1) upper, middle, lower lung distribution;
2) peripheral or central; and
3) distributions in relation to a secondary pulmonary lobule (i.e., lymphatic, centrilobular, and random).
Top and Bottom Disease
Upper Lung Zones
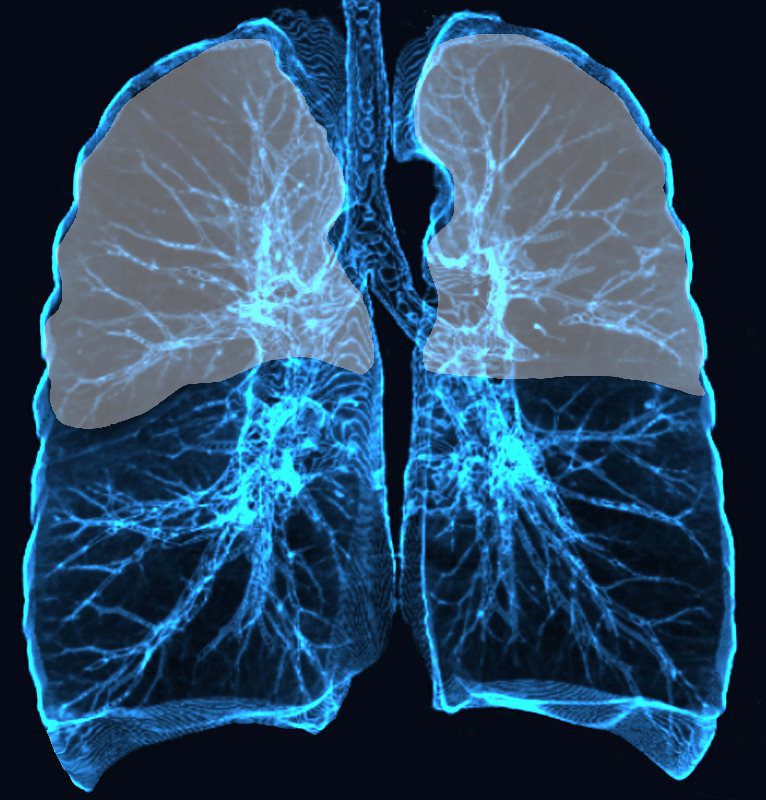
Upper and mid lung field distribution
Ashley Davidoff MD TheCommonvein.net lungs-0772
-
-
- TB
- Tuberculosis (TB) is an infectious disease caused by the bacterium Mycobacterium tuberculosis, and it is known to primarily affect the upper lobes of the lungs. There are several reasons why this may be the case:
- Differences in lung physiology: The upper lobes of the lungs have a greater blood supply and a higher oxygen concentration than the lower lobes. These factors may make the upper lobes more favorable for the growth and replication of M. tuberculosis.
- Gravity: When a person is standing or sitting upright, the upper lobes of the lungs are more exposed to inhaled air, making them more susceptible to the initial infection with M. tuberculosis.
- Immune response: The immune response to TB can also contribute to the preferential localization of the infection in the upper lobes. Macrophages, a type of immune cell that fights TB, are less abundant in the upper lobes than in the lower lobes. This may allow the bacteria to evade the immune system and establish an infection in the upper lobes.
- Tuberculosis (TB) is an infectious disease caused by the bacterium Mycobacterium tuberculosis, and it is known to primarily affect the upper lobes of the lungs. There are several reasons why this may be the case:
- Sarcoidosis,
- One theory suggests that the distribution of sarcoid granulomas in the lungs may be related to the differences in airflow and blood flow between the upper and lower lobes. The upper lobes of the lungs receive a greater amount of airflow and blood supply than the lower lobes, which may make them more susceptible to inflammation and immune-mediated disorders like sarcoidosis.Another theory suggests that the distribution of sarcoidosis in the lungs may be related to the location of the lymphatic tissue that is involved in the immune response. The lymphatic tissue is more abundant in the upper lobes of the lungs, particularly in the hilar region, which may explain why sarcoidosis granulomas are often found in this area.
- Hypersensitivity pneumonitis,
- One theory suggests that the distribution of HP in the lungs may be related to the deposition of inhaled allergens. When a person inhales an allergen, it is deposited in the small airways and alveoli of the lungs. The upper lobes of the lungs have a greater number of small airways and alveoli, which may make them more susceptible to allergen deposition and subsequent inflammation.
Another theory proposes that the distribution of HP in the lungs may be related to the pattern of airflow within the lungs. The upper lobes of the lungs have a greater airflow than the lower lobes, which may result in a greater exposure to inhaled allergens and subsequent inflammation.
Additionally, the anatomy of the lymphatic drainage in the upper lobes of the lungs may also play a role in the preferential distribution of HP. The lymphatic vessels that drain the upper lobes of the lungs are located near the hilum of the lungs, which is a common site for inflammation and scarring in HP.
Overall, while the exact reason for the preferential distribution of HP in the upper lobes of the lungs is not fully understood, it is likely due to a combination of factors, including allergen deposition, airflow patterns, and lymphatic drainage.
- One theory suggests that the distribution of HP in the lungs may be related to the deposition of inhaled allergens. When a person inhales an allergen, it is deposited in the small airways and alveoli of the lungs. The upper lobes of the lungs have a greater number of small airways and alveoli, which may make them more susceptible to allergen deposition and subsequent inflammation.
- Silicosis
- Deposition of silica particles: When silica particles are inhaled, they tend to deposit in the upper lobes of the lungs due to their larger size and the direction of airflow in the lungs. This deposition leads to the accumulation of silica in the lungs and subsequent inflammation and scarring.
- Greater air volume: The upper lobes of the lungs have a greater air volume than the lower lobes, which can result in a greater exposure to silica particles.
- Greater oxygen tension: The upper lobes of the lungs have a greater oxygen tension than the lower lobes, which can make them more susceptible to the toxic effects of silica particles.
- Langerhans Cell Histiocytosis
- The upper lobes of the lungs have a greater number of small airways and alveoli, which may make them more susceptible to the accumulation of Langerhans cells and subsequent inflammation.
- Airflow patterns: The upper lobes of the lungs have a greater airflow than the lower lobes, which may result in a greater exposure to inhaled agents, such as cigarette smoke or other environmental toxins, which can contribute to the development of LCH.
- Immune response: The immune response to LCH may also contribute to the preferential localization of the disease in the upper lobes of the lungs. The immune cells that fight LCH, such as T-cells, may be more active in the upper lobes of the lungs, which can lead to a greater accumulation of Langerhans cells in these areas.
- Chronic Eosinophillic Pneumonia
-
- Anatomy of the lungs: The upper lobes of the lungs have a greater number of smaller airways and alveoli, which may make them more susceptible to inflammation and eosinophil accumulation.
- Ventilation and perfusion: The upper lobes of the lungs are more highly ventilated and perfused compared to the lower lobes, which may make them more susceptible to the effects of inhaled antigens or allergens.
- Regional lymph nodes: The lymph nodes that drain the upper lobes of the lungs are located near the hilum of the lungs, which is a common site of inflammation and scarring in CEP.
- Immunological factors: The immune response to CEP may also play a role in its preferential involvement in the upper lobes of the lungs, with certain immune cells being more active in these areas.
It is important to note that while CEP often involves the upper lobes of the lungs, it can also affect other areas of the lungs. The exact reason for this distribution is not fully understood and requires further investigation.
-
- TB
-
Lower Lung Fields
Anywhere Disease (Upper and Lower)
- COP
Central and Peripheral Disease
Central or Perihilar Disease
Peripheral Disease
( terminal bronchiole with several acini )
-
Central
- pulmonary edema
- alveolar proteinosis
- sarcoidosis
-
Pleural and Subpleural Disease
-
Extension Along Fissures
- Sarcoidosis
- NSIP
- UIP
-
Secondary Lobule
- Interlobular septal thickening
- CHF
- Sarcoid
- lymphangitis
- Acute eosinophilic pneumonia
- Interlobular septal thickening
Links and References
- Nishino, N et al A Practical Approach to High-Resolution CT of Diffuse Lung Disease Eur J Radiol. 2014 Jan; 83(1): 6–19.
- Covington
