Etymology
- Derived from the Greek words bronchion, meaning “small airway,” and ektasis, meaning “expansion.” The term refers to abnormal, permanent dilation of the bronchioles.
AKA
- Small airway dilation
What is it?
- Bronchiolectasis is a condition characterized by abnormal, permanent dilation of the bronchioles due to destruction of their walls, often in association with chronic inflammatory or fibrotic lung diseases.
- Bronchiolectasis is a condition characterized by abnormal, permanent dilation of the bronchioles due to destruction of their walls, often in association with chronic inflammatory or fibrotic lung diseases.
Caused by:
- Most common causes:
- Chronic inflammatory processes in the lungs
- Fibrotic lung diseases (e.g., idiopathic pulmonary fibrosis, hypersensitivity pneumonitis)
- Less common causes:
- Infection:
- Tuberculosis
- Nontuberculous mycobacterial infections
- Inflammation:
- Chronic bronchitis
- Connective tissue diseases (e.g., rheumatoid arthritis)
- Immune:
- Immune deficiency syndromes (e.g., common variable immunodeficiency)
- Neoplasm:
- Post-obstructive processes due to tumors
- Mechanical:
- Bronchial obstruction causing distal airway dilation
- Trauma:
- Radiation-induced lung injury
- Inherited and Congenital:
- Primary ciliary dyskinesia
- Cystic fibrosis
- Other:
- Aspiration-induced damage
- Infection:
Resulting in:
- Chronic small airway damage and dilation
- Impaired mucociliary clearance
- Increased risk of recurrent infections and inflammation
Structural Changes:
- Irreversible dilation of bronchioles
- Loss of elastic and muscular support in the bronchiolar walls
- Mucus plugging and potential air trapping
Pathophysiology:
- Bronchiolectasis develops due to persistent inflammation or mechanical obstruction that leads to destruction of the elastic and muscular layers of the bronchioles. This results in their dilation and loss of structural integrity, contributing to mucus stasis and recurrent infections. Fibrotic processes in adjacent lung tissue often contribute to the traction and further dilation of bronchioles.
Pathology:
- Dilated bronchioles with thickened walls
- Chronic inflammatory infiltrates
- Adjacent fibrosis or scarring
Diagnosis
Clinical:
- Symptoms vary depending on the underlying condition:
- Chronic cough
- Dyspnea
- Recurrent respiratory infections
- Hemoptysis may occur in advanced disease
Radiology:
- CXR:
- Often non-specific but may show hyperinflation or fibrotic changes
- Subtle interstitial markings in advanced cases
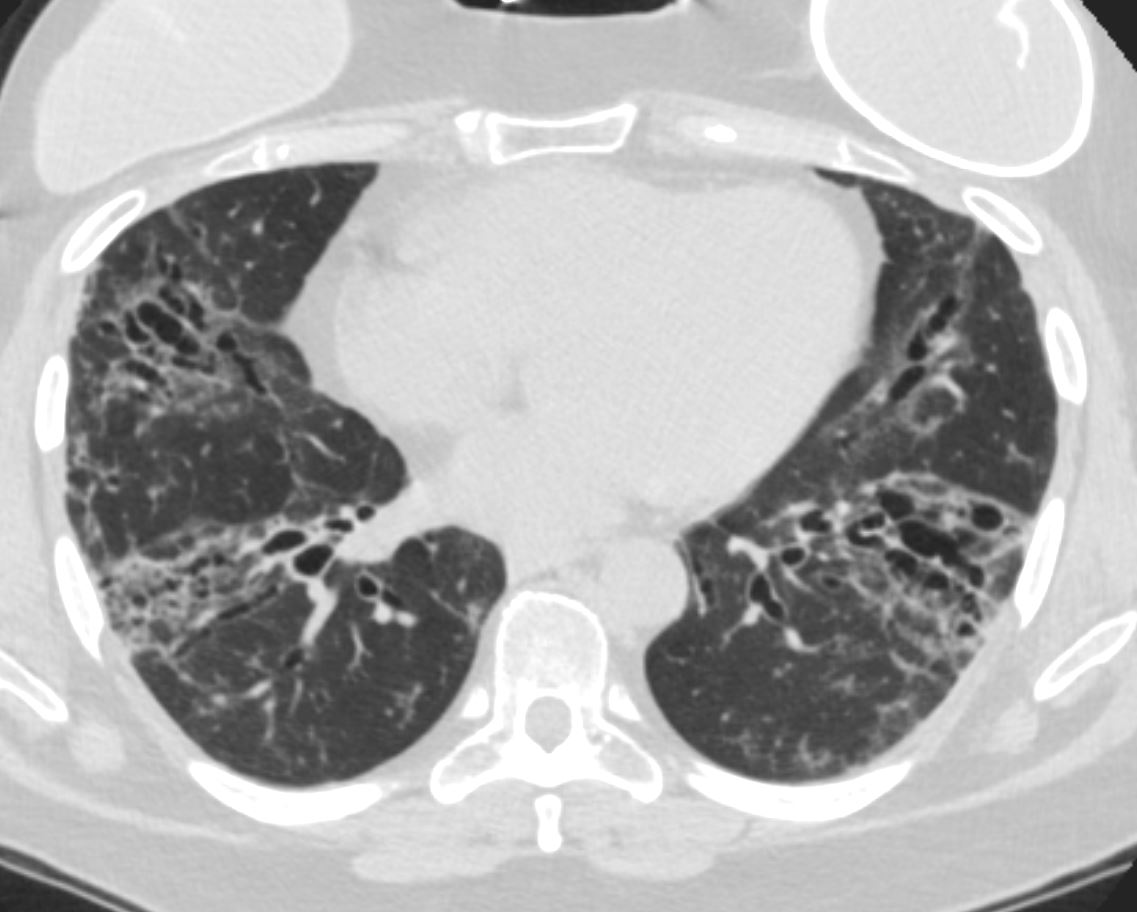
- CT of the Chest:
- Irregular, tubular structures in the peripheral lung zones
- Air trapping and small cyst-like dilations of bronchioles
- Associated findings of interstitial fibrosis or mosaic attenuation
Labs:
- Sputum cultures to identify infective organisms
- Tests for autoimmune diseases or immune deficiencies when indicated
Management:
- Treatment of underlying conditions:
- Anti-inflammatory therapies (e.g., corticosteroids) for fibrotic or autoimmune causes
- Antibiotics for recurrent infections
- Airway clearance techniques:
- Chest physiotherapy
- Bronchodilators in cases of concurrent airway obstruction
- Advanced interventions:
- Lung transplantation in end-stage disease
Radiology Detail
CXR
Findings:
- Subtle interstitial or fibrotic changes
- Hyperinflation in associated obstructive diseases
Associated Findings:
- Small cyst-like air spaces in advanced disease
CT of the Chest
Parts:
- Peripheral bronchioles, predominantly in fibrotic regions
Size:
- Small, tubular, or cystic dilations of bronchioles
- Under normal conditions, bronchioles less than 2 mm in diameter and located in the peripheral regions of the lung are not visible on CT. When their walls become thickened or they enlarge, they become visible, which by definition represents bronchiolectasis.
Shape:
- Irregular, beaded, or saccular dilations
Position:
- Most commonly seen in peripheral and lower lung zones
Character:
- Thickened bronchiolar walls
- Traction bronchiolectasis in fibrotic areas
Time:
- Chronic progression with periods of acute exacerbation
Associated Findings:
- Interstitial fibrosis, mosaic attenuation, or air trapping
Other relevant Imaging Modalities
MRI/PET CT/NM/US/Angio:
- MRI: Rarely used but may identify associated soft tissue abnormalities
- PET-CT: Useful in distinguishing active inflammation from fibrosis
Pulmonary Function Tests (PFTs):
- May show restrictive, obstructive, or mixed patterns depending on the underlying condition
Recommendations:
- Use CT of the Chest to confirm the diagnosis and evaluate the extent of bronchiolectasis
- Address underlying causes with targeted therapy
- Implement airway clearance and infection control measures
Key Points and Pearls:
- Bronchiolectasis refers to permanent dilation of bronchioles, often associated with chronic inflammatory or fibrotic lung diseases.
- CT of the Chest is the gold standard for identifying small airway dilations and associated findings. Under normal conditions, bronchioles less than 2 mm in diameter and located in the peripheral regions of the lung are not visible on CT. When their walls become thickened or they enlarge, they become visible, which by definition represents bronchiolectasis.
- Traction bronchiolectasis is a key feature in fibrotic lung diseases.
- Management focuses on treating the underlying condition, maintaining airway clearance, and preventing recurrent infections.
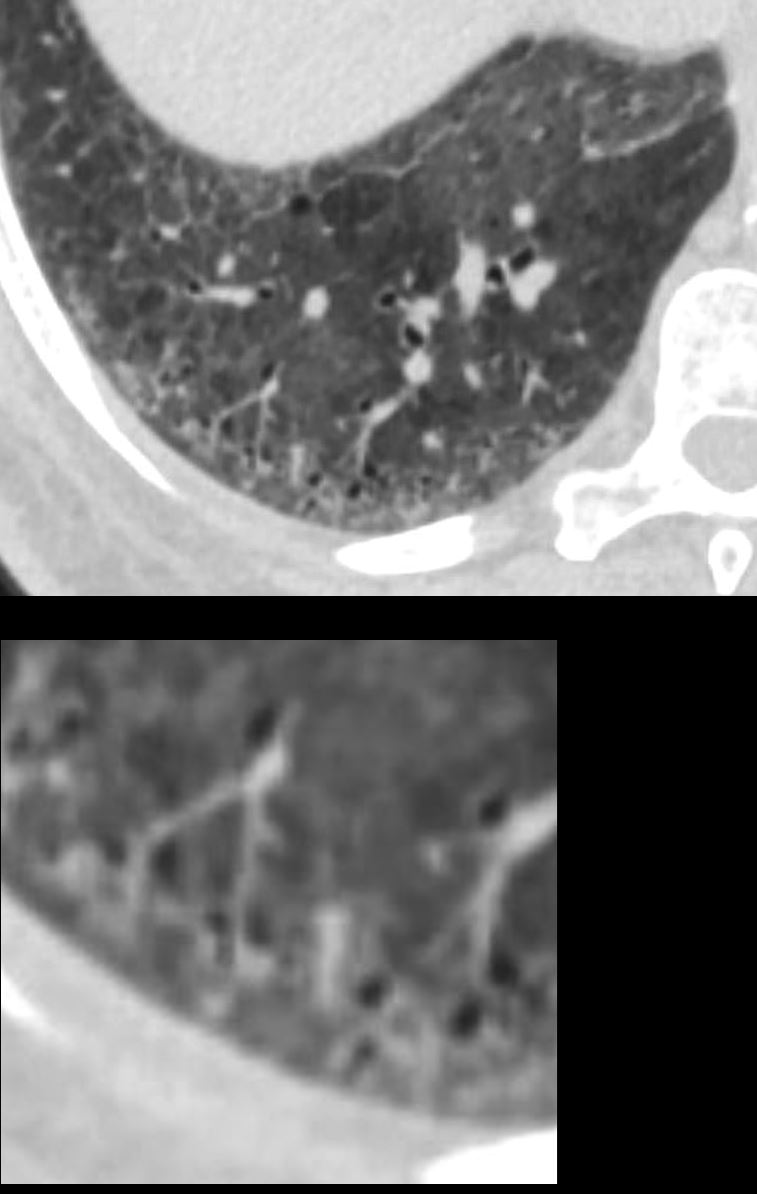
51-year-old female smoker with a history of COPD asthma and pulmonary hypertension presents with progressive dyspnea. Axial CT through the right posterior recess shows patchy ground glass changes with some regions of mosaicism. The bronchovascular bundle subtending 2 secondary lobules is highlighted in the lower panel. The centrilobular arteriole and ectatic bronchiole are magnified
Pathology confirmed a diagnosis of DIP
Ashley Davidoff MD TheCommonVein.net 252Lu 135981c
Ashley Davidoff MD TheCommonVein.net
Links and References
Fleischner Society
bronchiolectasis
Pathology.—Bronchiolectasis is defined as dilatation of bronchioles. It is caused by inflammatory airways disease (potentially reversible) or, more frequently, fibrosis.
CT scans.—When dilated bronchioles are filled with exudate and are thick walled, they are visible as a tree-in-bud pattern or as centrilobular nodules (,31,,32). In traction bronchiolectasis, the dilated bronchioles are seen as small, cystic, tubular airspaces, associated with CT findings of fibrosis (,Fig 12). (See also traction bronchiectasis and traction bronchiolectasis, tree-in-bud pattern.)
