- Fibrosing mediastinitis
- rare condition characterized by
- docal or
- diffuse fibrosis in the mediastinum
Rossi et al Radiographics
Rossi et al Radiographics
https://pubs.rsna.org/doi/10.1148/radiographics.21.3.g01ma17737
Rossi et al Radiographics
Histoplasmosis
Rossi et al Radiographics
https://pubs.rsna.org/doi/10.1148/radiographics.21.3.g01ma17737
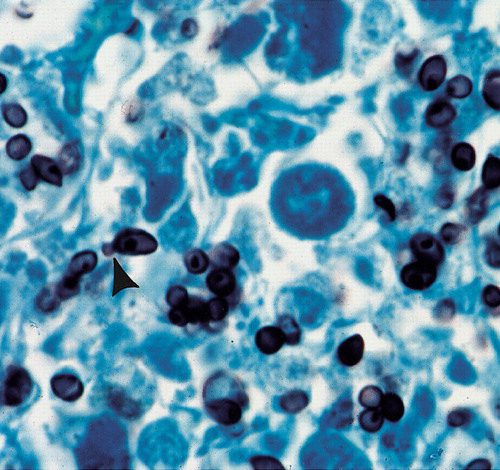
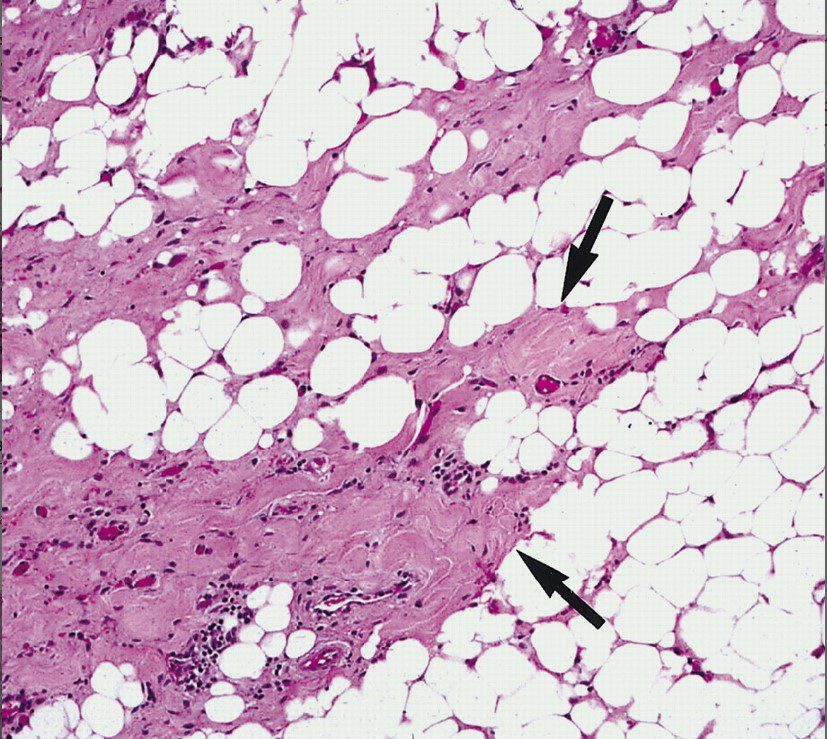
Oil immersion photomicrograph (original magnification, ×500; Grocott methenamine-silver stain) shows small oval-shaped yeasts of H capsulatum. Note the rare budding forms (arrowhead).
Rossi et al Radiographics
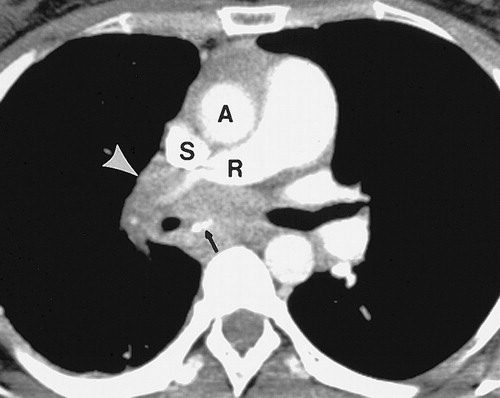
Contrast-enhanced CT scan (mediastinal window) shows a right hilar and subcarinal soft-tissue mass obstructing the right pulmonary artery (R) and superior pulmonary vein (arrowhead). More caudal images (not shown) demonstrated obstruction of the inferior pulmonary vein. Note punctate subcarinal calcification (arrow). A = aorta, S = superior vena cava.
Rossi et al Radiographics
Rossi et al Radiographics
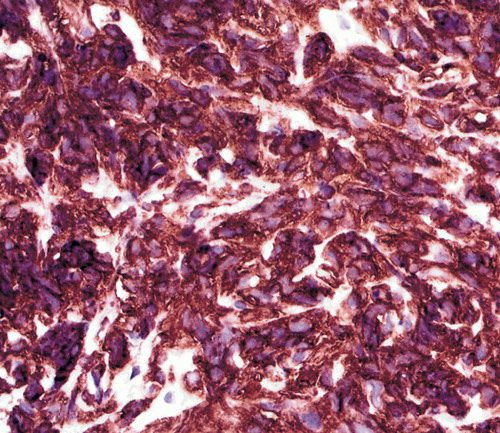
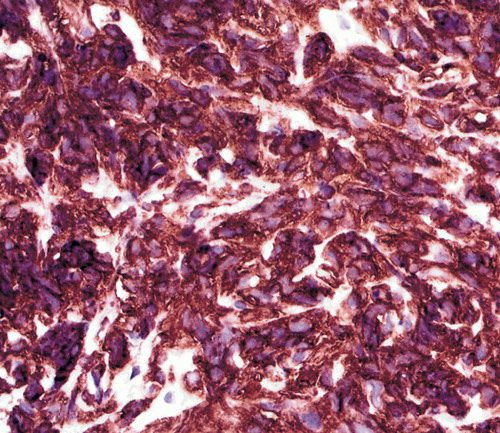
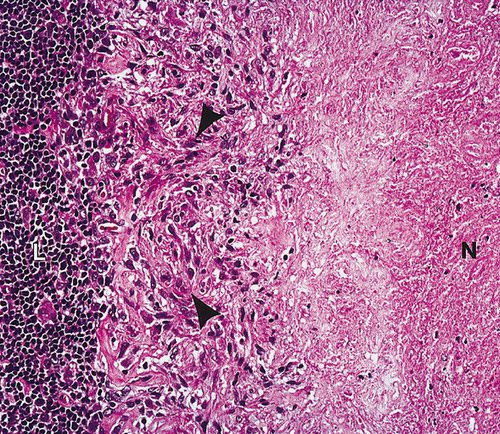
High-power photomicrograph (original magnification, ×400) of a specimen stained with immunohistochemistry for CD20 (B-cell marker) shows positive cytoplasmic staining.
Rossi et al Radiographics
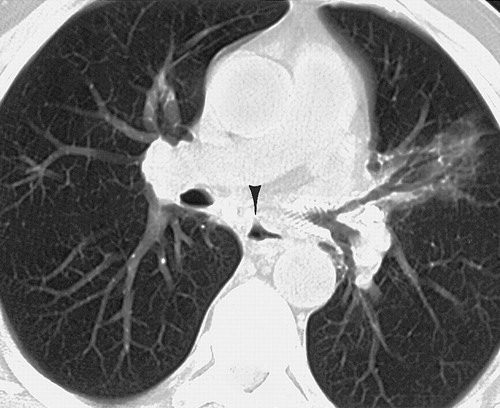
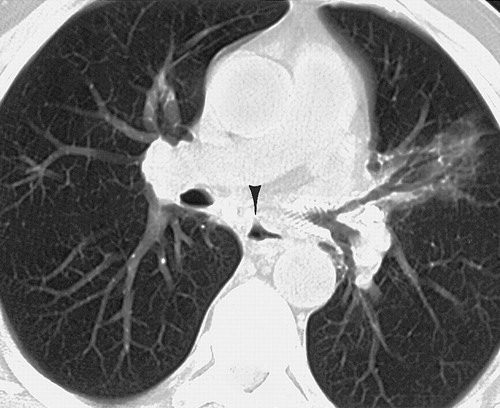
CT Appearance


Radiopaedia
Case courtesy of Darel E Heitkamp, Radiopaedia.org, rID: 13520
Encasement of Structures
Bronchus


Rossi et al Radiographics
Rossi et al Radiographics
SVC
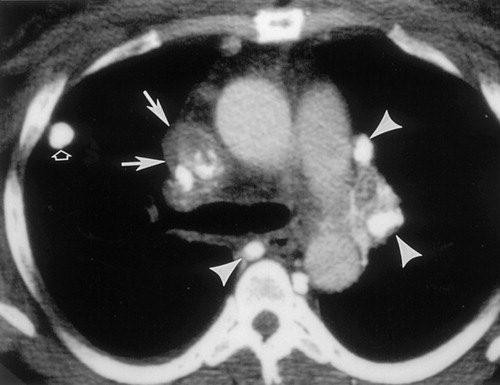
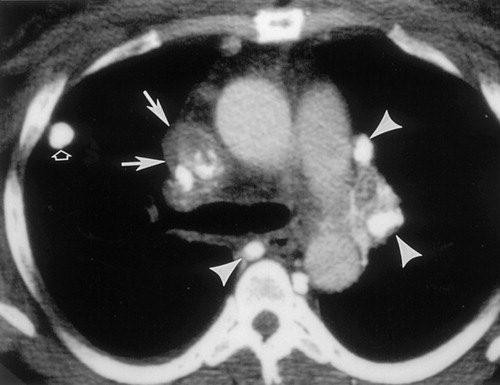
Contrast material-enhanced CT scan (mediastinal window) shows the infiltrating soft-tissue mass (solid arrows) with dense calcification in the right paratracheal region. Note obstruction of the superior vena cava, enhancement of multiple mediastinal collateral veins (arrowheads), and the densely calcified pulmonary nodule (open arrow).
Rossi et al Radiographics


Rossi et al Radiographics
Pulmonary Arteries and Veins
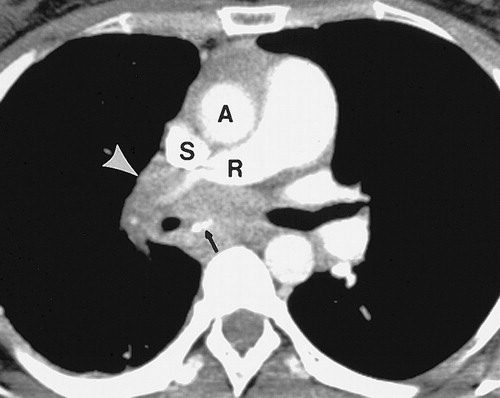
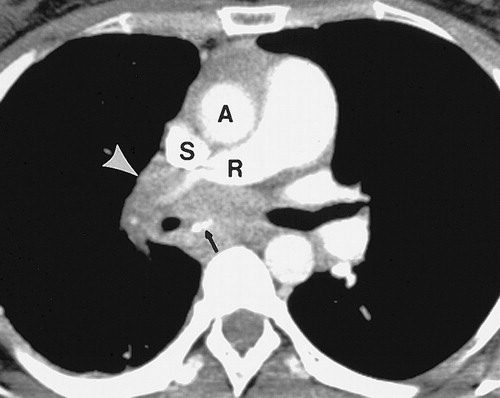
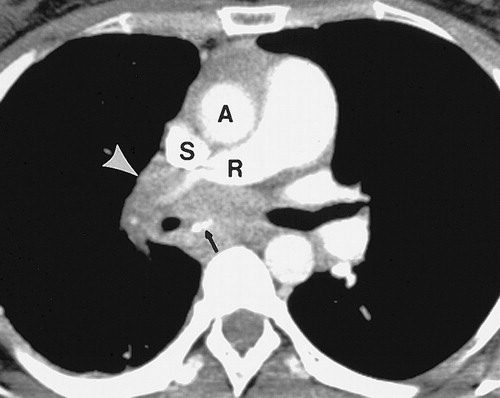
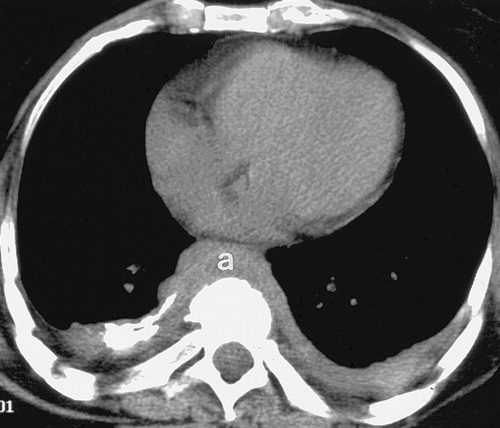
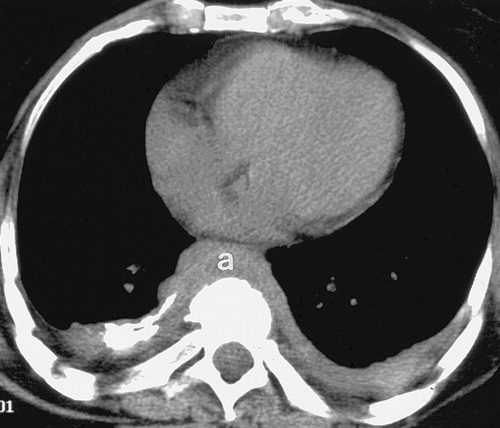
Contrast-enhanced CT scan (mediastinal window) shows a right hilar and subcarinal soft-tissue mass obstructing the right pulmonary artery (R) and superior pulmonary vein (arrowhead). More caudal images (not shown) demonstrated obstruction of the inferior pulmonary vein. Note a metallic mesh stent.
Rossi et al Radiographics
a metallic mesh stent.
Rossi et al Radiographics
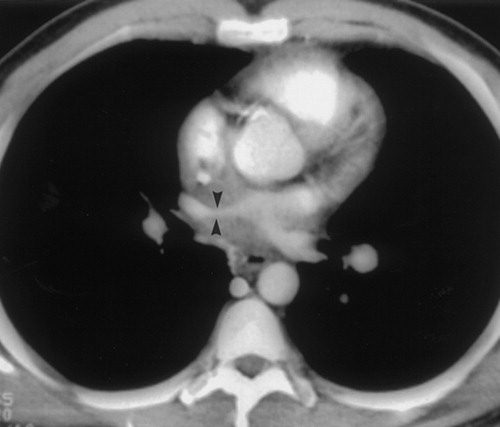
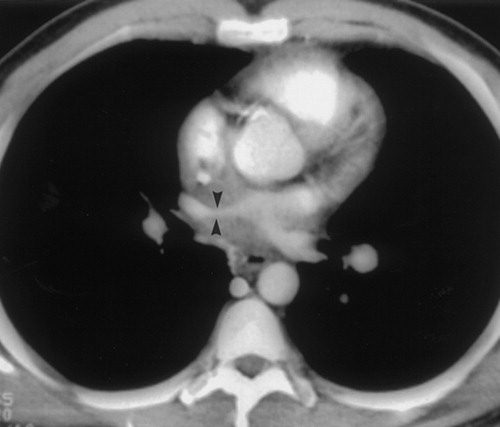
Contrast-enhanced CT scan (mediastinal window) obtained at a more caudal level shows encasement and narrowing of the right superior pulmonary vein (arrowheads).
a metallic mesh stent.
Rossi et al Radiographics
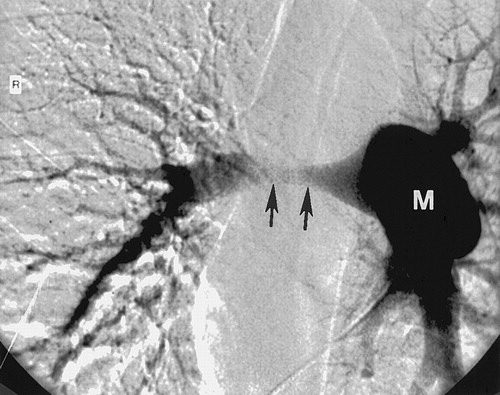
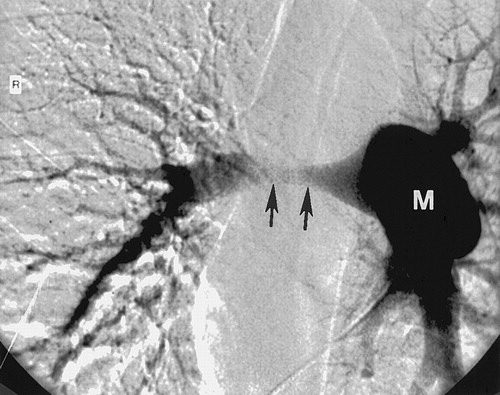
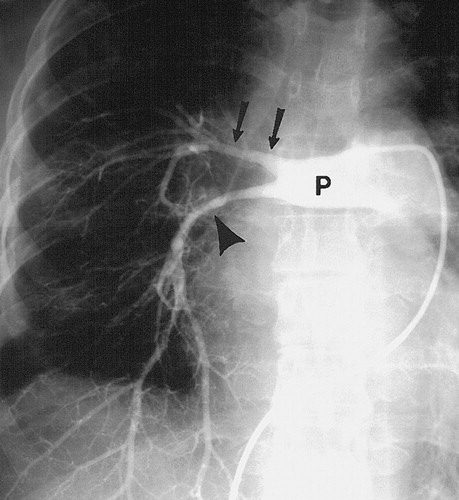
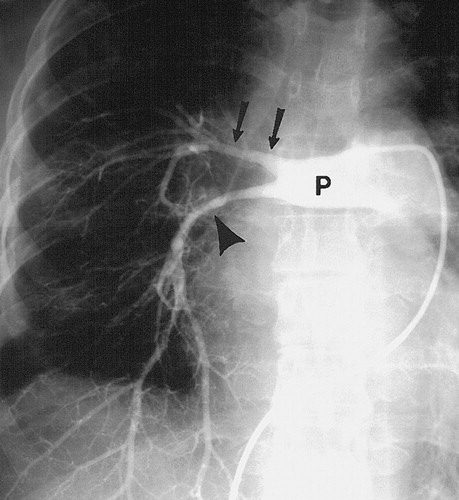
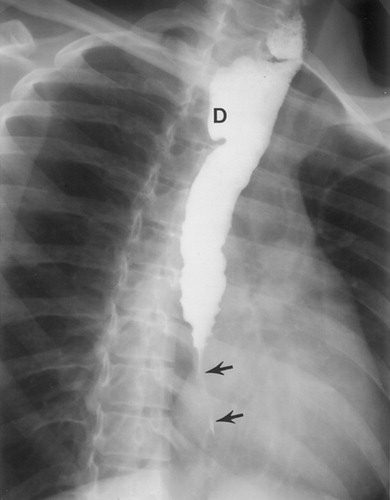
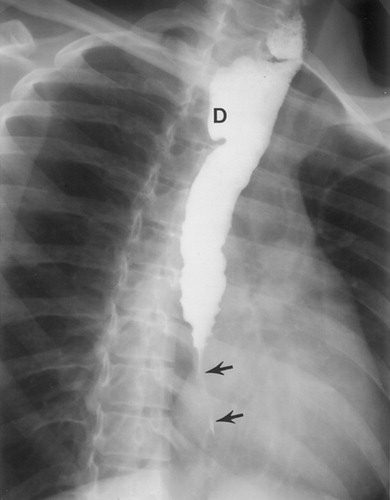
Frontal pulmonary arteriogram shows smooth long-segment narrowing (arrows) of the right main pulmonary artery (M).
a metallic mesh stent.
Rossi et al Radiographics
Aorta
Rossi et al Radiographics
Esophagus
a metallic mesh stent.
Rossi et al Radiographics
- Cause
- idiopathic:
- ? IgG4-related disease 17
- ? abnormal immune response to a
- Infection
-
- fungal
- Histoplasma capsulatum infection (histoplasmosis)
- localised pattern
- Histoplasma capsulatum infection (histoplasmosis)
- bacterial infection
- TB
- fungal
-
- Inflammatory Disease
-
-
- sarcoidosis
- radiation therapy
-
-
- Malignancy
-
-
- intrathoracic malignancy
-
-
- Metabolic
-
-
- drugs: e.g. methysergide therapy 8
-
-
- Associations
-
-
- Reidel thyroiditis
- rheumatoid arthritis (RA)
- systemic lupus erythematosus (SLE) 7
- Behçet disease
- retroperitoneal fibrosis
-
- results
- excessive growth of fibrous tissue in the mediastinum,
-
- focal: ~80%
- diffuse: ~20%
-
- excessive growth of fibrous tissue in the mediastinum,
-
- Clinical
- Symptoms of fibrosing mediastinitis can include
- chest pain,
- cough,
- compression of the
-
- superior vena cava,
- pulmonary veins or arteries,
- central airways, or
- esophagus
-
- resulting in
- shortness of breath, and
- difficulty swallowing.
- obstruction or
- Symptoms of fibrosing mediastinitis can include
- Diagnosis
- CT
- Mediastinum
- diffuse
- focal
- middle mediastinum
- mediastinal mass
- hilar mass
- loss of fat planes
- encasement of structures
- trachea
- arteries
- veins
- bronchial arteries due to vascular compromise
- calcifications of the
- mass or associated
- lymph nodes:
- histoplasmosis
- Mediastinum
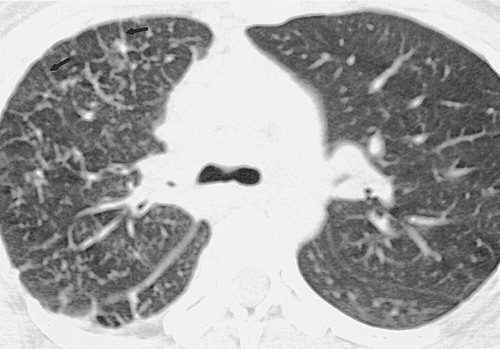
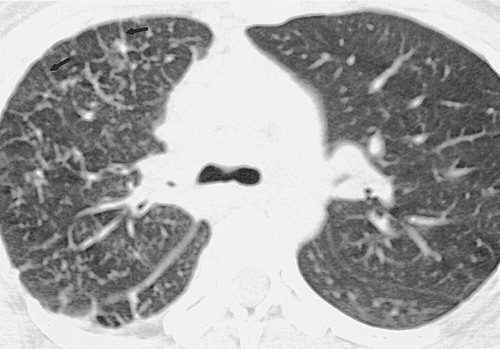
- Parenchymal changes secondary to
- compression of
- veins or lymphatics
- prominent interstitial pattern
- crazy paving secondary lymphatic or venous obstruction
- veins or lymphatics
- compression of
- CT
-
- MRI scans, and
- biopsy
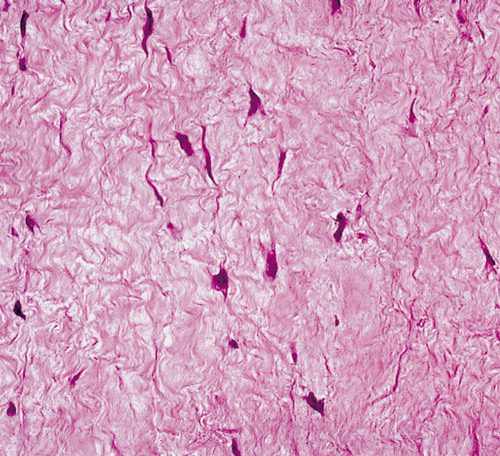
soft-tissue attenuation which obliterates normal mediastinal fat planes and encases or invades adjacent structures: diffuse form
- MRI
- Fibrous tissue with inflammation and therefore
- T1: dark
- isointense to muscle
- heterogeneous
- T2: variable with both
- dark
- light intensities
- T1 C+ (Gd):
- heterogeneous enhancement
- T1: dark
- Fibrous tissue with inflammation and therefore
- Treatment and prognosis
- slowly progressive
- unpredictable course, with both
- spontaneous remission or
- exacerbation
It usually tends to . There are three possible avenues for treatment: systemic antifungal or corticosteroid treatment, surgical resection, and local therapy for complications.
- Treatment
- limited
- Antifungalsm
- Steroids (diffuse disease more responsive)
- managing symptoms and
- preventing complications,
- medication to reduce inflammation and pain,
- interventions to
- relieve compression
- preventing complications,
