39 year old male with limited SSc
scleroderma complicated by ILD and digital vasculopathy with ulcers.
Groundglass opacities are seen in a
predominantly peripheral and peribronchial location with a lower lobe
predominance. There is mild traction bronchiectasis and
bronchiolectasis. There are diffuse subpleural reticulations. No
honeycombing. There is no evidence of air trapping on expiratory
images.
cScleroderma Obliterative Bronchiolitis vs Cellular NSIP

39-year-old-male with a history of scleroderma associated with ILD and digital vasculopathy with ulcers.
Coronal CT shows mosaic attenuation peripheral ground glass changes with wall thickening of the bronchioles, bronchiolectasis, ground glass changes, and poorly defined ground glass centrilobular nodules.
In this clinical setting obliterative bronchiolitis (aka bronchiolitis obliterans aka constrictive bronchiolitis) Cellular NSIP is also a radiological consideration.
Ashley Davidoff MD TheCommonVein.net 132Lu 136665c
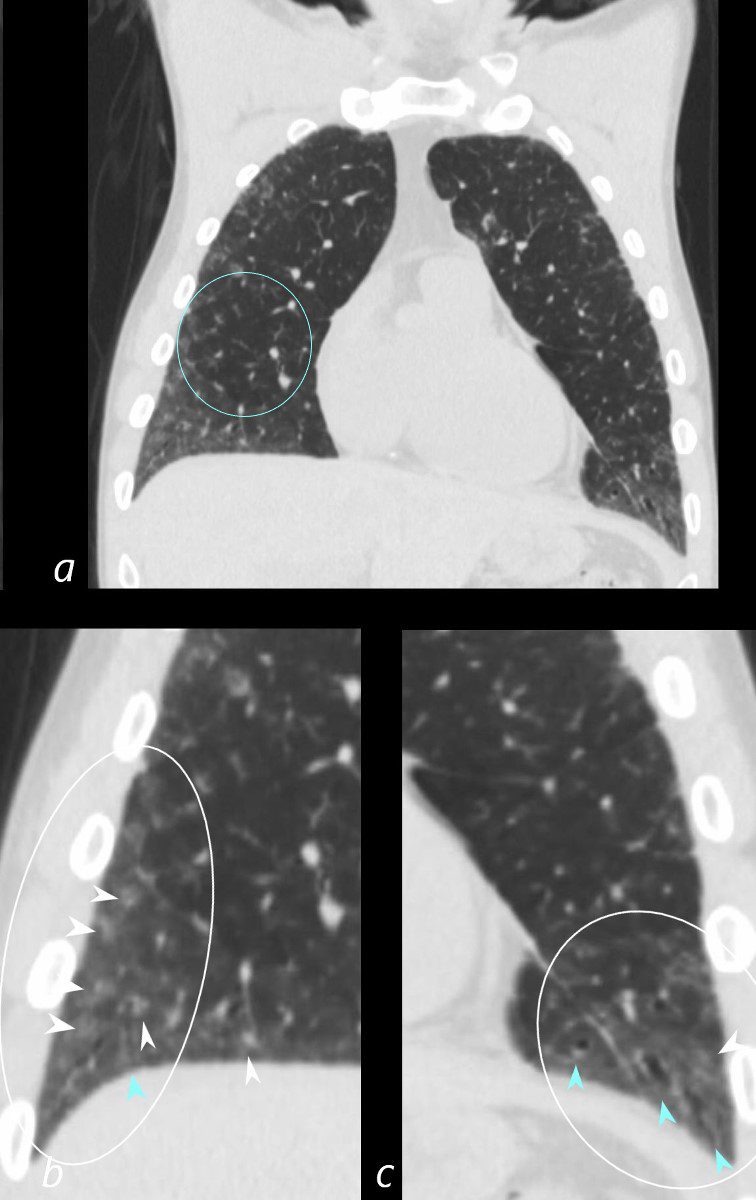
39-year-old-male with a history of scleroderma associated with ILD and digital vasculopathy with ulcers.
Coronal CT shows mosaic attenuation (a, ringed in teal) peripheral ground glass changes with wall thickening of the bronchioles, and bronchiolectasis (blue arrowheads, b, c) , ground glass changes (ringed in white), and poorly defined ground glass centrilobular nodules (white arrowheads).
In this clinical setting obliterative bronchiolitis (aka bronchiolitis obliterans aka constrictive bronchiolitis) is suggested. Cellular NSIP is also a radiological consideration.
Ashley Davidoff MD TheCommonVein.net 132Lu 136665cL

39-year-old-male with a history of scleroderma associated with ILD and digital vasculopathy with ulcers.
Coronal CT shows mosaic attenuation peripheral ground glass changes with wall thickening of the bronchioles, bronchiolectasis, ground glass changes, and poorly defined ground glass centrilobular nodules.
In this clinical setting obliterative bronchiolitis (aka bronchiolitis obliterans aka constrictive bronchiolitis) is suggested. Cellular NSIP is also a radiological consideration.
Ashley Davidoff MD TheCommonVein.net 132Lu 136667
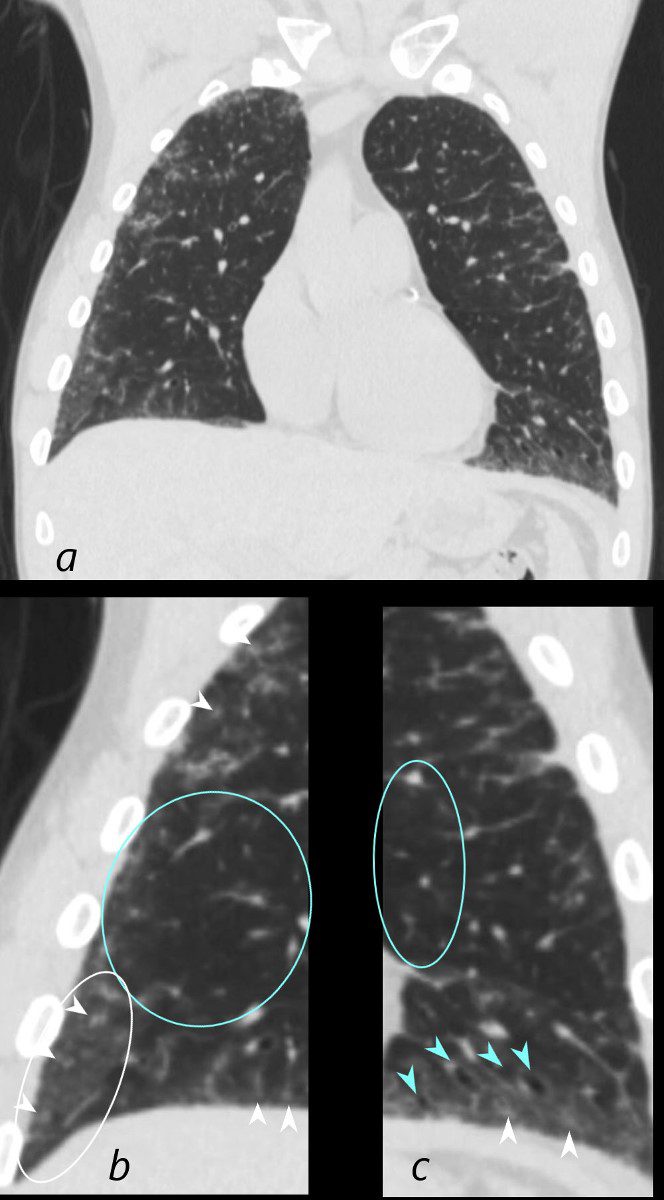
39-year-old-male with a history of scleroderma associated with ILD and digital vasculopathy with ulcers.
Coronal CT shows mosaic attenuation (ringed in teal, b, c) peripheral ground glass changes with wall thickening of the bronchioles, and bronchiolectasis,( teal arrowheads, c) ground glass changes,(ringed in white, b) and poorly defined ground glass centrilobular nodules (white arrowheads b,c).
In this clinical setting obliterative bronchiolitis (aka bronchiolitis obliterans aka constrictive bronchiolitis) is suggested. Cellular NSIP is also a radiological consideration.
Ashley Davidoff MD TheCommonVein.net 132Lu 136667cL

39-year-old-male with a history of scleroderma associated with ILD and digital vasculopathy with ulcers.
Coronal CT shows mosaic attenuation, peripheral ground glass changes poorly defined ground glass centrilobular nodules and mild reticulation.
In this clinical setting obliterative bronchiolitis (aka bronchiolitis obliterans aka constrictive bronchiolitis) is suggested. Cellular NSIP is also a radiological consideration.
Ashley Davidoff MD TheCommonVein.net 132Lu 136668
Airway Disease Segmental Subsegmental and Small Airways
CT Scleroderma Obliterative Bronchiolitis
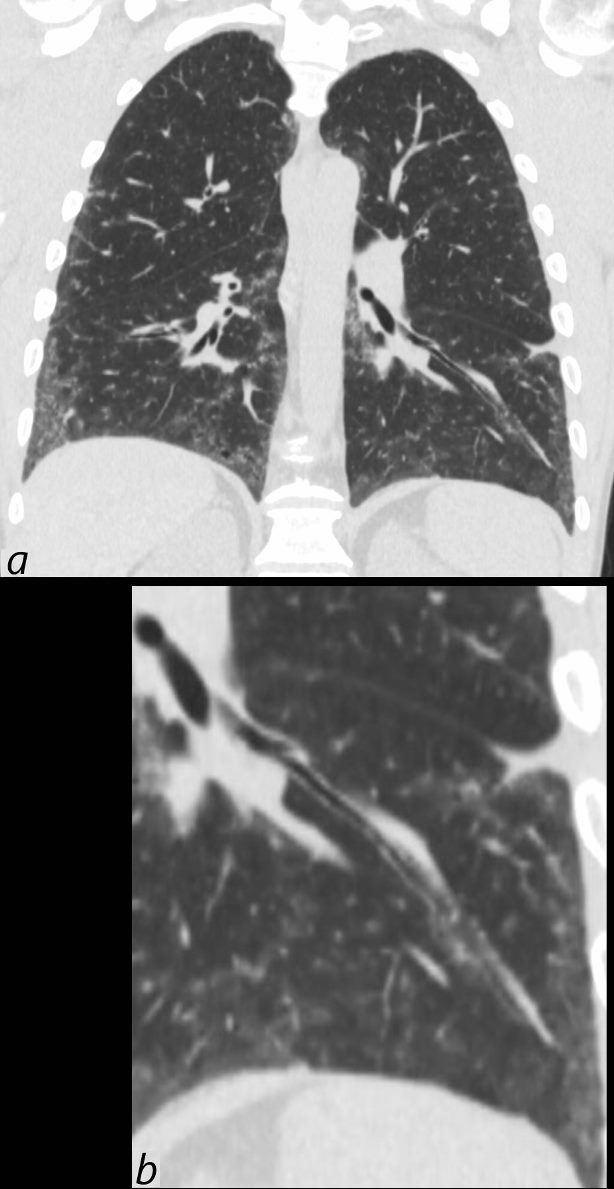
39-year-old-male with a history of scleroderma associated with ILD and digital vasculopathy with ulcers.
Coronal CT shows thickening of the segmental and subsegmental airway supplying the lateral basal segment of the left lower lobe. In addition there is a background of peripheral ground glass changes poorly defined ground glass centrilobular nodules and mild reticulation.
In this clinical setting obliterative bronchiolitis (aka bronchiolitis obliterans aka constrictive bronchiolitis) is suggested. Cellular NSIP is also a radiological consideration.
Ashley Davidoff MD TheCommonVein.net 132Lu 136669c
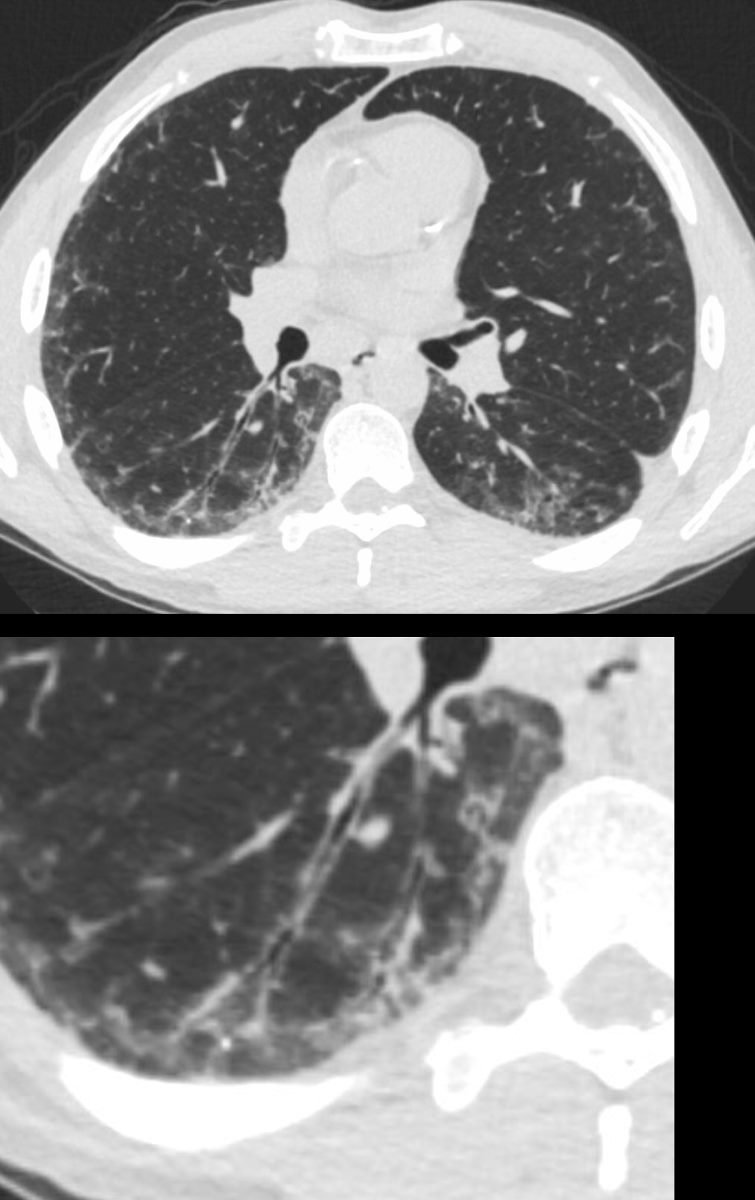
39-year-old-male with a history of scleroderma associated with ILD and digital vasculopathy with ulcers.
Axial CT shows thickening of the segmental, subsegmental and small airways supplying the posterior basal segment of the right lower lobe. In addition there is a background poorly defined ground glass changes and mild reticulation.
In this clinical setting obliterative bronchiolitis (aka bronchiolitis obliterans aka constrictive bronchiolitis) is suggested. Cellular NSIP is also a radiological consideration.
Ashley Davidoff MD TheCommonVein.net 132Lu 136669c
Micronodules and Ground Glass with Peripheral Sparing
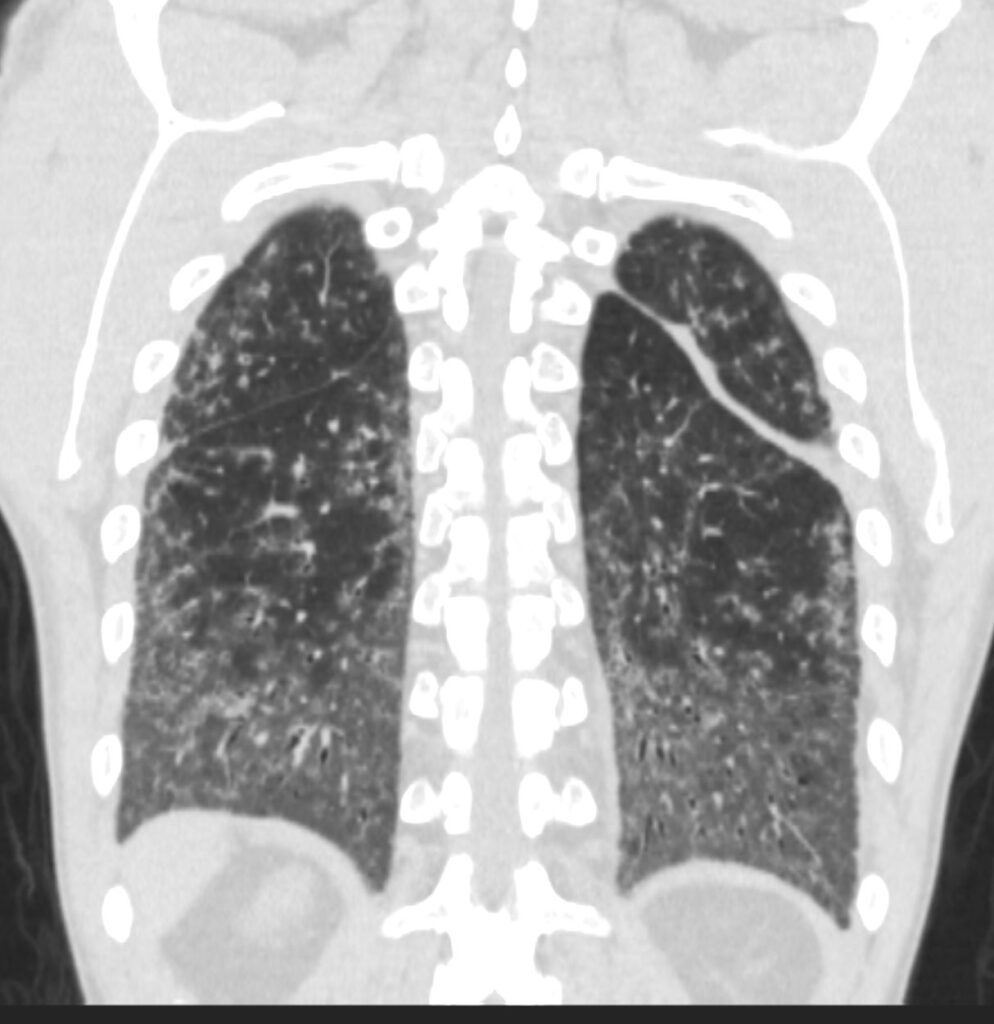
39-year-old-male with a history of scleroderma associated with ILD and digital vasculopathy with ulcers.
Coronal CT at the level of the spine shows extensive ground glass in the lower lung fields, with subpleural sparing better visualized on the left. Ill defined ground glass centrilobular nodules and mosaic attenuation suggest small airway disease.
In this clinical setting obliterative bronchiolitis (aka bronchiolitis obliterans aka constrictive bronchiolitis) and cellular NSIP are radiological considerations.
Ashley Davidoff MD TheCommonVein.net 132Lu 136667
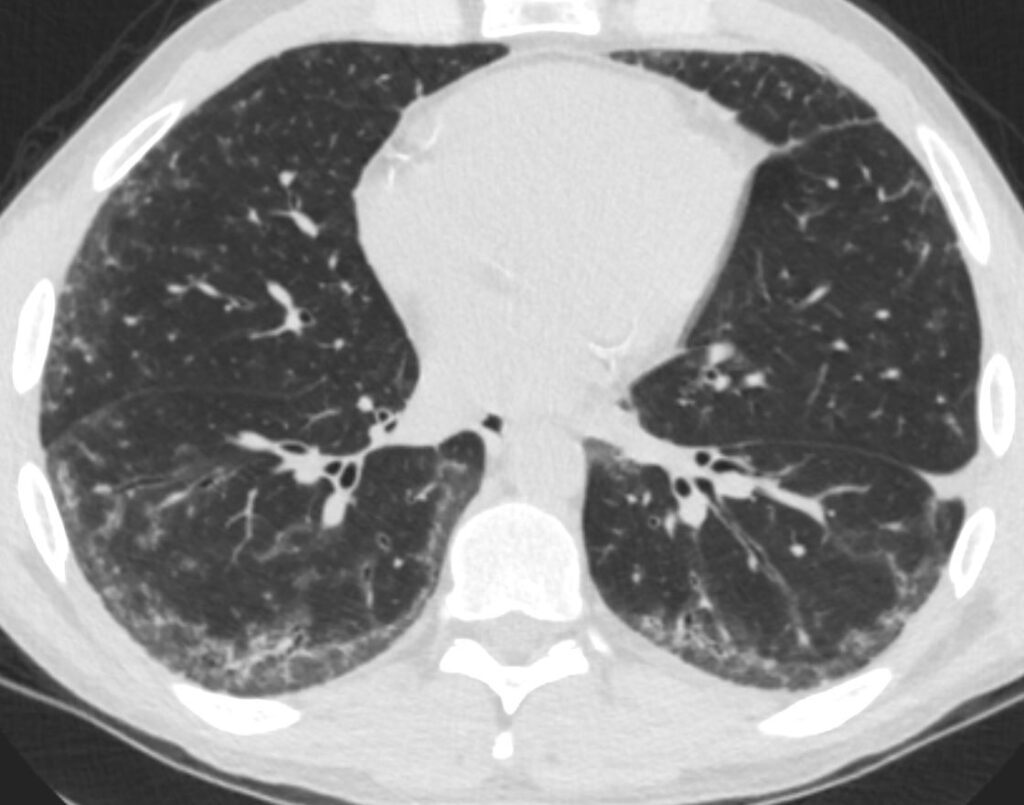
39-year-old-male with a history of scleroderma associated with ILD and digital vasculopathy with ulcers.
Axial CT at the lung bases shows bibasilar peripheral ground glass changes, with subpleural sparing. Ill defined ground glass centrilobular nodules and mosaic attenuation suggest small airway disease.
In this clinical setting obliterative bronchiolitis (aka bronchiolitis obliterans aka constrictive bronchiolitis) and cellular NSIP are radiological considerations.
Ashley Davidoff MD TheCommonVein.net 132Lu 136675
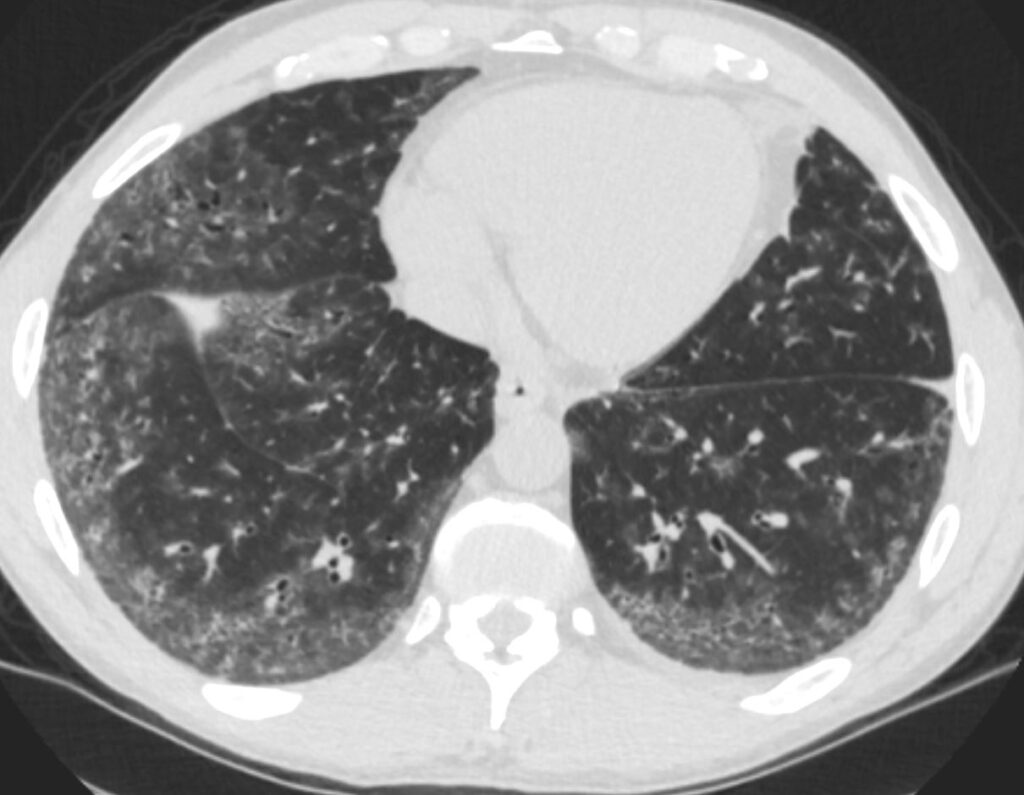
39-year-old-male with a history of scleroderma associated with ILD and digital vasculopathy with ulcers.
Axial CT at the lung bases shows bibasilar peripheral ground glass changes, with subpleural sparing. Ill defined ground glass centrilobular nodules suggest small airway disease.
In this clinical setting obliterative bronchiolitis (aka bronchiolitis obliterans aka constrictive bronchiolitis) and cellular NSIP are radiological considerations.
Ashley Davidoff MD TheCommonVein.net 132Lu 136676
Bronchiolectasis
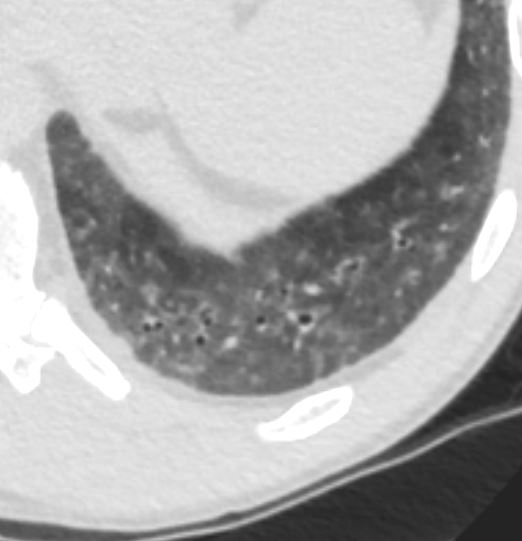
39-year-old-male with a history of scleroderma associated with ILD and digital vasculopathy with ulcers.
Axial CT through the left posterior recess shows peripheral ground glass changes, with subpleural sparing and bronchiolectasis without wall thickening. Ill defined ground glass centrilobular nodules suggest small airway disease.
In this clinical setting obliterative bronchiolitis (aka bronchiolitis obliterans aka constrictive bronchiolitis) and cellular NSIP are radiological considerations.
Ashley Davidoff MD TheCommonVein.net 132Lu 136678
Premature Coronary Calcification
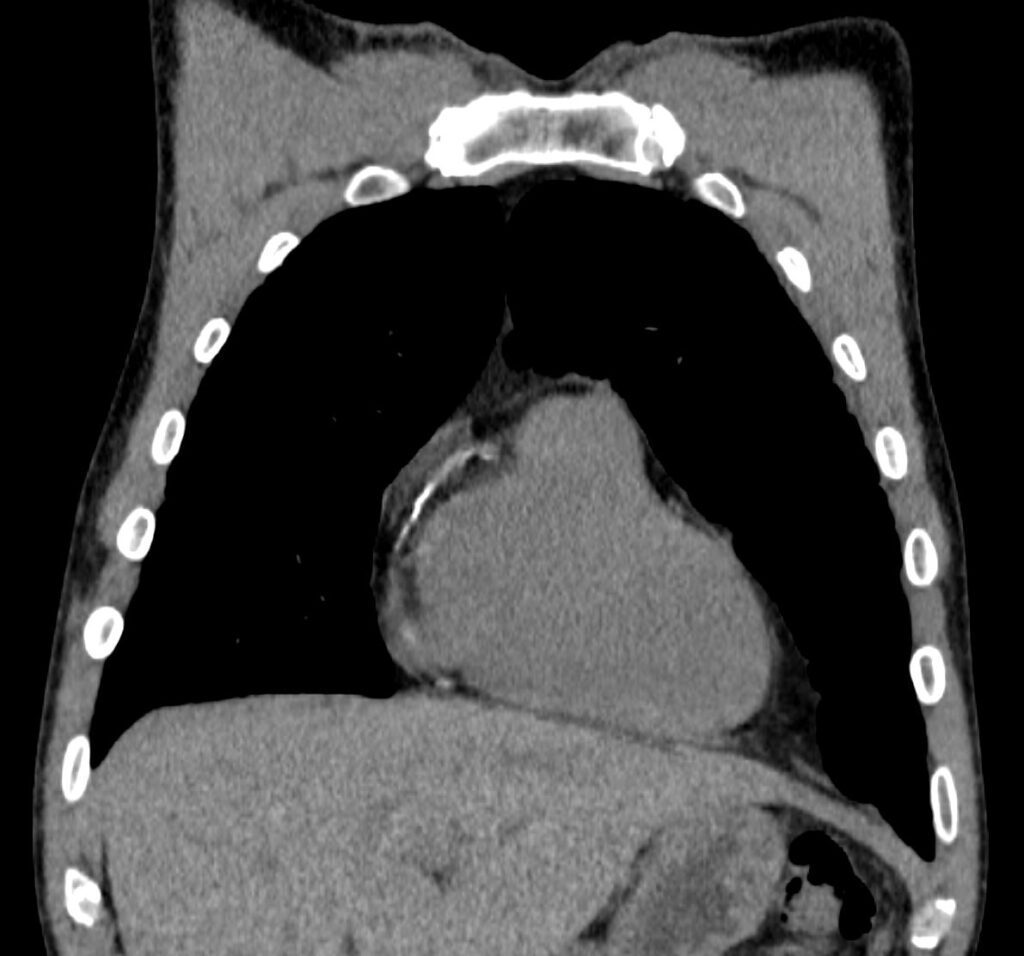
39-year-old-male with a history of scleroderma associated with ILD and digital vasculopathy with ulcers.
Coronal CT shows premature calcification of his right coronary artery
Ashley Davidoff MD TheCommonVein.net 132Lu 136666
