In a Nutshell
- Lymphoid Tissue
- Granuloma
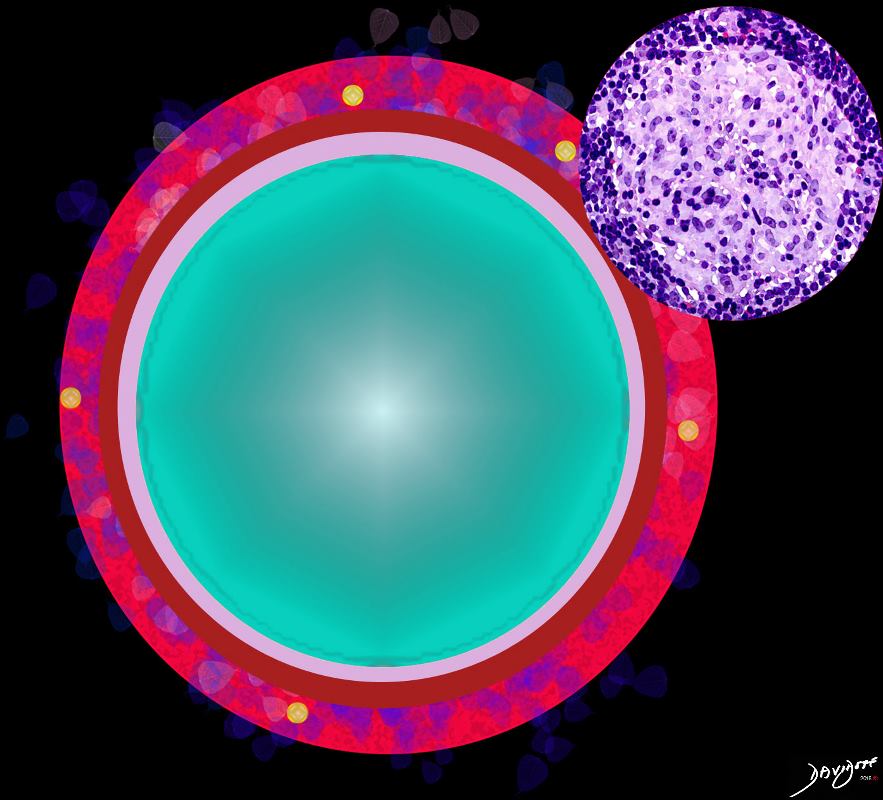
Normal Lymphoid Tissue
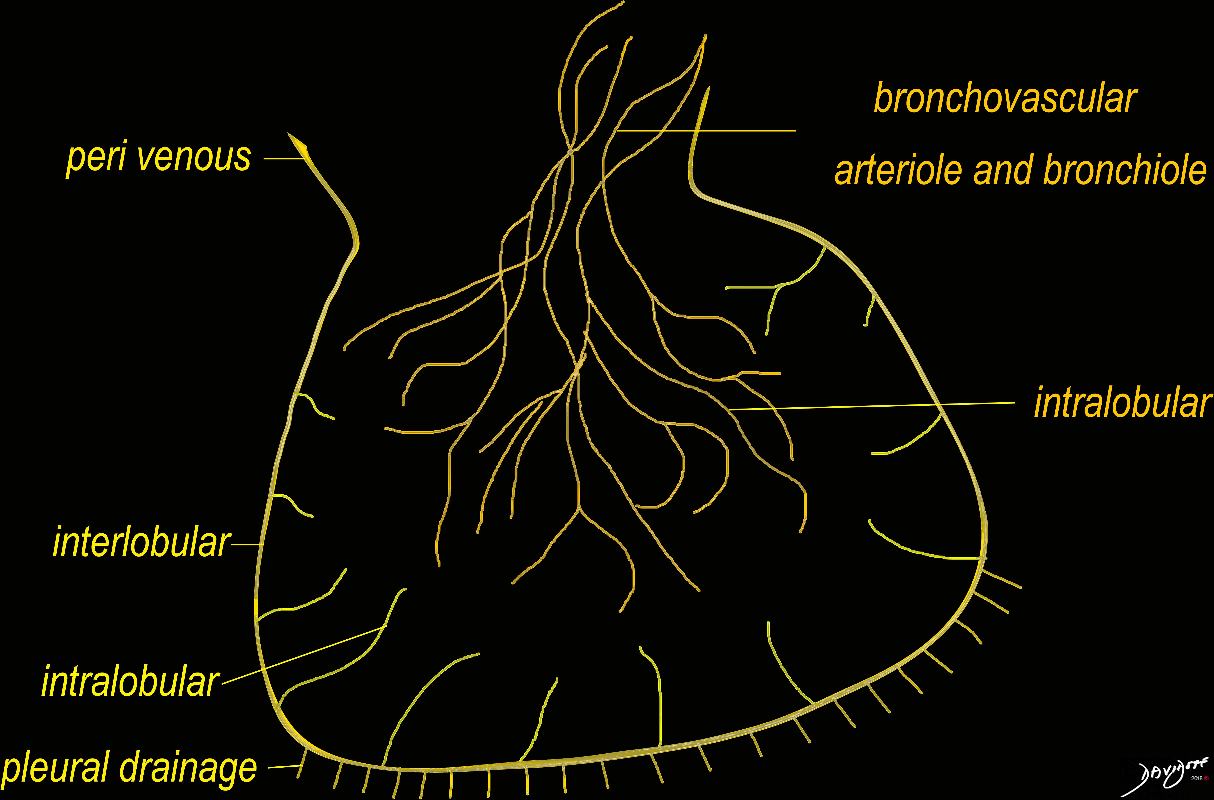
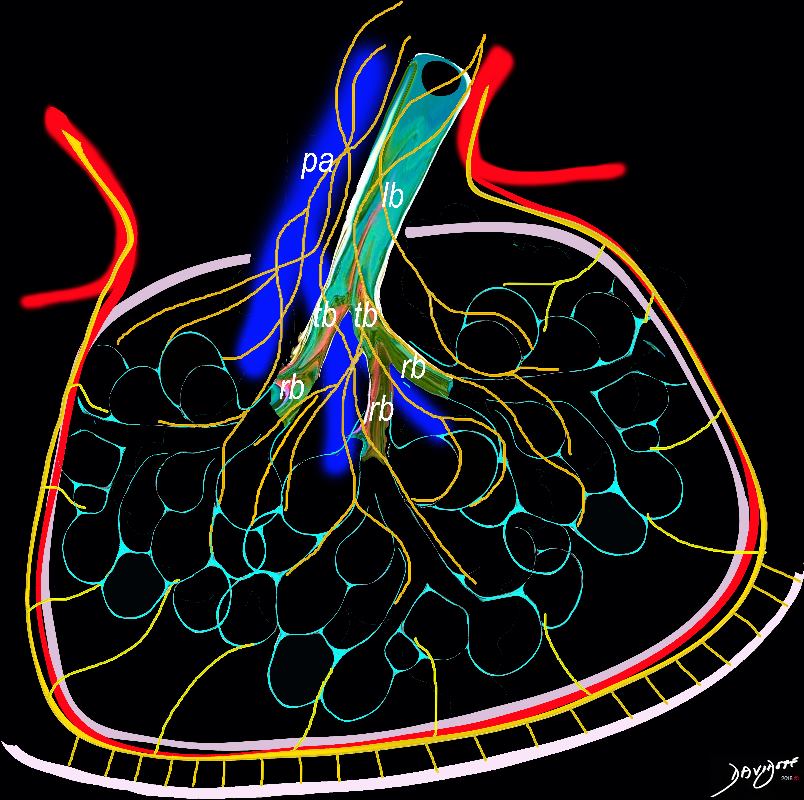
The diagram shows the 2 systems of lymphatic drainage at the level of the secondary lobule. The superficial system drains some of the interstitium of the secondary lobule, runs in the interlobular septa and drains all the pleura. Thee pathway to the lymph nodes in the mediastinum is via the pulmonary veins. The deeper system drains the interstitium in the interalveolar septa, and then they travel along the bronchovascular bundle accompanying the bronchi and pulmonary artery and into the lymph nodes of the hila and mediastinum
Ashley Davidoff MD TheCommonVein.net lungs-0767
Granuloma Distribution
Ashley Davidoff MD The CommonVein.net lungs-0766
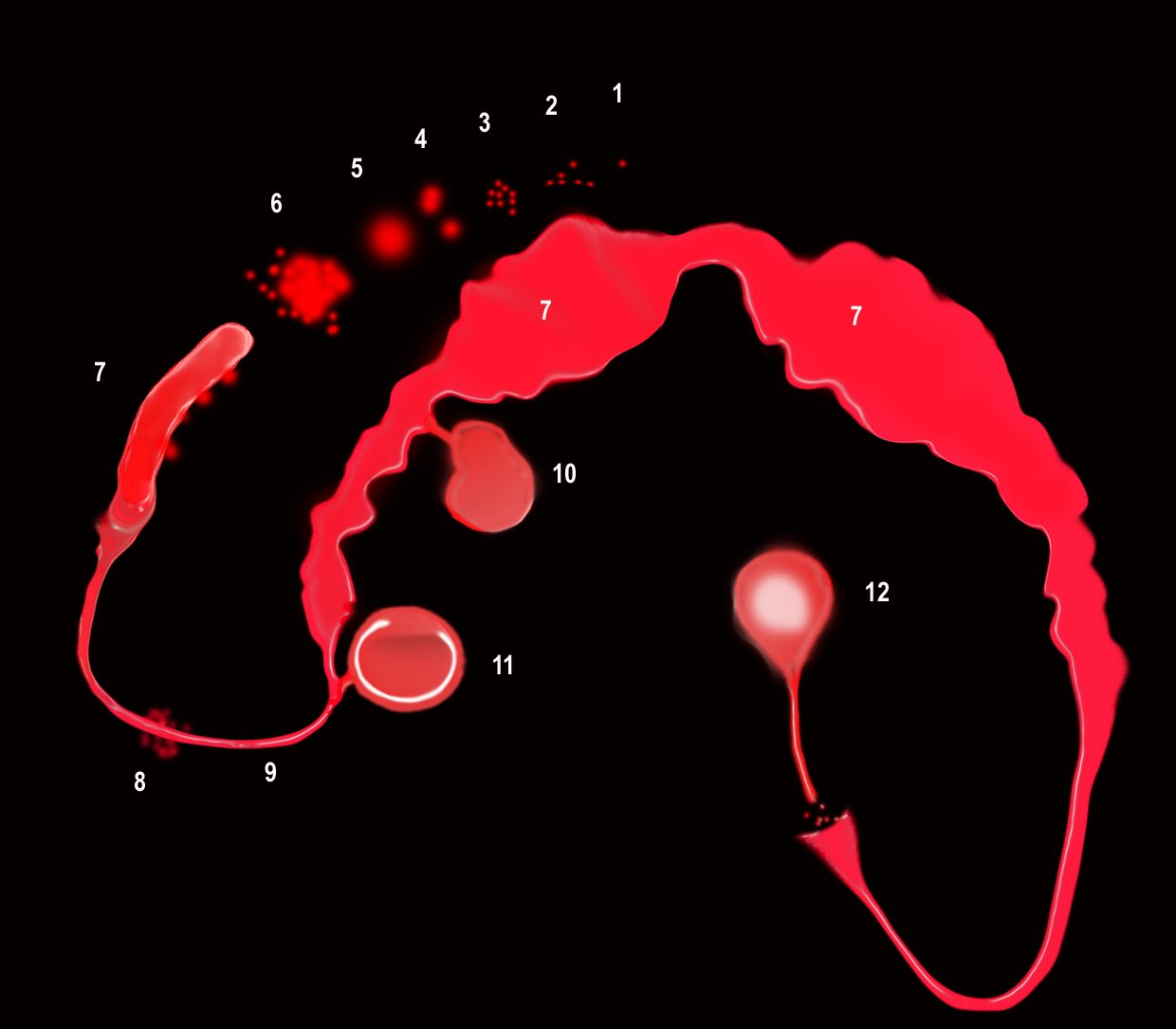
“S” of SARCOIDOSIS
The granulomas start as micronodules in close association with the lymphatics (1) spread in the intralobular septa and centrilobular bronchioles ((2) cluster and conglomerate to form macro nodules (4,5) sometimes manifesting as the galaxy sign (6). As they cluster and conglomerate they can cause conglomerate masses along the pathway (7) most commonly centrally as the lymphatics become confluent in the hila (7)
The lymphovascular bundles may be accompanied by nodularity (8) or just by thickening (9).
The lymph nodes in the mediastinum become significantly enlarged and fleshy (10). They often calcify (12) sometimes on the calcify on the rim of the node (eggshell calcification (11)
Sarcoidosis is a nodular granulomatous disease which predominated in the upper lobes and has its epicenter in the lymphoid tissue of the lungs.
The “S” drawn on the thoracic cage outlines the lymphatic distribution of the lungs, starting in the pleura involving the lymphatic system in the pleura, interlobular septa, bronchovascular bundles and lymph nodes.
The granulomas start out as micronodules and there is a tendency for these to coalesce, sometimes forming large granulomatous masses
When the disease affects the interlobular septa, it causes thickening and nodularity in the septa of the secondary lobule.
When it involves the lymphatics in the pleura or fissures it causes nodularity and thickening.
When it involves the lymphatics around the terminal bronchioles it results in centrilobular micronodules, and when it involves the larger airways it causes thickening and nodularity
Lymph nodes in the hila are characteristically large and flesh like (sarcoid = meat) The Pawnbrokers sign (aka Garland sign or the 1,2,3 sign) describes the enlarged right paratracheal node with bilateral hilar adenopathy.
Parenchymal nodules and micronodules sometimes coalesce to form a central confluent mass with surrounding micronodules, described as the galaxy sign.
Ashley Davidoff MD
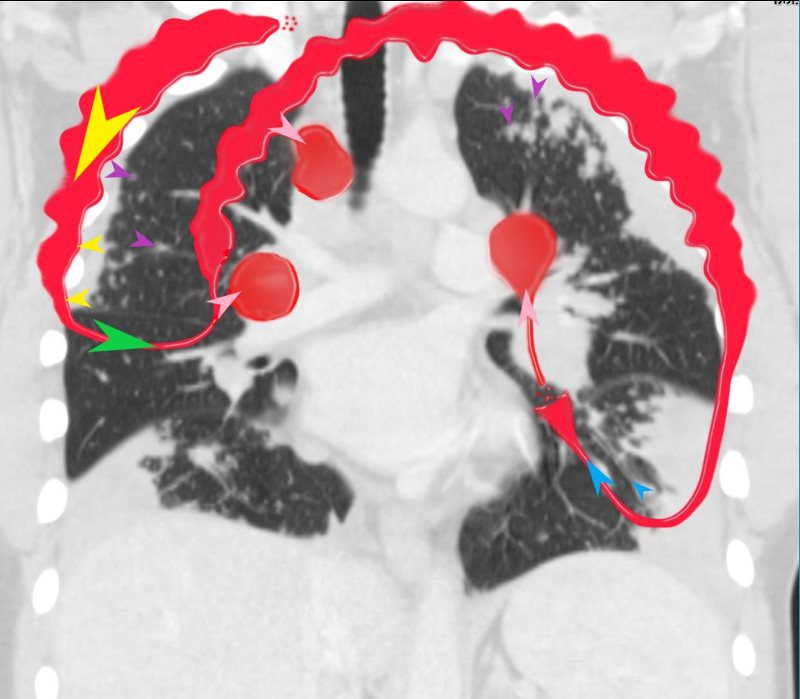
“S” of SARCOIDOSIS
In this diagram the arrows show the direction of flow of the lymphatics. Pleural lymphatics (yellow arrows), Fissural lymphatics, green arrows), flow from the interlobular septa (purple arrows) and along the bronchovascular bundles (blue arrows) all flow toward the lymph nodes in the hila and mediastinum (pink arrows).
Sarcoidosis is a nodular granulomatous disease which predominated in the upper lobes and has its epicenter in the lymphoid tissue of the lungs.
The “S” drawn on the thoracic cage outlines the lymphatic distribution of the lungs, starting in the pleura involving the lymphatic system in the pleura, interlobular septa, bronchovascular bundles and lymph nodes.
The granulomas start out as micronodules and there is a tendency for these to coalesce, sometimes forming large granulomatous masses
When the disease affects the interlobular septa, it causes thickening and nodularity in the septa of the secondary lobule.
When it involves the lymphatics in the pleura or fissures it causes nodularity and thickening.
When it involves the lymphatics around the terminal bronchioles it results in centrilobular micronodules, and when it involves the larger airways it causes thickening and nodularity
Lymph nodes in the hila are characteristically large and flesh like (sarcoid = meat) The Pawnbrokers sign (aka Garland sign or the 1,2,3 sign) describes the enlarged right paratracheal node with bilateral hilar adenopathy.
Parenchymal nodules and micronodules sometimes coalesce to form a central confluent mass with surrounding micronodules, described as the galaxy sign.
Ashley Davidoff MD
Pleura and Fissures
SARCOIDOSIS, ACTIVE – ALVEOLAR FORM
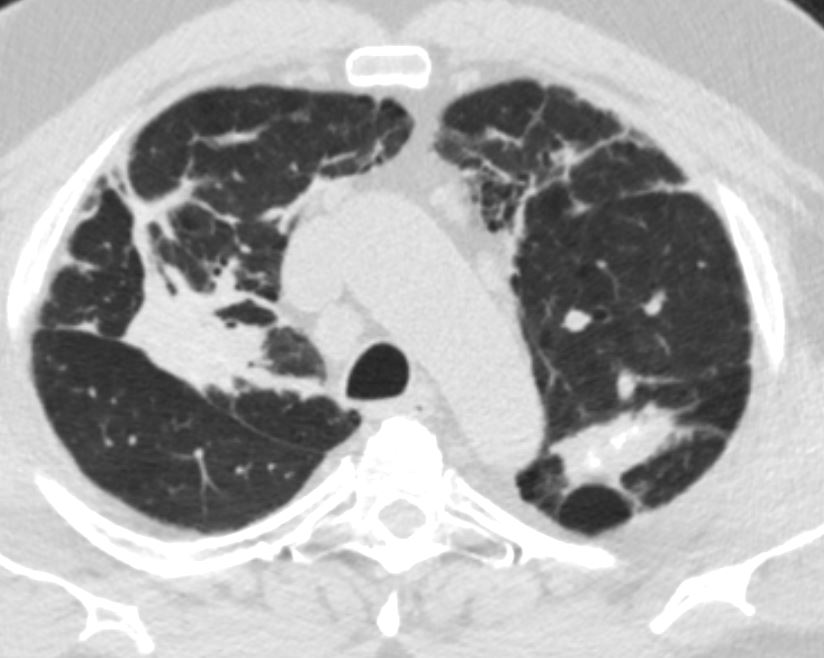
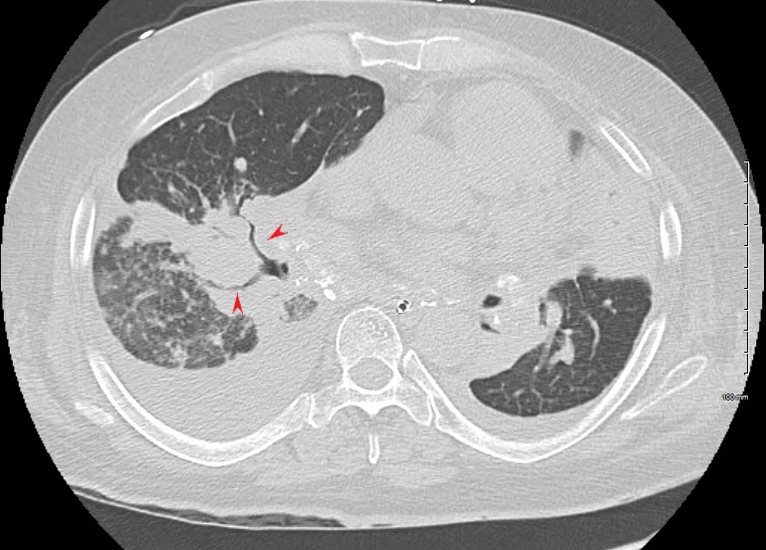
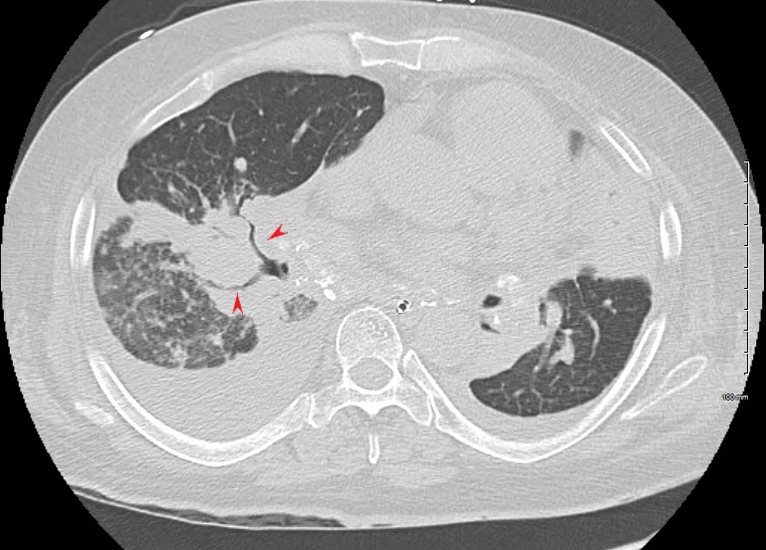
48-year-old previously well presented with dyspnea and initial CXR showed an infiltrate at the right base, and clinically resolved. He presented a year later with right chest pain and low grade ever and the CXR showed patchy opacities in the LUL and in the RLL
A subsequent CT showed LUL nodular opacities and subpleural rim of consolidation in the LUL and more prominently at both lung bases, associated with significant mediastinal adenopathy. Lympho-vascular nodularity was noted in the bronchovascular bundles as well as in the interlobular septa, consistent with sarcoidosis
CXR and CT 4 years later showed almost complete resolution of the parenchymal findings and the CT findings except for minimal reticulation and scarring in the subpleural regions
Ashley Davidoff MD
SARCOIDOSIS, ACTIVE – ALVEOLAR FORM
CXR and CT 4 years later showed almost complete resolution of the parenchymal findings and the CT findings except for minimal reticulation and scarring in the subpleural regions
Ashley Davidoff MD
Ashley Davidoff MD

CT WITH SUBPLEURAL NODULES AND MULTIPLE VARIABLY SIZED LEFT APICAL SOLID NODULES
Ashley Davidoff MD
Ashley Davidoff MD
Bronchovascular Bundles
SARCOIDOSIS, ACTIVE – ALVEOLAR FORM
Lymphovascular nodularity was noted in the bronchovascular bundles as well as in the interlobular septa, consistent with sarcoidosis
Ashley Davidoff MD
Small Airways

Ashley Davidoff TheCommonVein.net 29289
Ashley Davidoff TheCommonVein.net 29288m
Along Venules
Secondary Lobule
SARCOIDOSIS, ACTIVE – ALVEOLAR FORM
Ashley Davidoff MD
SARCOIDOSIS, ACTIVE – ALVEOLAR FORM
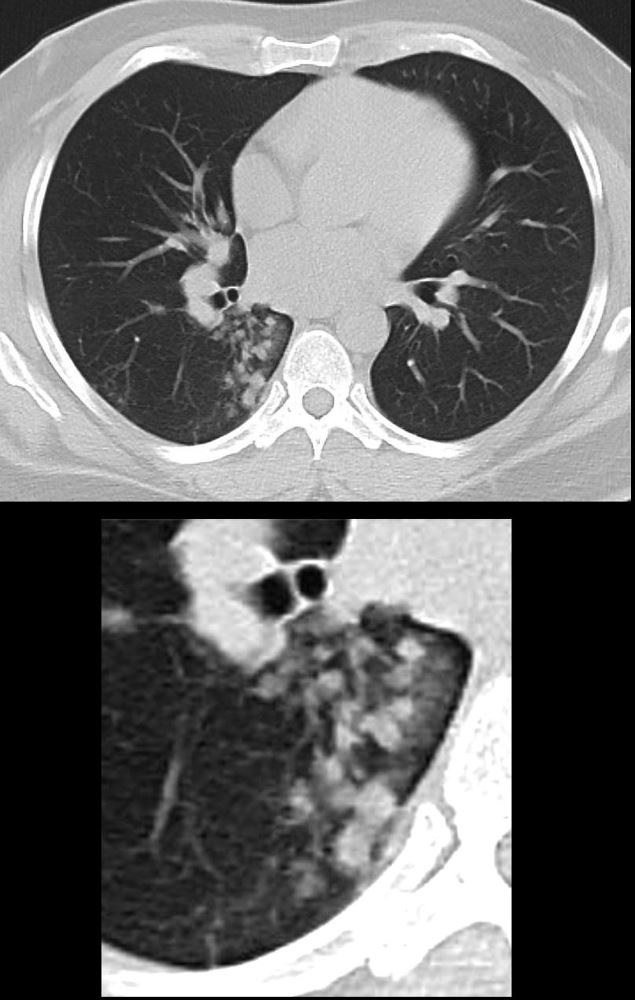
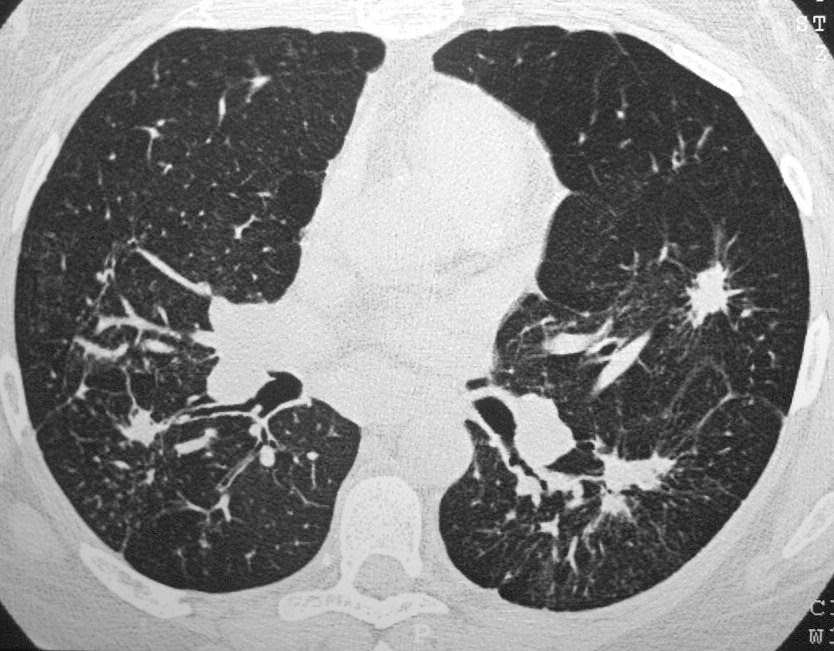
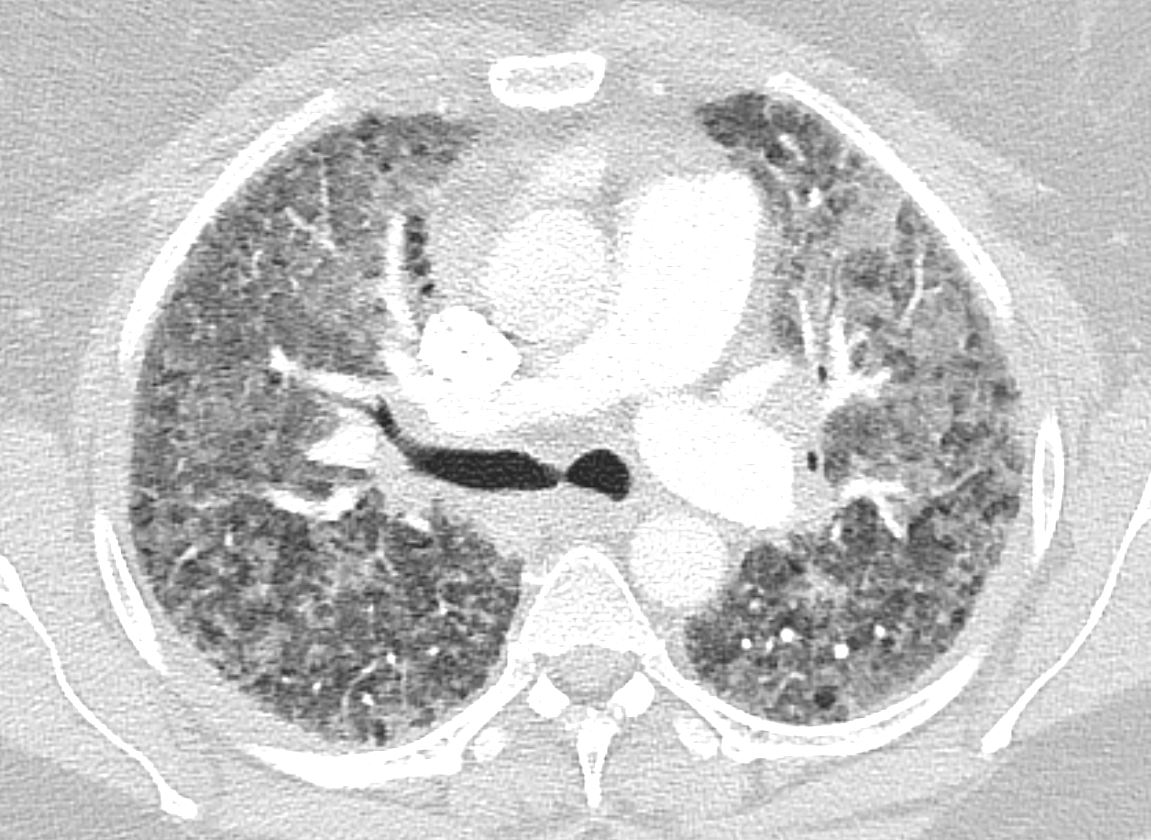
48-year-old previously well presented with dyspnea and initial CXR showed an infiltrate at the right base, and clinically resolved. He presented a year later with right chest pain and low grade ever and the CXR showed patchy opacities in the LUL and in the RLL
A subsequent CT showed LUL nodular opacities and subpleural rim of consolidation in the LUL and more prominently at both lung bases, associated with significant mediastinal adenopathy. Lymphovascular nodularity was noted in the bronchovascular bundles as well as in the interlobular septa, consistent with sarcoidosis
CXR and CT 4 years later showed almost complete resolution of the parenchymal findings and the CT findings except for minimal reticulation and scarring in the subpleural regions
Ashley Davidoff MD
Ashley Davidoff MD
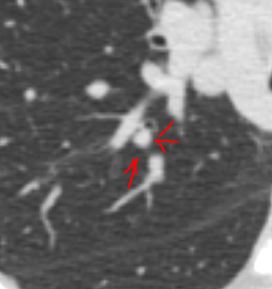
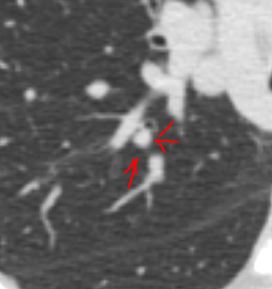
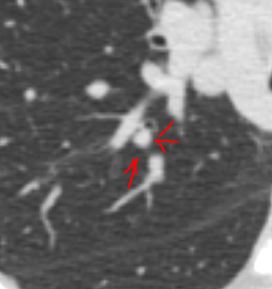
Localized Larger Nodules Along Bronchovascular Bundles
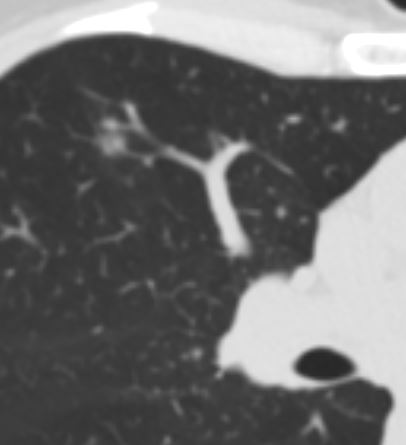
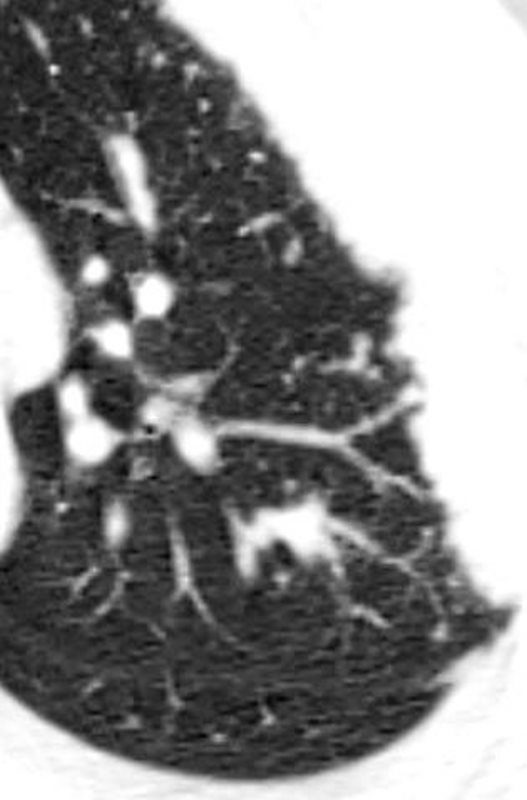
60 -year-old male with a cough. CT shows relatively large nodules in a subsegmental distribution along a bronchovascular distribution the right lower lobe apical segment
Ashley Davidoff MD TheCommonVein.net 135736
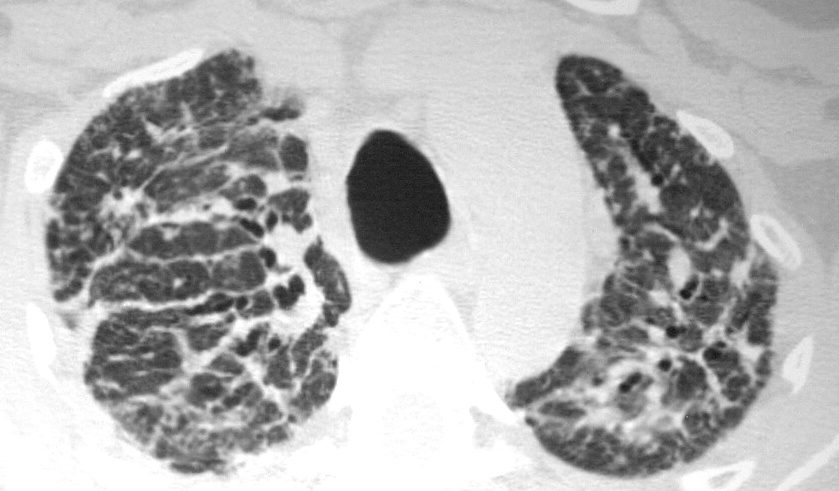
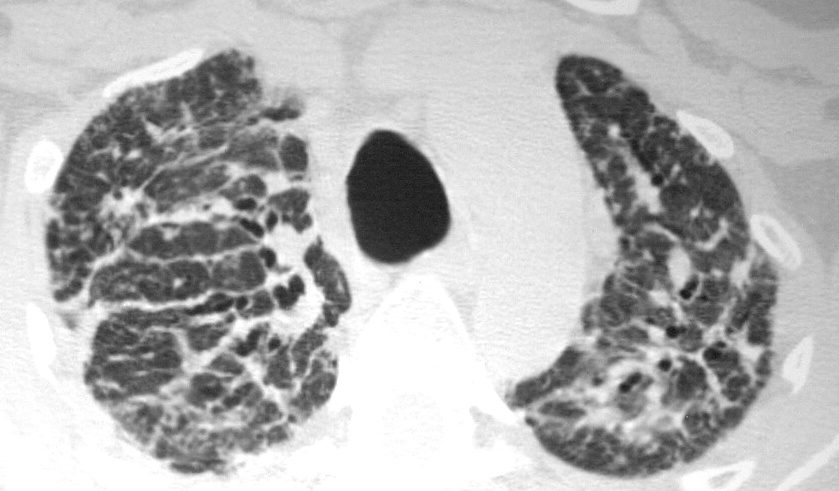
Thickened Interlobular Septa
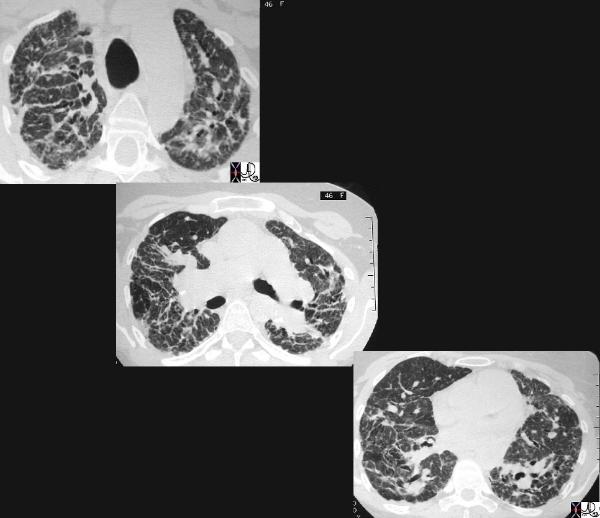
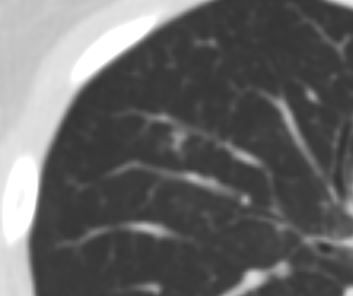
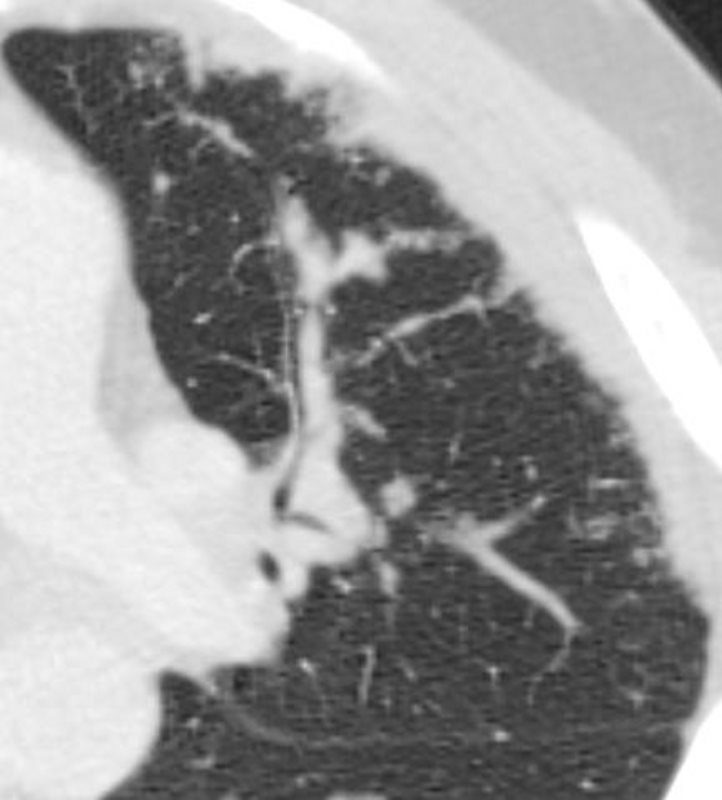
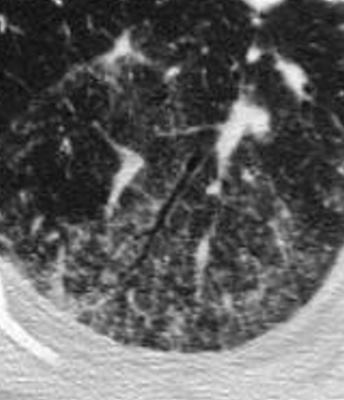
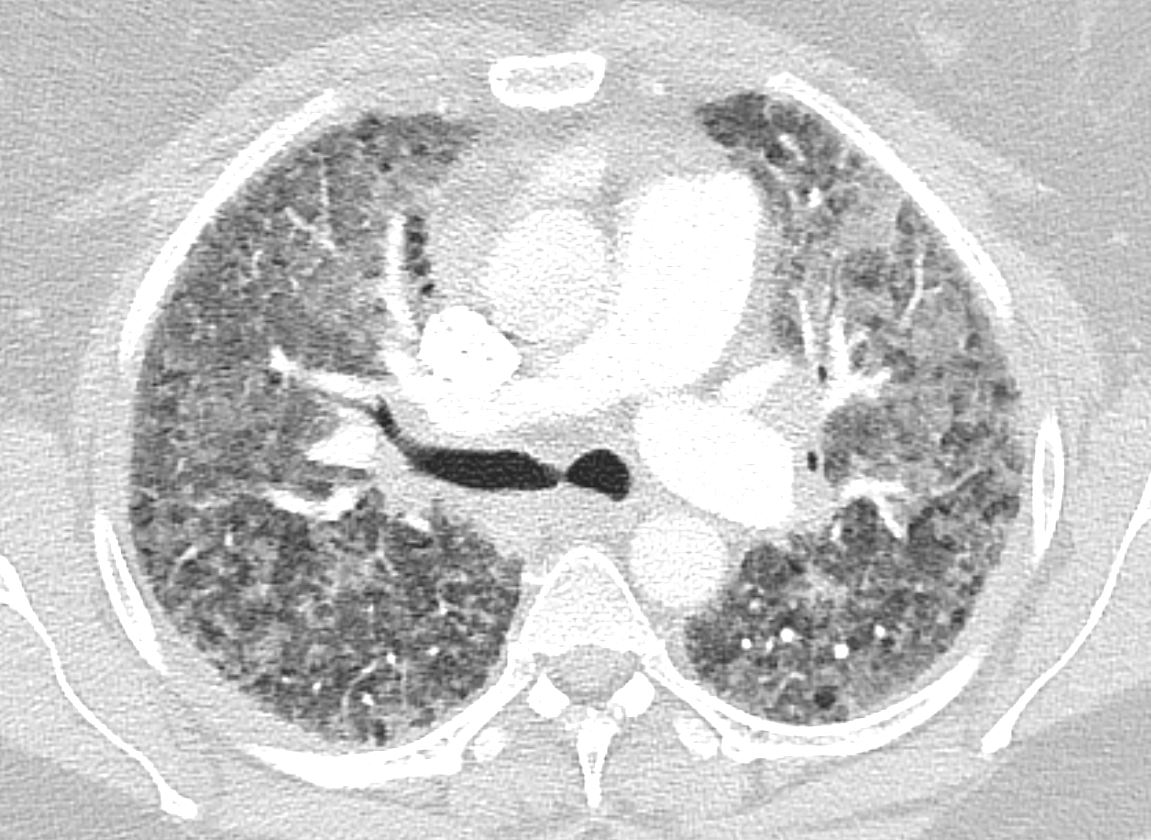
This cross sectional series of 3 CT images shows end stage sarcoidosis characterised by marked thickening along the lymphovascular bundles. The first image in the upper left shows marked thickening of the interlobular septa caused by granulomatous changes along the lymphatics. Courtesy Priscilla Slanetz MD. 31866c
REGIONS
Ashley Davidoff MD
SARCOIDOSIS – CHARACTERISTIC NODULES
Ashley Davidoff MD
Fissures

The axial CTscan shows thickening and irregularity of the major fissure, a band of fibrosis in the right upper lobe, thickening of a segmental bronchus in the right upper lobe and bronchocentric fibrosis in the left upper lobe and multiple micronodules
Ashley Davidoff MD TheCommonvein.net lungs sarcoid 002
Courtesy Paul Kohanteb MD
TheCommonVein.net
Courtesy Paul Kohanteb MD
TheCommonVein.net
Bronchovascular Bundles

Ashley Davidoff MD TheCommonVein.com sarcoidosis 003 35M
Ashley Davidoff MD TheCommonVein.com sarcoidosis 001 35M
Trachea
Main Stem Bronchi
Segmental and Subsegmental Airways
Ashley Davidoff MD TheCommonVein.com sarcoidosis 001 35M



Ashley Davidoff MD TheCommonVein.com sarcoidosis 003 35M


Ashley Davidoff MD TheCommonVein.com sarcoidosis 002 35M
Parenchymal Nodules


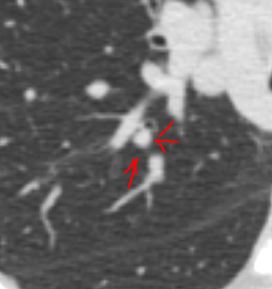
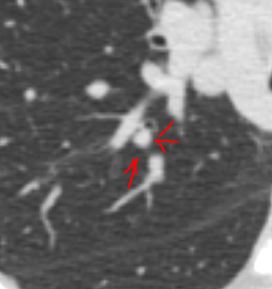
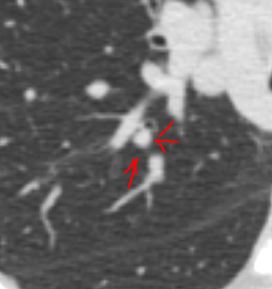
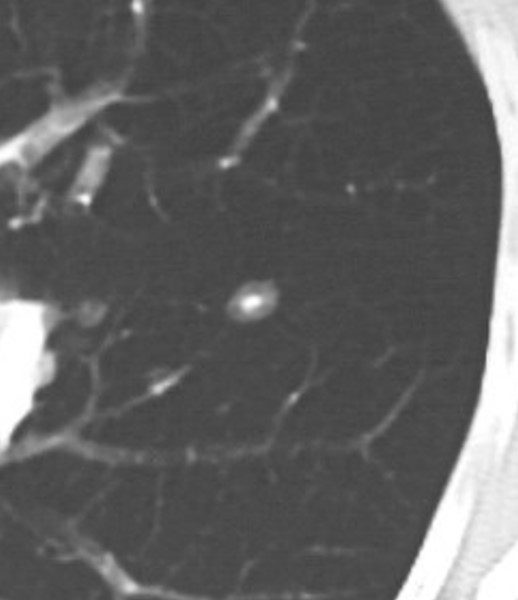
A small nodule (red arrow a,b,c)was identified on the CT in this 60 year old female who is a smoker . The SUV at 1.3 was low (usually >2.5 in malignancy. At pathology it was found to be a necrotizing pneumonia. Most necrotizing granulomas are related to infection. Wegener’s granulomatosis Churg-Strauss syndrome, vasculitis, and sarcoidosis are more often associated with non necrotizing nodules
Ashley Davidoff MD TheCommonVein.net 72372c03
Calcified Nodules
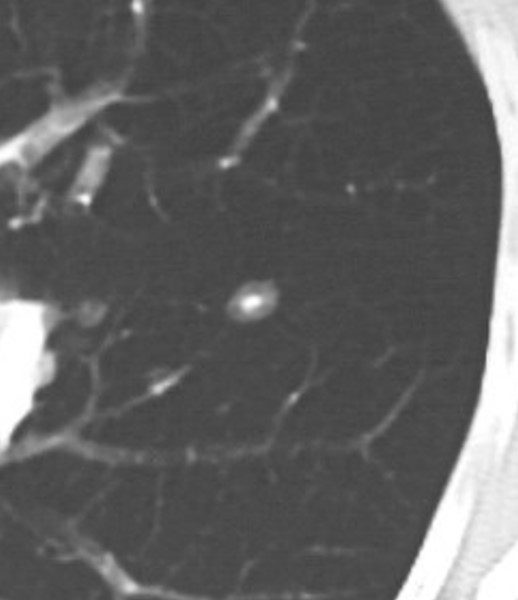
CT scan shows a 6mm nodule with central calcification
Ashley Davidoff TheCommonVein.net 70060b


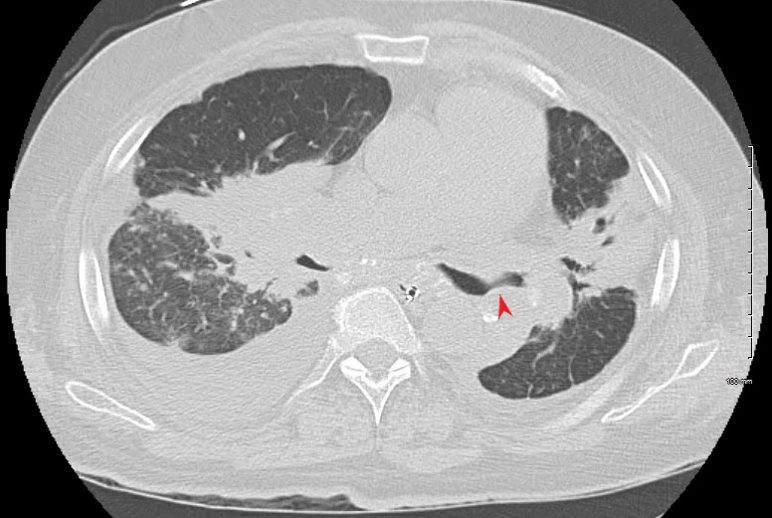
Sarcoid-like granulomatosis of the lung in an asymptomatic 75-year-old man with metastatic melanoma treated with pembrolizumab. (a) Axial CT image shows a parenchymal conglomerate opacity in the right lower lobe of the lung (arrow), which had been gradually increasing over time on serial scans obtained during therapy. Note that the patient had a previous left pneumonectomy.
Nishino, M et al Thoracic Complications of Precision Cancer Therapies: A Practical Guide for Radiologists in the New Era of Cancer Care RadioGraphicsVol. 37, No. 5
Irregular spiculated solid nodule
Ashley Davidoff
TheCommonVein.net
42 year old female with known history of sarcoidosis characterised by confluent granulomas, with spiculated nodules, retractile fibrosis and moderate adenopathy
Ashley Davidoff MD TheCommonVein.net 31828
Irregular solid bilobed nodule
Ashley Davidoff
TheCommonVein.net
Parenchymal Infiltrates
Confluent Fibrotic Bands Extending to the Hilum
Micronodules Ground Glass Changes
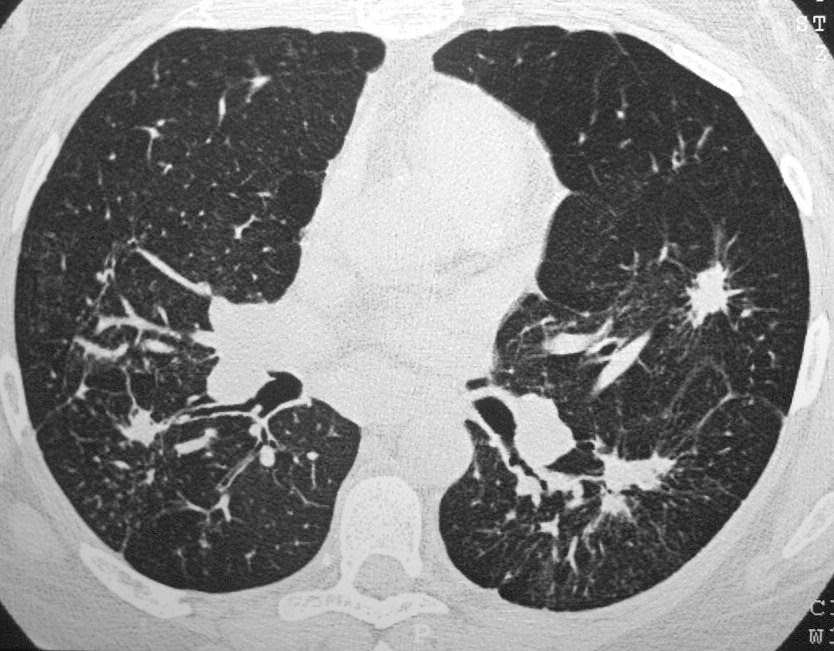
SARCOIDOSIS, STABLE DIFFUSE GROUND GLASS AND ADENOPATHY OVER 9 YEARS
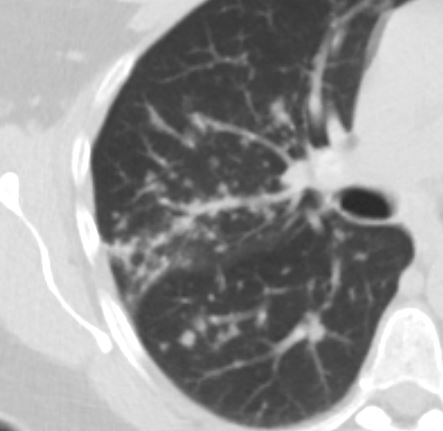
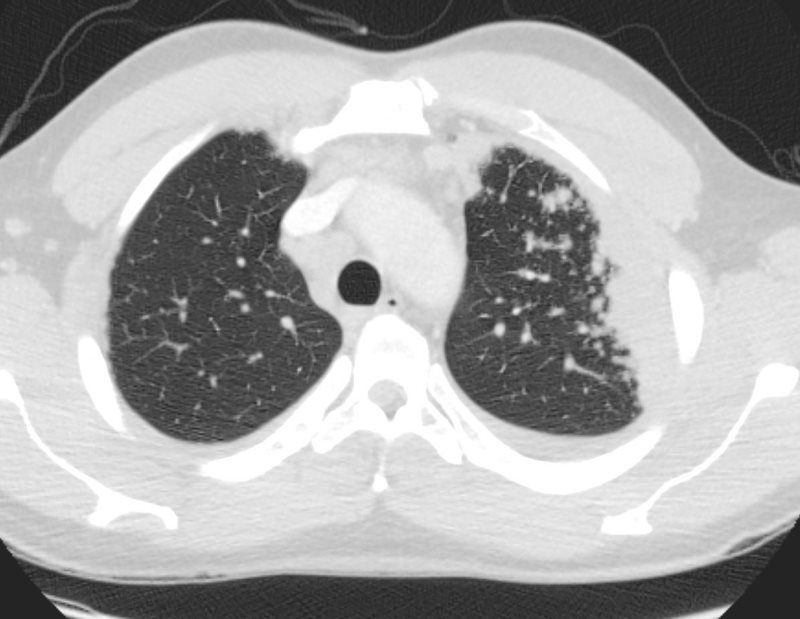
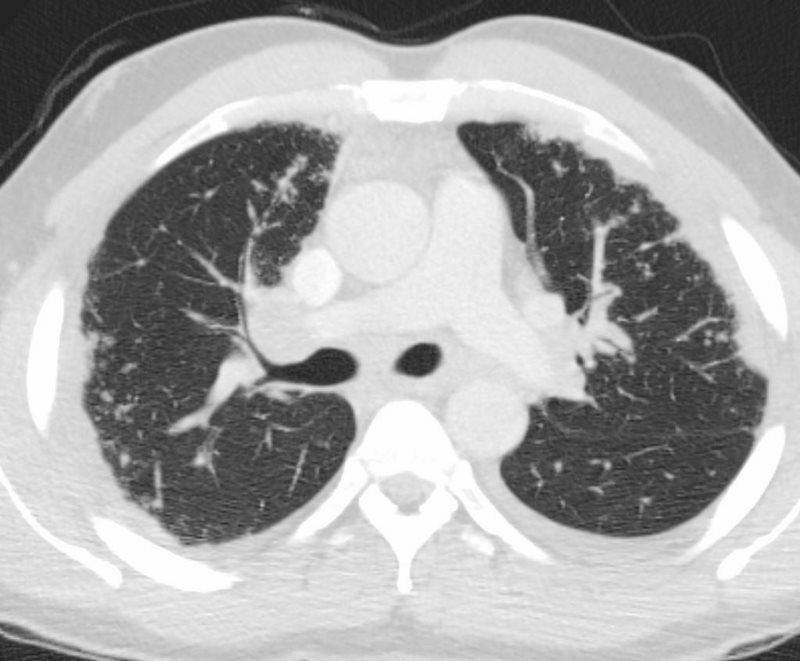
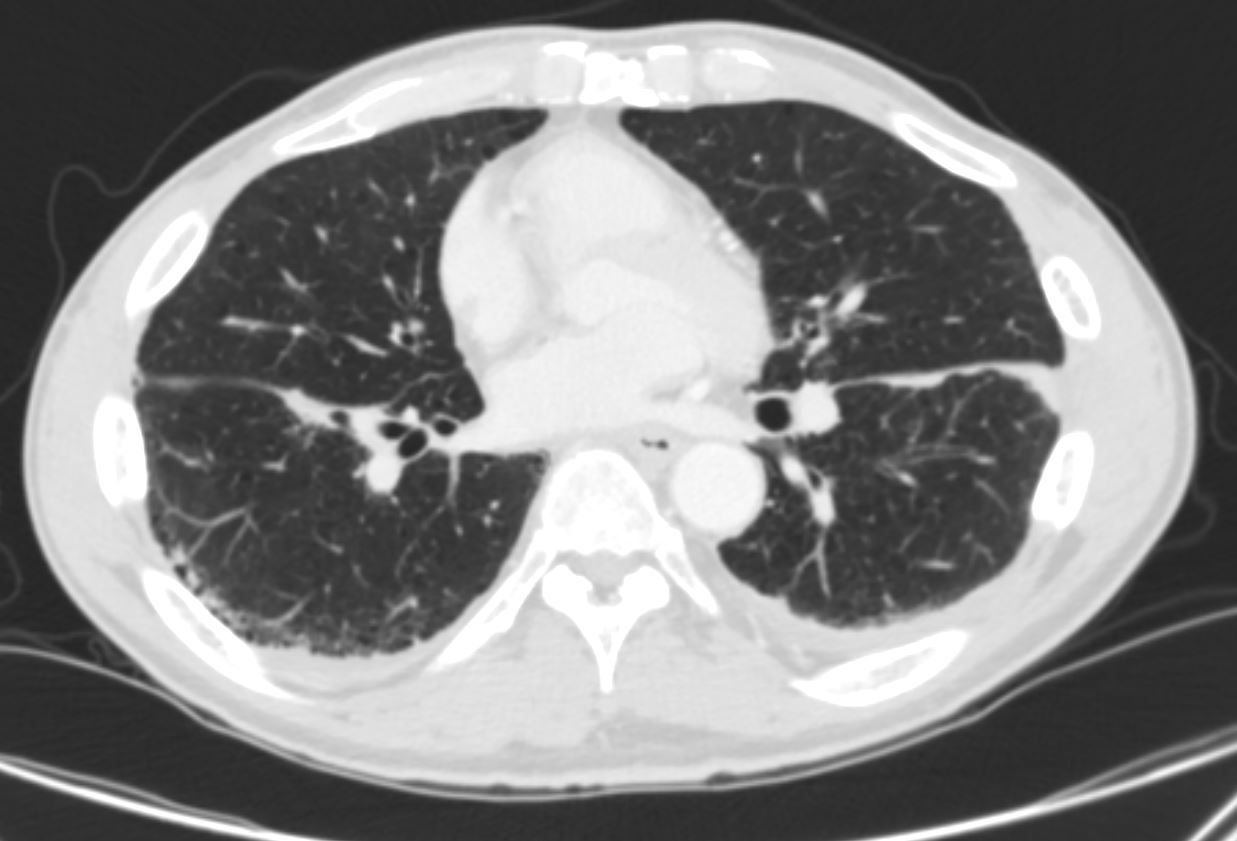
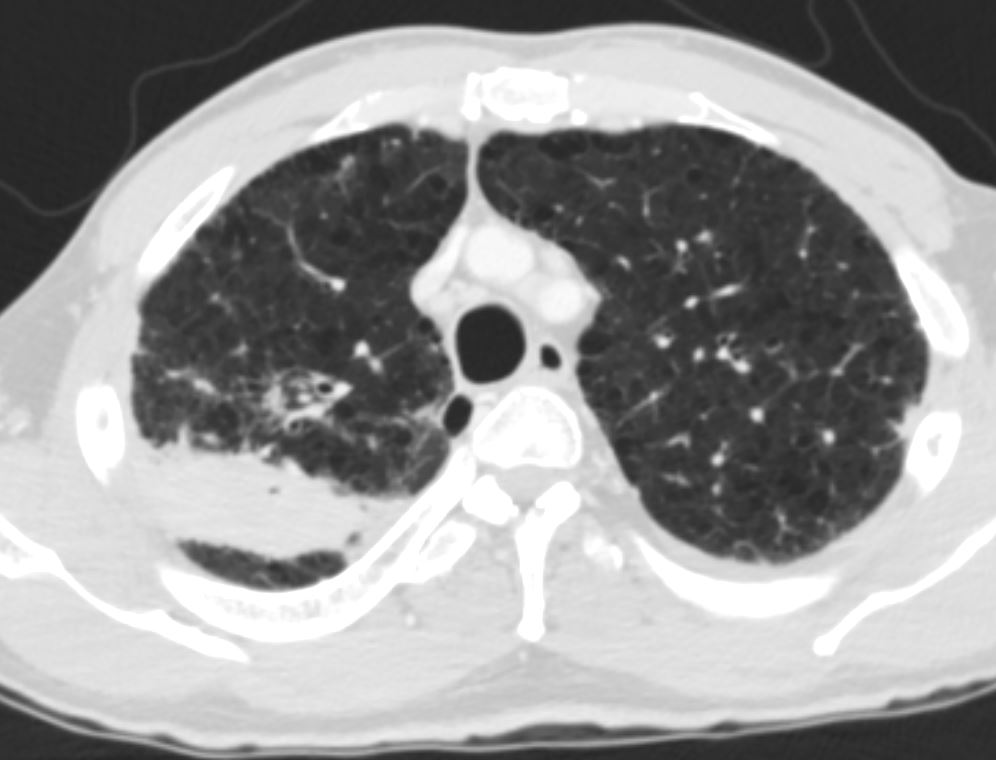
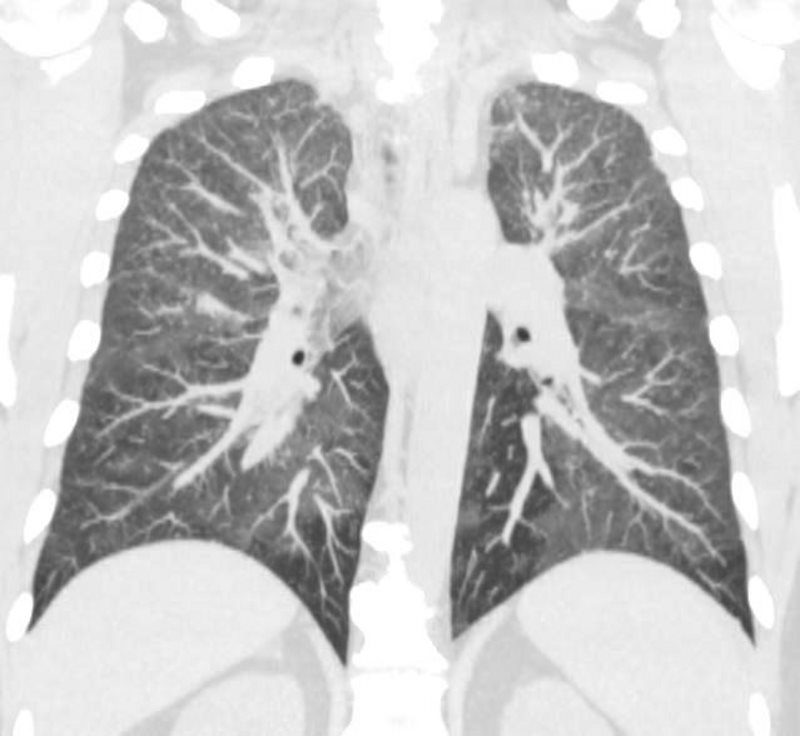
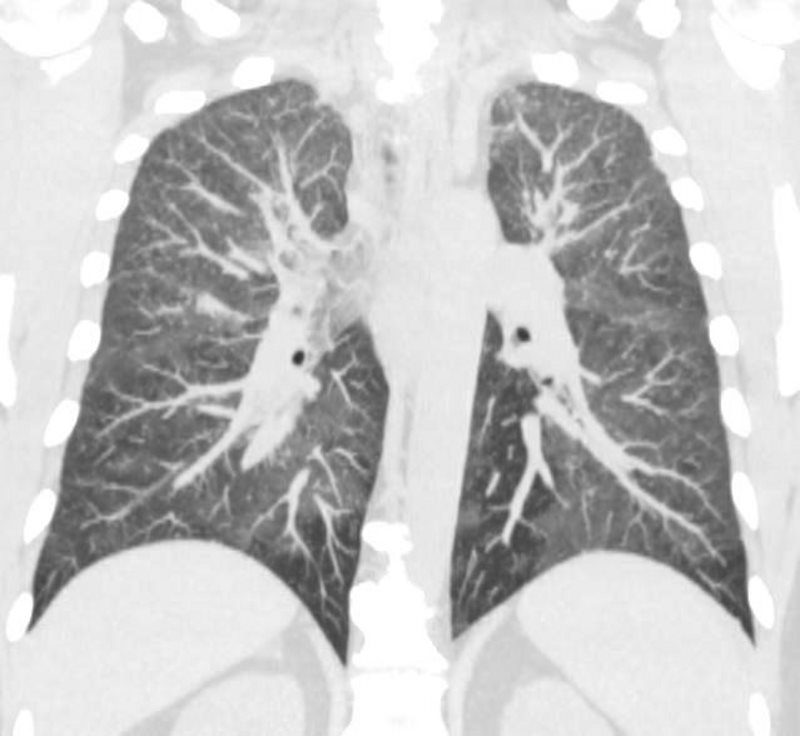
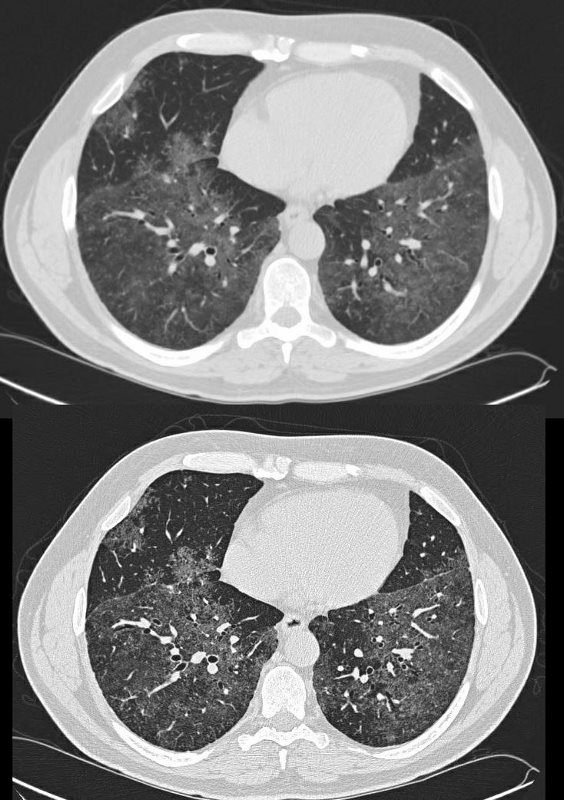
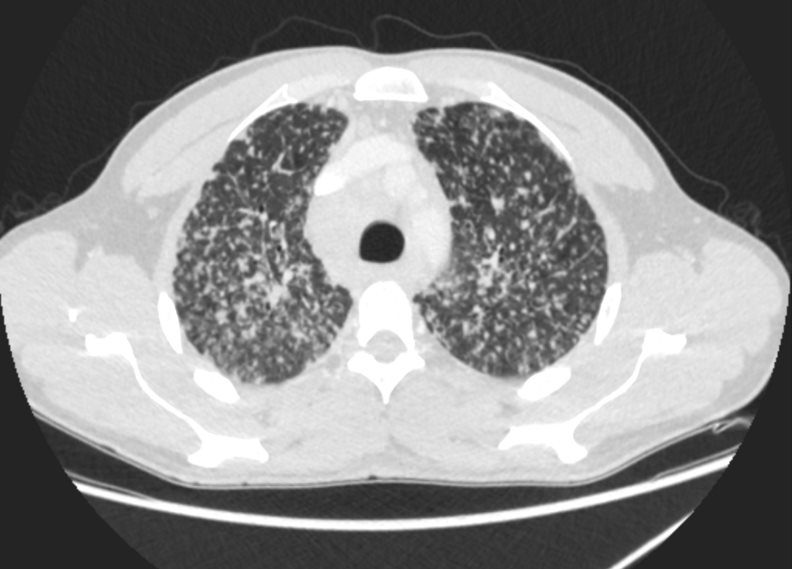
44-year-old male presents with history of sarcoidosis manifesting as diffuse ground glass involving the upper lobes and lower lobes sparing the middle lobe and lingula to some extent.
Associate pathological lymphadenopathy was relatively stable as well
The only available CXR shows a diffuse interstitial pattern with little suggestion of the moderate sized adenopathy apparent on the CT
A cardiac echo was normal, and there was no suggestion of cardiac disease on his CT or CXR.
Ashley Davidoff MD
SARCOIDOSIS, STABLE DIFFUSE GROUND GLASS AND ADENOPATHY OVER 9 YEARS
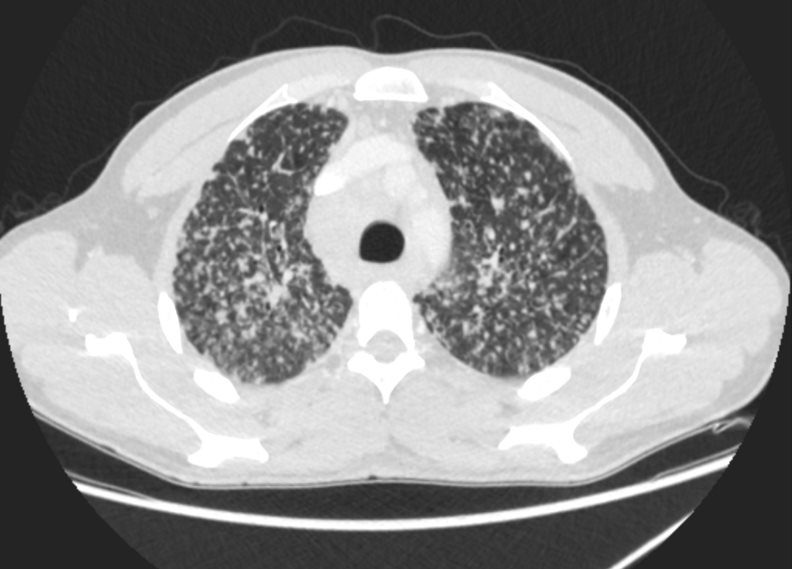
44-year-old male presents with history of sarcoidosis manifesting as diffuse ground glass involving the upper lobes and lower lobes sparing the middle lobe and lingula to some extent.
Associate pathological lymphadenopathy was relatively stable as well
The only available CXR shows a diffuse interstitial pattern with little suggestion of the moderate sized adenopathy apparent on the CT
A cardiac echo was normal, and there was no suggestion of cardiac disease on his CT or CXR.
Ashley Davidoff MD
SARCOIDOSIS, STABLE DIFFUSE GROUND GLASS AND ADENOPATHY OVER 9 YEARS
44-year-old male presents with history of sarcoidosis manifesting as diffuse ground glass involving the upper lobes and lower lobes sparing the middle lobe and lingula to some extent.
Associate pathological lymphadenopathy was relatively stable as well
The only available CXR shows a diffuse interstitial pattern with little suggestion of the moderate sized adenopathy apparent on the CT
A cardiac echo was normal, and there was no suggestion of cardiac disease on his CT or CXR.
Ashley Davidoff MD
Miliary Pattern
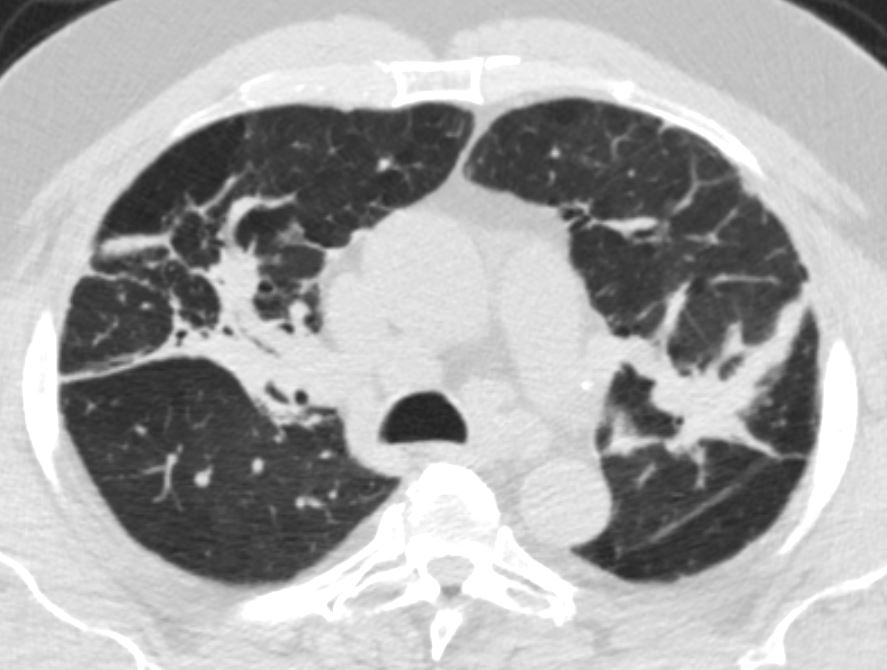
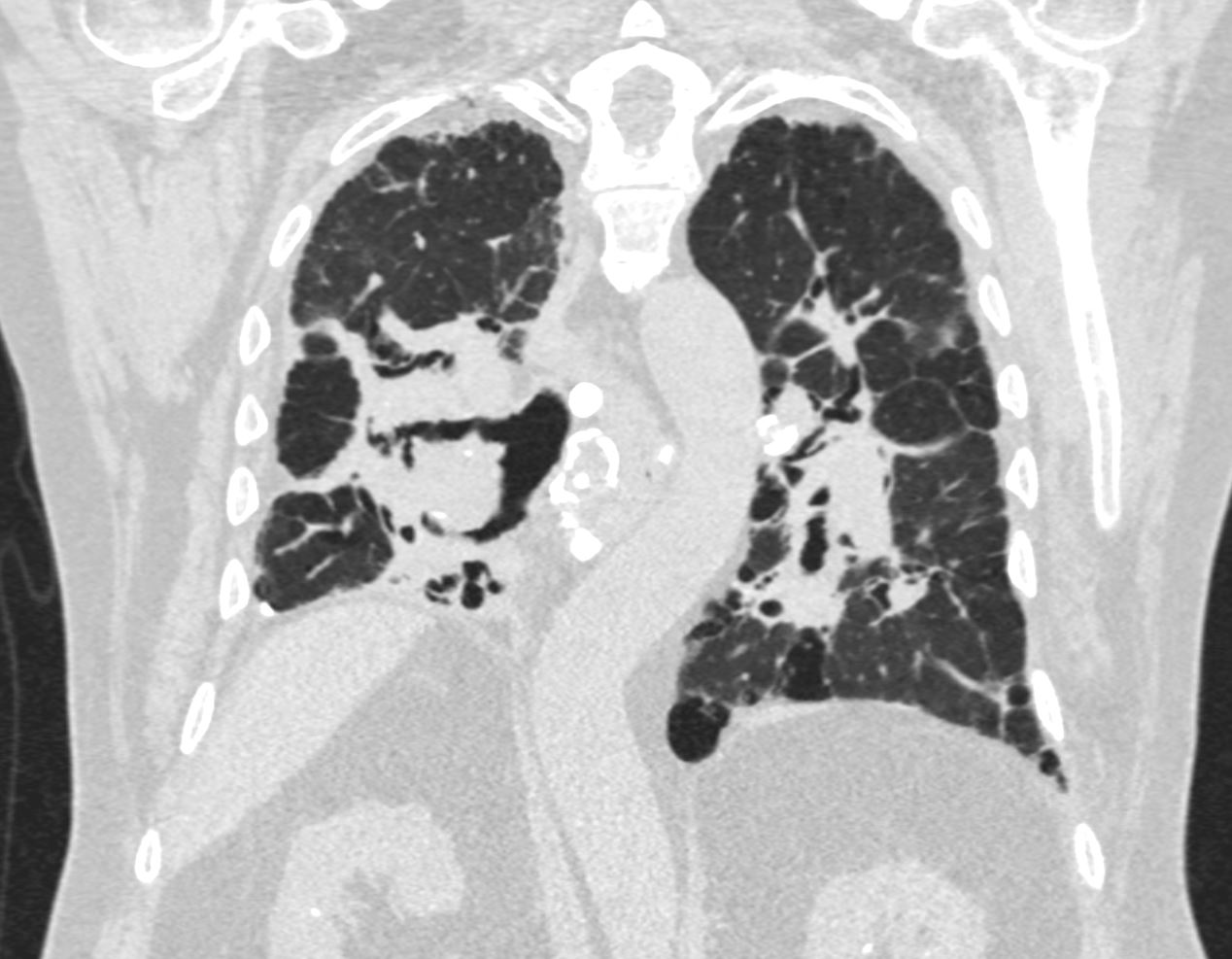
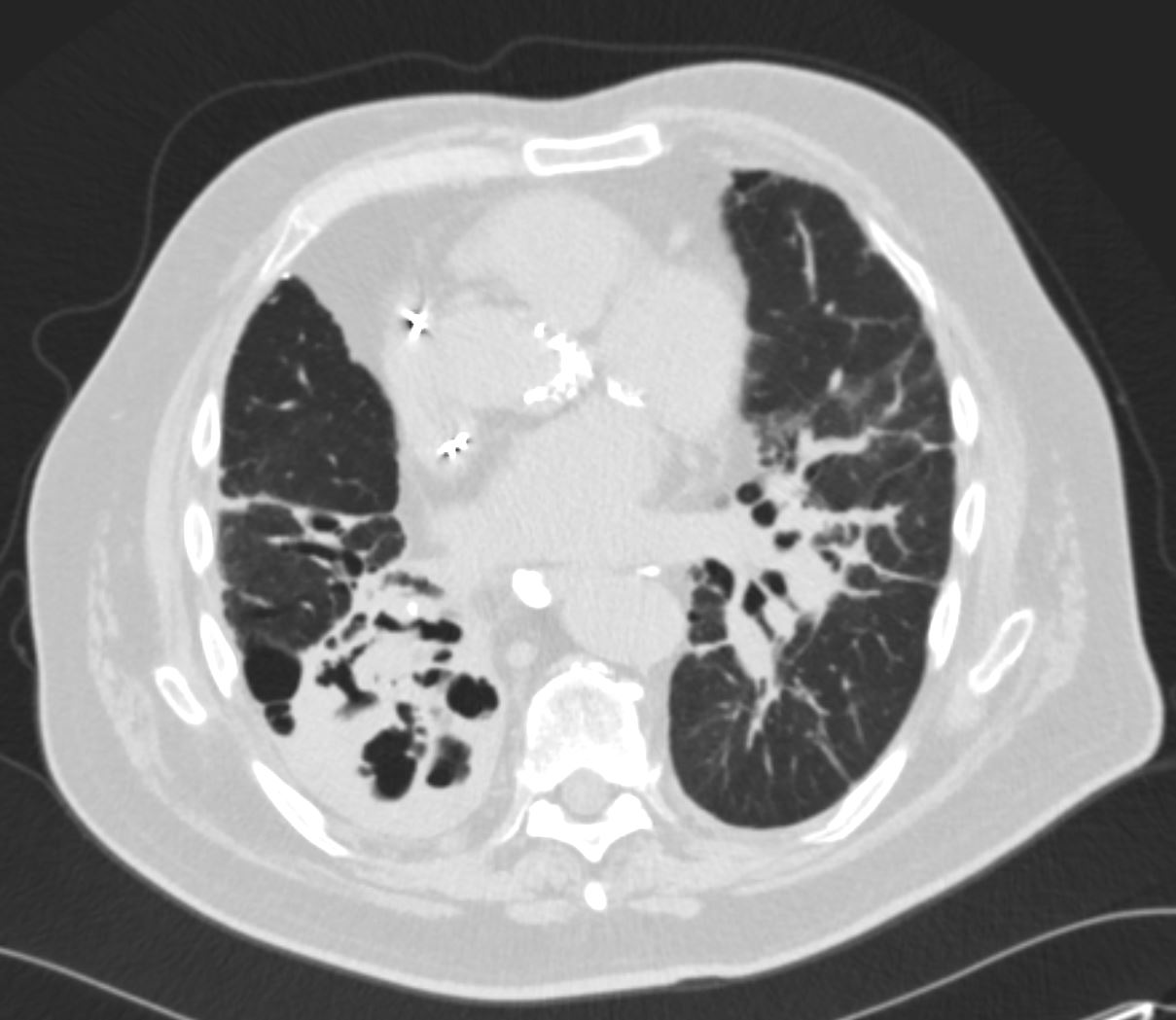
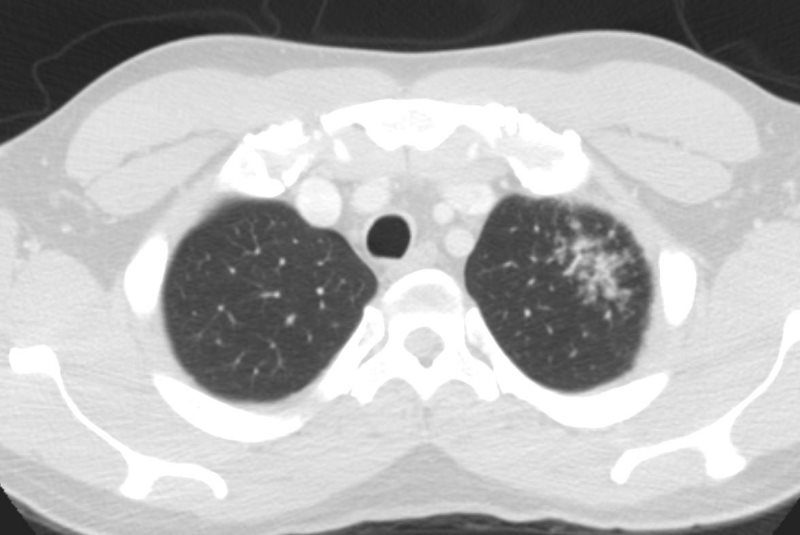
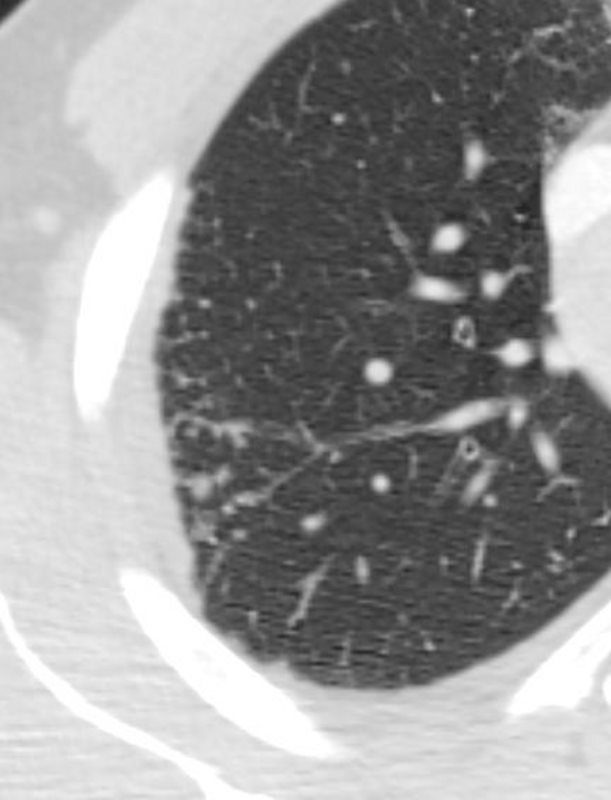
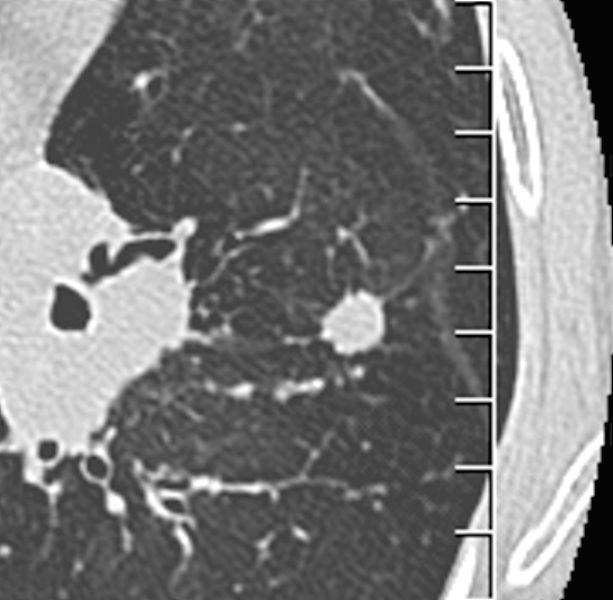
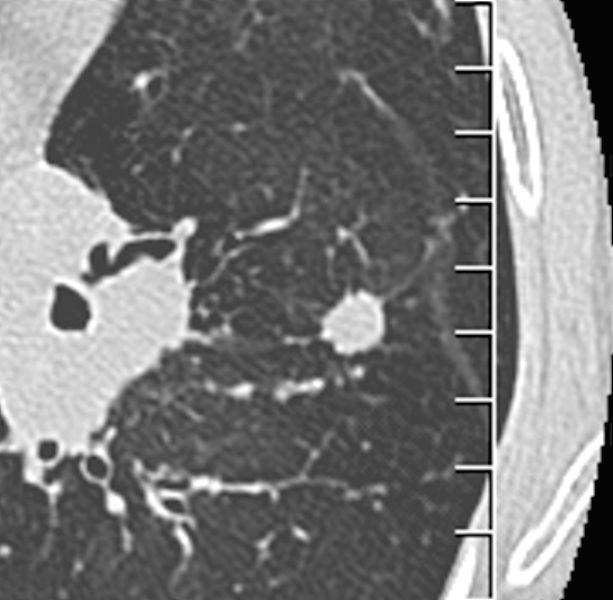
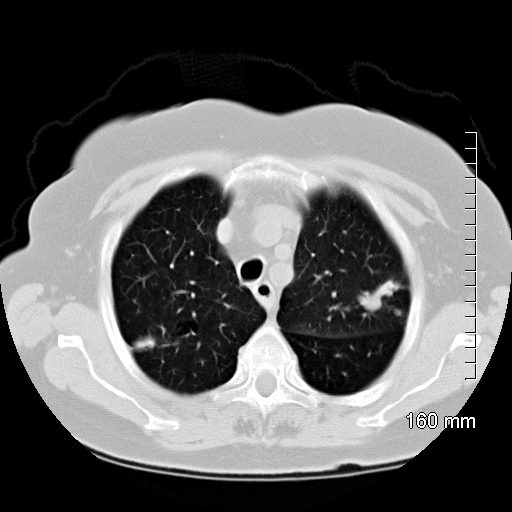
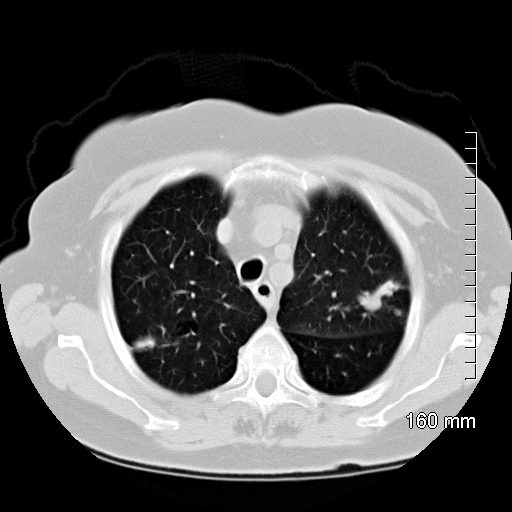
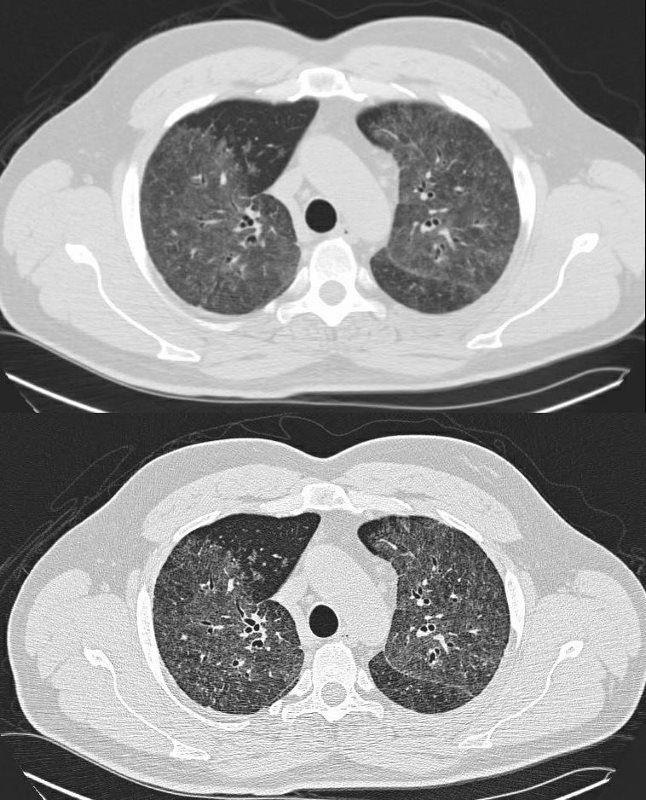
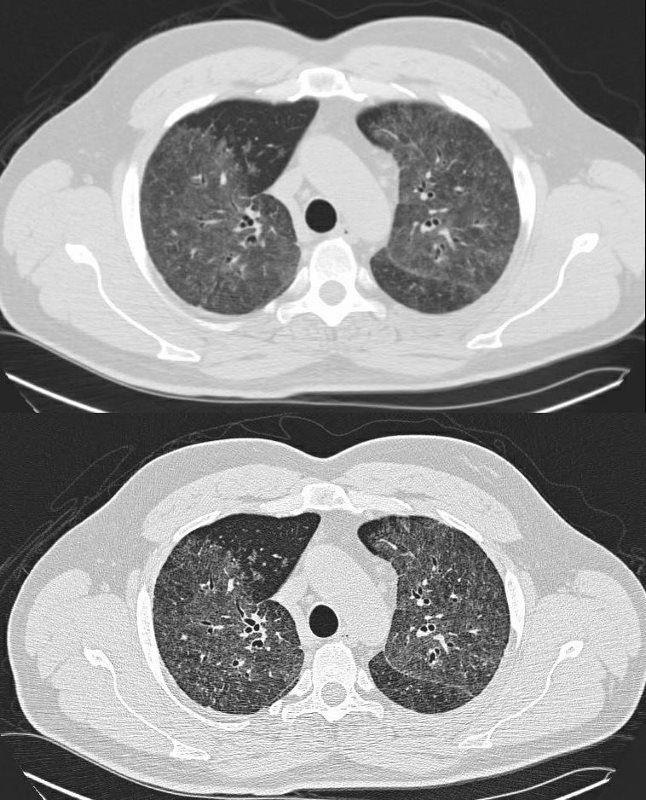
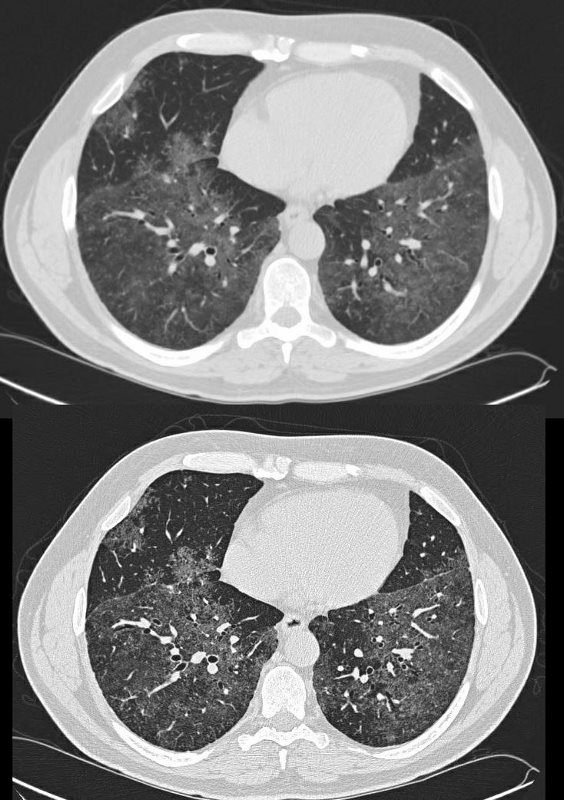
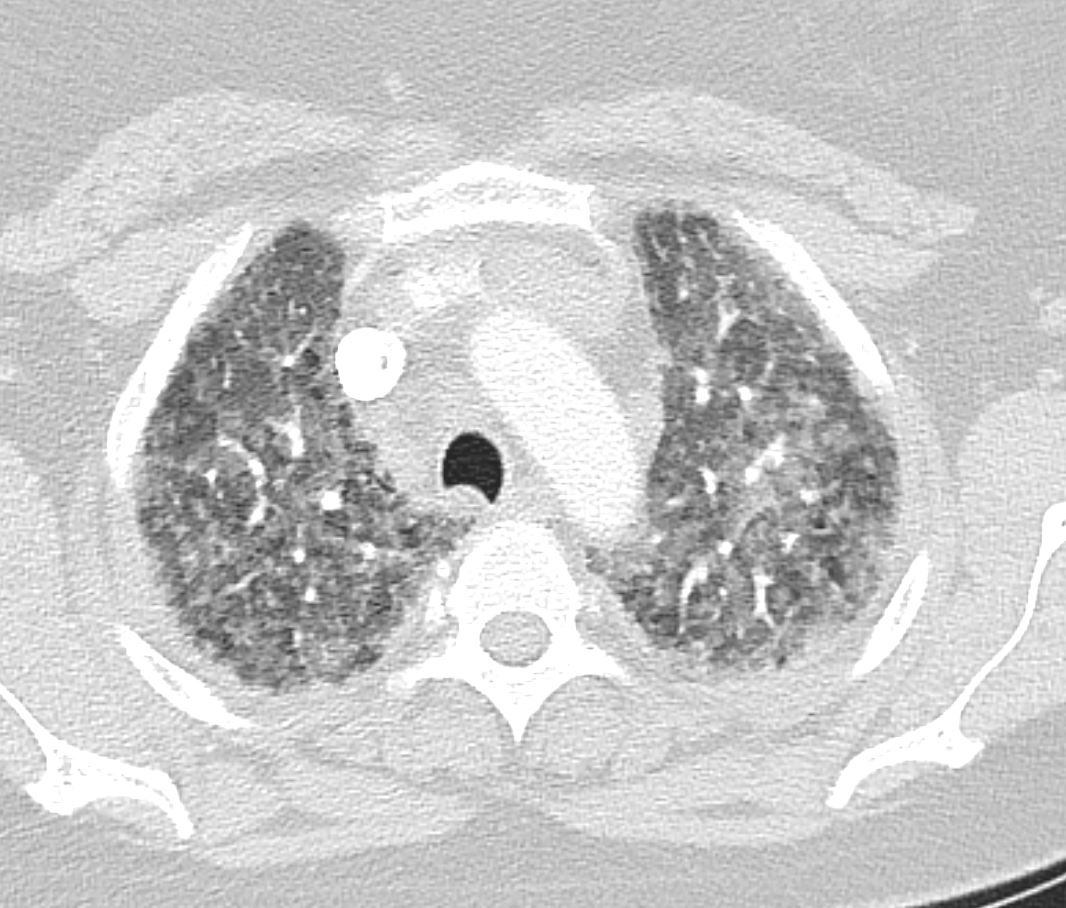
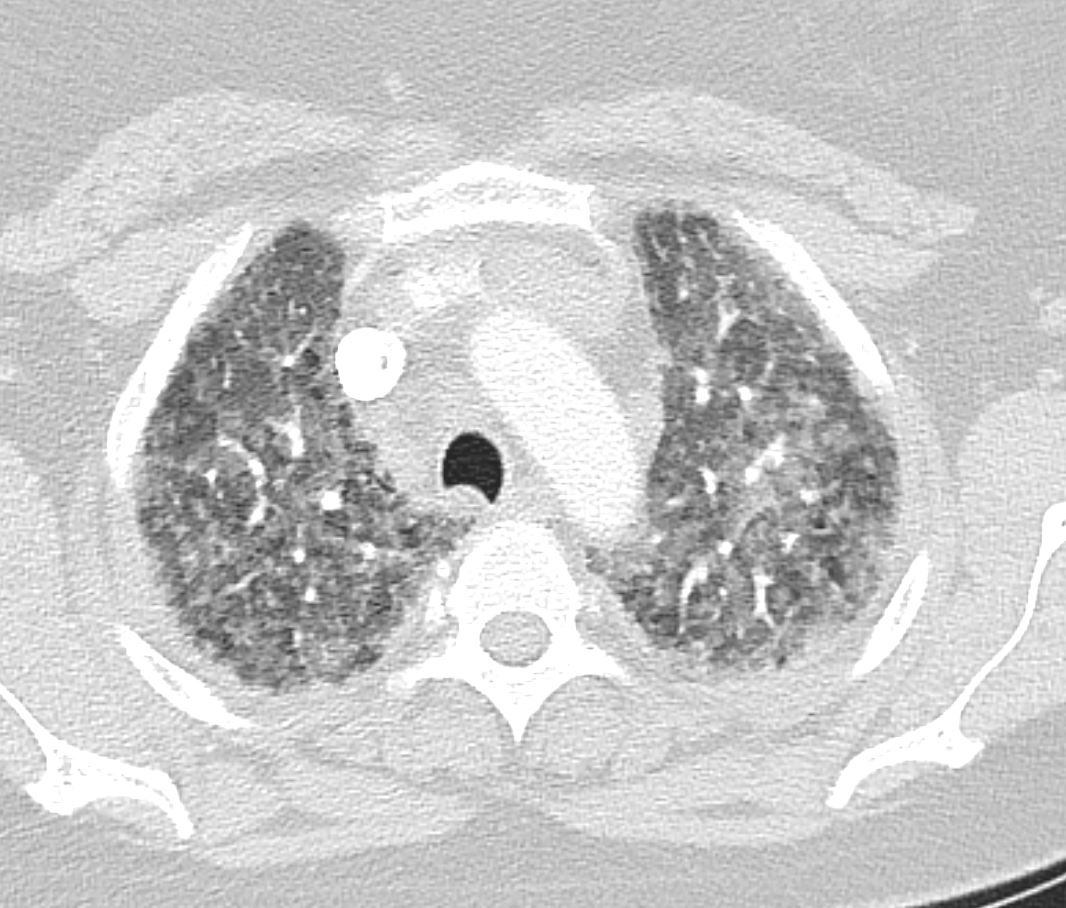
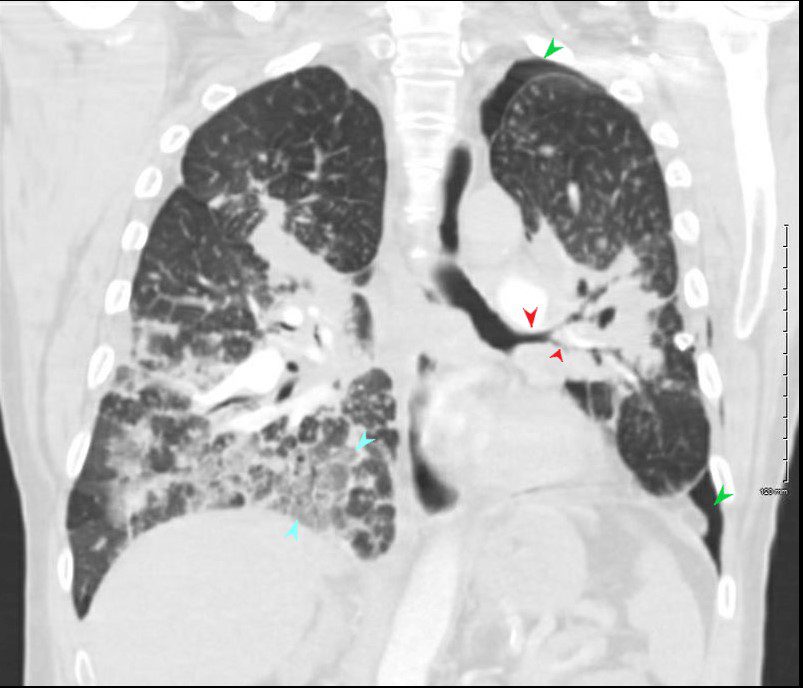
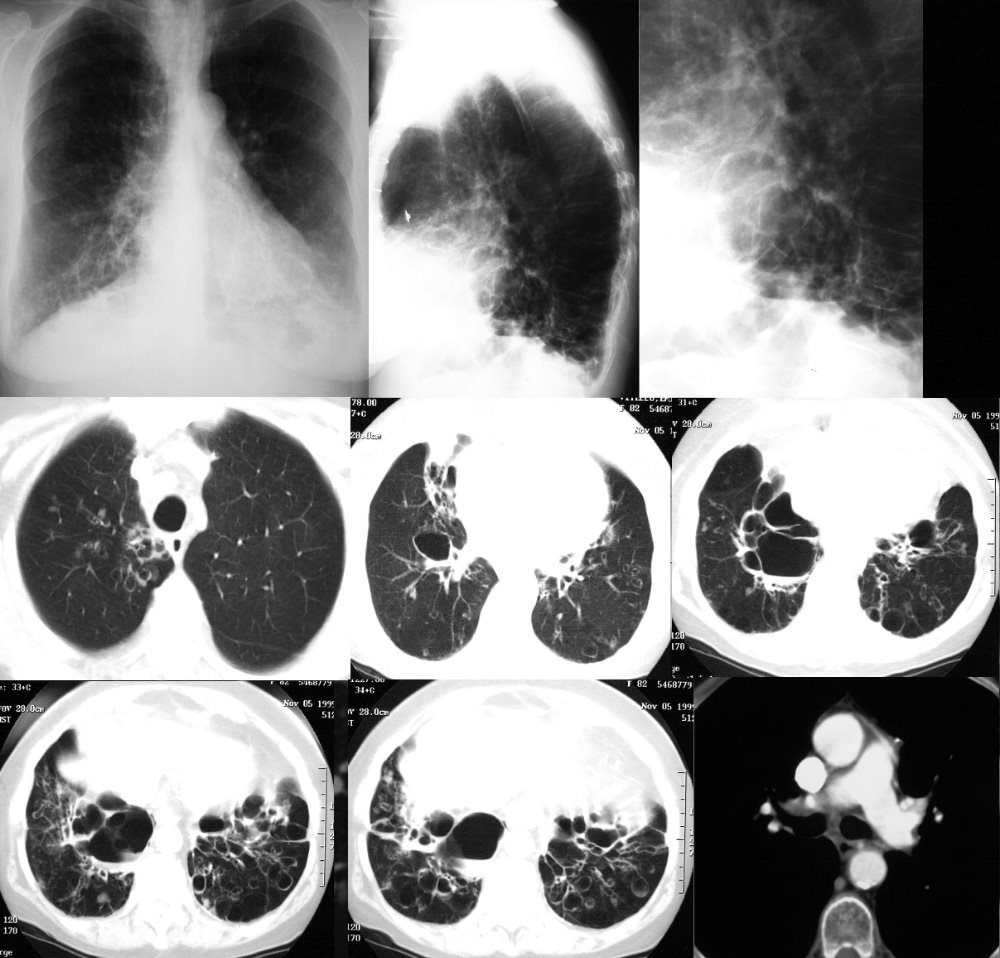
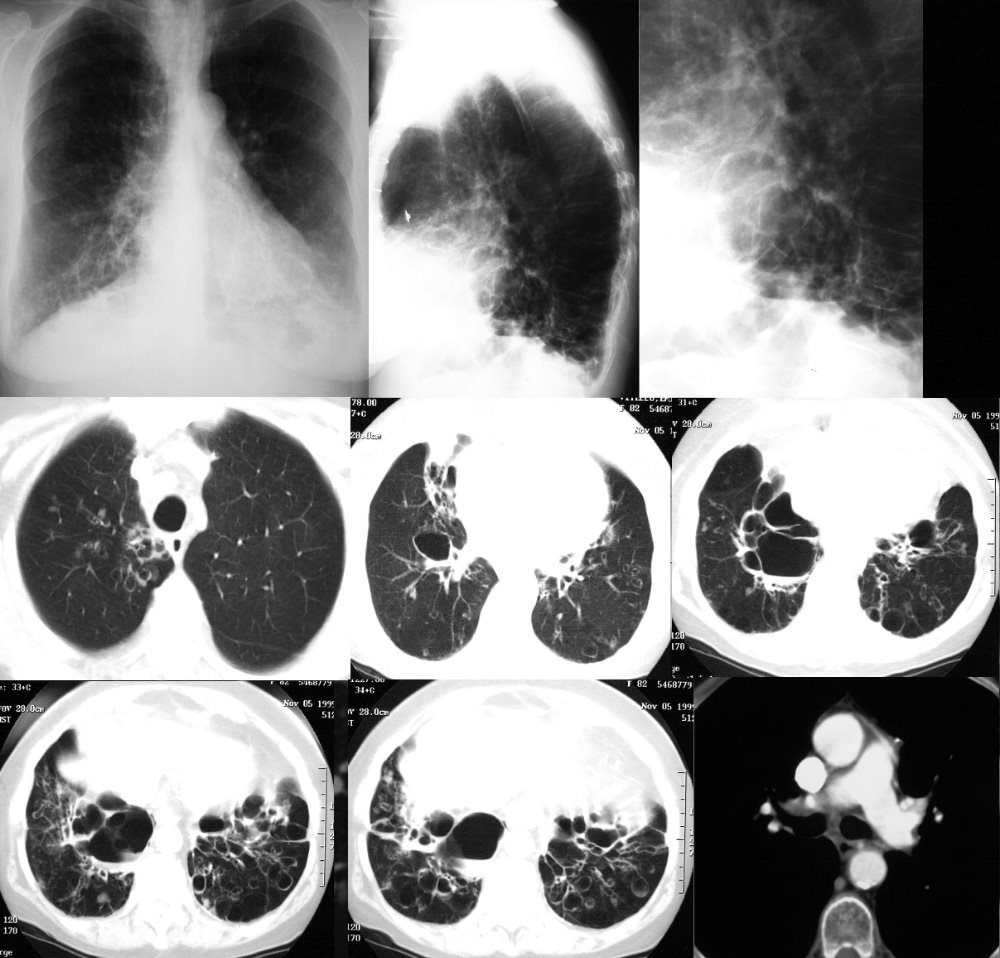
42-year-old cement worker presents with dyspnea .
A CXR performed 5 years prior was close to normal with possible right hilar prominence.
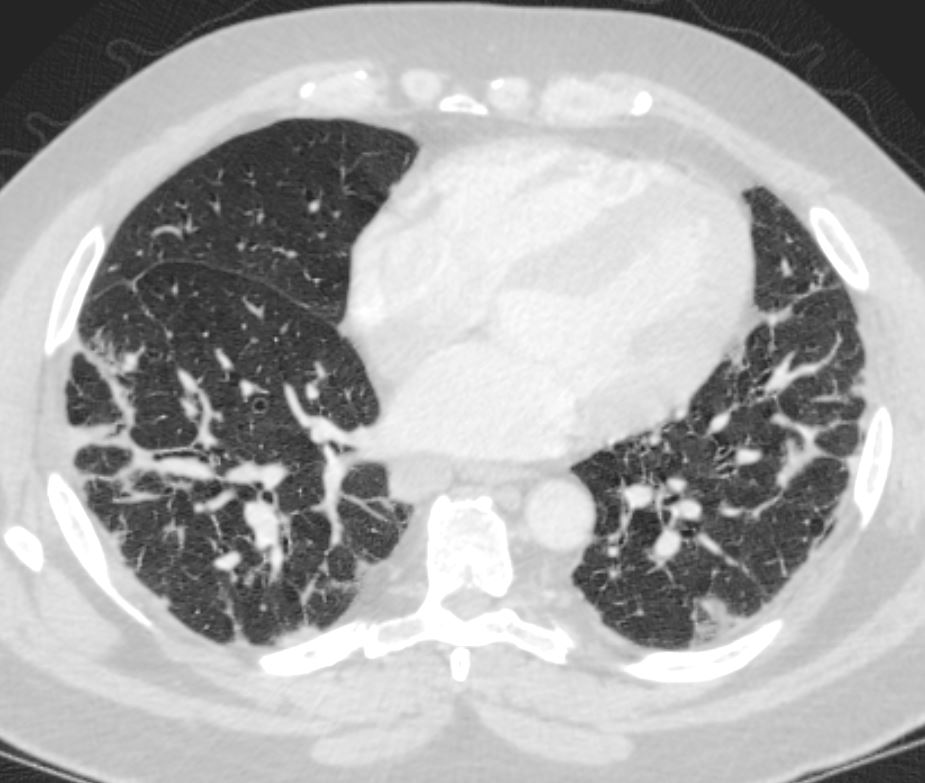
The CT scan, shows diffuse micronodular lung disease, predominantly in the upper lobes with mediastinal widening consistent with mediastinal lymphadenopathy, dominant in the right paratracheal region and in the subcarinal region.
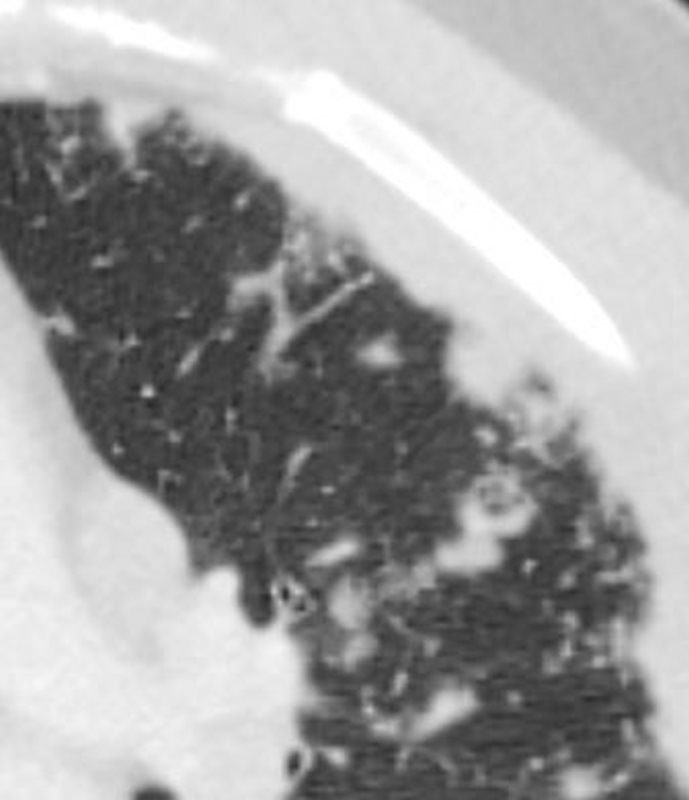
Lung windows show the presence of extensive diffuse micronodular disease accumulating along lymphatics along fissures and pleural surfaces, and along the bronchovascular bundles. Although there is diffuse disease, the upper lobes are slightly more involved than the lower lobes. The extensive thickening along bronchovascular bundles and prominent adenopathy favors a diagnosis of sarcoidosis but with a work history of being a cement worker, silicosis still remains in the differential diagnosis as a less likely possibility.
Ashley Davidoff MD TheCommonVein.net 131749
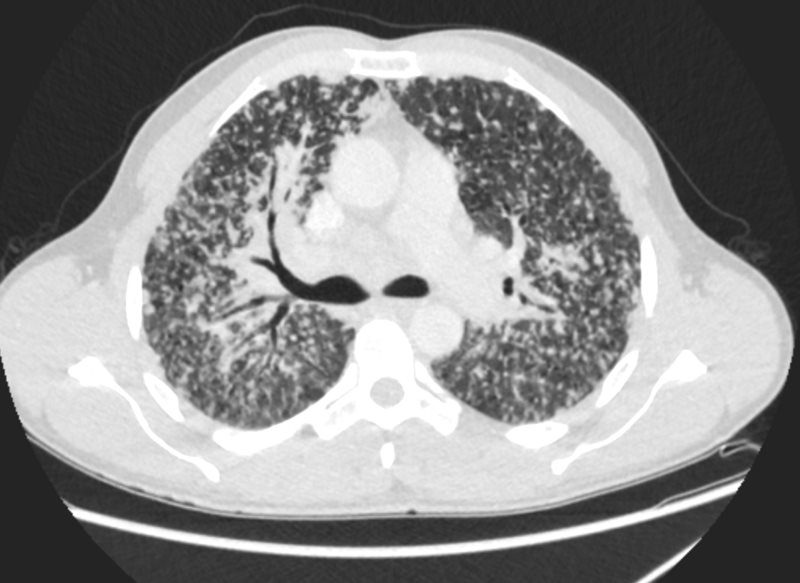
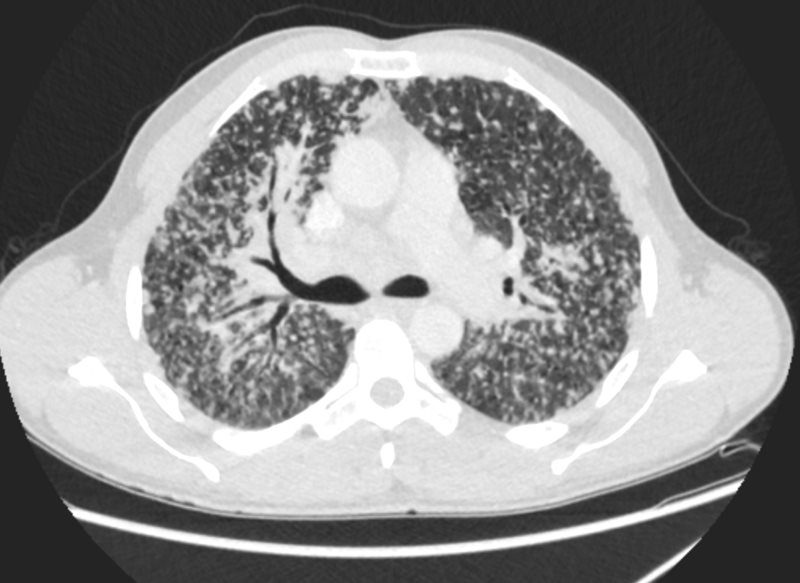
42-year-old cement worker presents with dyspnea .
A CXR performed 5 years prior was close to normal with possible right hilar prominence.
The CT scan, shows diffuse micronodular lung disease, predominantly in the upper lobes with mediastinal widening consistent with mediastinal lymphadenopathy, dominant in the right paratracheal region and in the subcarinal region.
Lung windows show the presence of extensive diffuse micronodular disease accumulating along lymphatics along fissures and pleural surfaces, and along the bronchovascular bundles. Although there is diffuse disease, the upper lobes are slightly more involved than the lower lobes. The extensive thickening along bronchovascular bundles and prominent adenopathy favors a diagnosis of sarcoidosis but with a work history of being a cement worker, silicosis still remains in the differential diagnosis as a less likely possibility.
Ashley Davidoff MD
Alveolar Sarcoid
Bronchiectasis
Lymph Nodes
Stage 1 lymphadenopathy
Ashley Davidoff MD thecommonvein.net
CTscan
SARCOIDOSIS, STAGE IV, PTX, ENCASEMENT
Ashley Davidoff MD
51-year-old male with Stage 2II Sarcoidosis and egg shell calcification of lymph nodes
Ashley Davidoff MD
Pneumothorax Encasement of Airways


Ashley Davidoff MD
SARCOIDOSIS, STAGE IV, PTX, ENCASEMENT
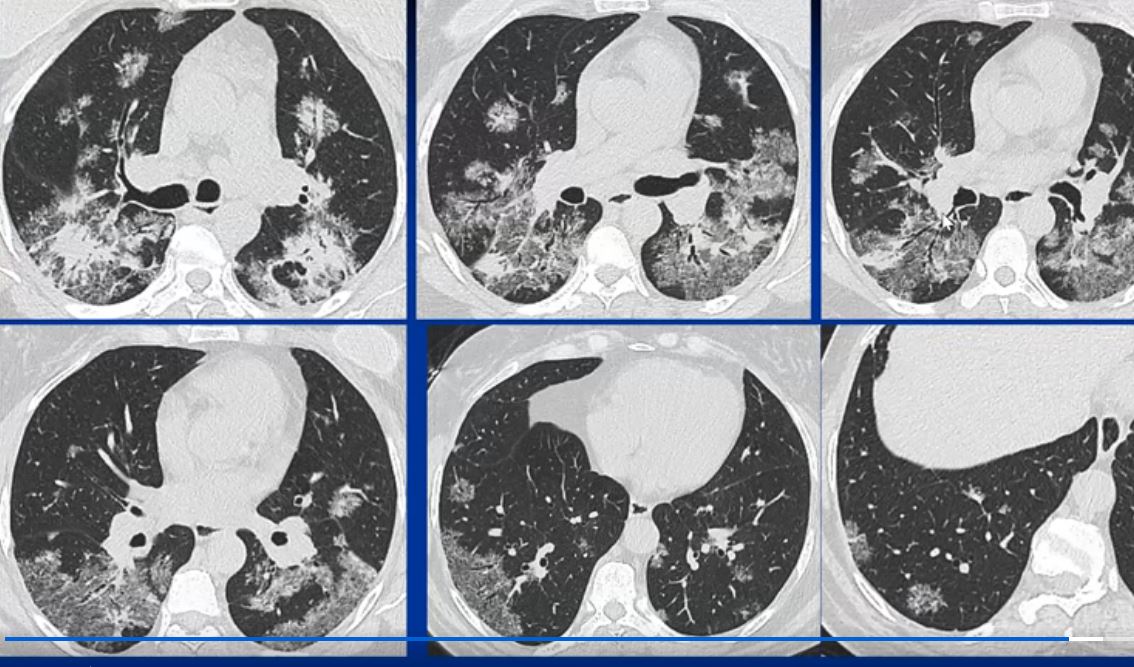
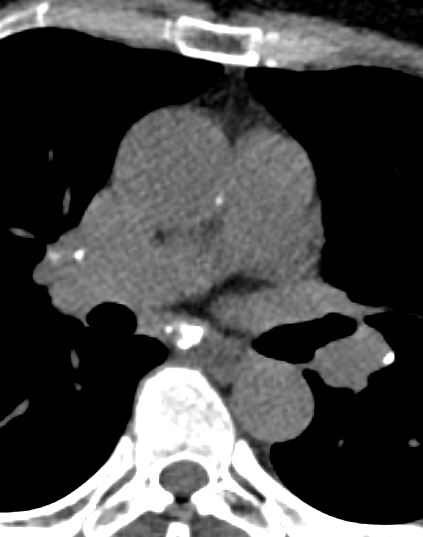
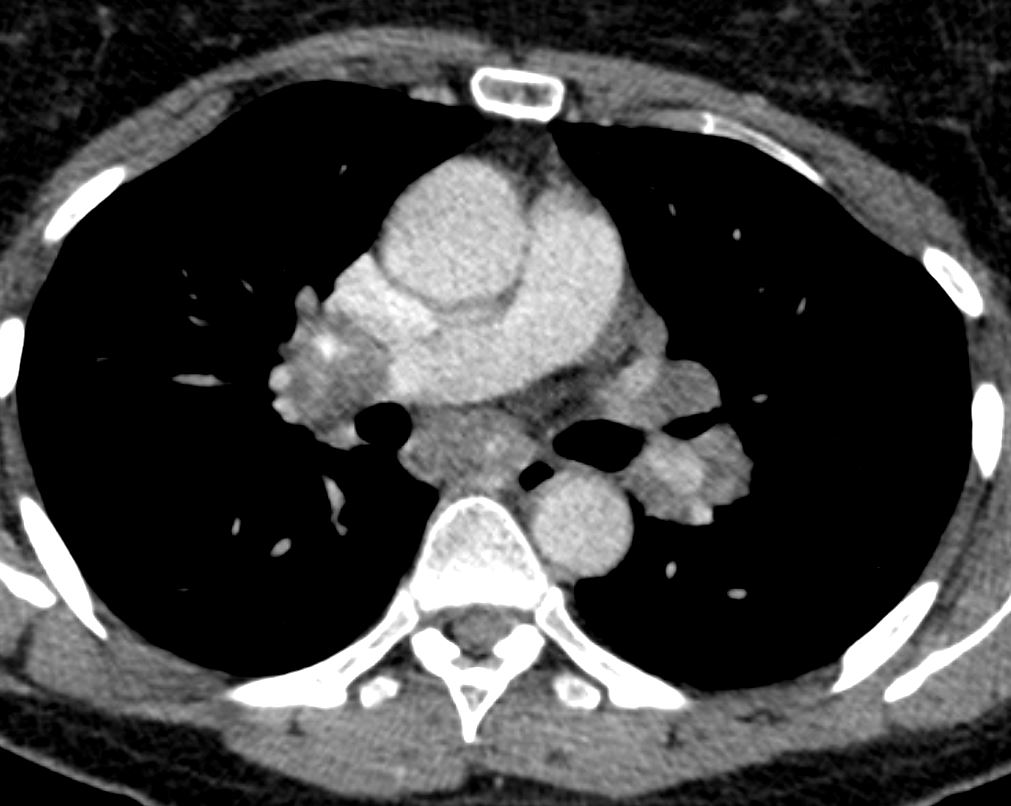
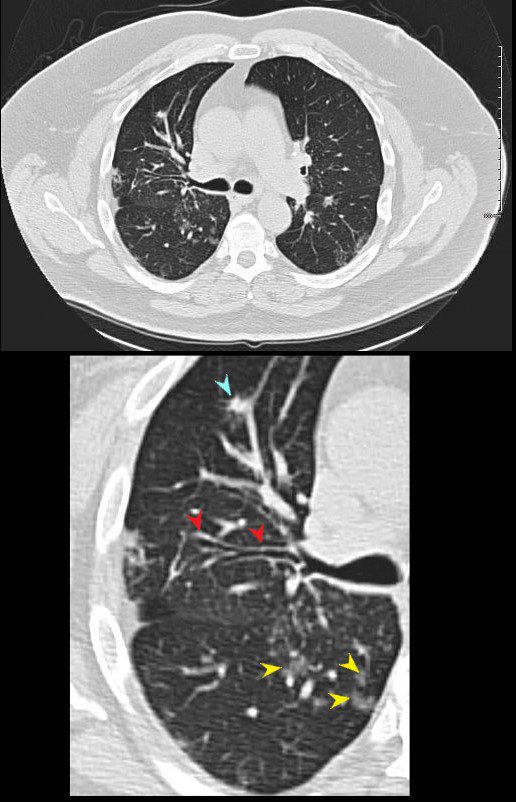
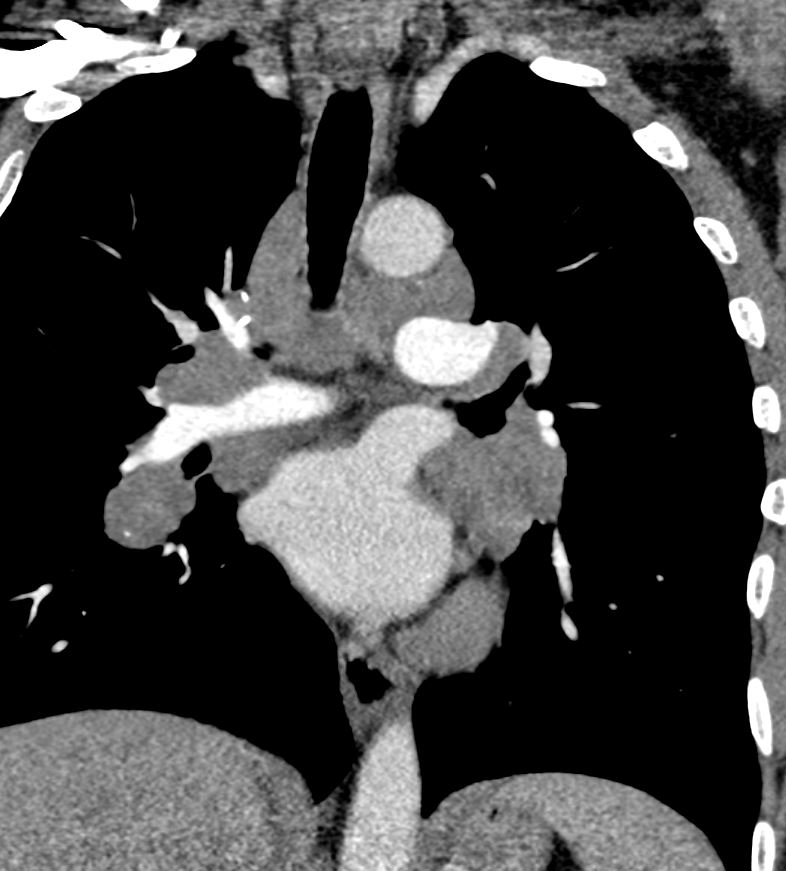
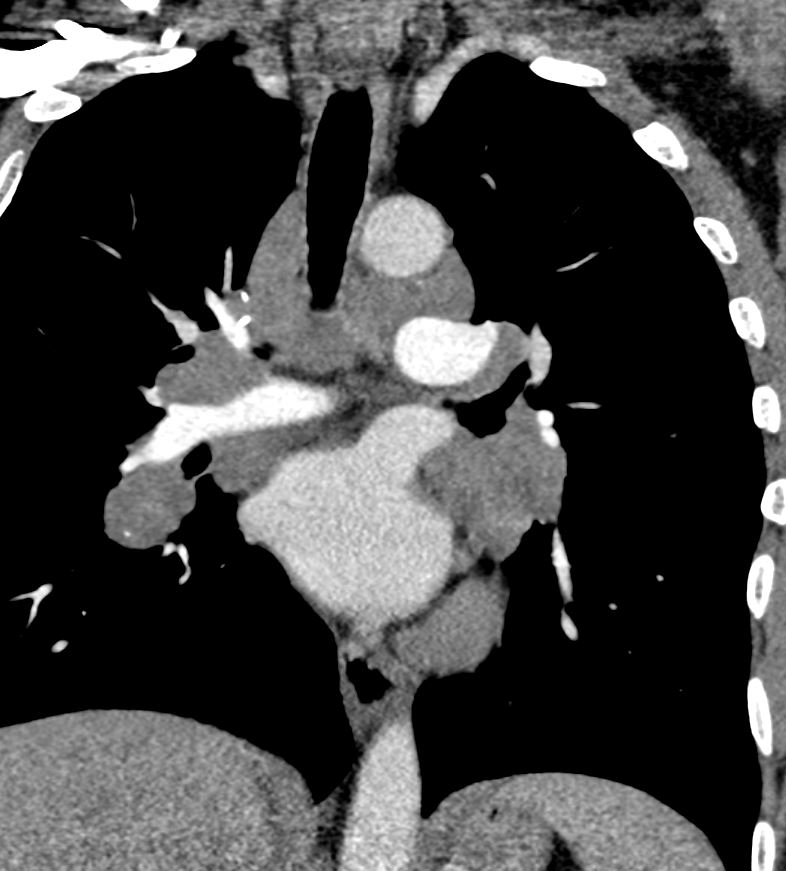
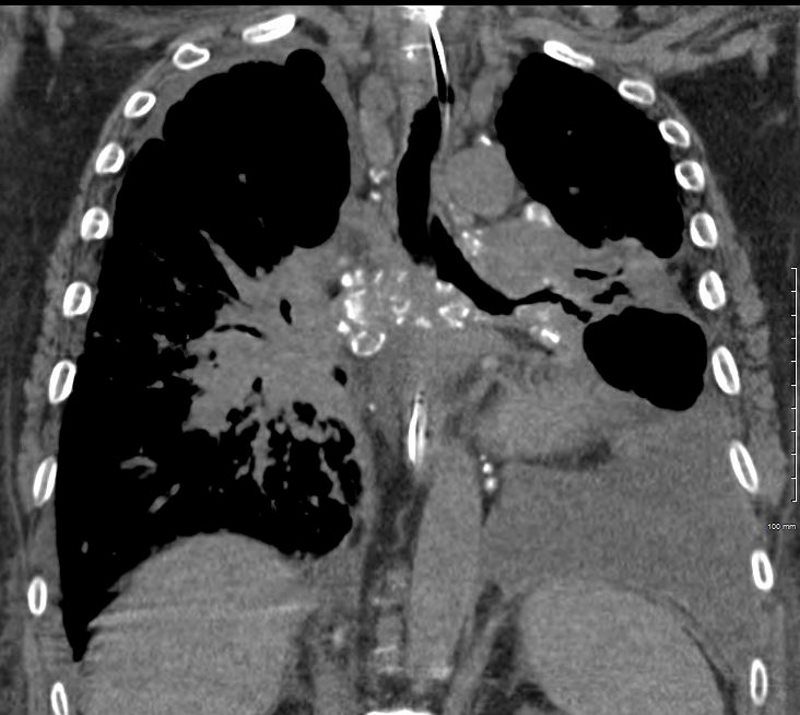
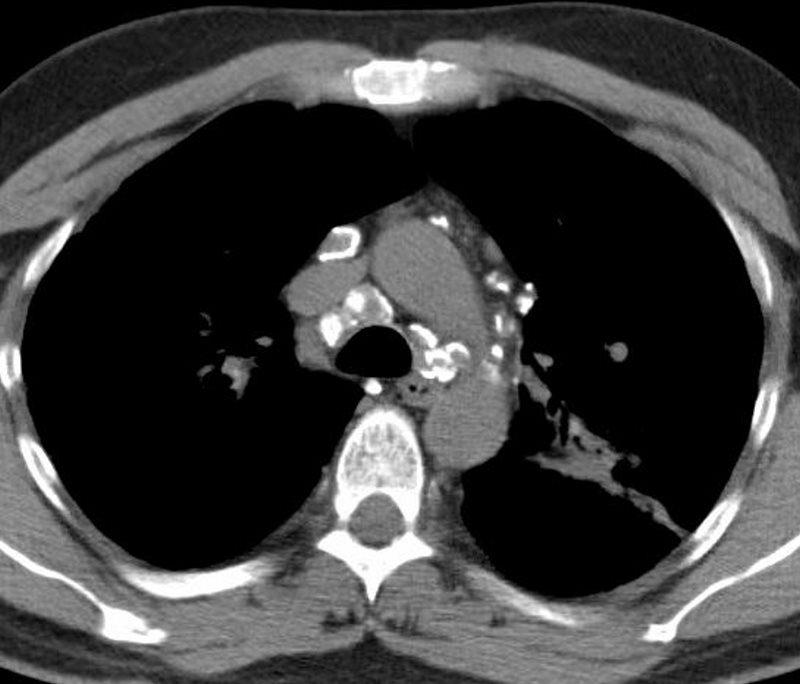
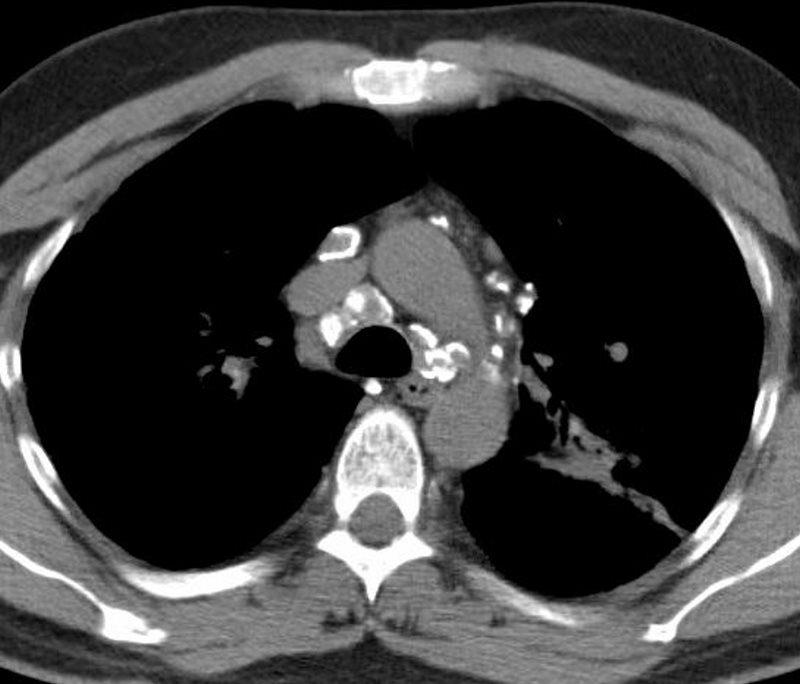
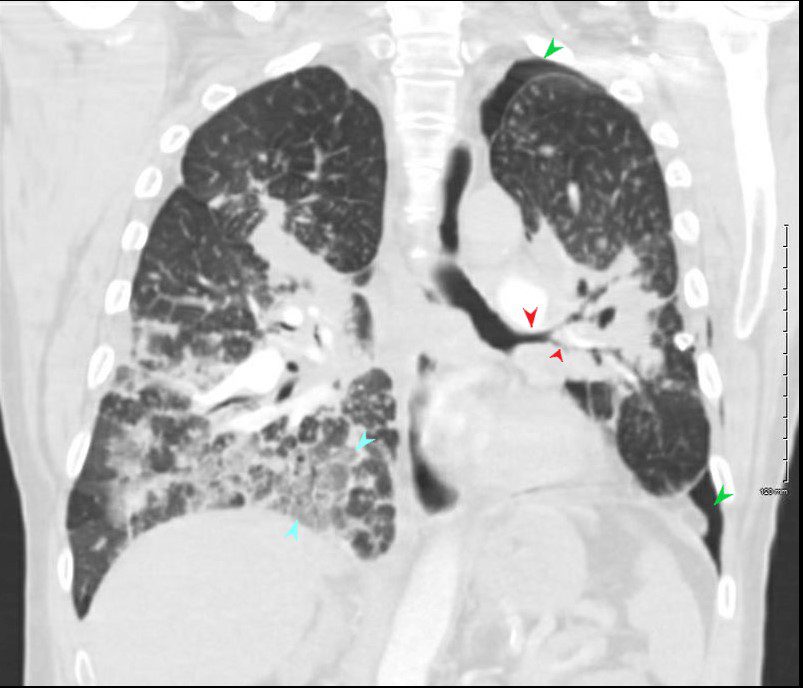
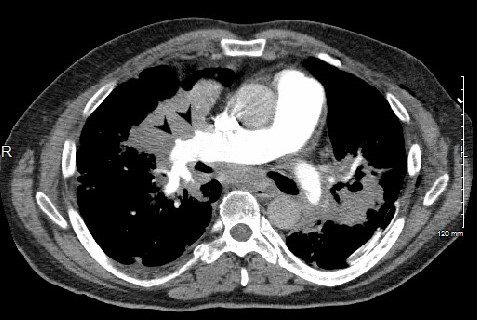
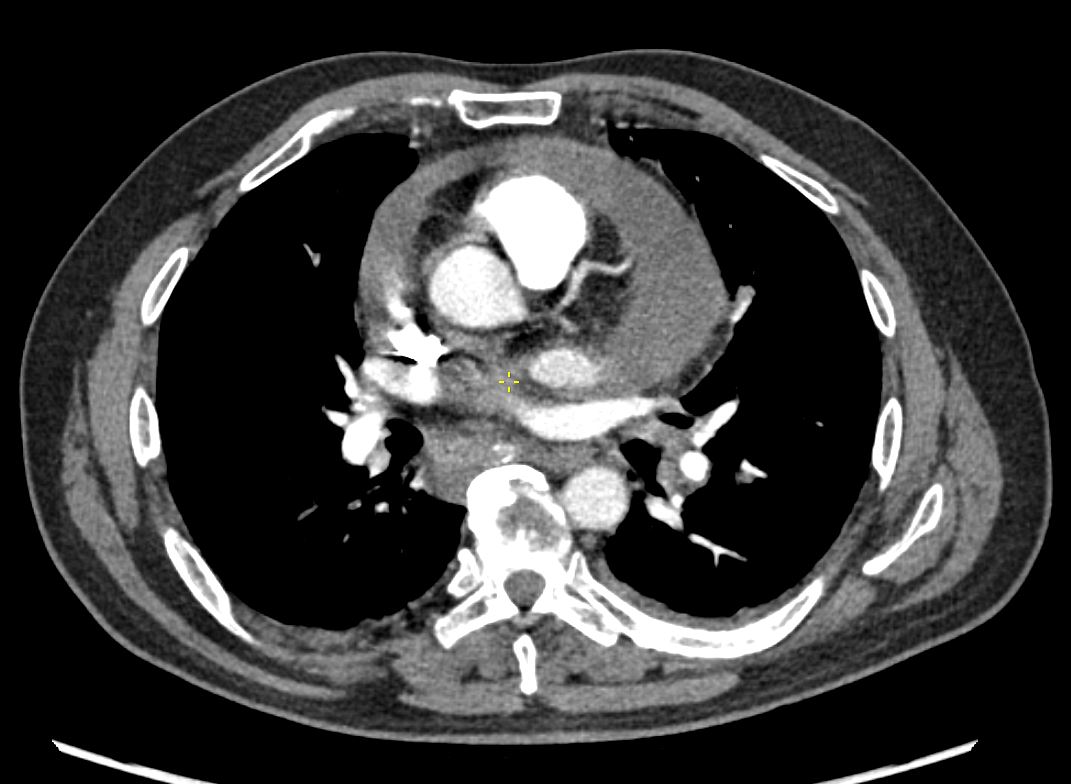
50-year-old male presents with history of Stage 4 sarcoidosis acute chest pain and dyspnea
The initial CXR shows a left sided pneumothorax, diffuse nodular pattern with confluent perihilar infiltrates and a left pleural effusion
A chest tube was placed and a chest CT showed confluent fibrotic masses in the hilar regions totally surrounding the bronchovascular bundles with encasement of the middle lobe artery. In addition, multiple lymphovascular micronodules are demonstrated. The pulmonary artery measures 32.7mm indicating pulmonary hypertension.
A CXR during this admission shows re-expansion of the pneumothorax. Left lung volume is reduced.
The patient presents 2 years later, again with progressive dyspnea and chest pain and CT PA shows encasement of the airways, right middle lobe pulmonary artery and left lower pulmonary vein by the fibrotic broncho vascular masses, and non-occlusive, subacute pulmonary embolus of the LPA. There are moderate bilateral pleural effusions, calcified lymph nodes, with ongoing pulmonary hypertension with right ventricular enlargement, right atrial enlargement, tricuspid regurgitation and pulmonary hypertension. At this time the patient is intubated.
He again presents 1 month after with chest pain and dyspnea. At this time, he has a tracheostomy. The scout frontal view shows persistent encasement of the left upper lobe bronchus and significant reduction on the volume of the left lung with elevated left hemidiaphragm.
CT PA has similar findings with a large right pleural effusion and unresolved large non occlusive thrombus in the left pulmonary artery.
Ashley Davidoff MD TheCommonVein.net 132195.8L
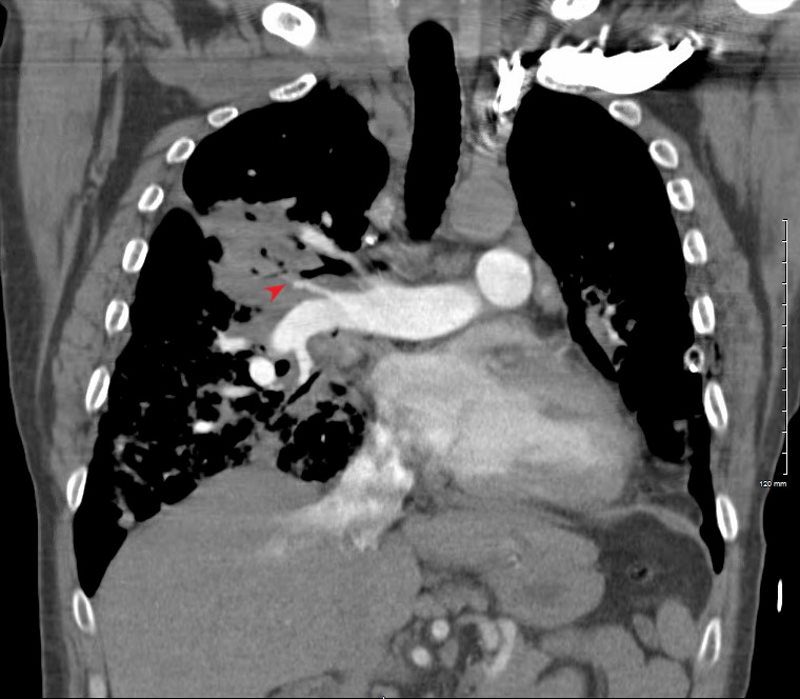
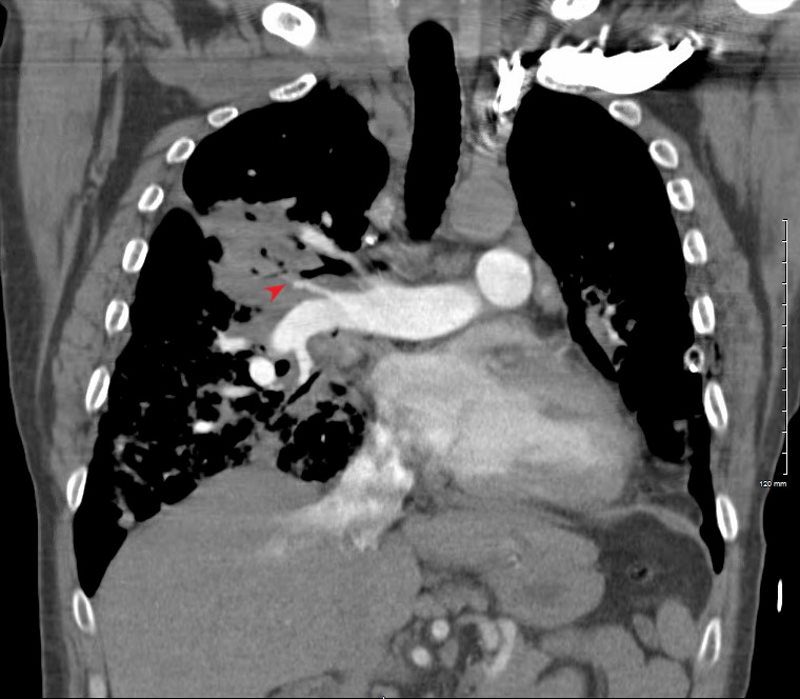
50-year-old male presents with history of Stage 4 sarcoidosis acute chest pain and dyspnea
The initial CXR shows a left sided pneumothorax, diffuse nodular pattern with confluent perihilar infiltrates and a left pleural effusion
A chest tube was placed and a chest CT showed confluent fibrotic masses in the hilar regions totally surrounding the bronchovascular bundles with encasement of the middle lobe artery. In addition, multiple lymphovascular micronodules are demonstrated. The pulmonary artery measures 32.7mm indicating pulmonary hypertension.
A CXR during this admission shows re-expansion of the pneumothorax. Left lung volume is reduced.
The patient presents 2 years later, again with progressive dyspnea and chest pain and CT PA shows encasement of the airways, right middle lobe pulmonary artery and left lower pulmonary vein by the fibrotic broncho vascular masses, and non-occlusive, subacute pulmonary embolus of the LPA. There are moderate bilateral pleural effusions, calcified lymph nodes, with ongoing pulmonary hypertension with right ventricular enlargement, right atrial enlargement, tricuspid regurgitation and pulmonary hypertension. At this time the patient is intubated.
He again presents 1 month after with chest pain and dyspnea. At this time, he has a tracheostomy. The scout frontal view shows persistent encasement of the left upper lobe bronchus and significant reduction on the volume of the left lung with elevated left hemidiaphragm.
CT PA has similar findings with a large right pleural effusion and unresolved large non occlusive thrombus in the left pulmonary artery.
Ashley Davidoff MD
Ashley Davidoff MD
SARCOIDOSIS, STAGE IV, PTX, ENCASEMENT
Ashley Davidoff MD
SARCOIDOSIS, STAGE IV, PTX, ENCASEMENT
Ashley Davidoff MD
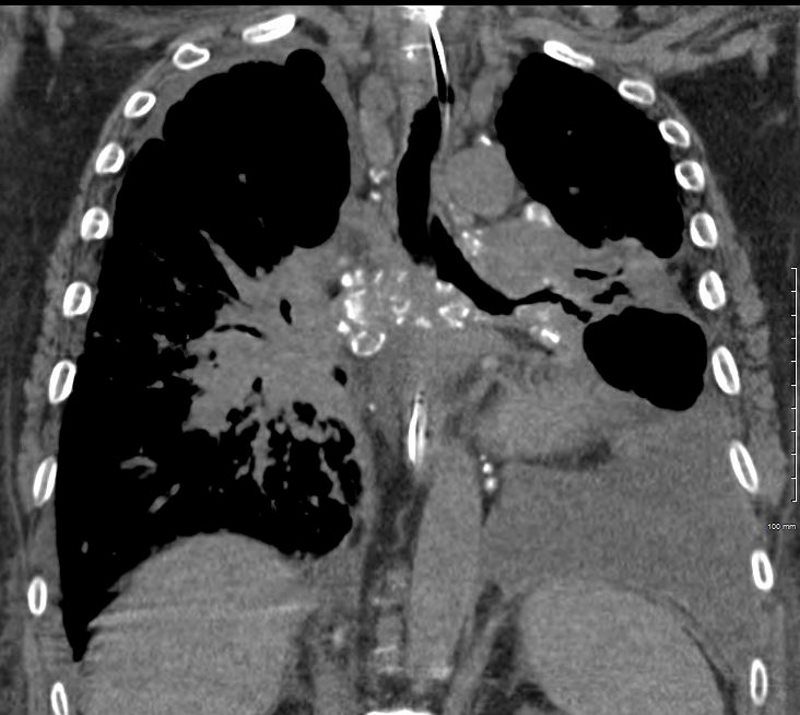
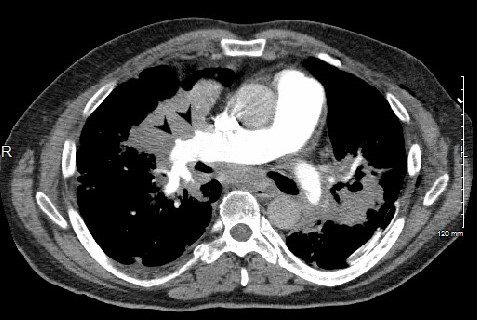
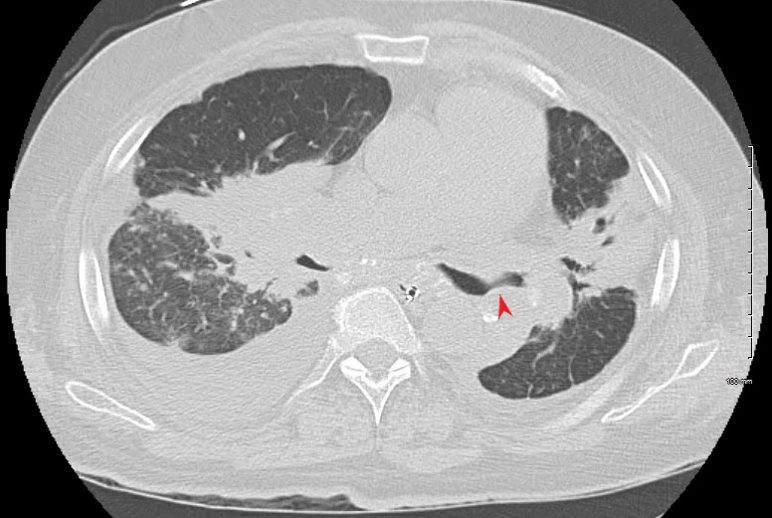
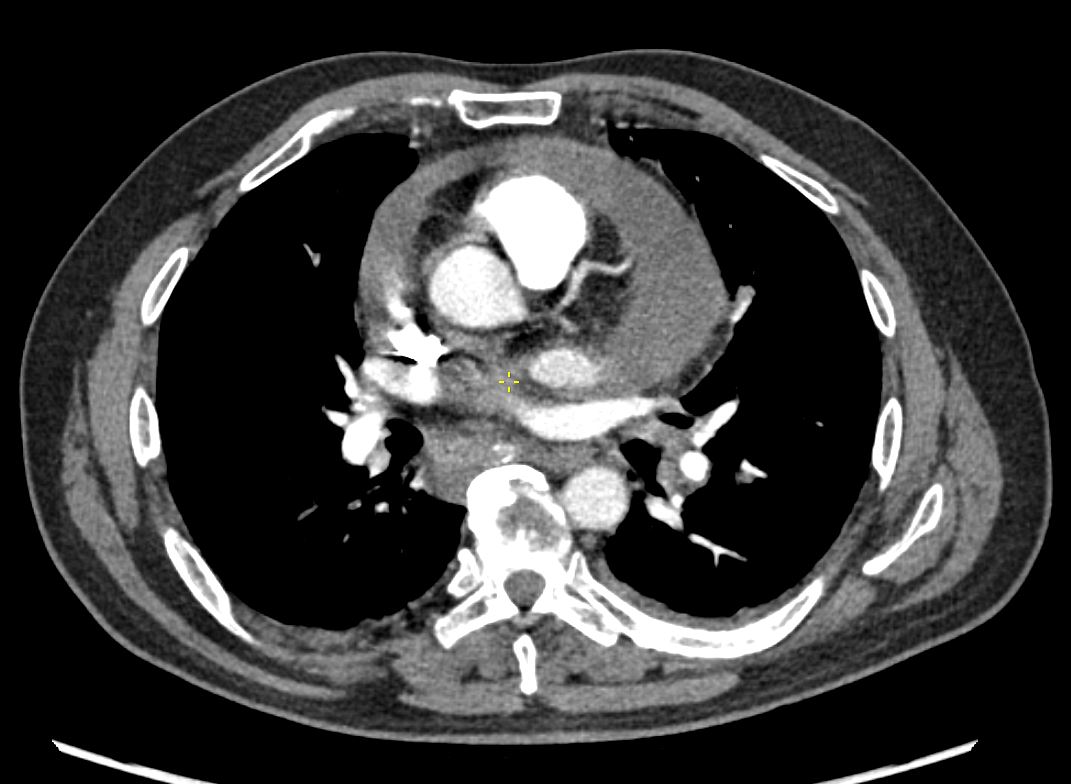
Pulmonary Artery Encasement
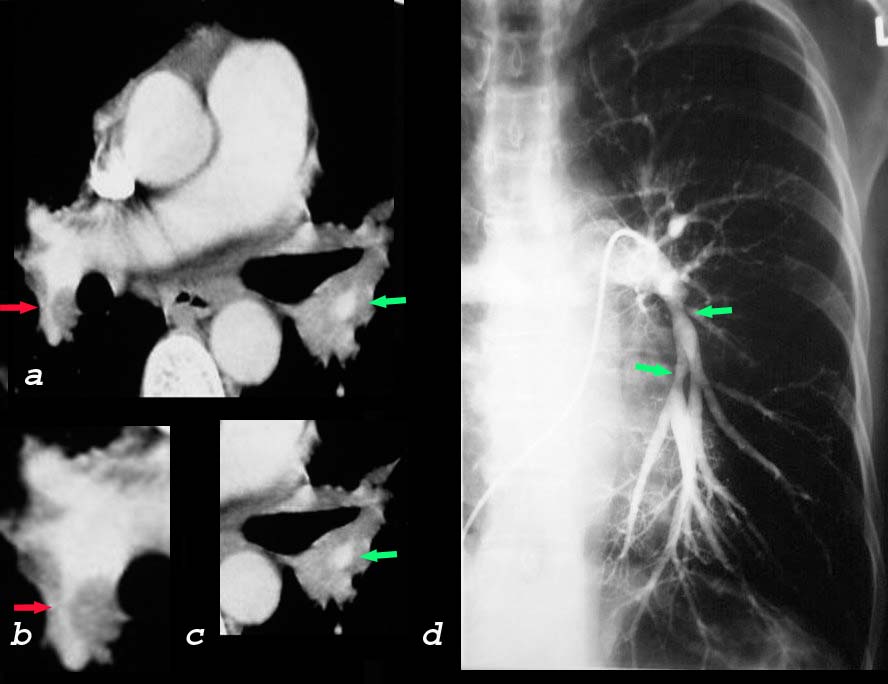
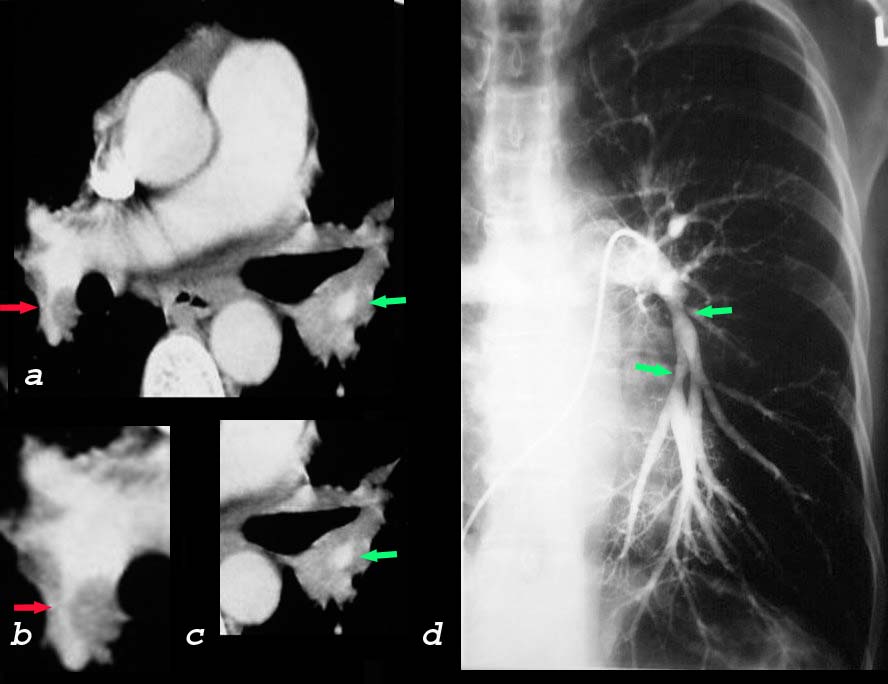
47 year old female with sarcoidosis, a V/Q scan with high probability and an angiogram showing encasement of the pulmonary arteries by the central granulomatous process
CT (a,b, c) shows encasement and narrowing of the descending right pulmonary artery red arrows (a,b) and of the left descending artery on CT (green arrows a,b) and on the pulmonary angiogram (green arrow d)
Courtesy Priscilla Slanetz MD MPH
TheCommonVein.net 31946cL
Cystic Form of Sarcoidosis
End Stage Sarcoidosis
Diffuse Interstitial Fibrosis
Ashley Davidoff TheCommonVein.net 31919
Small Airways
Secondary Lobules
Interlobular Septa
Intralobular Disease
Heart
Sarcoidosis and Pericarditis
48 year old woman with path proven sarcoidosis of the lung presents with a moderate sized pericardial effusion. There is enhancement of the pericardium anterolaterally characterized by enhancing pericardium. Echo showed no tamponade. She was treated with anti-inflammatory medications and the pericardial effusion resolved . tentative diagnosis of pericarditis secondary to sarcoidosis
Spleen
Liver
Nodules