Human Herpes Virus 8 and primary Effusion Lymphoma (PEL)
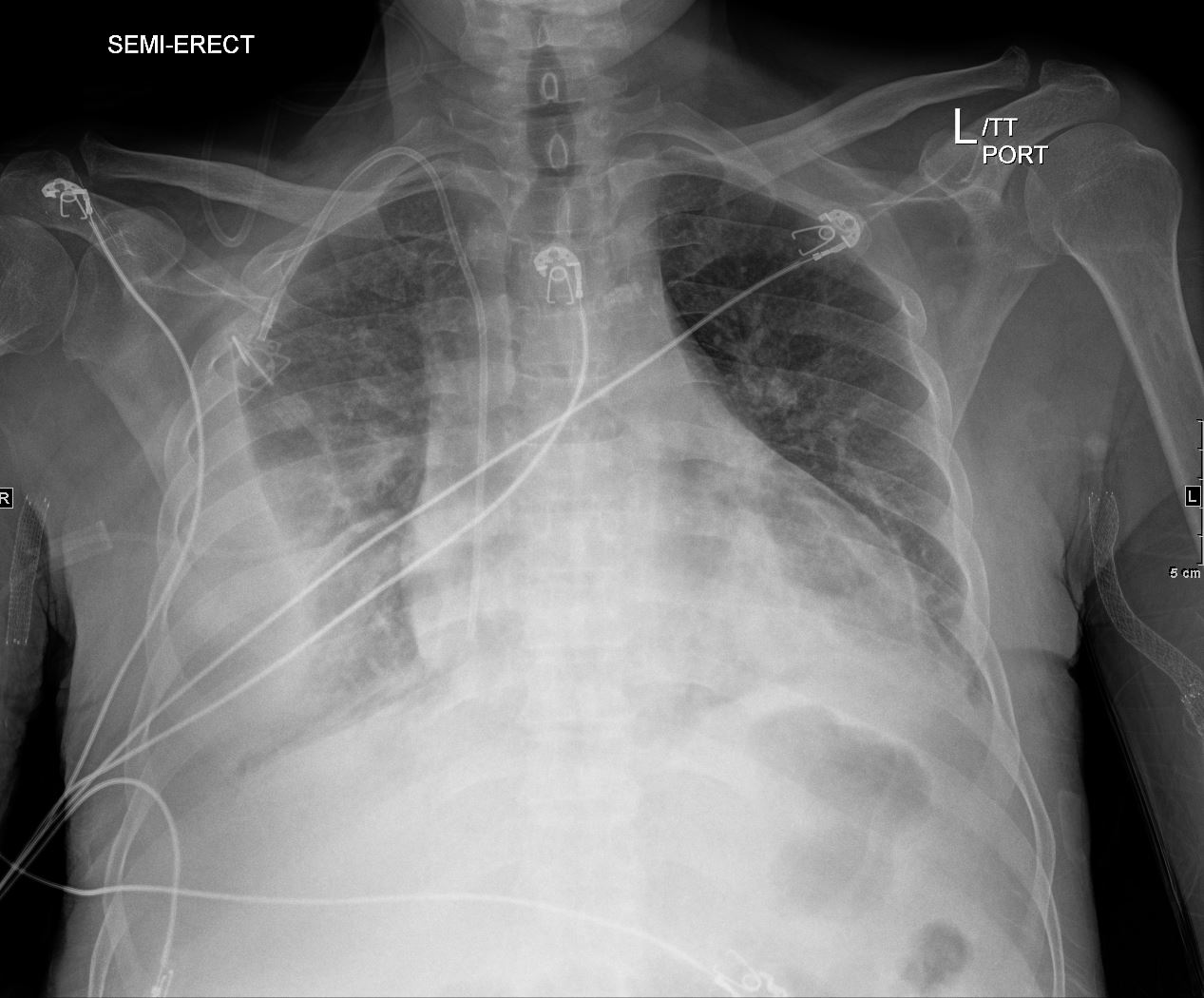
CXR of 71-year-old male shows a complex and loculated effusion on the right and a retrocardiac infiltrate on the left, The patient has known human herpes virus which has a known association with pleural lymphoma. An entity called primary effusion lymphoma (PEL) is a rapidly progressing non-Hodgkin’s B-cell lymphoma that develops in body cavities
Ashley Davidoff MD TheCommonVein.net 135683
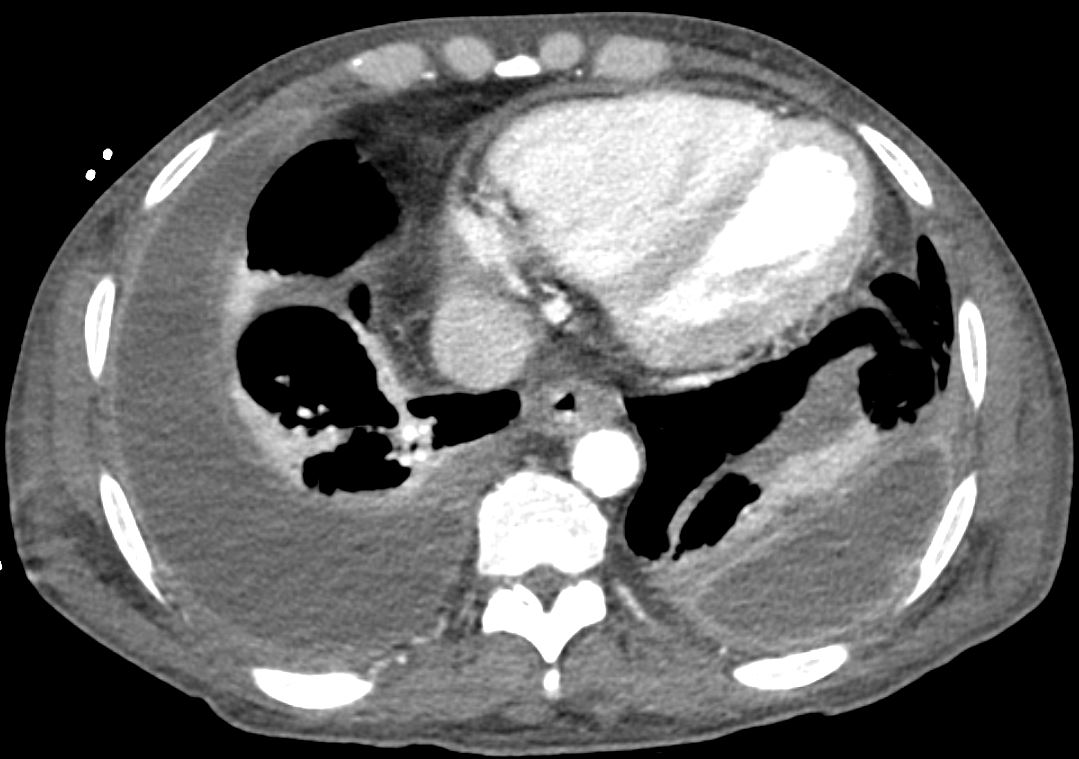
Axial CT scan with contrast of 71-year-old male shows bilateral complex and loculated effusions with thickened enhancing pleura. Pleural tap of the left effusion revealed evidence of lymphoma likely related to the patients underlying herpes virus infection. An entity called primary effusion lymphoma (PEL) is a rapidly progressing non-Hodgkin’s B-cell lymphoma that develops in body cavities
Ashley Davidoff MD TheCommonVein.net 135684
