Methotrexate Lung Disease (Methotrexate-Induced Pneumonitis)
Etymology:
Named after methotrexate, an immunosuppressive and chemotherapeutic agent, and its association with pulmonary toxicity.
AKA:
- Methotrexate-induced pneumonitis.
- Methotrexate pulmonary toxicity.
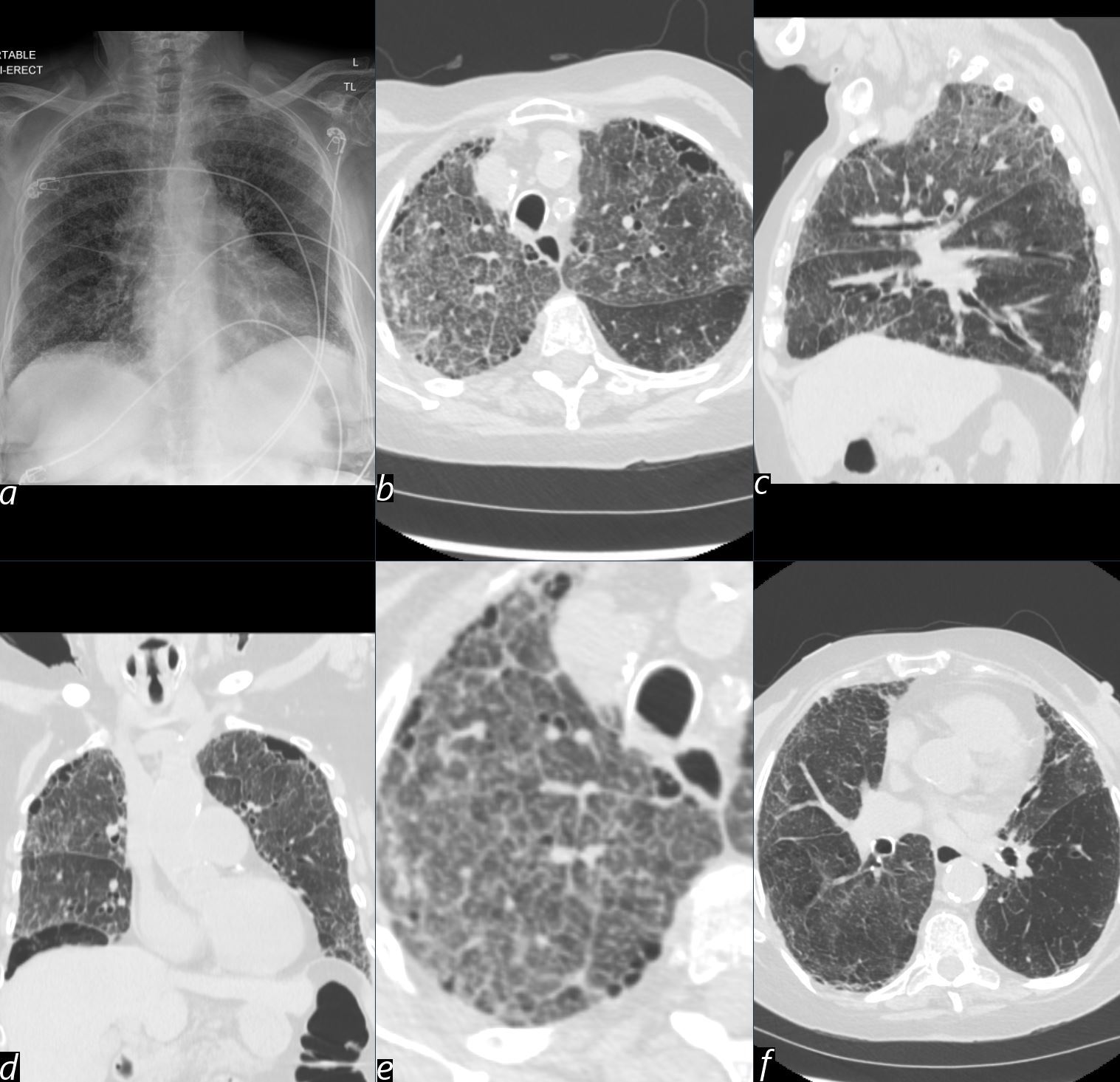
An 89-year-old female with a known diagnosis of rheumatoid arthritis presents with shortness of breath and cough.
Findings
• (a) Frontal chest radiograph reveals a diffuse interstitial pattern, setting the stage for further CT analysis.
• (b, e) Axial CT through the upper lobes (magnified in e), demonstrates a crazy paving pattern, characterised by ….. and a hallmark of alveolar and interstitial involvement.
• (c) Sagittal CT reconstruction highlights the upper lobe predominance of the crazy paving pattern.
• (d) Coronal CT shows ground-glass changes extending into the middle lobe and lingula, reflecting more diffuse involvement.
• (f) Axial CT through the lower lobes demonstrates relative sparing, which helps narrow the differential diagnosis.
Comment
The crazy paving pattern reflects a combination of alveolar damage and interstitial involvement. Methotrexate pneumonitis most commonly involves the upper lobes, but the pattern of involvement, including sparing of the lower lobes, provides valuable diagnostic clues. Other imaging findings may include consolidation, mosaic attenuation, or airspace nodules.
Differential diagnosis includes other drug-induced pneumonitis, infections (e.g., pneumocystis pneumonia), and interstitial lung diseases such as hypersensitivity pneumonitis. Early recognition of these imaging features is critical, particularly in patients on methotrexate therapy, to prevent further progression and complications.
Ashley Davidoff MD TheCommonVein.net (b12389)
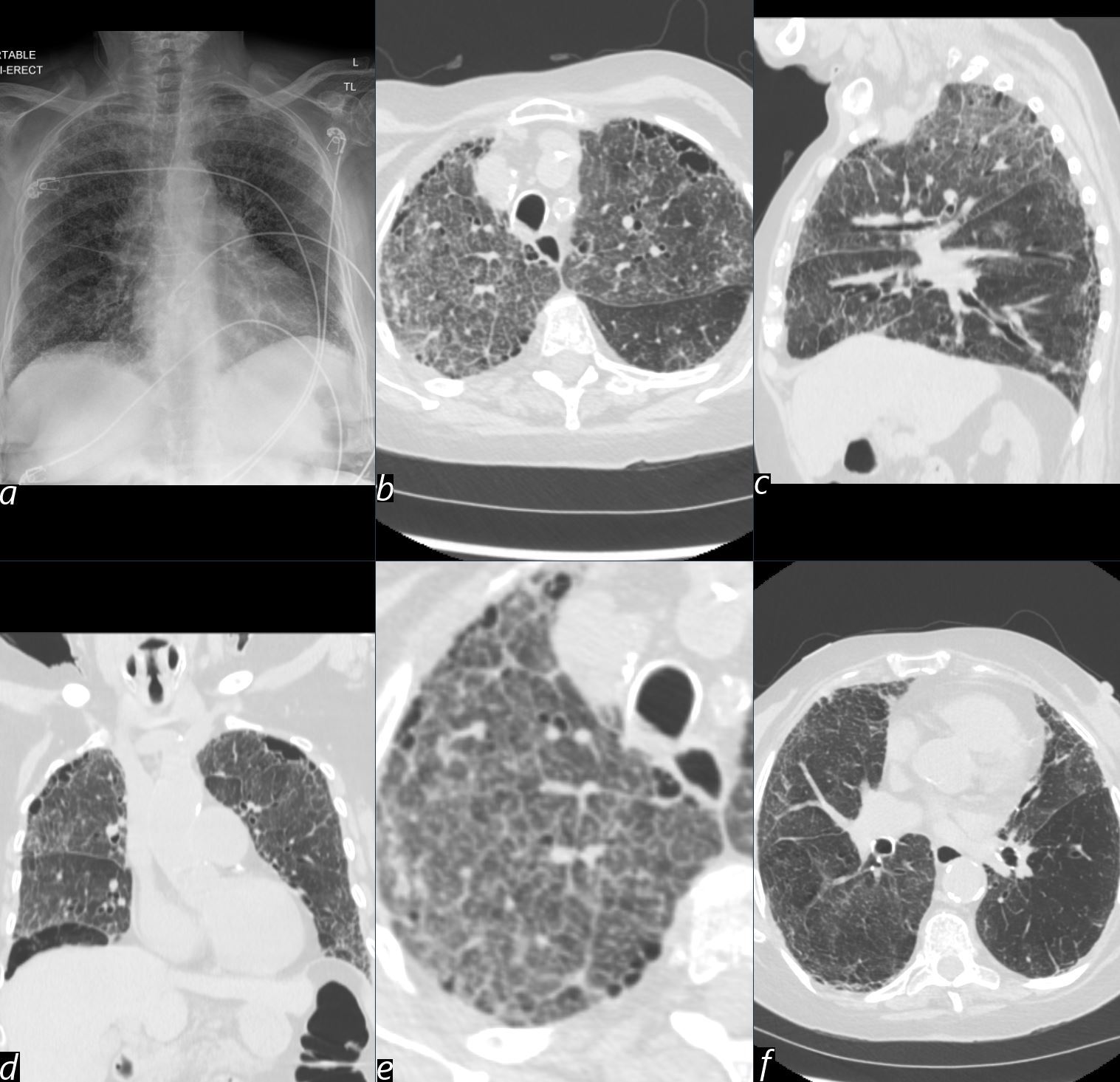
An 89-year-old female with a known diagnosis of rheumatoid arthritis presents with shortness of breath and cough.
Findings
(a) Frontal chest radiograph reveals a diffuse interstitial pattern, setting the stage for further CT analysis.
(b, e) Axial CT through the upper lobes (magnified in e) demonstrates a crazy paving pattern, characterized by ground-glass opacities and interlobular septal thickening, a hallmark of alveolar and interstitial involvement.
(c) Sagittal CT reconstruction highlights the crazy paving pattern, with diffuse involvement across the lungs.
(d) Coronal CT shows ground-glass changes extending into the middle lobe and lingula, reflecting more widespread involvement.
(f) Axial CT through the lower lobes demonstrates no significant sparing, with diffuse changes present throughout the lungs.
Comment
Methotrexate-induced pneumonitis typically presents with bilateral, diffuse involvement across the lungs. While imaging findings can occasionally appear more prominent in one region (e.g., upper or lower lobes), the overall pattern generally lacks a strong regional preference. In some cases, involvement of the lower lung fields may be observed, further emphasizing the diffuse nature of the disease.
The characteristic crazy paving pattern, as seen here, reflects a combination of alveolar damage and interstitial involvement. Other findings may include consolidation, mosaic attenuation, or airspace nodules.
Differential diagnosis includes other drug-induced pneumonitis, infections (e.g., pneumocystis pneumonia), and interstitial lung diseases such as hypersensitivity pneumonitis. Early recognition of these imaging features is critical, particularly in patients on methotrexate therapy, to prevent further progression and complications.
Ashley Davidoff MD TheCommonVein.net (b12389)
What is it?
A rare, potentially life-threatening hypersensitivity reaction or toxic response of the lungs to methotrexate, resulting in inflammation and interstitial damage.
Caused by:
- Methotrexate therapy, typically in the context of treatment for autoimmune diseases (e.g., rheumatoid arthritis) or certain cancers.
Most common:
- Trigger: Methotrexate use, even at low doses.
- Population: More frequent in older adults and those with preexisting lung disease.
Based on Categories
Inflammation/Immune:
- Hypersensitivity reaction leading to interstitial inflammation and alveolitis.
Idiopathic:
- Exact mechanism remains unclear but is suspected to involve immune dysregulation and direct cytotoxic effects.
Resulting in:
- Acute or subacute onset of diffuse interstitial lung disease (ILD).
- Impaired oxygen exchange due to alveolar inflammation.
Structural Changes:
Parts:
- Primarily involves the lung interstitium and alveoli.
Size:
- Diffuse involvement, often bilaterally.
Shape:
- Irregular areas of ground-glass opacities and consolidation.
Position:
- Typically diffuse, but lower lobe predominance may occur.
Character:
- Acute inflammation with potential for progression to fibrosis.
Time:
- Onset is usually subacute, occurring weeks to months after starting methotrexate.
Pathophysiology:
- Hypersensitivity reaction leads to immune-mediated alveolitis.
- Methotrexate may also exert direct toxic effects on pulmonary cells, leading to apoptosis and interstitial inflammation.
Other Relevant Basic Science Application:
- Folate antagonist activity of methotrexate may impair cellular repair processes in the lungs.
Diagnosis:
Clinical:
- Symptoms: Acute or subacute onset of dyspnea, non-productive cough, fever, and fatigue.
- Physical Exam: Inspiratory crackles and hypoxemia.
Radiology:
X-Ray:
Findings:
- Diffuse or patchy bilateral interstitial opacities.
Associated Findings:
- Volume loss in advanced cases.
CT:
Findings:
- Ground-glass opacities, reticulation, and areas of consolidation.
- May mimic NSIP or OP patterns.
Associated Findings:
- Bronchial wall thickening and subpleural sparing.
MRI:
Rarely used; findings parallel CT with T2 hyperintensity in inflamed regions.
US:
Findings:
- Thickened pleural lines and subpleural consolidations.
Associated Findings:
- Rarely used in primary diagnosis.
Other Relevant Imaging Modalities:
- PET CT: Hypermetabolic regions in inflamed lung parenchyma (not specific).
Other Diagnostic Procedures:
- Bronchoalveolar lavage (BAL): Lymphocytic predominance supports hypersensitivity pneumonitis.
- Lung biopsy (if needed): Confirms interstitial pneumonitis and alveolitis.
Labs:
- Elevated inflammatory markers (e.g., ESR, CRP).
- Rule out infections with cultures and serologies.
Differential Diagnosis
Most common:
- Hypersensitivity pneumonitis (non-drug related).
- Infection (e.g., Pneumocystis jirovecii pneumonia, bacterial pneumonia).
Categories:
Inflammation/Immune:
- Autoimmune disease-associated ILD (e.g., rheumatoid arthritis).
Idiopathic:
- Idiopathic interstitial pneumonias.
Recommendations:
- Immediate discontinuation of methotrexate.
- Corticosteroid therapy for severe cases.
- Avoid rechallenge with methotrexate due to high risk of recurrence.
Key Points and Pearls:
- Methotrexate-induced lung disease can occur even at low doses and in patients with no prior pulmonary disease.
- Early recognition is crucial, as symptoms may overlap with infection or autoimmune disease flares.
- Ground-glass opacities and interstitial patterns on imaging are key diagnostic clues.
4
