Upper and mid lung field distribution
Ashley Davidoff MD TheCommonvein.net lungs-0772
Structures Involved
Small Airways
Lung Parenchyma
Interstitial Tissue
Imaging Appearances
- Upper Lung Predominance:
- Nodules and Cysts:
- cysts are often irregularly shaped and
- may vary in size.
- Centrilobular Nodules:
- Ground-Glass Opacities:
- Ground-glass opacities may be observed on CT scans, representing areas of increased lung density. These opacities can be associated with inflammation and infiltration of Langerhans cells.
Early
-
- cellular interstitial infiltrates of
- Langerhans’ cells,
- Staining with antibodies against CD1a antigen on the cell surface
- lymphocytes,
- macrophages,
eosinophils, plasma cells, and fibroblasts
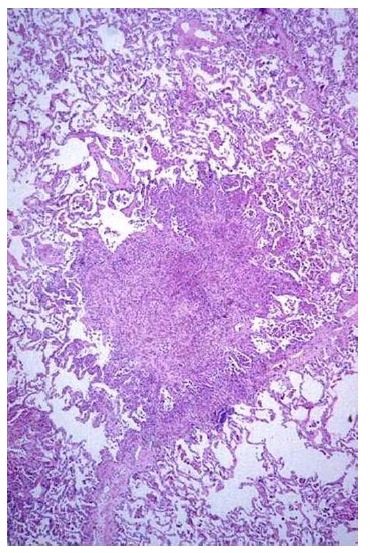
- Mid stages
- infiltrates enlarge to form nodules centered on small airways (peribronchial)
- often stellate in configuration
Early Phase
-

Figure 9. Nodular infiltrates with a stellate border extending into the surrounding interstitium in a patient with PLCH. (Courtesy of Professor A. Pesci, University of Parma.) - next Phase
- Cavitation within nodules due to
- either an airway remnant or
- de novo cavitation due to an enlarging
inflammatory infiltrate
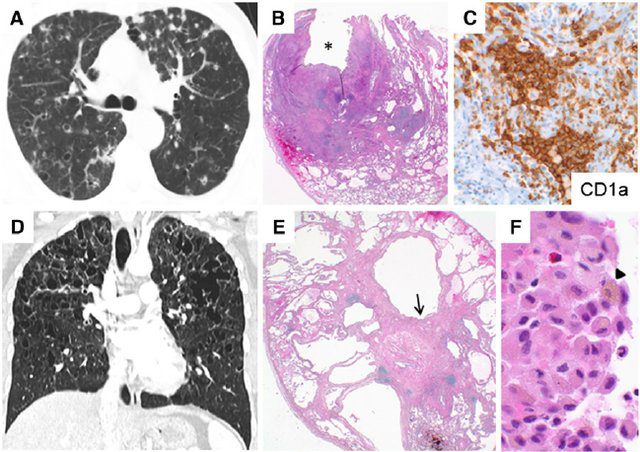
Gupta et al Diffuse Cystic Lung Disease: Part I American Journal of Respiratory and Critical Care Medicine 191(12) April 2015
Cavitation
Cyst Formation Initially Thick Walled
Then Thin Walled Cysts
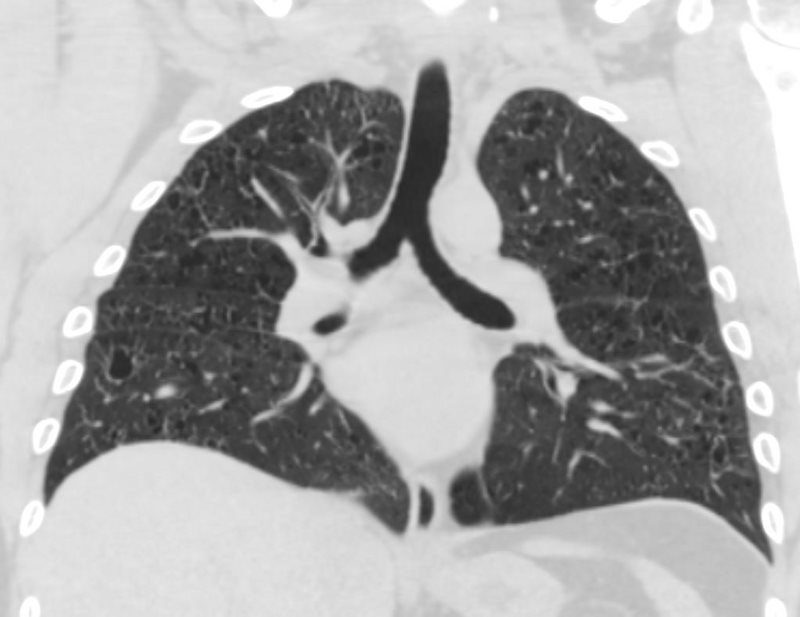
CT UPPER LUNG ZONE PROMINENCE OF SMALL THIN WALLED CYSTS
LANGERHANS HISTIOCYTOSIS
Ashley Davidoff MD
53-year-old female with nicotine dependence presents with dyspnea and cough
CXR (PA and Lateral) shows bilateral and extensive reticular nodular changes slightly more prominent in the upper lung zones
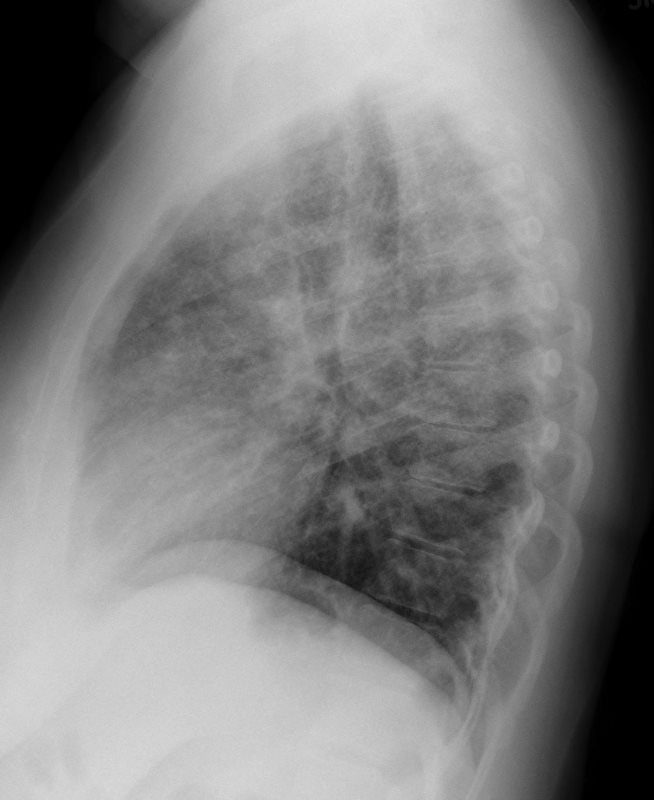
CXR (PA and Lateral) shows bilateral and extensive reticular nodular changes slightly more prominent in the upper lung zones
Ashley Davidoff MD
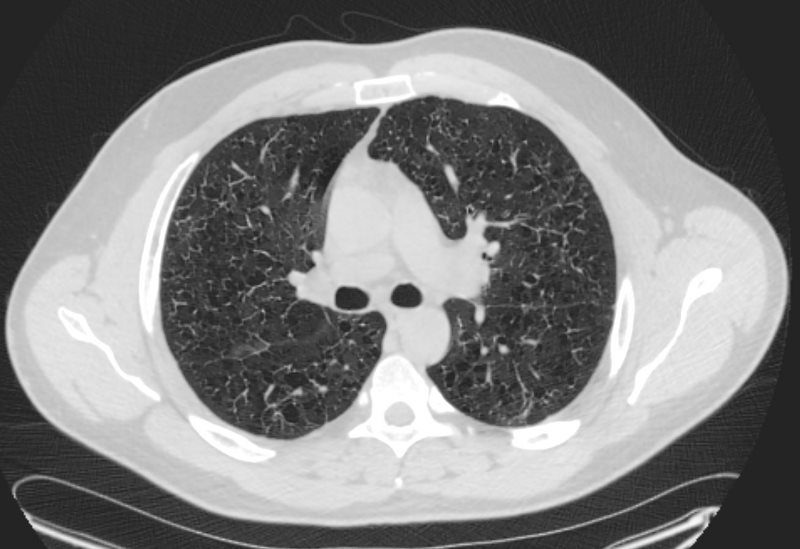
CT scan shows multiple relatively thick-walled cysts predominantly in the upper lobes. The cysts are round and air filled large and are between 5mm-8mm
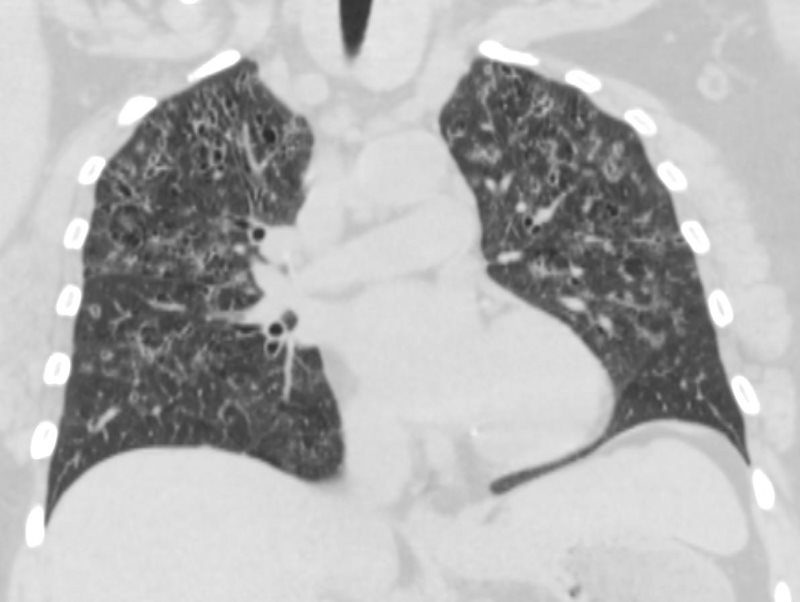
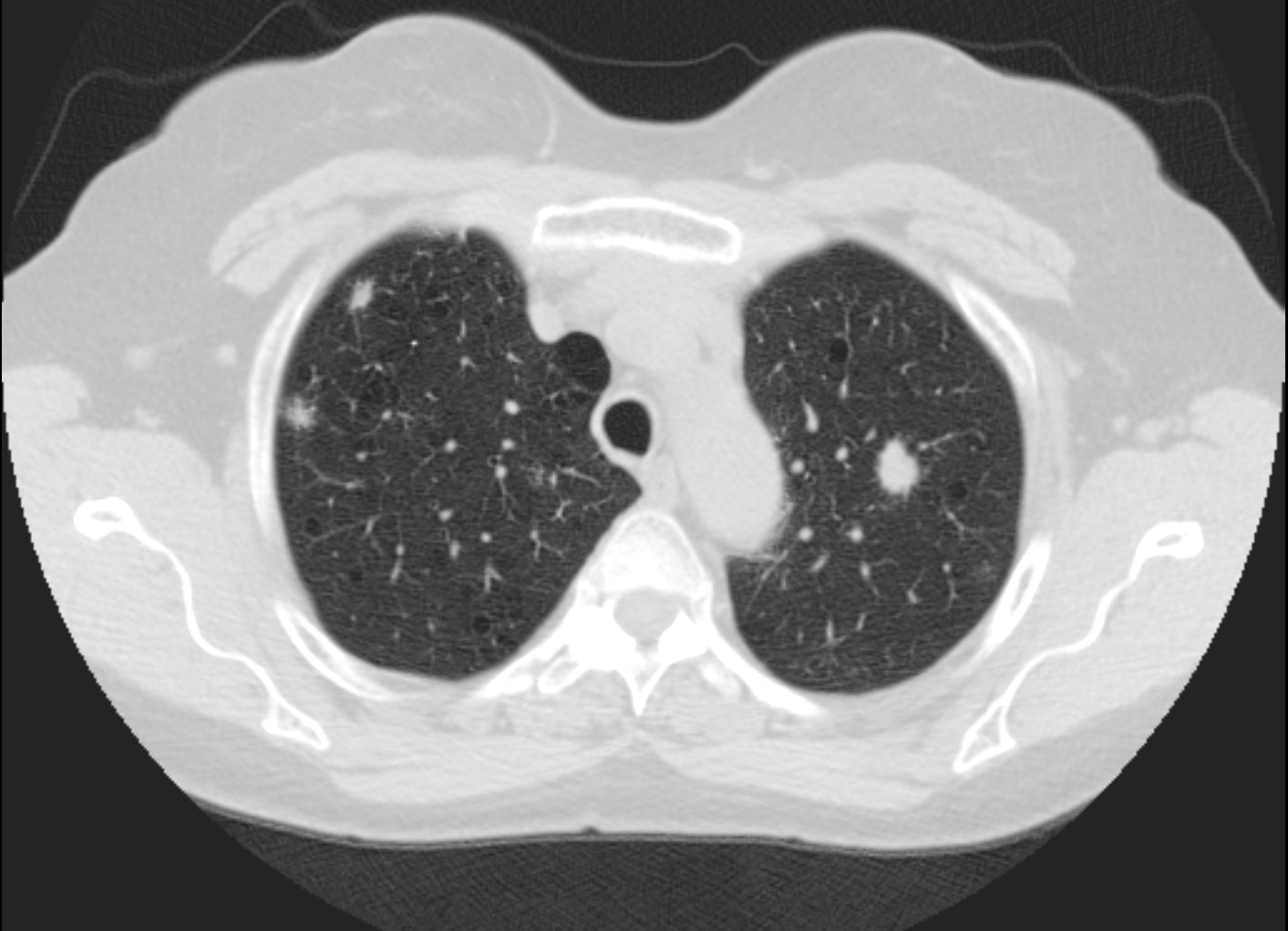
53-year-old female with nicotine dependence presents with dyspnea and cough
CXR (PA and Lateral) shows bilateral and extensive reticular nodular changes slightly more prominent in the upper lung zones
CT scan from 16 months prior showed multiple relatively thick-walled cysts predominantly in the upper lobes. The cysts are round and air filled large and are between 5mm-8mm
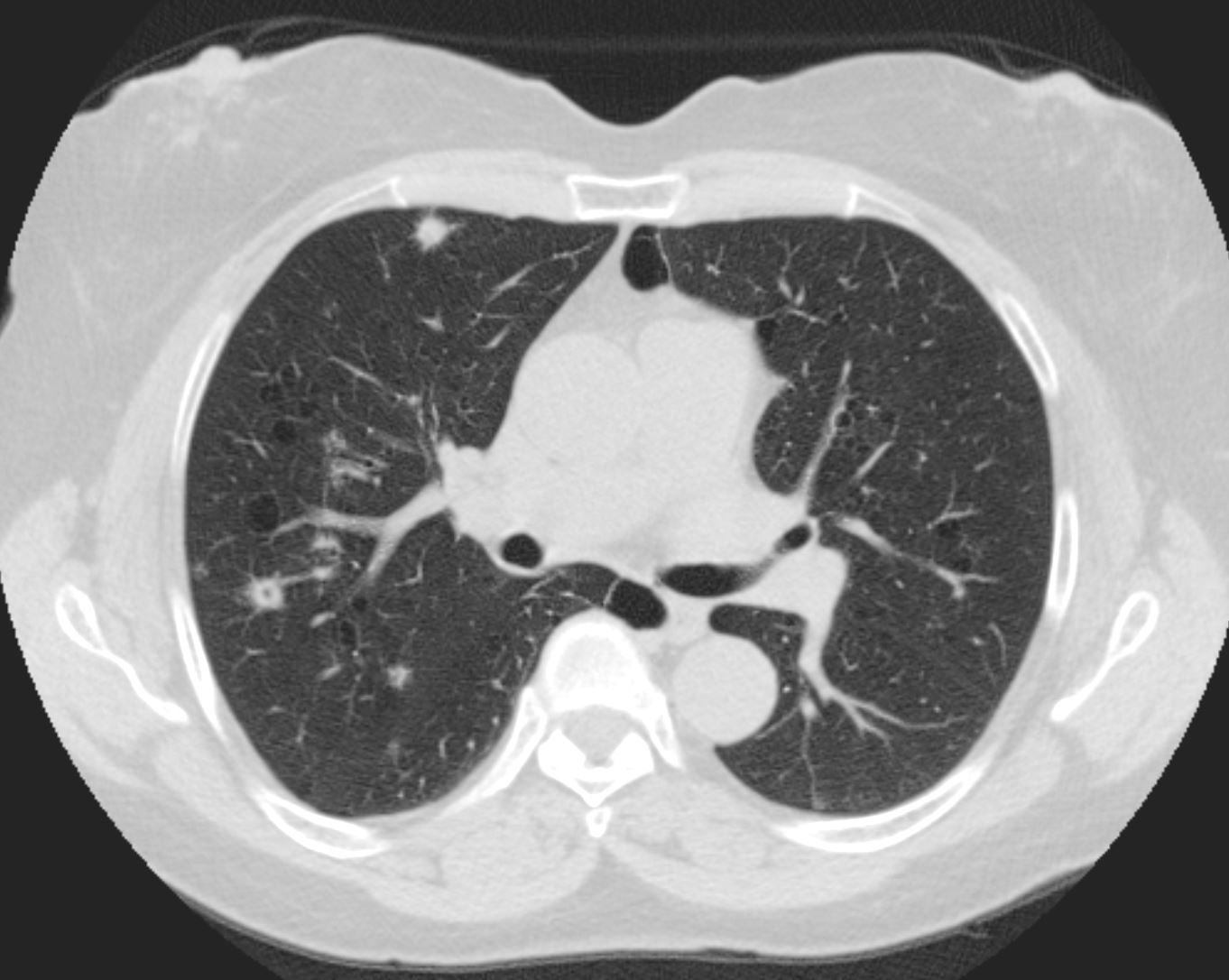
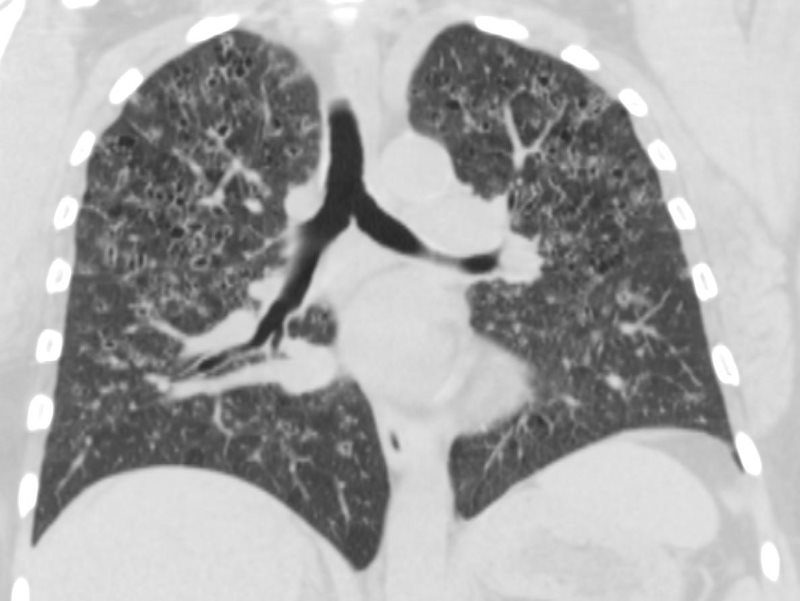
CT scan 9 months later shows improvement in the thickened walls of the cysts but maintenance of diffuse cystic changes predominantly in the upper lobes
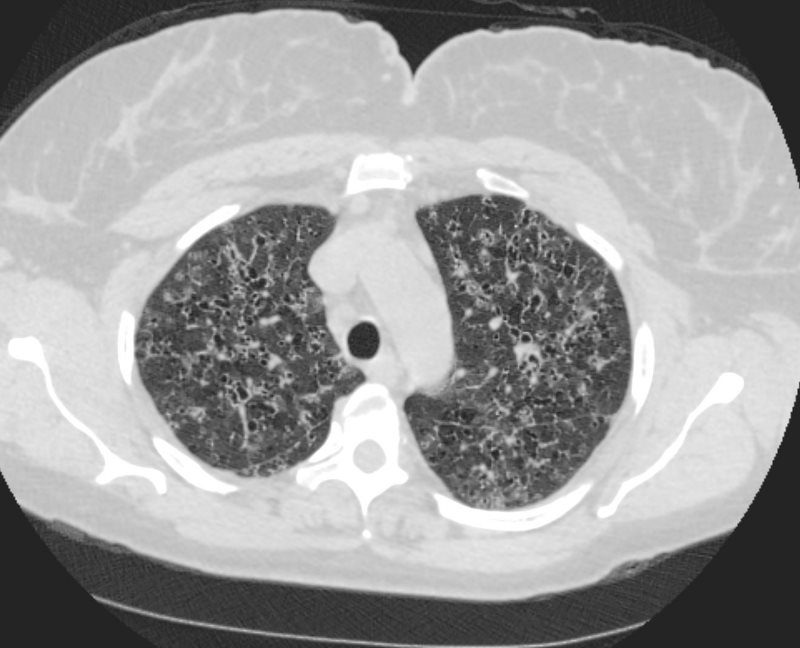
A CT scan done 2 years later shows no significant change in the diffuse bilateral cystic changes, dominant in the upper lobes and consistent with Langerhans histiocytosis
Ashley Davidoff MD
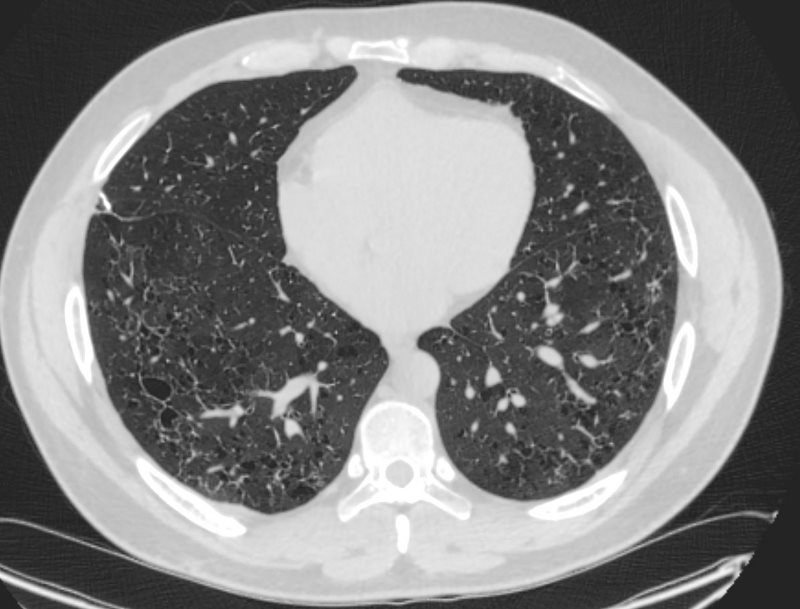
53-year-old female with nicotine dependence presents with dyspnea and cough
CXR (PA and Lateral) shows bilateral and extensive reticular nodular changes slightly more prominent in the upper lung zones
CT scan from 16 months prior showed multiple relatively thick-walled cysts predominantly in the upper lobes. The cysts are round and air filled large and are between 5mm-8mm
CT scan 9 months later shows improvement in the thickened walls of the cysts but maintenance of diffuse cystic changes predominantly in the upper lobes
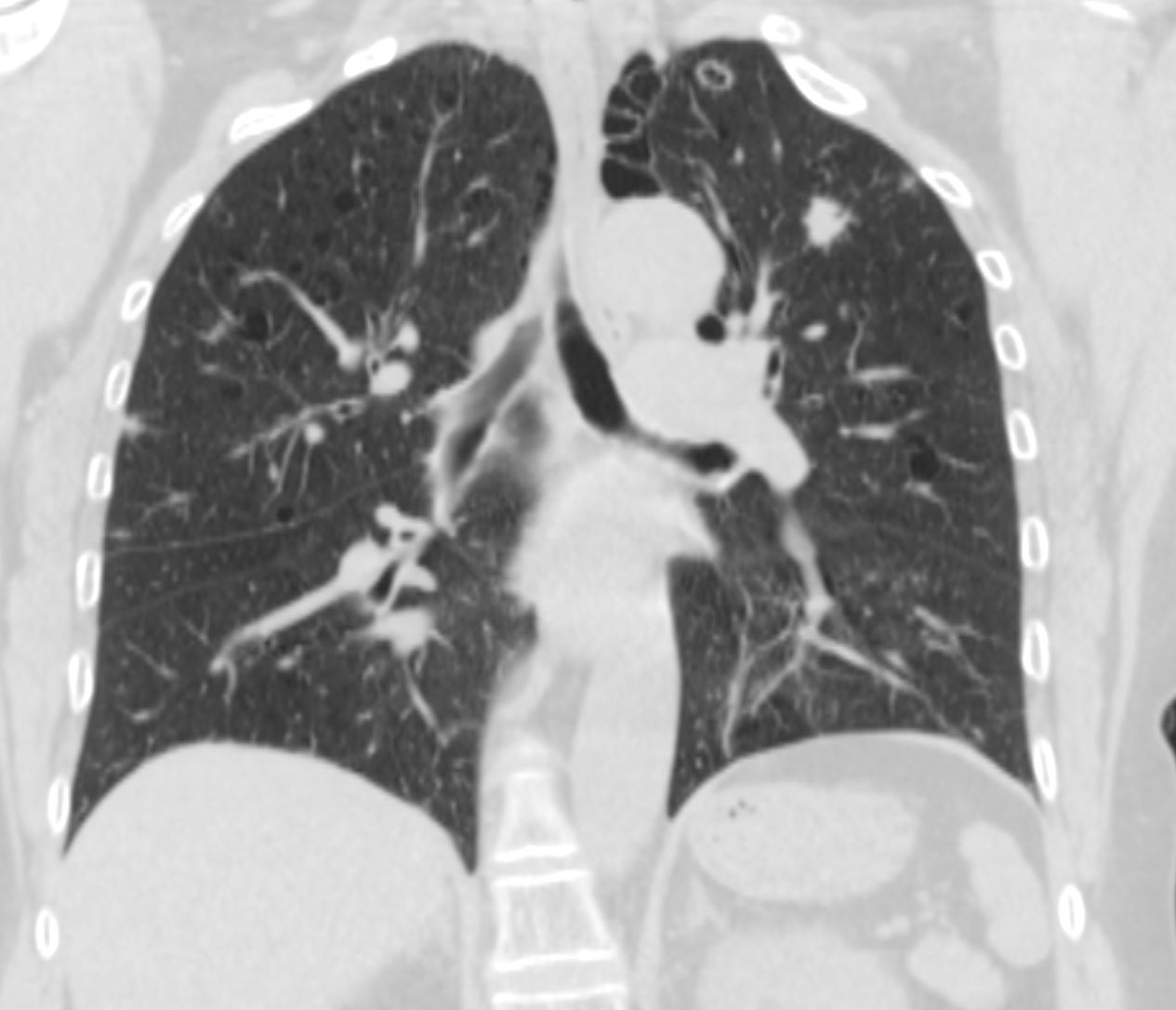
A CT scan done 2 years later shows no significant change in the diffuse bilateral cystic changes, dominant in the upper lobes and consistent with Langerhans histiocytosis
Ashley Davidoff MD
LANGERHANS HISTIOCYTOSIS
53-year-old female with nicotine dependence presents with dyspnea and cough
CXR (PA and Lateral) shows bilateral and extensive reticular nodular changes slightly more prominent in the upper lung zones
CT scan from 16 months prior showed multiple relatively thick-walled cysts predominantly in the upper lobes. The cysts are round and air filled large and are between 5mm-8mm
CT scan 9 months later shows improvement in the thickened walls of the cysts but maintenance of diffuse cystic changes predominantly in the upper lobes
A CT scan done 2 years later shows no significant change in the diffuse bilateral cystic changes, dominant in the upper lobes and consistent with Langerhans histiocytosis
Ashley Davidoff MD

Ashley Davidoff MD

Ashley Davidoff MD
A Second Case
28 -year-old male with only minimal reported nicotine dependence presents with dyspnea and cough
CXR shows no acute cardiopulmonary disease with mild interstitial prominence
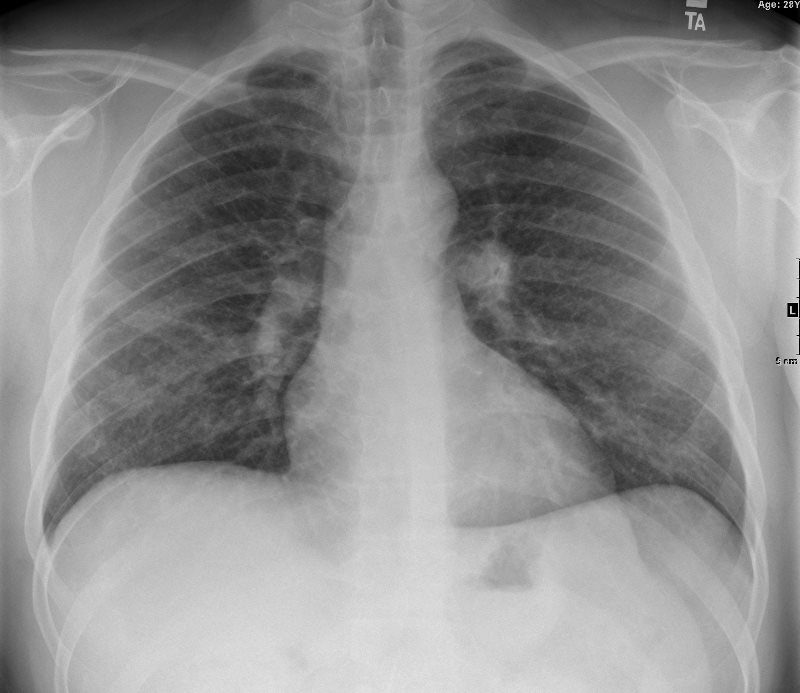
CXR shows no acute cardiopulmonary disease with mild interstitial prominence
CT scan shows multiple small cysts predominantly in the upper lobes. The cysts are round and air filled large and are between 5mm-8mm
These findings are consistent with Langerhans histiocytosis though the relatively minor smoking history was inconsistent with the diagnosis and thus the person was subjected to multicentric wedge biopsies.
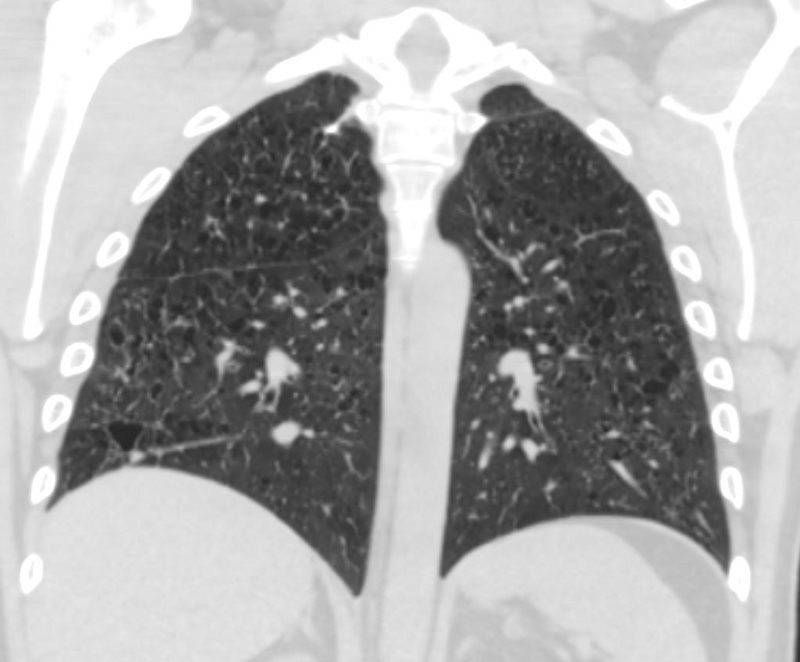
LANGERHANS HISTIOCYTOSIS
Ashley Davidoff MD
LANGERHANS HISTIOCYTOSIS
Ashley Davidoff MD
LANGERHANS HISTIOCYTOSIS
Ashley Davidoff MD
Ashley Davidoff MD
References and Links
Leatherwood D et al Pulmonary Langerhans Cell Histiocytosis RadioGraphicsVol. 27, No. 1
-
References and Links