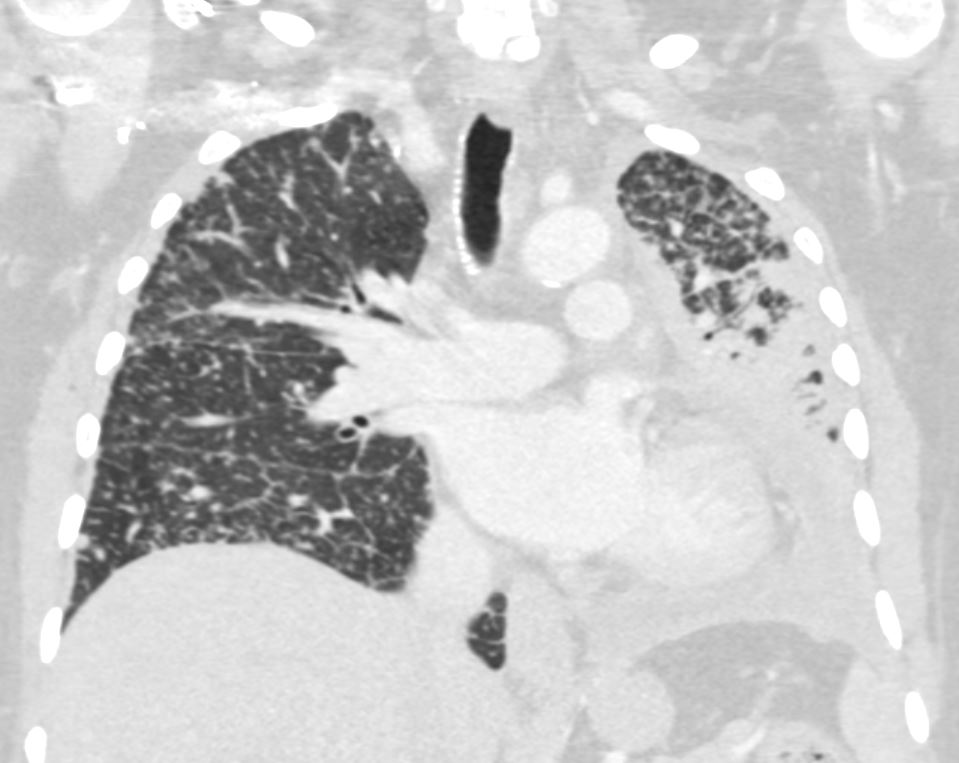
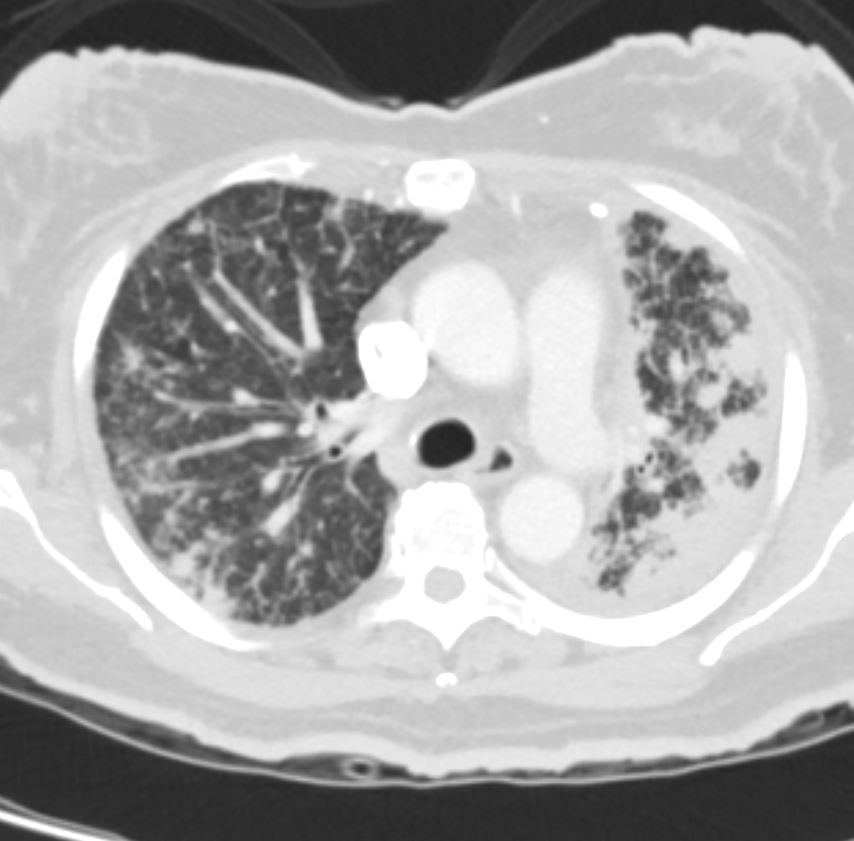
22-year-old female presents with flu like symptoms and has a normal CXR
3 weeks later a chest CT shows extensive diffuse bilateral micronodular military disease associated with mediastinal lymphadenopathy, and hepatosplenomegaly.
A week later she was admitted to the ICU with confluent pneumonic infiltrates with air bronchograms in the lower lobes.
Later that month her CXR started to improve but still showed military disease.
A CXR 9 months later shows resolution.
Ashley Davidoff MD
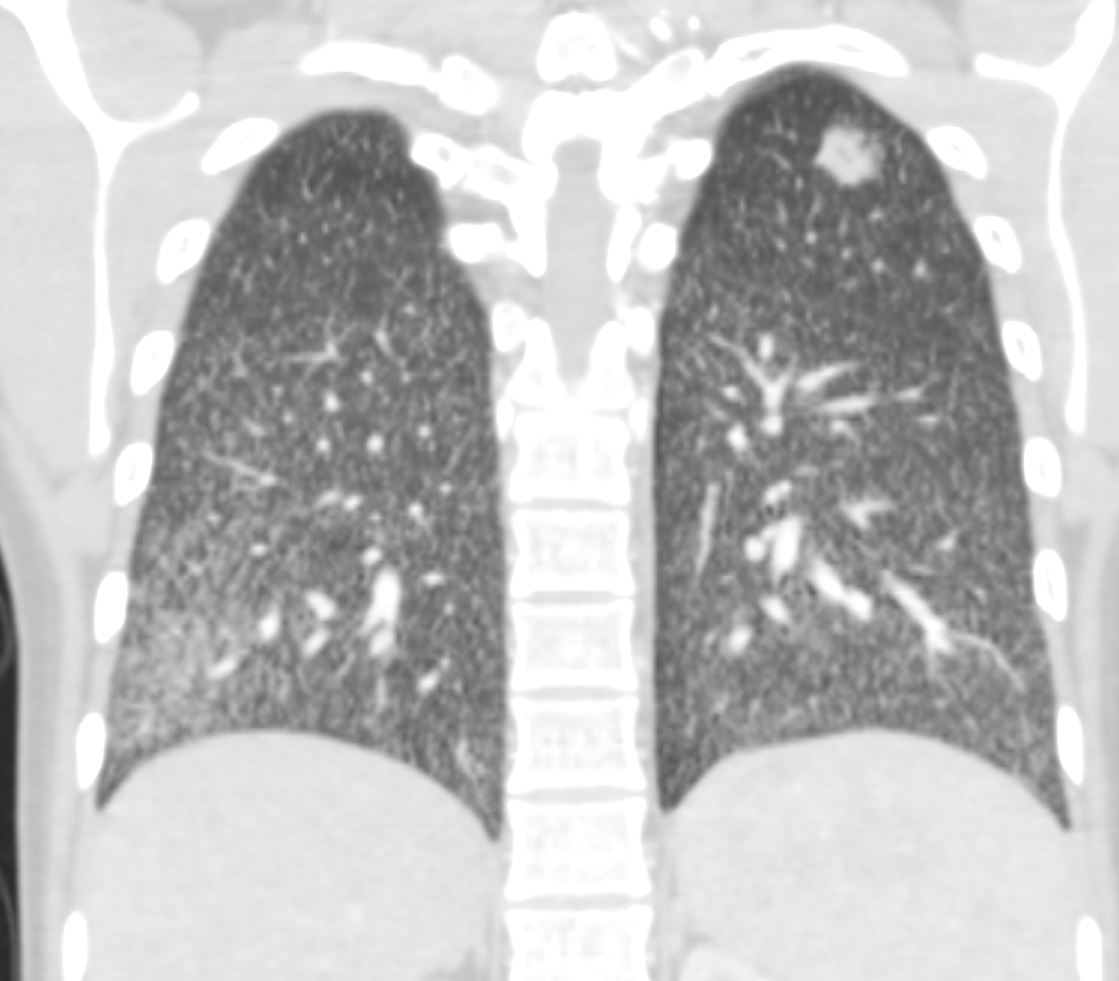
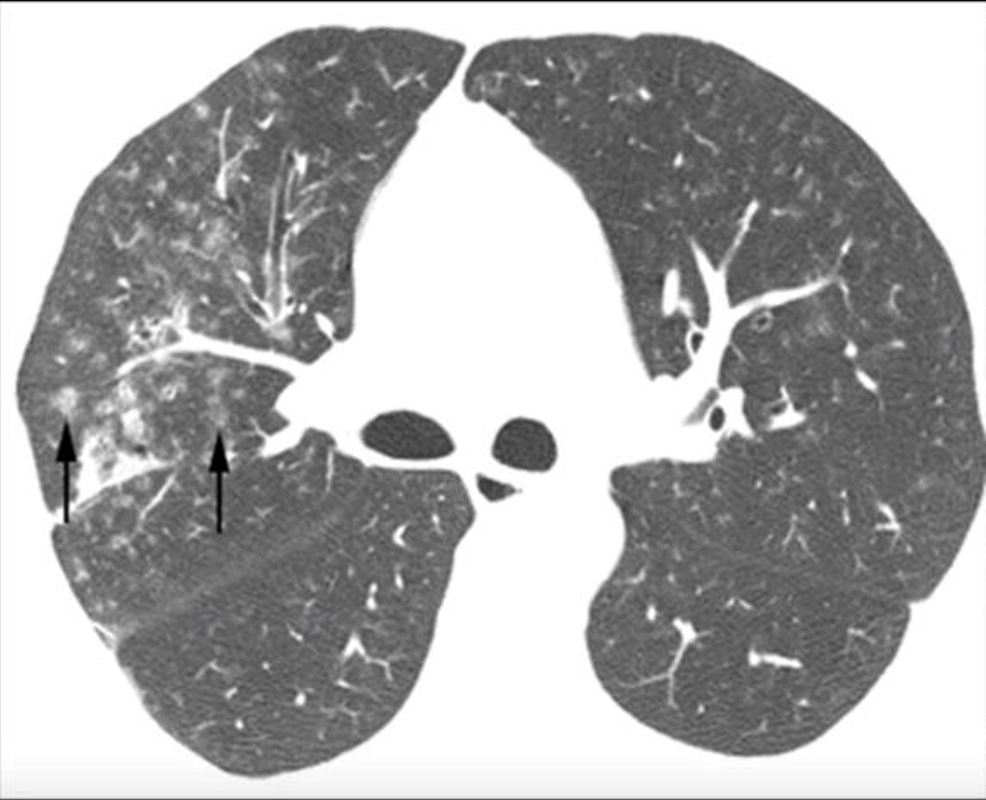
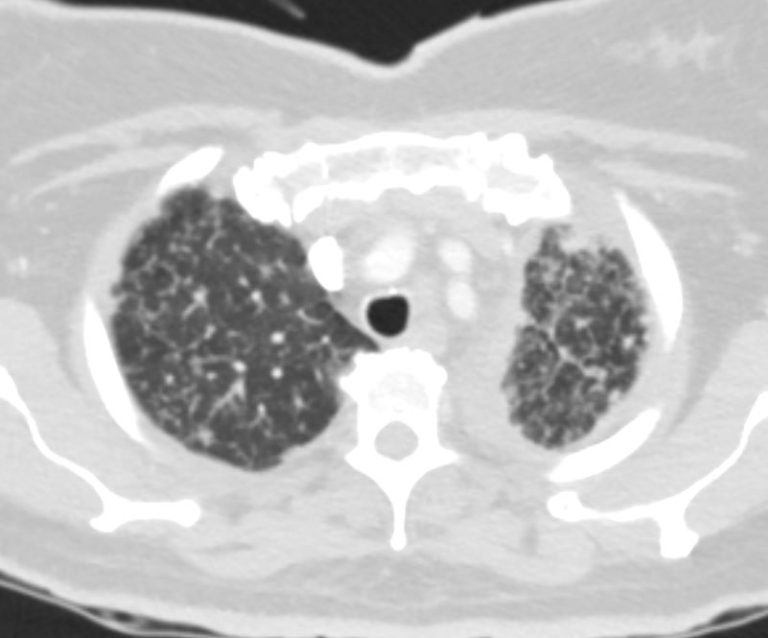
22-year-old female presents with flu like symptoms and has a normal CXR
3 weeks later a chest CT shows extensive diffuse bilateral micronodular military disease associated with mediastinal lymphadenopathy, and hepatosplenomegaly.
A week later she was admitted to the ICU with confluent pneumonic infiltrates with air bronchograms in the lower lobes.
Later that month her CXR started to improve but still showed military disease.
A CXR 9 months later shows resolution.
Ashley Davidoff MD
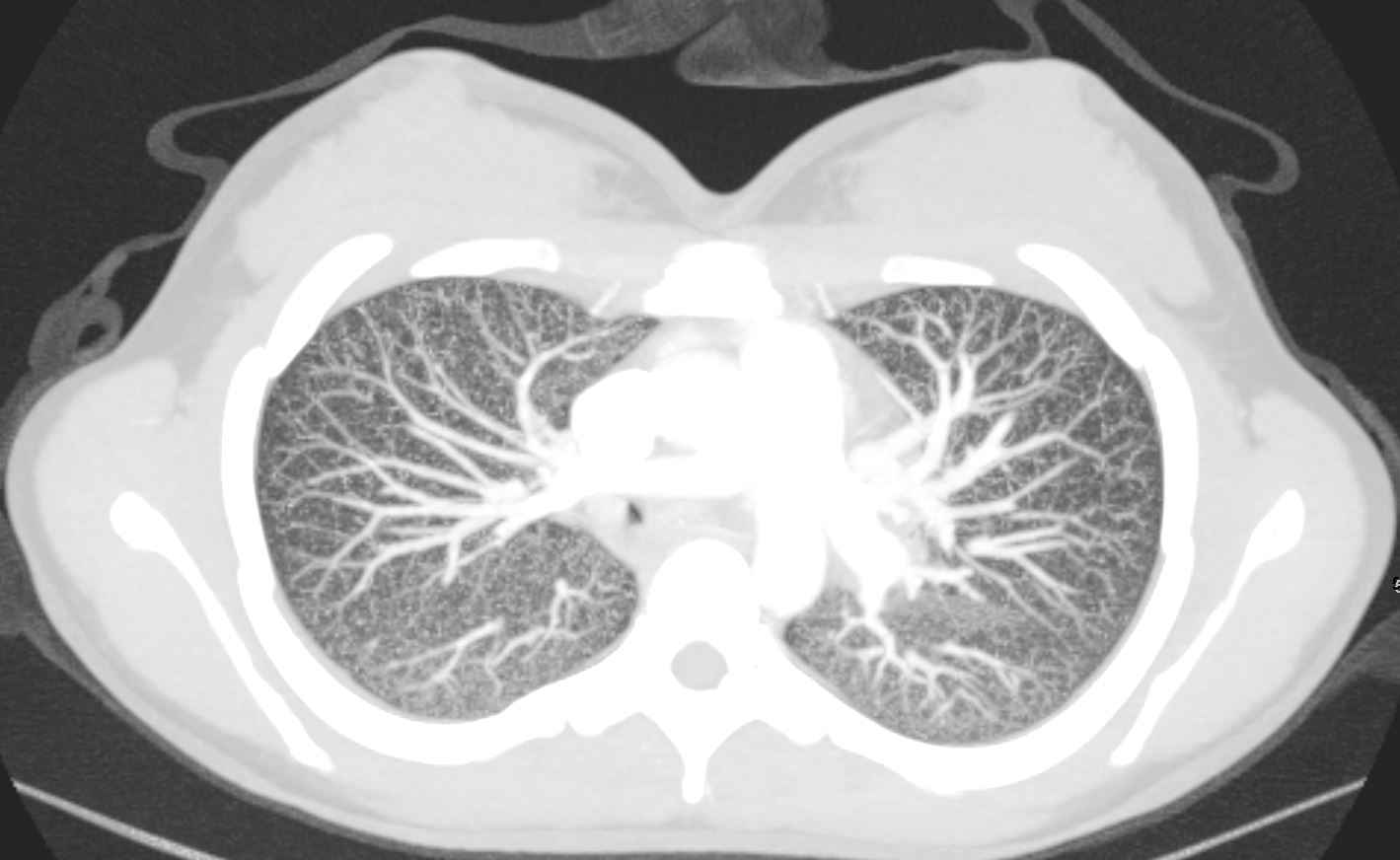
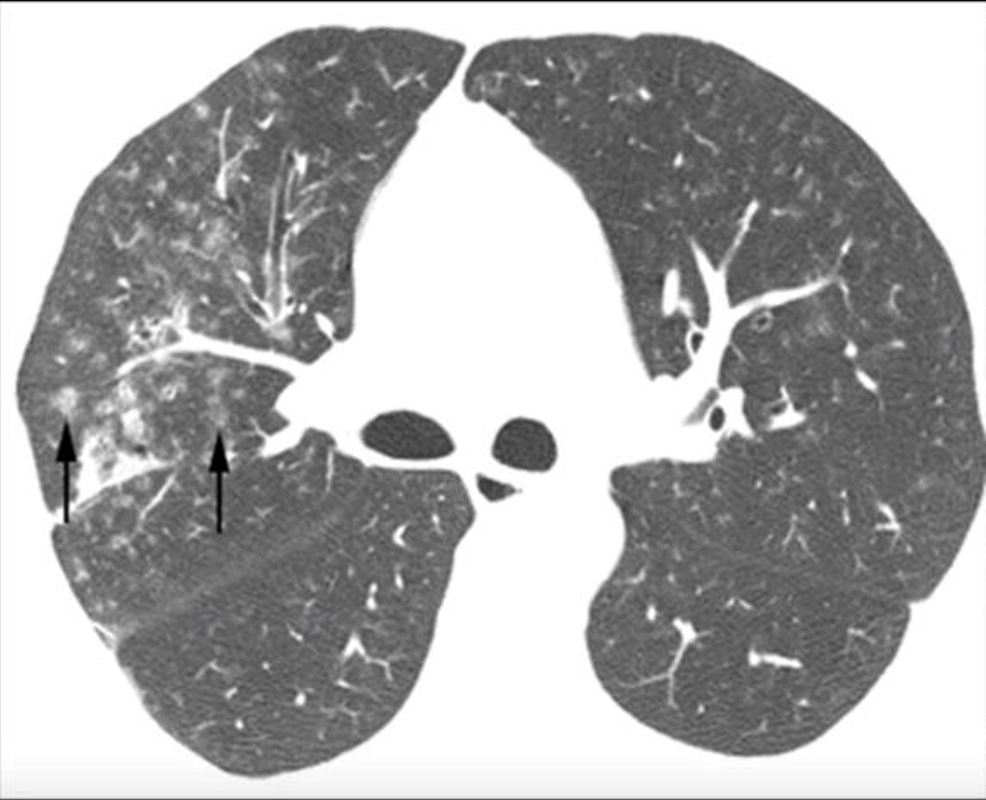
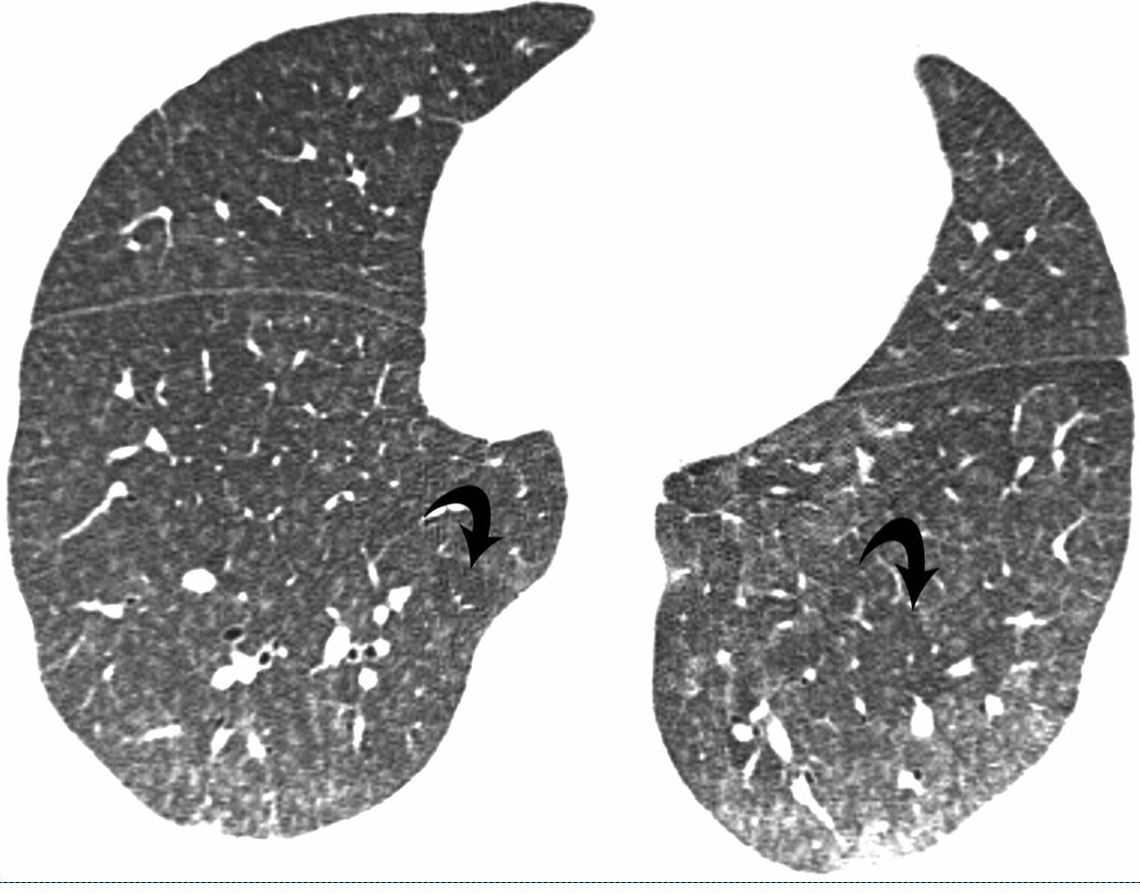
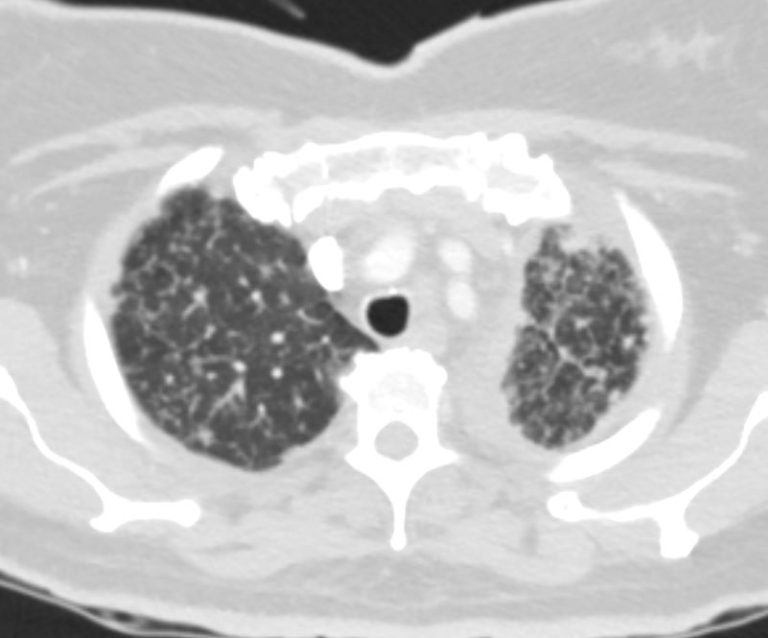
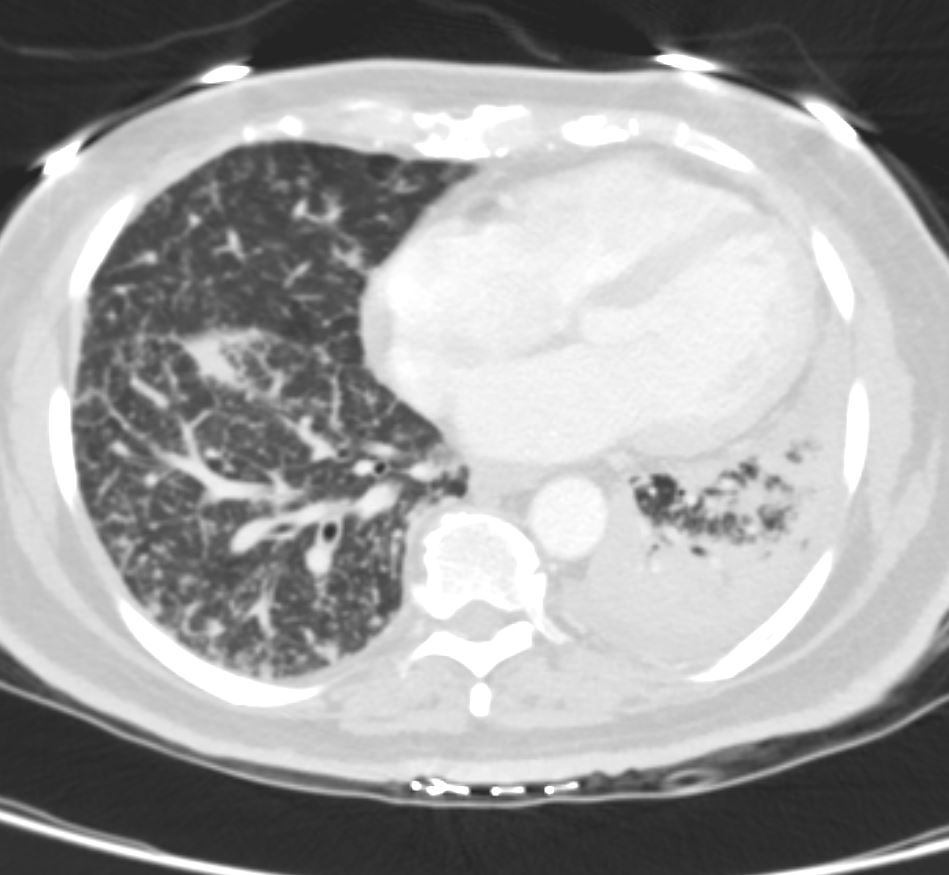
22-year-old female presents with flu like symptoms and has a normal CXR
3 weeks later a chest CT shows extensive diffuse bilateral micronodular military disease associated with mediastinal lymphadenopathy, and hepatosplenomegaly.
A week later she was admitted to the ICU with confluent pneumonic infiltrates with air bronchograms in the lower lobes.
Later that month her CXR started to improve but still showed military disease.
A CXR 9 months later shows resolution.
Ashley Davidoff MD

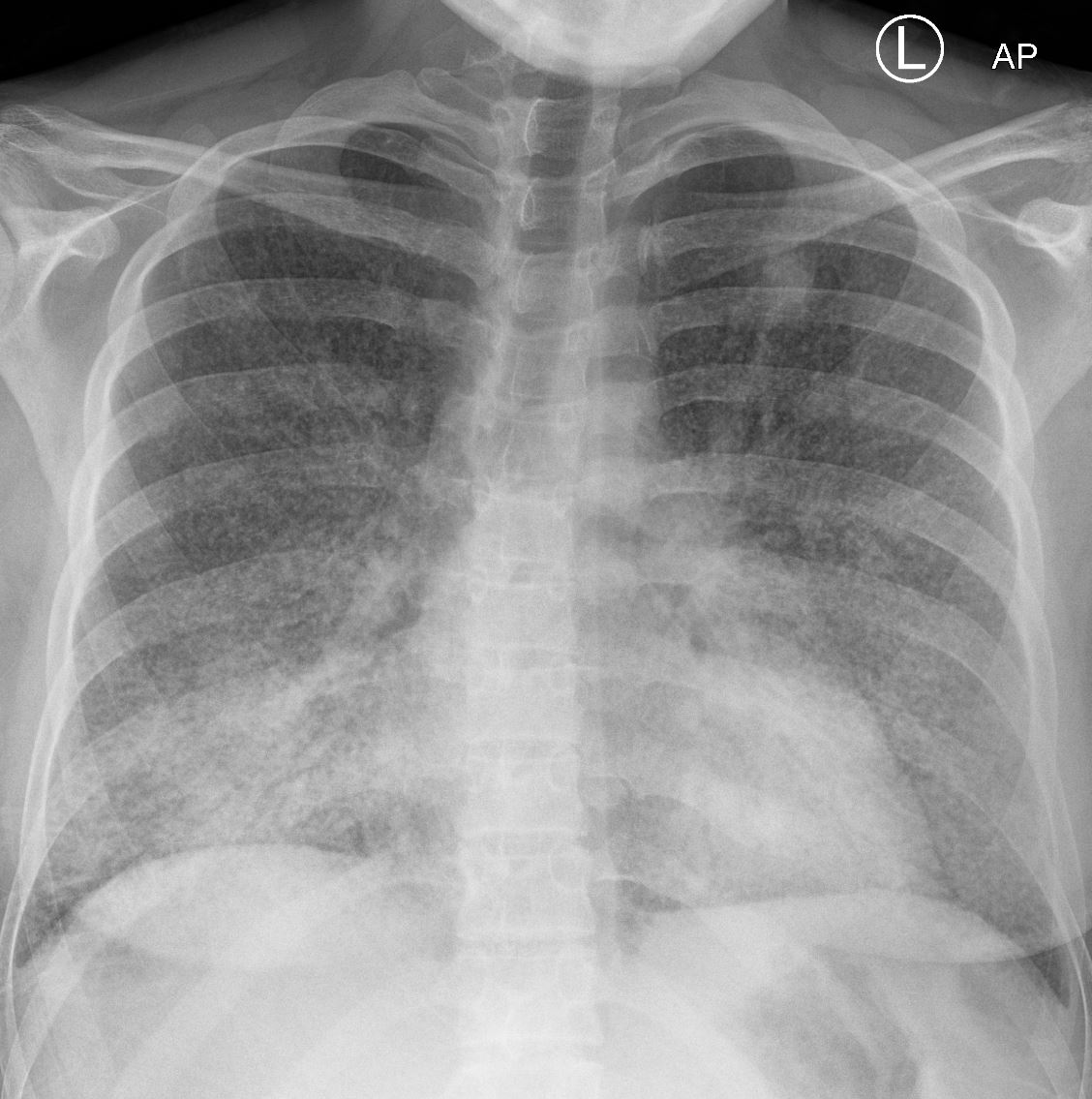
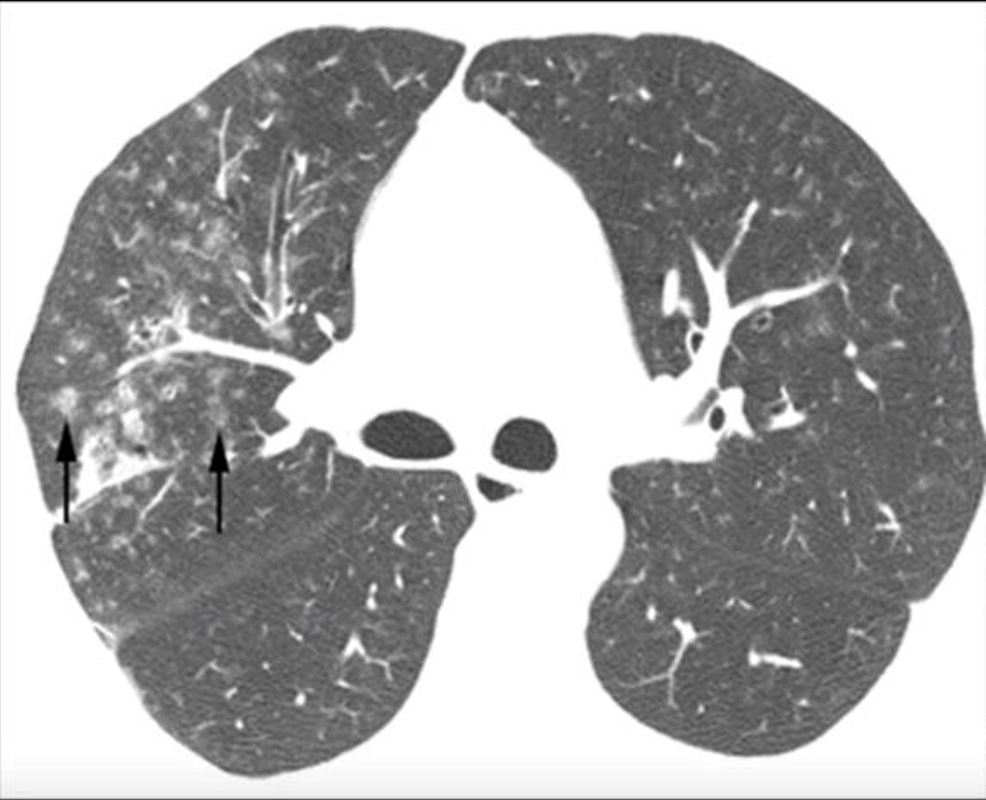
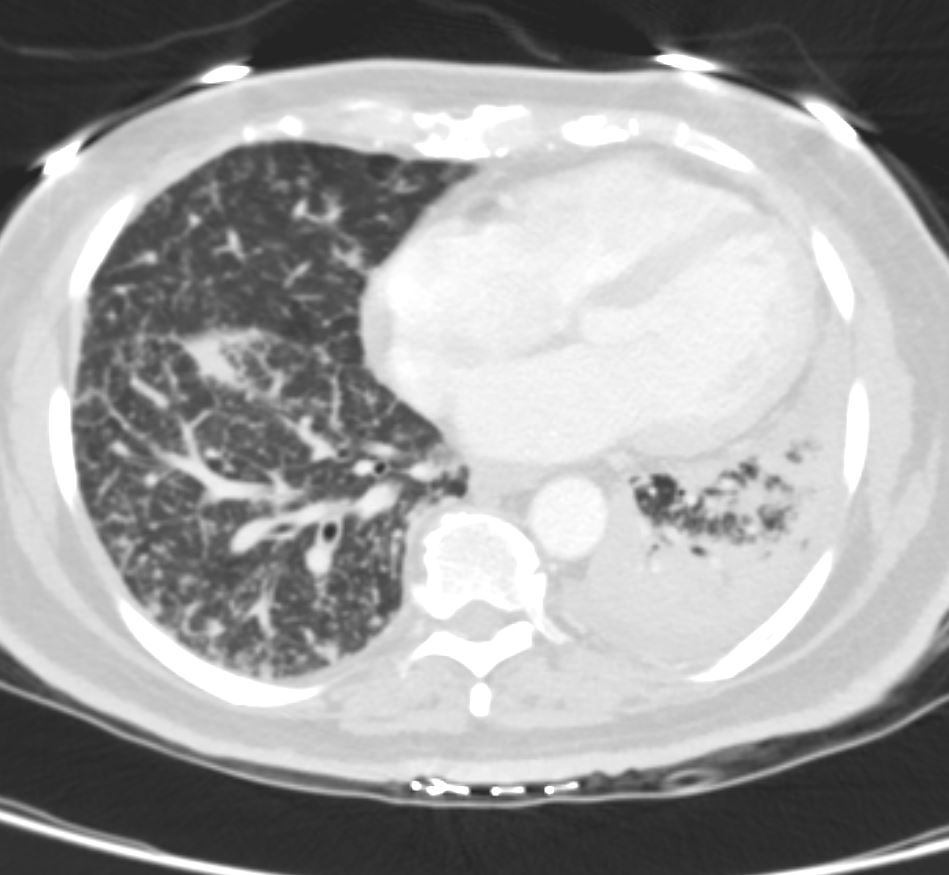
22-year-old female presents with flu like symptoms and has a normal CXR
3 weeks later a chest CT shows extensive diffuse bilateral micronodular military disease associated with mediastinal lymphadenopathy, and hepatosplenomegaly.
A week later she was admitted to the ICU with confluent pneumonic infiltrates with air bronchograms in the lower lobes.
Later that month her CXR started to improve but still showed military disease.
A CXR 9 months later shows resolution.
Ashley Davidoff MD

22-year-old female presents with flu like symptoms and has a normal CXR
3 weeks later a chest CT shows extensive diffuse bilateral micronodular military disease associated with mediastinal lymphadenopathy, and hepatosplenomegaly.
A week later she was admitted to the ICU with confluent pneumonic infiltrates with air bronchograms in the lower lobes.
Later that month her CXR started to improve but still showed military disease.
A CXR 9 months later shows resolution.
Ashley Davidoff MD
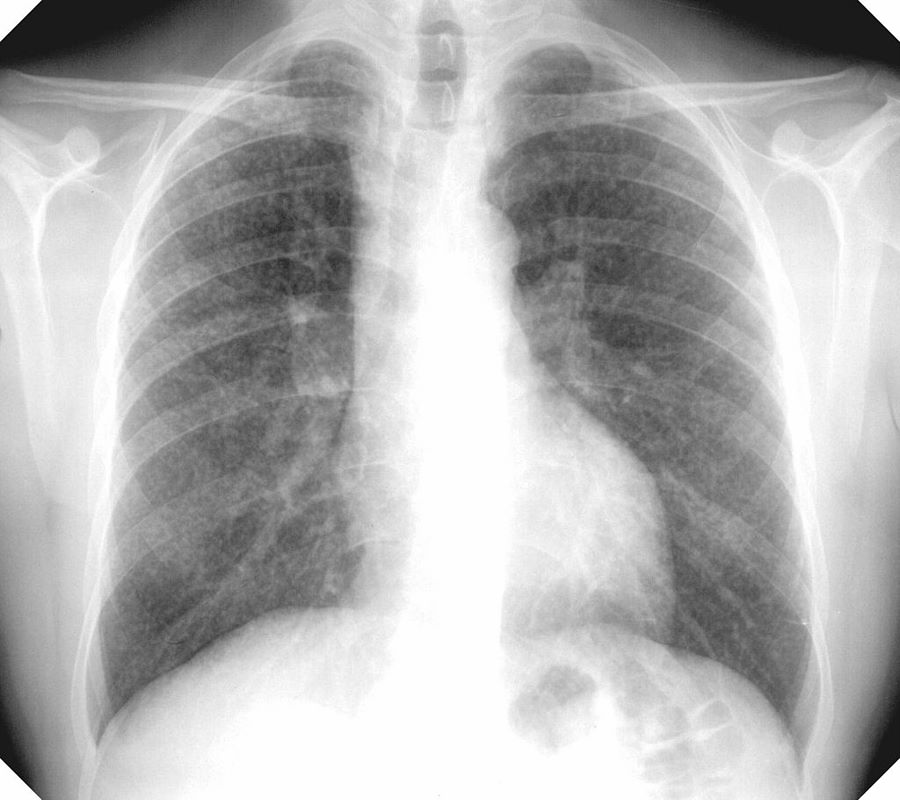
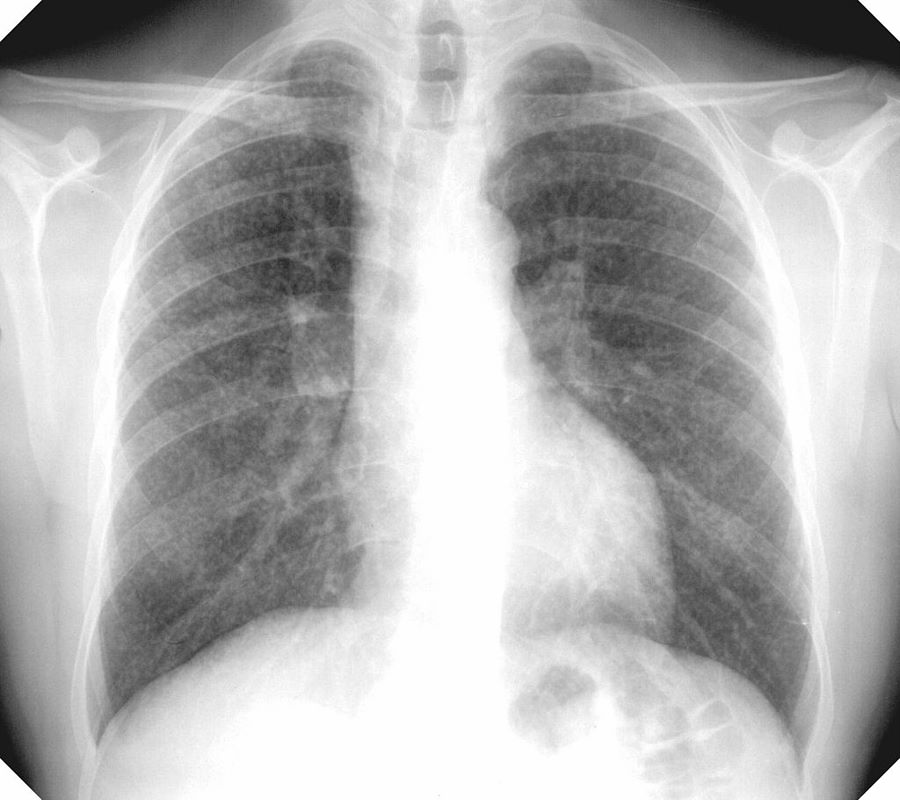
MICRONODULES IN ILD

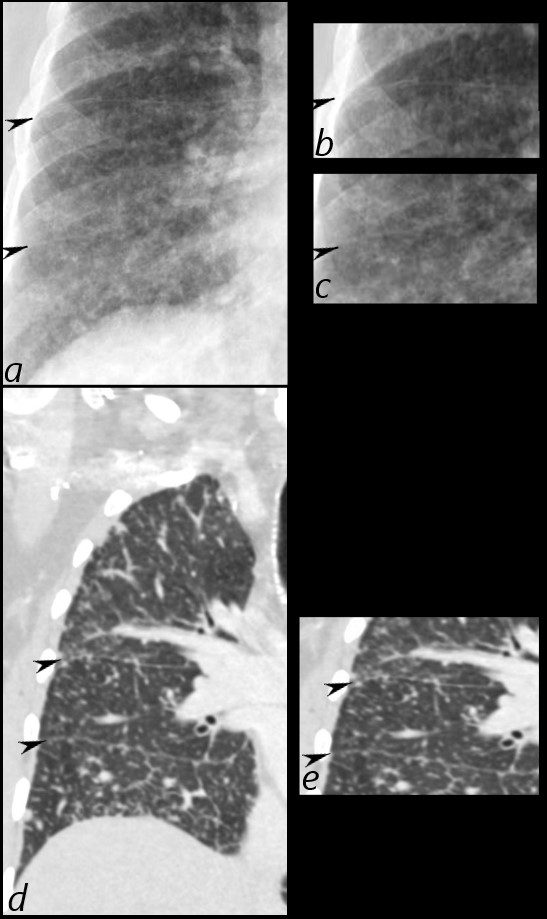
Frontal view exemplifies a diffuse nodular pattern of ILD such as is seen in silicosis and sarcoidosis
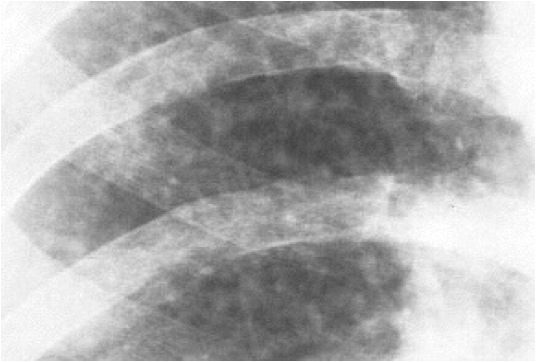
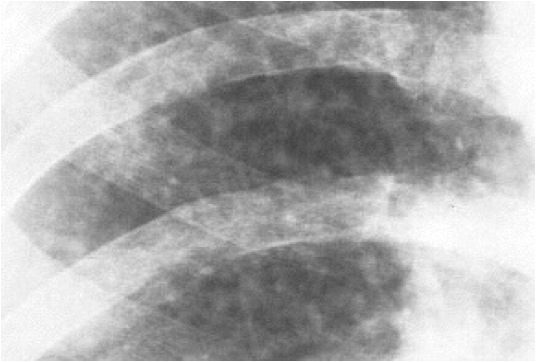
Micronodules in ILD is another feature of interstitial lung disease and is characterised by nodules of a variety of shapes and sizes and likely centrilobular in origin. Sometimes they are ill defined such as in this case.
Micronodules in ILD is another CT feature of interstitial lung disease and is characterised by nodules of a variety of shapes and sizes and likely centrilobular in origin. Sometimes they are ill defined such as in this case.
Silicosis
Chest X-ray showing uncomplicated silicosis
Courtesy Gumersindorego
Courtesy DrSHaber
Silicosis vs Sarcoidosis
42-year-old cement worker presents with dyspnea .
A CXR performed 5 years prior was close to normal with possible right hilar prominence.
The CT scan, shows diffuse micronodular lung disease, predominantly in the upper lobes with mediastinal widening consistent with mediastinal lymphadenopathy, dominant in the right paratracheal region and in the subcarinal region.
Lung windows show the presence of extensive diffuse micronodular disease accumulating along lymphatics along fissures and pleural surfaces, and along the bronchovascular bundles. Although there is diffuse disease, the upper lobes are slightly more involved than the lower lobes. The extensive thickening along bronchovascular bundles and prominent adenopathy favors a diagnosis of sarcoidosis but with a work history of being a cement worker, silicosis still remains in the differential diagnosis as a less likely possibility.


Ashley Davidoff MD


Ashley Davidoff MD


Ashley Davidoff MD
Hypersensitivity Pneumonitis
Bilateral Lymphangitis Carcinomatosis in a Patient with Adenocarcinoma


50 year old female with primary adenocarcinoma of the left lung with diffuse bilateral lymphangitic spread of disease characterized by lymphovascular distribution.
The nodularity on the fissures characterize the lymphatic distribution and the nodules are likely of a mixed nature, some being in the interlobular septa, and some in a centrilobular distribution .
Ashley Davidoff MD
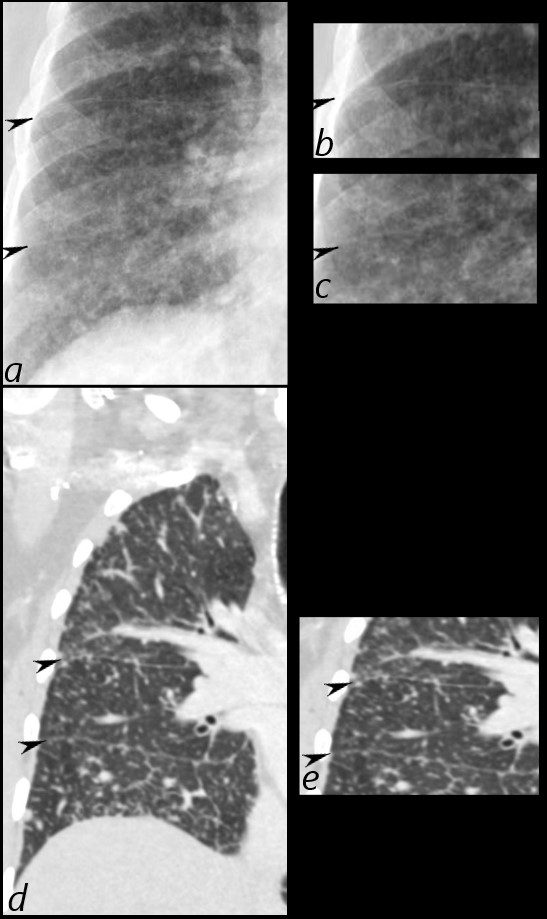
50 year old female with primary adenocarcinoma of the left lung with diffuse bilateral lymphangitic spread of disease characterized by lymphovascular distribution.
The nodularity on the fissures characterize the lymphatic distribution and the nodules are likely of a mixed nature, some being in the interlobular septa, and some in a centrilobular distribution .
Ashley Davidoff MD








References and Links
Videos
See around 25minutes
