75-year-old male with cardiomyopathy and treated for 3 months with amiodarone for atrial fibrillation and now presents with dyspnea.
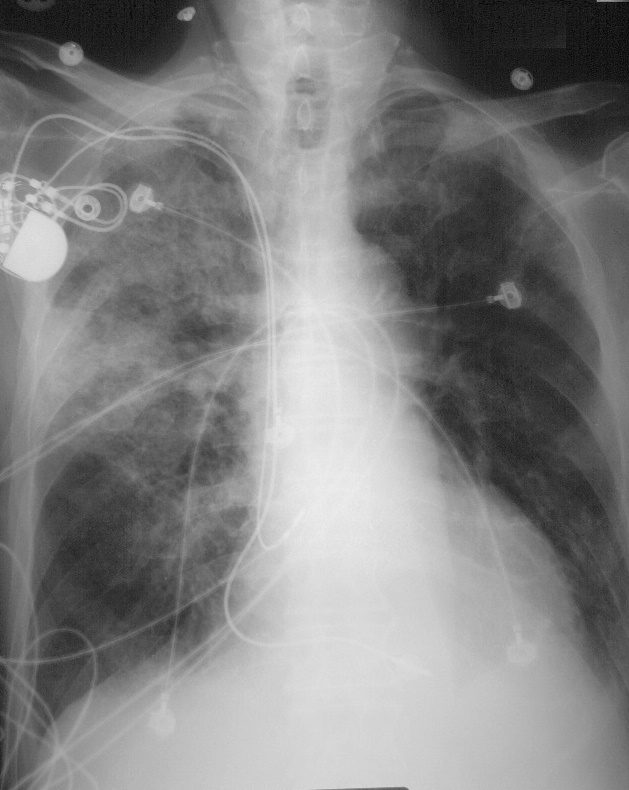
75-year-old male with cardiomyopathy and treated for 3 months with amiodarone for atrial fibrillation and now presents with dyspnea. CXR shows a prominent right upper lobe infiltrate with air bronchograms, a smaller RLL infiltrate, and no evidence of CHF
Ashley Davidoff MD TheCommonVein.278Lu 32475

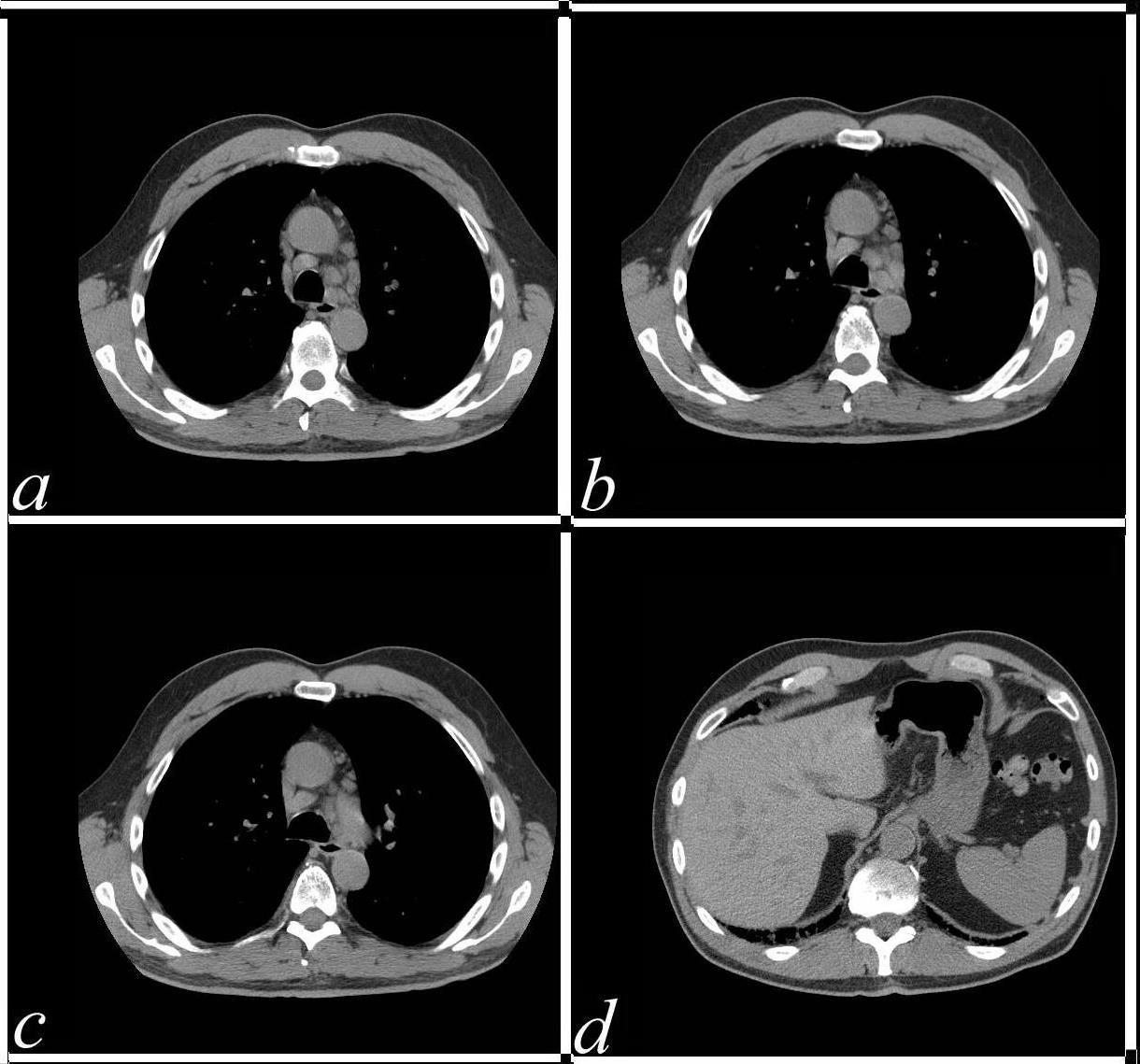
75-year-old male with cardiomyopathy atrial fibrillation and treatment with amiodarone and a RUL infiltrate thought to be related to amiodarone therapy. There was no clinical evidence nor radiological evidence of heart failure.
CT scan shows ground glass changes with multicentric crazy paving appearance that was thought to be related to amiodarone toxicity. bilateral small effusions are present, right greater than left. Following withdrawal of amiodarone and steroids administration he improved clinically and radiologically 3 months later confirming the probability of amiodarone toxicity
Ashley Davidoff MD TheCommonVein.278 Lu 32471

75-year-old male with cardiomyopathy atrial fibrillation and treatment with amiodarone and a RUL infiltrate thought to be related to amiodarone therapy.
There was no clinical evidence nor radiological evidence of heart failure.
CT scan shows ground glass changes with multicentric crazy paving appearance that was thought to be related to amiodarone toxicity.
Ashley Davidoff MD TheCommonVein.net
278 Lu 32470
CXR 6 Weeks Later
After Amiodarone Withdrawn and Treatment with Steroids
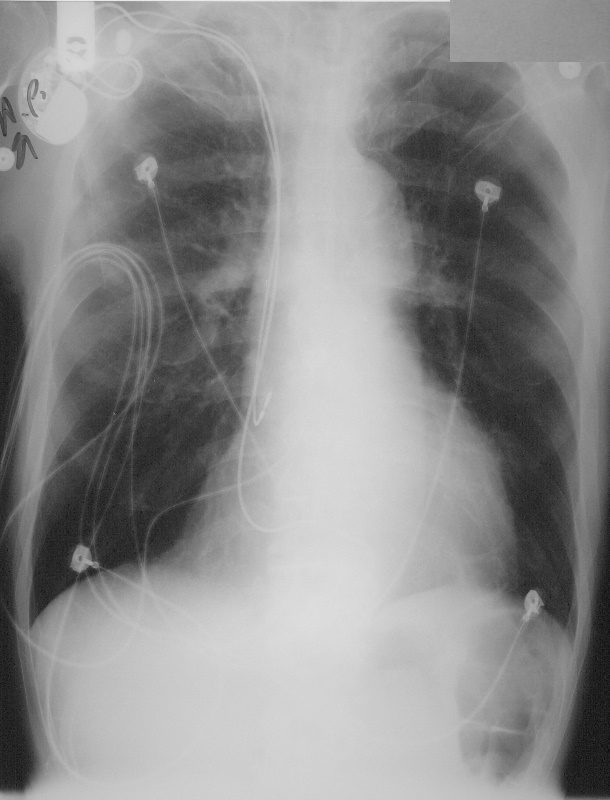
75-year-old male with cardiomyopathy atrial fibrillation and treatment with amiodarone and a RUL infiltrate thought to be related to amiodarone therapy.
CXR 6 weeks after withdrawal of amiodarone and treatment with steroids shows almost complete resolution of previously identified infiltrates. These findings are consistent with amiodarone toxicity
Ashley Davidoff MD TheCommonVein.net 278Lu 32479.8
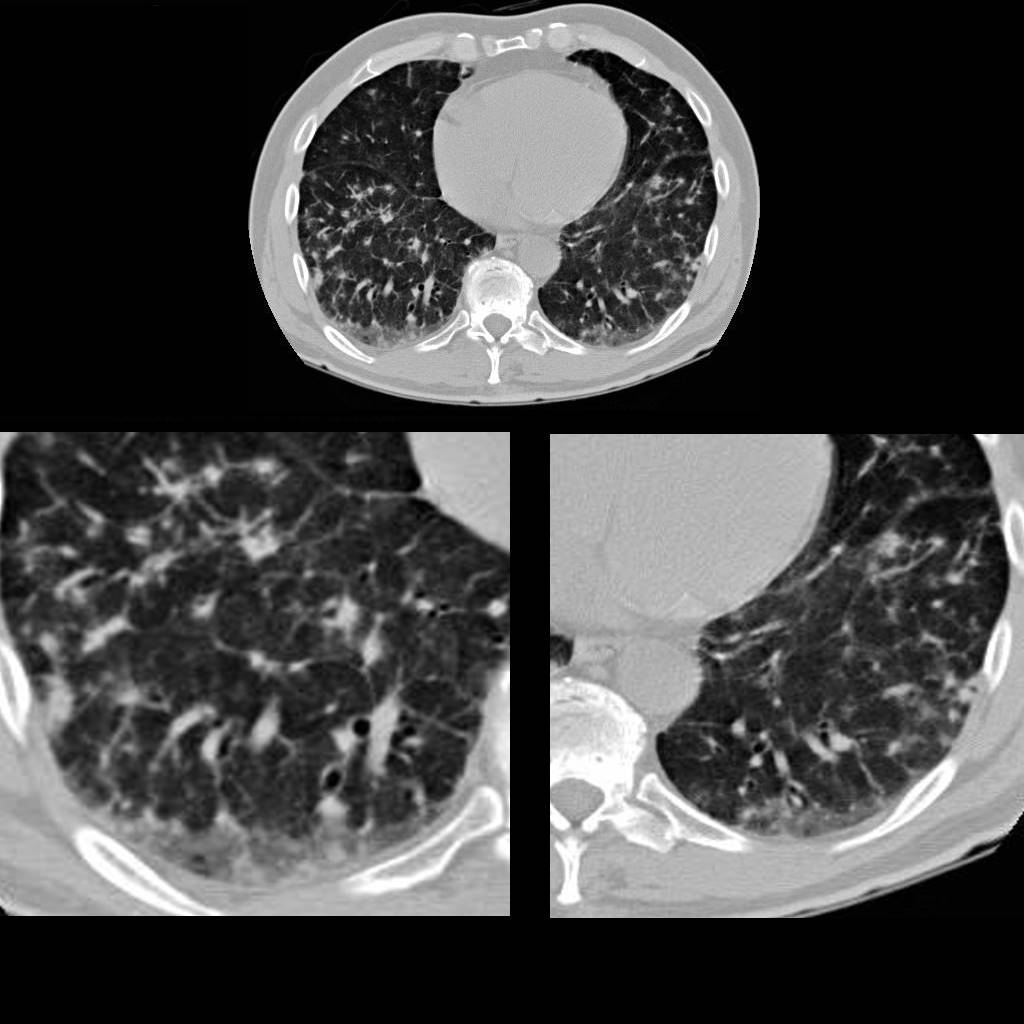
68-year-old male presented with atrial fibrillation during an acute episode of diverticulitis. He was started on amiodarone with good response. He presents 9 months later with dyspnea. CT scan in the axial plane through the lung bases show reticular changes characterised by irregular thickening of the interlobular septa, mild heterogeneous ground glass changes mosaic attenuation centrilobular nodules and bronchiolectasis suggesting a combination of small airway disease and an alveolitis with early fibrotic changes . These findings are consistent with amiodarone toxicity
Ashley Davidoff MD TheCommonVein.277Lu 37873c
68-year-old male presented with atrial fibrillation during an acute episode of diverticulitis. He was started on amiodarone with good response. He developed dyspnea 9months later and chest CT showed findings consistent with amiodarone toxicity. His abdominal CT 9 Months later shows increased density of the liver to 74HU (previously 53HU) His lymph nodes have enlarged and also show an increased density (from 52HU to 98 HU)
Ashley Davidoff MD TheCommonVein.277Lu 37851b120303d
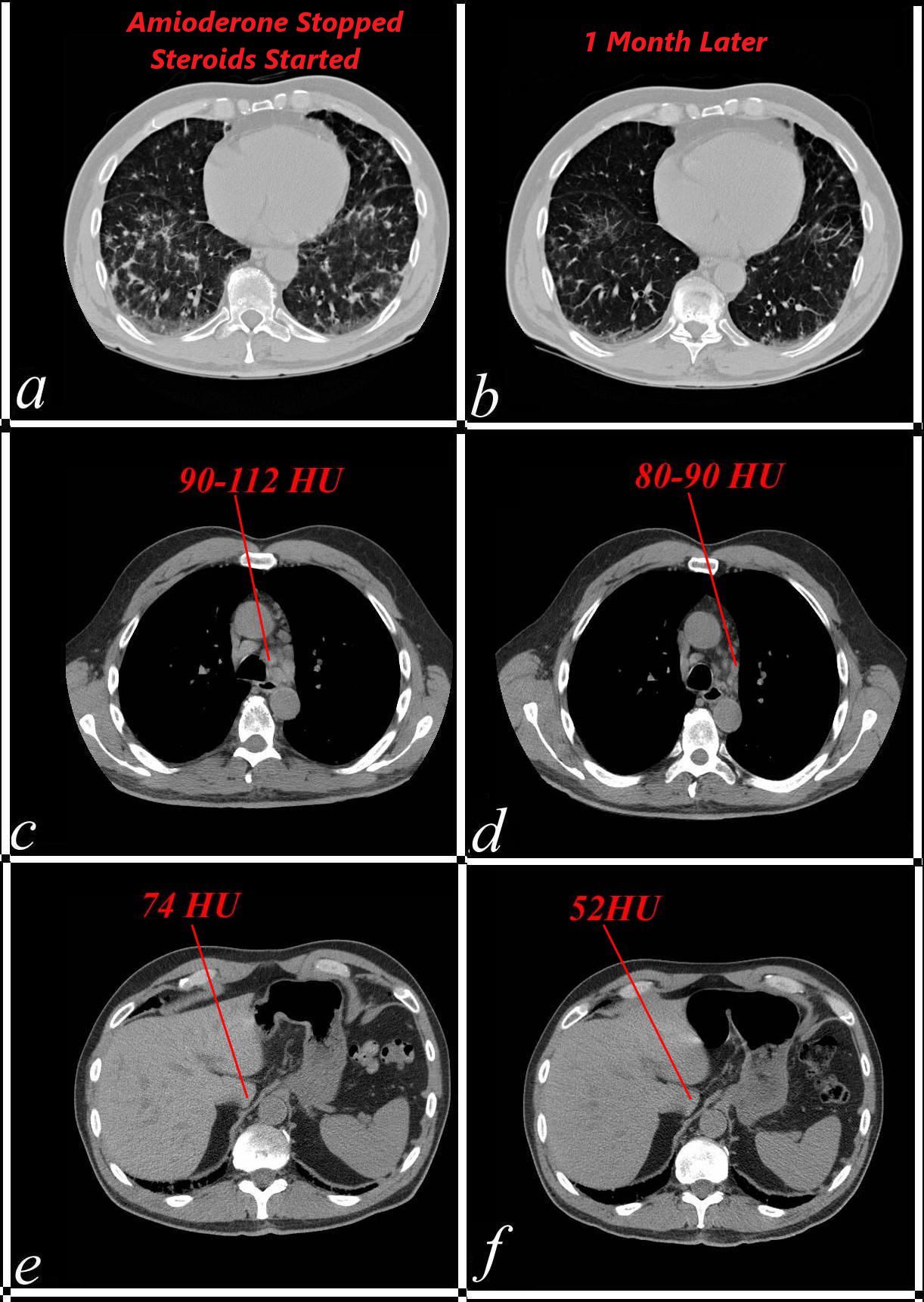
68-year-old male presented with atrial fibrillation during an acute episode of diverticulitis. He was started on amiodarone with good response. He presented 9 months later with dyspnea. At that time he had a prominent interstitial process at his lung bases consistent with amiodarone toxicity (a) with increased density in enlarged mediastinal nodes (c) and liver (e). The amiodarone was discontinued and steroids initiated. CTscan 1 month following treatment shows improvement in the bibasilar interstitial process (b) decreased size and density of the lymph nodes, (d) and normalization of the liver density (f). These findings confirm the diagnosis of amiodarone toxicity
Ashley Davidoff MD TheCommonVein.277Lu 37922c05
