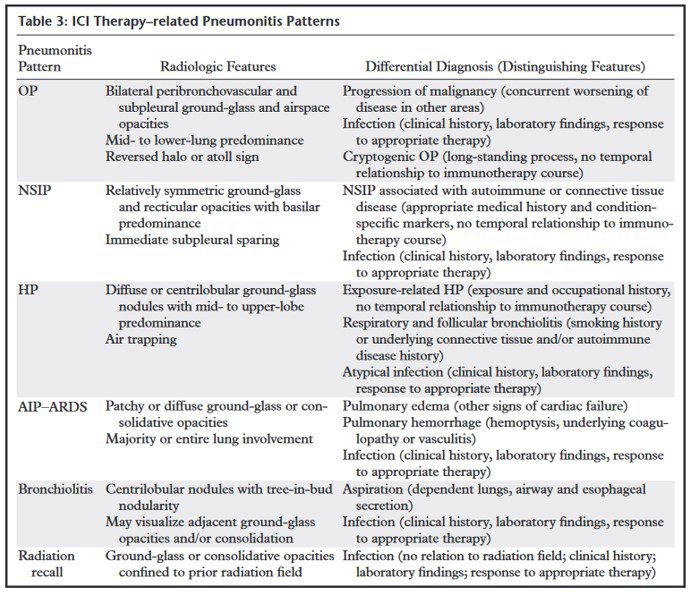
Uncommon but important complication of ICI therapy
- (a) organizing pneumonia,
- (b) nonspecific interstitial pneumonia,
- (c) hypersensitivity pneumonitis,
- (d) acute interstitial pneumonia–acute respiratory distress syndrome,
- (e) bronchiolitis, and
- (f) radiation recall pneumonitis.
Kalisz KR, Ramaiya NH, Laukamp KR, Gupta A. Immune Checkpoint Inhibitor Therapy-related Pneumonitis: Patterns and Management. Radiographics. 2019 Nov-Dec;39(7):1923-1937
PD-1 inhibitor pneumonitis: AIP/ARDS pattern in a 38-year-old woman with advanced melanoma who was treated with nivolumab. Axial (a) and coronal (b) chest CT images obtained at 15 weeks of therapy show diffuse GGOs and traction bronchiectasis, with markedly decreased lung volumes seen on the coronal image and an elevated right hemidiaphragm, findings indicative of a radiologic AIP/ARDS pattern. The patient was admitted to the intensive care unit, was treated with intravenous corticosteroids, and also required infliximab (an anti–tumor necrosis factor-α immunosuppressive agent) therapy.
Nishino, M et al Thoracic Complications of Precision Cancer Therapies: A Practical Guide for Radiologists in the New Era of Cancer Care RadioGraphicsVol. 37, No. 5

PD-1 inhibitor pneumonitis: AIP/ARDS pattern in a 38-year-old woman with advanced melanoma who was treated with nivolumab. Axial (a) and coronal (b) chest CT images obtained at 15 weeks of therapy show diffuse GGOs and traction bronchiectasis, with markedly decreased lung volumes seen on the coronal image and an elevated right hemidiaphragm, findings indicative of a radiologic AIP/ARDS pattern. The patient was admitted to the intensive care unit, was treated with intravenous corticosteroids, and also required infliximab (an anti–tumor necrosis factor-α immunosuppressive agent) therapy.
Nishino, M et al Thoracic Complications of Precision Cancer Therapies: A Practical Guide for Radiologists in the New Era of Cancer Care RadioGraphicsVol. 37, No. 5
Nishino, M et al Thoracic Complications of Precision Cancer Therapies: A Practical Guide for Radiologists in the New Era of Cancer Care RadioGraphicsVol. 37, No. 5
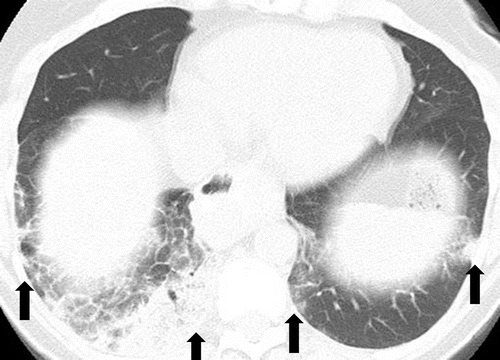
Pneumonitis with AIP/ARDS pattern in a 70-year-old man with melanoma who was treated with sequentially administered nivolumab and ipilimumab combination therapy. Axial chest CT images obtained at 5.6 months of therapy (a at the level of the carina; b at a lower level than a) show GGOs, reticular opacities, consolidation, and traction bronchiectasis, as well as pleural effusions (*) involving both lungs. (Figure reprinted from reference 7.)
Nishino, M et al Thoracic Complications of Precision Cancer Therapies: A Practical Guide for Radiologists in the New Era of Cancer Care RadioGraphicsVol. 37, No. 5
PD-1 inhibitor pneumonitis: NSIP pattern in a 58-year-old man with advanced melanoma who was treated with nivolumab. Axial chest CT image obtained at 7 weeks of therapy shows GGOs and reticular opacities in a subpleural distribution, representing an NSIP pattern of PD-1 inhibitor pneumonitis. * = metastatic lesion in the lung.
Nishino, M et al Thoracic Complications of Precision Cancer Therapies: A Practical Guide for Radiologists in the New Era of Cancer Care RadioGraphicsVol. 37, No. 5

PD-1 inhibitor pneumonitis: COP pattern in a 69-year-old man with advanced NSCLC who was treated with nivolumab. At 6 months of therapy, the patient presented with increased shortness of breath and cough, without fever. Axial chest CT image shows multifocal areas of consolidation and GGOs in a predominantly peripheral and basilar distribution (arrows), representing a COP pattern of PD-1 inhibitor–related pneumonitis. Bronchial dilatation was noted within the areas of consolidation. Nivolumab was withheld, and the patient was treated with corticosteroids, with subsequent improvement.
Nishino, M et al Thoracic Complications of Precision Cancer Therapies: A Practical Guide for Radiologists in the New Era of Cancer Care RadioGraphicsVol. 37, No. 5
a- PD-1 inhibitor pneumonitis: Hypersensitivity pneumonitis pattern in a 68-year-old man with metastatic renal cell carcinoma who was treated with nivolumab and presented with a new cough at 6 months of therapy. (a) Axial chest CT image shows new multifocal GGOs in a centrilobular distribution throughout both lungs and mosaic attenuation, findings that represent pneumonitis with a hypersensitivity pneumonitis pattern. Nivolumab therapy was withheld, and the patient underwent corticosteroid therapy.
Nishino, M et al Thoracic Complications of Precision Cancer Therapies: A Practical Guide for Radiologists in the New Era of Cancer Care RadioGraphicsVol. 37, No. 5
b
Axial follow-up CT image obtained after 1 month of corticosteroid therapy shows marked improvement of pneumonitis and resolution of GGOs. Nivolumab continued to be withheld, and corticosteroid therapy was tapered. At 1.5 months after completing the corticosteroid taper, without restarting nivolumab or any other systemic therapy, the patient experienced a worsening cough.
Nishino, M et al Thoracic Complications of Precision Cancer Therapies: A Practical Guide for Radiologists in the New Era of Cancer Care RadioGraphicsVol. 37, No. 5
a
PD-1 inhibitor pneumonitis flare in a 72-year-old man with stage IV squamous NSCLC who was treated with nivolumab and presented with progressive dyspnea with cough and wheezing but no fever. (a) Axial chest CT image at 15 weeks of therapy demonstrates multifocal areas of GGOs, reticular opacities, and consolidation (arrows) involving all lobes, as well as centrilobular nodularity and traction bronchiectasis in a predominantly peripheral distribution. The overall features demonstrate a COP pattern. The patient was treated with prednisone for pneumonitis.
Nishino, M et al Thoracic Complications of Precision Cancer Therapies: A Practical Guide for Radiologists in the New Era of Cancer Care RadioGraphicsVol. 37, No. 5

b
Axial follow-up CT image after 4 weeks of prednisone therapy shows a significant decrease in the findings, with residual GGOs. Note the “reversed halo” sign manifesting as a central GGO surrounded by a crecent-shaped dense airspace consolidation (arrow), a finding that has been reported as a radiologic manifestation of COP. (c) Axial CT image obtained 4 weeks after the completion of prednisone therapy shows the development of a bilateral dense consolidation with GGOs and reticular opacities (arrows) in peripheral and multifocal distributions, again demonstrating a COP pattern as noted during the first episode of PD-1 inhibitor pneumonitis. Given the similarity of the radiologic and clinical manifestations to those of the first episode, the patient restarted prednisone for treatment of pneumonitis flare. Follow-up chest CT images obtained 2 weeks after starting the second course of prednisone therapy (not shown) demonstrated a decrease in the findings, indicative of improving pneumonitis in response to corticosteroid therapy. (Figure 7 reprinted from reference 21.)
Nishino, M et al Thoracic Complications of Precision Cancer Therapies: A Practical Guide for Radiologists in the New Era of Cancer Care RadioGraphicsVol. 37, No. 5

a
PD-1 inhibitor pneumonitis flare in a 72-year-old man with stage IV squamous NSCLC who was treated with nivolumab and presented with progressive dyspnea with cough and wheezing but no fever. (a) Axial chest CT image at 15 weeks of therapy demonstrates multifocal areas of GGOs, reticular opacities, and consolidation (arrows) involving all lobes, as well as centrilobular nodularity and traction bronchiectasis in a predominantly peripheral distribution. The overall features demonstrate a COP pattern. The patient was treated with prednisone for pneumonitis.
Nishino, M et al Thoracic Complications of Precision Cancer Therapies: A Practical Guide for Radiologists in the New Era of Cancer Care RadioGraphicsVol. 37, No. 5
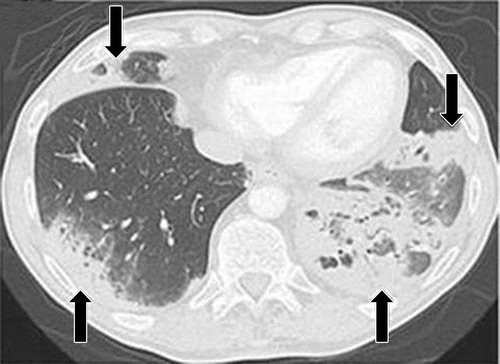
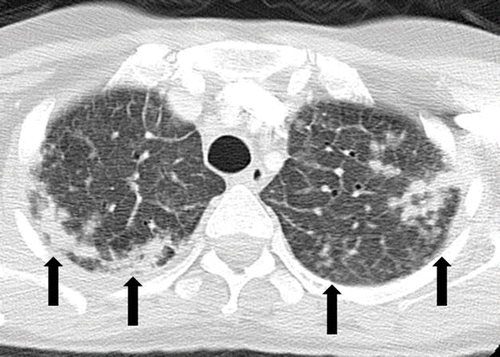
Pneumonitis in a 71-year-old man with metastatic renal cell carcinoma treated with temsirolimus. Axial CT image at 4 weeks of therapy shows multifocal GGOs and reticular opacities in a predominantly peripheral and basilar distribution (arrows), findings that represent mTOR inhibitor–related pneumonitis. The patient was symptomatic and was switched to an alternate therapy.
Nishino, M et al Thoracic Complications of Precision Cancer Therapies: A Practical Guide for Radiologists in the New Era of Cancer Care RadioGraphicsVol. 37, No. 5
Pneumonitis in a 66-year-old woman with Waldenström macroglobulinemia treated with mTOR inhibitor therapy. Axial CT image at 6 months of therapy shows consolidation, GGOs, and reticular opacities (arrows) that represent a COP pattern.
Nishino, M et al Thoracic Complications of Precision Cancer Therapies: A Practical Guide for Radiologists in the New Era of Cancer Care RadioGraphicsVol. 37, No. 5
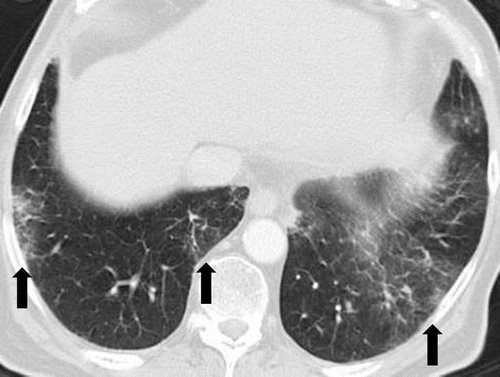
Pneumonitis in a 42-year-old man with an EGFR exon 19 deletion mutation who was treated with erlotinib in the United States. Axial chest CT images (b obtained at a lower level than a) obtained at 8 weeks of therapy show multifocal areas of GGOs in both lungs, findings that represent pneumonitis. Note the absence of traction bronchietasis or volume loss.
Nishino, M et al Thoracic Complications of Precision Cancer Therapies: A Practical Guide for Radiologists in the New Era of Cancer Care RadioGraphicsVol. 37, No. 5
Pneumonitis in a 42-year-old man with an EGFR exon 19 deletion mutation who was treated with erlotinib in the United States. Axial chest CT images (b obtained at a lower level than a) obtained at 8 weeks of therapy show multifocal areas of GGOs in both lungs, findings that represent pneumonitis. Note the absence of traction bronchietasis or volume loss.
Nishino, M et al Thoracic Complications of Precision Cancer Therapies: A Practical Guide for Radiologists in the New Era of Cancer Care RadioGraphicsVol. 37, No. 5
Nishino, M et al Thoracic Complications of Precision Cancer Therapies: A Practical Guide for Radiologists in the New Era of Cancer Care RadioGraphicsVol. 37, No. 5
ALK inhibitor–related pneumonitis in a 55-year-old woman with ALK-positive stage IV adenocarcinoma of the lung. The patient experienced disease progression while taking a first-generation ALK inhibitor (crizotinib) and was then treated with a second-generation ALK inhibitor (ceritinib). She presented with an increasing dry cough and dyspnea at 7 months of ceritinib therapy. (a, b) Axial (a) and coronal (b) CT images show biapical consolidation and GGOs in both upper lobes (arrows) in a striking peripheral distribution, indicative of a COP pattern.
Nishino, M et al Thoracic Complications of Precision Cancer Therapies: A Practical Guide for Radiologists in the New Era of Cancer Care RadioGraphicsVol. 37, No. 5

ALK inhibitor–related pneumonitis in a 55-year-old woman with ALK-positive stage IV adenocarcinoma of the lung. The patient experienced disease progression while taking a first-generation ALK inhibitor (crizotinib) and was then treated with a second-generation ALK inhibitor (ceritinib). She presented with an increasing dry cough and dyspnea at 7 months of ceritinib therapy. (a, b) Axial (a) and coronal (b) CT images show biapical consolidation and GGOs in both upper lobes (arrows) in a striking peripheral distribution, indicative of a COP pattern.
Nishino, M et al Thoracic Complications of Precision Cancer Therapies: A Practical Guide for Radiologists in the New Era of Cancer Care RadioGraphicsVol. 37, No. 5
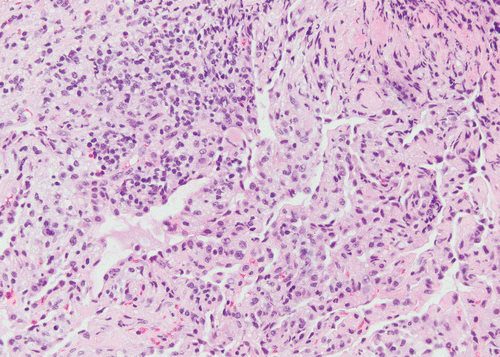
c
(c, d) Photomicrographs from transbronchial lung biopsy specimen show organizing interstitial pneumonia characterized by alveolar interstitial widening by lymphocytic infiltrates, increased extracellular matrix material, reactive pneumocyte hyperplasia, scattered eosinophils (arrow in d), and numerous airspace foamy macrophages. There was no evidence of tumor in the biopsy specimen. (Hematoxylin-eosin stain; original magnification, ×200 in c, ×400 in d.)
Nishino, M et al Thoracic Complications of Precision Cancer Therapies: A Practical Guide for Radiologists in the New Era of Cancer Care RadioGraphicsVol. 37, No. 5
Pneumonitis in a 62-year-old woman with advanced pancreatic neuroendocrine tumor treated with everolimus and temozolomide. Axial CT image obtained at 10.3 months of therapy shows diffuse bilateral GGOs and reticular opacities that are indicative of a hypersensitivity pneumonitis pattern. The patient had mild shortness of breath and was treated with prednisone.
Nishino, M et al Thoracic Complications of Precision Cancer Therapies: A Practical Guide for Radiologists in the New Era of Cancer Care RadioGraphicsVol. 37, No. 5
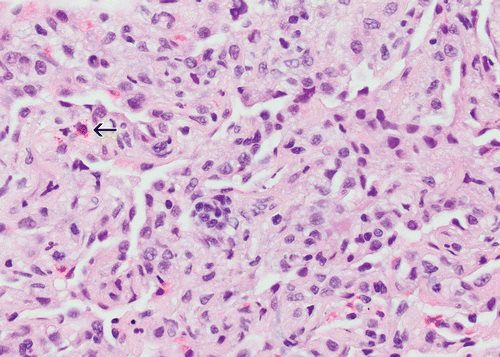
d
(c, d) Photomicrographs from transbronchial lung biopsy specimen show organizing interstitial pneumonia characterized by alveolar interstitial widening by lymphocytic infiltrates, increased extracellular matrix material, reactive pneumocyte hyperplasia, scattered eosinophils (arrow in d), and numerous airspace foamy macrophages. There was no evidence of tumor in the biopsy specimen. (Hematoxylin-eosin stain; original magnification, ×200 in c, ×400 in d.)
Nishino, M et al Thoracic Complications of Precision Cancer Therapies: A Practical Guide for Radiologists in the New Era of Cancer Care RadioGraphicsVol. 37, No. 5

Pneumonitis in a 65-year-old man with diffuse large B-cell lymphoma after three cycles of rituximab with cyclophosphamide, doxorubicin hydrochloride, vincristine sulfate, and prednisone (R-CHOP) therapy who presented with new shortness of breath. Axial CT image shows bilateral diffuse GGOs and areas of consolidation in both lungs, with traction bronchiectasis and loss of lung volumes. The findings reflect an AIP/ARDS pattern of pneumonitis related to rituximab. Bilateral pleural effusions were also present. The patient’s condition significantly deteriorated, and he died 1 month after presentation. Autopsy results showed diffuse alveolar damage in the lungs.
Nishino, M et al Thoracic Complications of Precision Cancer Therapies: A Practical Guide for Radiologists in the New Era of Cancer Care RadioGraphicsVol. 37, No. 5
a)
Sarcoid-like lymphadenopathy in an asymptomatic 81-year-old man with metastatic melanoma treated with ipilimumab. (a) Coronal contrast-enhanced reformatted chest CT image obtained 4.9 months after the initiation of ipilimumab therapy shows new bilateral symmetric mediastinal and hilar lymphadenopathy (arrows) resembling findings of sarcoidosis.
Nishino, M et al Thoracic Complications of Precision Cancer Therapies: A Practical Guide for Radiologists in the New Era of Cancer Care RadioGraphicsVol. 37, No. 5
ial CT image shows bilateral irregular and nodular parenchymal opacities (arrows) with upper- and middle-lung predominance and peribronchovascular involvement. The findings fall in the spectrum of lung parenchymal manifestations of pulmonary sarcoidosis. (Figure reprinted from reference 16.)
Nishino, M et al Thoracic Complications of Precision Cancer Therapies: A Practical Guide for Radiologists in the New Era of Cancer Care RadioGraphicsVol. 37, No. 5

Sarcoid-like granulomatosis of the lung in an asymptomatic 75-year-old man with metastatic melanoma treated with pembrolizumab. (a) Axial CT image shows a parenchymal conglomerate opacity in the right lower lobe of the lung (arrow), which had been gradually increasing over time on serial scans obtained during therapy. Note that the patient had a previous left pneumonectomy.
Nishino, M et al Thoracic Complications of Precision Cancer Therapies: A Practical Guide for Radiologists in the New Era of Cancer Care RadioGraphicsVol. 37, No. 5
Photomicrograph of specimen from a lung core biopsy of the right lower lobe lesion shows a sarcoid-like reaction characterized by interstitial nonnecrotizing granulomas (arrows) with associated lymphocytic infiltrates. (Hematoxylin-eosin stain; original magnification, ×200.). Gram, silver, and acid-fast bacilli stains (not shown) were negative for microorganisms.
Nishino, M et al Thoracic Complications of Precision Cancer Therapies: A Practical Guide for Radiologists in the New Era of Cancer Care RadioGraphicsVol. 37, No. 5
Links and References
Checkpoint Inhibitor Therapy-related Pneumonitis:
Kalisz KR, Ramaiya NH, Laukamp KR, Gupta A. Immune Checkpoint Inhibitor Therapy-related Pneumonitis: Patterns and Management. Radiographics. 2019 Nov-Dec;39(7):1923-1937
