-
-
Etymology: Derived from the Latin word acinus, meaning “berry” or “cluster,” referring to the terminal units of the lung where gas exchange occurs.
AKA:
- Clustered nodules
- Acinar shadows
Abbreviation: AN (Acinar Nodules)
What is it? Acinar nodules are small, round opacities (5–10 mm in diameter) representing filling of the terminal respiratory unit (acini) with fluid, cells, or other material. These nodules result from various infectious, inflammatory, hemorrhagic, or neoplastic processes affecting the alveoli and surrounding airways.
Distinction from Acinar Pattern: Acinar nodules refer to individual small, round opacities representing filling of the terminal respiratory unit, while an acinar pattern describes a broader radiologic pattern involving clusters of these nodules with more diffuse alveolar filling, commonly seen in pneumonia, hemorrhage, or edema.
Caused by:
- Most Common Causes:
- Bacterial pneumonia
- Tuberculosis
- Viral infections
- Diffuse alveolar hemorrhage
- Other Causes:
- Fungal infections (e.g., histoplasmosis, aspergillosis)
- Hypersensitivity pneumonitis
- Sarcoidosis
- Anticoagulation
- Heart failure
- Lymphangitic carcinomatosis
- Most Common Causes:
- Bacterial pneumonia
- Tuberculosis
- Viral infections
- Other Causes:
- Fungal infections (e.g., histoplasmosis, aspergillosis)
- Hypersensitivity pneumonitis
- Sarcoidosis
- Diffuse alveolar hemorrhage
- Anticoagulation
- Heart failure
- Lymphangitic carcinomatosis
- Infectious processes: Bacterial pneumonia, tuberculosis, viral infections, fungal infections (e.g., histoplasmosis, aspergillosis)
- Inflammatory conditions: Hypersensitivity pneumonitis, sarcoidosis
- Hemorrhagic events: Diffuse alveolar hemorrhage, anticoagulation, heart failure
- Neoplastic processes: Lymphangitic carcinomatosis
Resulting in:
- Clustered or lobular distribution of nodules
- Alveolar filling pattern
- Varying opacities depending on the underlying cause
Structural Changes:
- Filling of terminal respiratory units with material (fluid, cells, etc.)
- Loss of air content in affected alveoli
Pathophysiology:
- Infections and inflammation lead to fluid, cells, or pathogens accumulating in the alveoli.
- Hemorrhagic causes involve capillary rupture and blood filling the alveoli.
Pathology:
- Cellular infiltration in alveoli
- Presence of inflammatory exudates or blood
- Variable fibrosis depending on the chronicity
Diagnosis:
- Based on imaging findings combined with clinical history.
- Requires confirmation through imaging and potentially invasive tests for certain cases.
Clinical:
- Symptoms depend on the underlying cause (e.g., fever, hemoptysis, dyspnea).
- Hemorrhagic causes may present with anemia and hemoptysis.
Radiology:
CXR:
- Findings: Poorly defined opacities, often subtle
- Associated Findings: Air bronchograms may be present
CT:
- Parts: Clustered, small nodules (5-10 mm)
- Size: 5-10 mm
- Shape: Round or oval
- Position: Centrilobular or peribronchovascular distribution
- Character: Ground-glass opacity, consolidation, ill-defined nodules
- Associated Findings: Potential confluence of nodules into larger opacities
Other Imaging Modalities:
- HRCT: Preferred for assessing acinar nodules and distribution
- Expiratory CT: May reveal air trapping in inflammatory causes
Pulmonary Function Tests (PFTs):
- Generally normal unless significant parenchymal involvement
Management:
- Further Evaluation:
- High-resolution CT for detailed imaging
- Bronchoscopy with lavage for hemorrhage, infection, or malignancy
- Expiratory CT for air trapping assessment
- Laboratory Workup:
- Autoimmune panel (ANCA, ANA) for vasculitis
- Microbial cultures for infections
- Coagulation profile for hemorrhagic cases
Differential Diagnosis:
- Most Common Causes:
- Bacterial pneumonia
- Tuberculosis
- Viral infections
- Diffuse alveolar hemorrhage
- Other Causes:
- Fungal infections (e.g., histoplasmosis, pneumocystis pneumonia)
- Hypersensitivity pneumonitis
- Sarcoidosis (rare acinar pattern)
- Heart failure
- Anticoagulation
- Lymphangitic carcinomatosis
- Cryptogenic organizing pneumonia (COP)
- Most Common Causes:
- Bacterial pneumonia
- Tuberculosis
- Viral infections
- Other Causes:
- Fungal infections (e.g., histoplasmosis, pneumocystis pneumonia)
- Hypersensitivity pneumonitis
- Sarcoidosis (rare acinar pattern)
- Diffuse alveolar hemorrhage
- Heart failure
- Anticoagulation
- Lymphangitic carcinomatosis
- Cryptogenic organizing pneumonia (COP)
- Infection:
- Bacterial pneumonia
- Tuberculosis
- Fungal infections (e.g., histoplasmosis, pneumocystis pneumonia)
- Viral infections (e.g., influenza, COVID-19)
- Inflammation:
- Hypersensitivity pneumonitis
- Sarcoidosis (rare acinar pattern)
- Hemorrhage:
- Diffuse alveolar hemorrhage
- Heart failure
- Anticoagulation
- Neoplasm:
- Lymphangitic carcinomatosis
- Idiopathic:
- Cryptogenic organizing pneumonia (COP)
Recommendations:
- High-resolution CT for better characterization
- Bronchoscopy and lavage in suspicious cases
- Laboratory workup tailored to suspected etiology
Key Points and Pearls:
- Acinar nodules represent a radiologic pattern, not a diagnosis.
- Hemorrhagic nodules may resolve rapidly, distinguishing them from infectious or neoplastic causes.
- Persistent nodules raise suspicion for malignancy or interstitial lung disease.
- Multidisciplinary evaluation is often necessary for diagnosis and management.
- Distinction from Acinar Pattern: Acinar nodules refer to small, round opacities representing filling of the terminal respiratory unit, whereas an acinar pattern involves clusters of nodules creating a more diffuse alveolar filling, commonly seen in pneumonia, hemorrhage, or edema.
- Acinar nodules represent a radiologic pattern, not a diagnosis.
- Hemorrhagic nodules may resolve rapidly, distinguishing them from infectious or neoplastic causes.
- Persistent nodules raise suspicion for malignancy or interstitial lung disease.
- Multidisciplinary evaluation is often necessary for diagnosis and management.
Feature Acinar Nodule Acinar Shadow Definition Localized, measurable nodule in the acini. Diffuse, ill-defined opacity in the acini. Imaging Modality Primarily described on CT. Historically used on chest X-rays. Appearance Well-defined nodules (5–10 mm). Diffuse, fluffy, or cloud-like opacities. Resolution High resolution allows discrete detection. Lower resolution; cannot resolve individual nodules. Pathological Implications Often specific and focal. More diffuse, suggesting widespread disease.
-
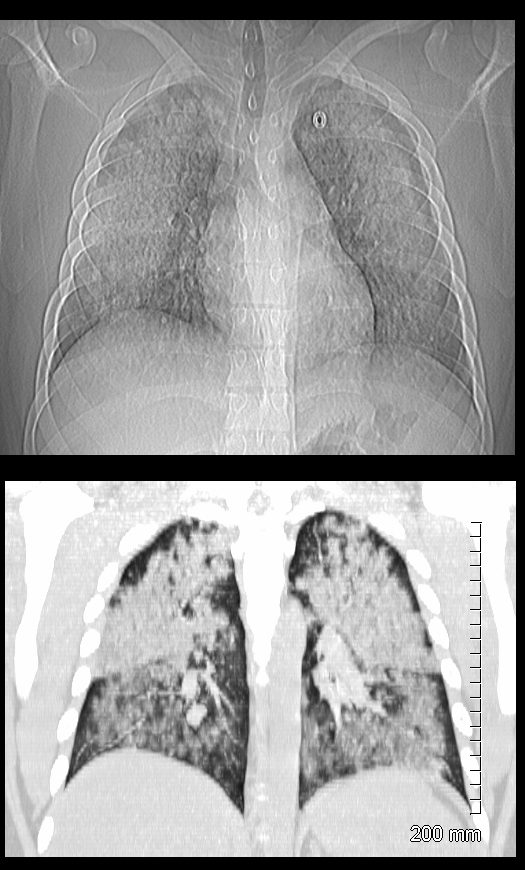
19 year old male previously well with history of hemoptysis, sweating, fevers, myalgias, arthritis over 3 weeks.
CT scan scout (above ) shows diffuse bilateral lobar infiltrates with subpleural sparing
Coronal CT shows bilateral symmetrical lobar nodular consolidations involving the upper and lower lobes. The upper lobes are more consolidative and the lower lobes have an acinar pattern. These finding are consistent with acute pulmonary hemorrhage
Lab shows ANCA positivity, acute renal failure (creatinine 6) and renal biopsy showing crescentic glomerulonephritis. Treated with cyclophosphamide
Ashley Davidoff MD TheCommonVein.net 139195c

19 year old male previously well with history of hemoptysis, sweating, fevers, myalgias, arthritis over 3 weeks.
CT scan in the axial projection shows diffuse bilateral nodular consolidations (acinar pattern) with subpleural sparing consistent with pulmonary hemorrhage
Lab shows ANCA positivity, acute renal failure (creatinine 6) and renal biopsy showing crescentic glomerulonephritis. Treated with cyclophosphamide
Ashley Davidoff MD TheCommonVein.net 139193c
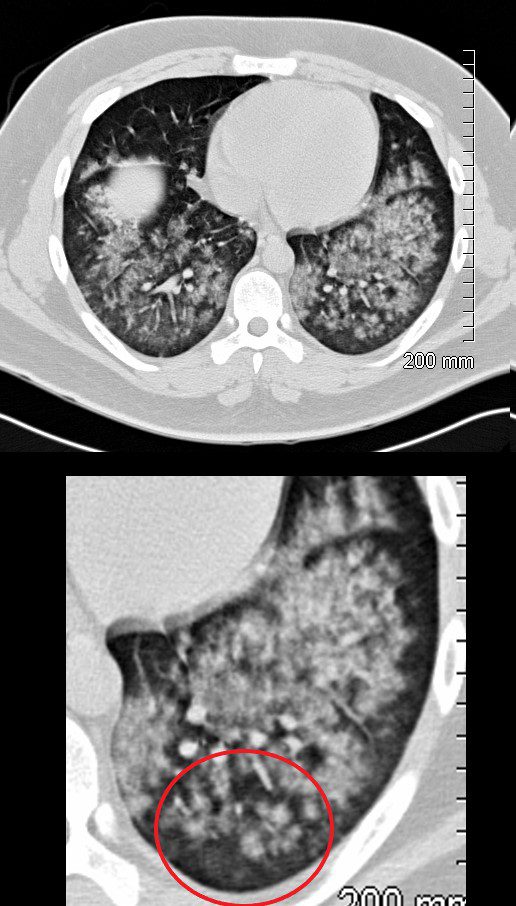
19 year old male previously well with history of hemoptysis, sweating, fevers, myalgias, arthritis over 3 weeks.
CT scan in the axial projection shows diffuse bilateral nodular consolidations (acinar pattern ringed in red) with subpleural sparing consistent with pulmonary hemorrhage
Lab shows ANCA positivity, acute renal failure (creatinine 6) and renal biopsy showing crescentic glomerulonephritis. These finding are consistent with a diagnosis of GPA. He was treated with cyclophosphamide
Ashley Davidoff MD TheCommonVein.net 139193cL
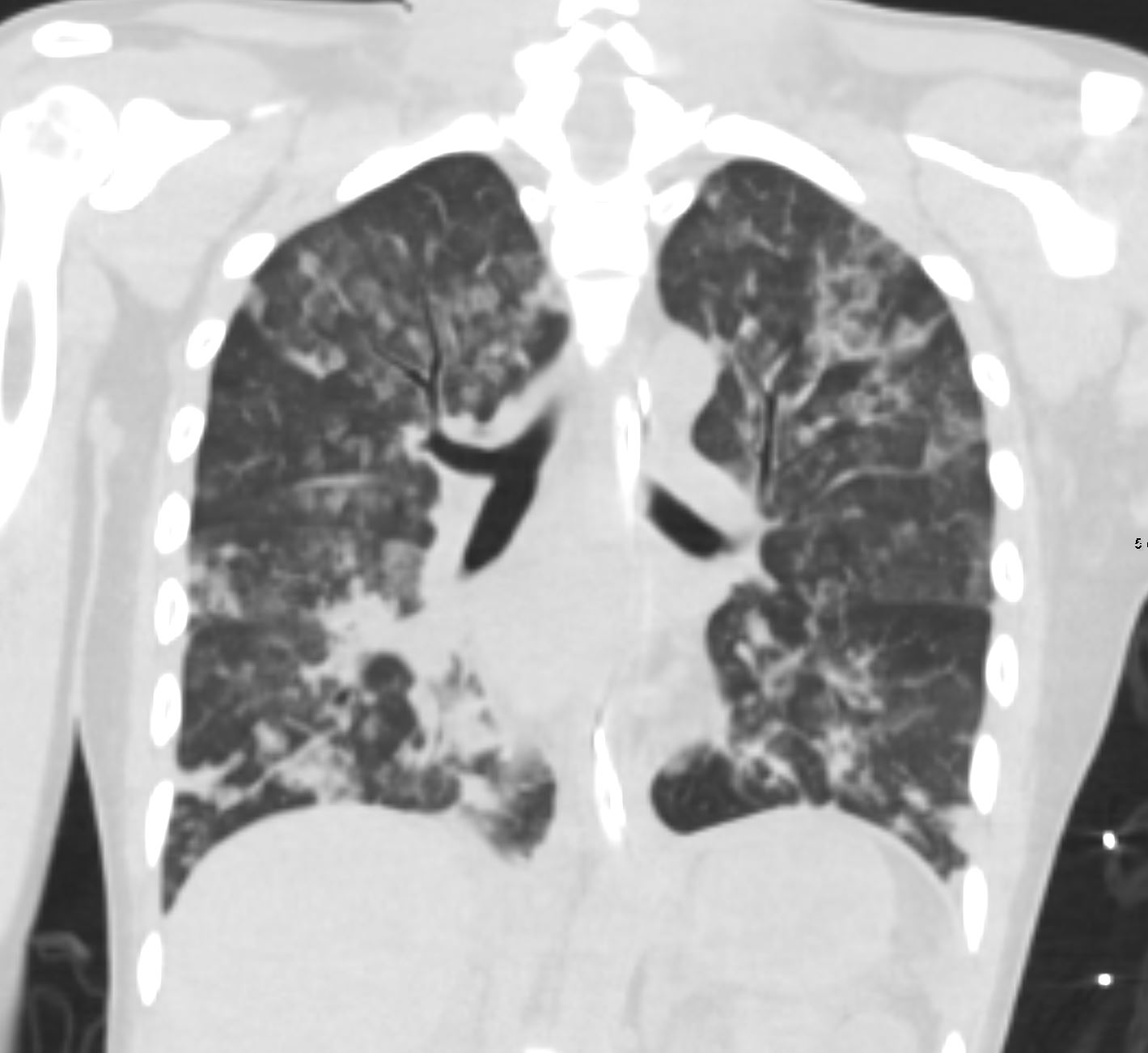
Coronal CT following trauma and resuscitative attempts in a 37 year old female shows 2-5mm solid and ground glass nodules in both the upper and lower lobes with confluence to form subsegmental foci of consolidation in the right lower lobe and right middle lobe. There is evidence of subpleural sparing with a more central distribution. These findings are consistent with hemorrhagic foci of acinar shadows or acinar nodules following trauma
Ashley Davidoff MD TheCommonVein.net 137270 key words .lungs GGO ground glass opacities acinar shadows hemorrhage contusion post resuscitation 37F
Radiological Features
- Chest X-Ray (CXR):
- Appearance:
- Small, ill-defined nodular opacities (2-5 mm).
- May appear clustered or confluent, forming larger areas of opacity.
- Distribution:
- Often diffuse or localized to specific regions depending on the underlying cause.
- Commonly seen in the perihilar, middle, or lower lung zones.
- Airspace Features:
- May resemble consolidation if confluent, with indistinct borders.
- Appearance:
- CT (High-Resolution CT – HRCT):
- Appearance:
- Better delineation of acinar nodules as discrete, small round or polygonal opacities.
- Often associated with ground-glass opacities or consolidation.
- Distribution:
- Centrilobular: Nodules centered around the bronchioles.
- Random: Scattered without a specific pattern.
- Air Bronchograms:
- Visible airways within opacified regions if extensive acinar involvement.
- Clustered Nodules:
- Nodules may coalesce, giving a patchy appearance.
- Appearance:
Characteristic Patterns on Imaging
- CXR:
- “Bat-Wing” Pattern:
- Seen in pulmonary edema where acinar shadows cluster around the hilar regions.
- “Cotton Wool” Appearance:
- Describes fluffy, ill-defined nodules (e.g., in infections or organizing pneumonia).
- “Bat-Wing” Pattern:
- CT:
- Tree-in-Bud Pattern:
- Small acinar nodules connected by branching structures, often seen in infections like tuberculosis or bronchopneumonia.
- Ground-Glass Halo:
- Acinar nodules surrounded by ground-glass opacity, suggestive of hemorrhage or fungal infections.
- Tree-in-Bud Pattern:
Differential Diagnosis
Acinar nodules or shadows can result from diseases affecting the alveoli, airspaces, or small airways. Common causes include:
- Infectious Diseases:
- Bacterial Pneumonia:
- Patchy acinar consolidation or nodules in a lobar or segmental distribution.
- Tuberculosis:
- Acinar nodules with a centrilobular distribution.
- Fungal Infections:
- Nodules with surrounding ground-glass halo (e.g., invasive aspergillosis).
- Viral Pneumonia:
- Diffuse ground-glass opacities with acinar nodules.
- Bacterial Pneumonia:
- Inflammatory/Immune Disorders:
- Organizing Pneumonia:
- Patchy, subpleural or peribronchial acinar nodules with surrounding ground-glass opacities.
- Hypersensitivity Pneumonitis:
- Centrilobular acinar nodules with ground-glass opacities.
- Organizing Pneumonia:
- Vascular Disorders:
- Pulmonary Hemorrhage:
- Ill-defined acinar nodules due to alveolar filling with blood.
- Septic Emboli:
- Randomly distributed nodules, sometimes cavitating.
- Pulmonary Hemorrhage:
- Neoplastic:
- Lymphangitic Carcinomatosis:
- Ill-defined nodular opacities along interlobular septa and acinar regions.
- Lymphangitic Carcinomatosis:
- Other Causes:
- Pulmonary Edema:
- Diffuse ill-defined acinar nodules in a perihilar distribution.
- Pulmonary Alveolar Proteinosis:
- Ground-glass opacities with superimposed acinar nodules.
- Pulmonary Edema:
Clinical Correlation
The diagnosis of acinar nodules requires correlation with clinical features:
- Acute symptoms: Suggest infection or edema.
- Chronic symptoms: May indicate neoplastic or inflammatory conditions.
- Systemic signs: Help differentiate vascular or autoimmune causes
