- Buzz Words
- Allergic response
- asthma
- cystic fibrosis
- bronchiectasis
- segmental subsegmental and small airways
- Allergic response
-
Structures Involved
Bronchi and Bronchioles:
ABPA primarily affects the segmental subsegmental and small airways
Imaging Findings
- Central Bronchiectasis:
- Mucus Plugging:.
- Finger-in-Glove Sign:
- Tree-in-Bud Appearance:
- Peribronchial Infiltrates:
- Parenchymal Infiltrates:
- Atelectasis:
- Pleural Effusion:
- Pleural effusion, though less common, can occur in ABPA. It involves the accumulation of fluid in the pleural space.
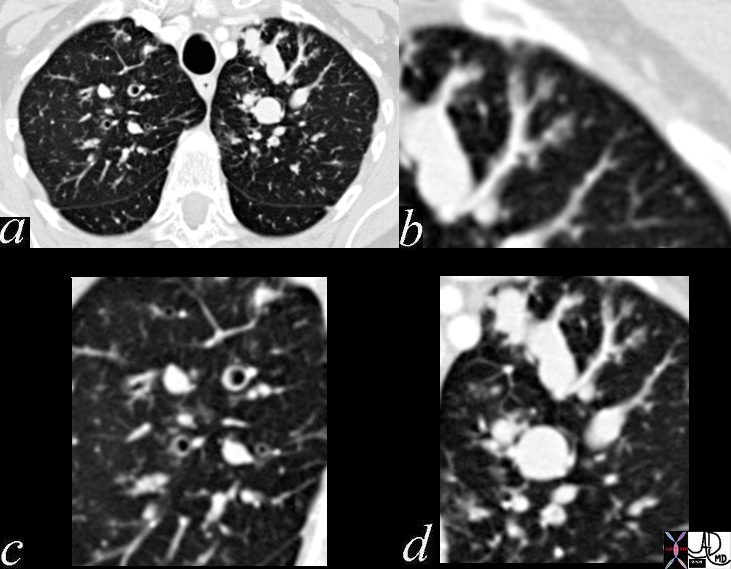
CT scan through the chest shows medium sized bronchi, bronchioles and small airways impacted with fluid. This collage is presented to reveal tree in bud changes resulting from impaction in the smaller terminal bronchioles and respiratory units. The tree-in-bud pattern also results in small centrilobular nodules connected to multiple branching linear structures of similar caliber from a single stalk. Originally it was felt to result from endobronchial spread of Mycobacterium tuberculosis, but is is now recognized in diverse entities including peripheral airway diseases caused by infection (bacterial, fungal, viral, or parasitic), congenital disorders, idiopathic disorders (obliterative bronchiolitis, pan bronchiolitis), aspiration or inhalation of foreign substances, immunologic disorders, connective tissue disorders and peripheral pulmonary vascular diseases such as neoplastic pulmonary emboli.
In this case there are also dilated medium sized airways, impacted with soft tissue characteristic of the finger in glove sign and most likely due to allergic bronchopulmonary aspergillosis (ABPA)
Ashley Davidoff MD Ashley Davidoff MD TheCommonVein.net
47113c01
- Allergic Bronchopulmonary Aspergillosis (ABPA):
- Hypersensitivity reaction to Aspergillus antigens in the airways.
- Primarily affects individuals with asthma or cystic fibrosis.
- Causes and Risk Factors:
- Exposure to Aspergillus antigens in the environment.
- Preexisting lung conditions like
- asthma or
- bronchiectasis.
- Symptoms:
- Wheezing, coughing, increased mucus production.
- Shortness of breath.
- Recurrent chest infections.
- Diagnostic Criteria:
- Clinical symptoms and history of underlying lung conditions.
- Elevated levels of specific antibodies (IgE and IgG) against Aspergillus.
- Radiological findings such as infiltrates, opacities, or bronchiectasis.
- Treatment:
- Corticosteroids to reduce inflammation and control immune response.
- Antifungal medications in some cases to target Aspergillus growth.
- Bronchodilators to relieve symptoms.
- Complications:
- Chronic inflammation can lead to lung damage and bronchiectasis.
- Recurrent exacerbations and respiratory symptoms.
- Potential progression to more severe conditions.
- Management:
- Regular monitoring of lung function and symptoms.
- Avoidance of Aspergillus exposure where possible.
- Adherence to prescribed medications and treatment plans.
- Prevention:
- Awareness of risk factors, especially in those with asthma or bronchiectasis.
ABPA and bronchiectasis
As the airways become chronically inflamed and damaged in ABPA, they can lose their structural integrity, leading to bronchiectasis. This can result in the airways becoming widened, scarred, and prone to accumulating mucus, which can lead to recurrent respiratory symptoms such as cough, sputum production, and frequent infections.
In individuals with bronchiectasis, the structural changes in the airways can disrupt the normal clearance of mucus and particles from the lungs, which can make it easier for Aspergillus antigens to accumulate and trigger an immune response. This, in turn, can lead to the characteristic symptoms of ABPA, including wheezing, coughing, increased mucus production, and occasionally fever.
while ABPA itself is an allergic response to Aspergillus, it can contribute to the development of conditions like chronic pulmonary aspergillosis (CPA) due to the underlying lung changes caused by repeated inflammation and damage.
