Cavitating Mass in the Lungs
- What is it:
- A cavitating mass in the lungs is a localized area of abnormal tissue growth with central necrosis or liquefaction, leading to the formation of an air- or fluid-filled cavity.
- Cavitation is typically seen within a lung mass due to infection, malignancy, or other pathological processes.
- Etymology:
- The term “cavitation” derives from the Latin word cavus, meaning “hollow,” describing the cavity formation within the mass.
- AKA:
- Cavitary lesion, cavitating tumor (if malignancy is suspected).
- How does it appear on each relevant imaging modality:
- Chest CT (preferred):
- Parts: A thick-walled mass with a central cavity containing air, fluid, or both.
- Size: Variable, depending on the underlying etiology.
- Shape: Irregular or round margins with a cavity inside.
- Position: May be central, peripheral, or in association with pre-existing lung pathology.
- Character:
- Wall thickness: Malignancies usually have thicker walls (>15 mm), while benign lesions often have thinner walls (<5 mm).
- Presence of air-fluid levels: Indicates communication with the bronchial tree or superimposed infection.
- Adjacent findings: Possible surrounding ground-glass opacities, consolidation, or lymphadenopathy.
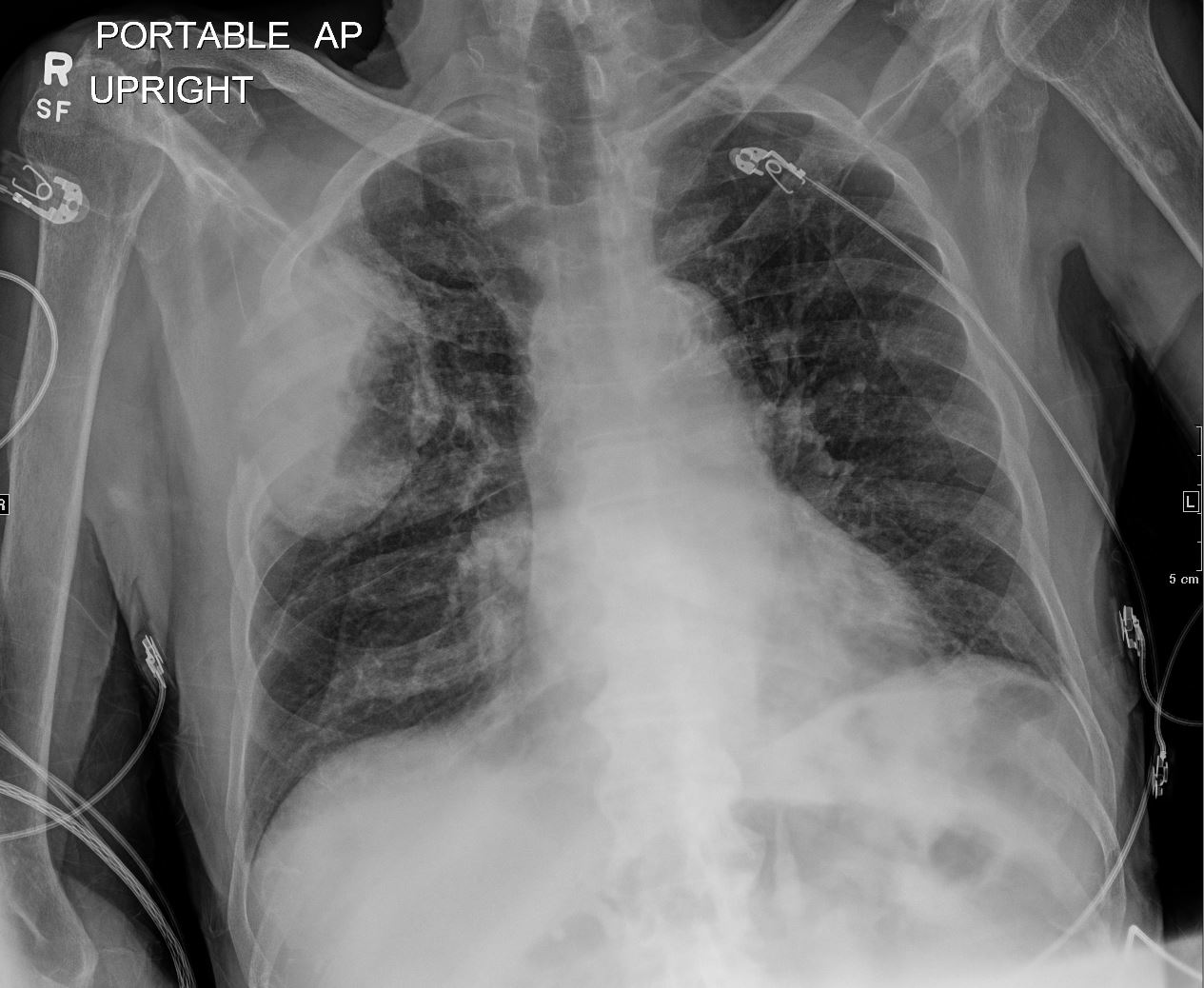
- Chest X-ray:
- Appears as a thick-walled mass with a radiolucent center.
- May show air-fluid levels.
- Limited sensitivity for subtle features compared to CT.
- PET-CT:
- Increased metabolic activity (high SUV) is suggestive of malignancy.
- Benign processes like infections may also show moderate uptake.
- Ultrasound:
- Rarely used but may show a hypoechoic lesion with internal air or fluid (pleural-based masses).
- Chest CT (preferred):
- Differential diagnosis:
- Infectious:
- Pulmonary abscess.
- Tuberculosis with cavitation.
- Fungal infections (e.g., aspergillosis, histoplasmosis).
- Neoplastic:
- Primary lung cancer with necrosis (e.g., squamous cell carcinoma).
- Metastatic disease with cavitation (e.g., squamous carcinoma, sarcomas).
- Inflammatory: Rheumatoid nodule, Wegener’s granulomatosis (GPA).
- Trauma: Post-traumatic hematoma with secondary infection.
- Congenital: Bronchogenic cyst with secondary infection.
- Infectious:
- Recommendations:
- Further evaluation:
- Contrast-enhanced CT to better characterize the lesion and identify vascularity or bronchial communication.
- PET-CT for metabolic assessment if malignancy is suspected.
- Bronchoscopy for direct visualization and biopsy.
- CT-guided biopsy for histopathological and microbiological analysis.
- Follow-up imaging:
- Short-interval CT for indeterminate lesions.
- Clinical correlation:
- Consider recent infections, malignancy risk factors (e.g., smoking), or autoimmune diseases.
- Further evaluation:
- Key considerations and pearls:
- Wall thickness is a key feature to distinguish between benign and malignant causes.
- Air-fluid levels often suggest infection but can also be seen in necrotic tumors.
- Adjacent findings, such as lymphadenopathy or invasion of surrounding structures, favor malignancy.
- Cavitation in squamous cell carcinoma is a classic finding, especially in smokers.
- Superimposed infection can complicate interpretation and management, especially in immunocompromised patients.
This structured format provides clarity and guidance for interpreting cavitating masses in the lungs.
CXR
Ashley Davidoff MD
TheCommonVein.net

CT Pre XRT
Ashley Davidoff MD
TheCommonVein.net
