Etymology
Derived from Latin multi- (many) and focus (point), referring to the presence of abnormalities in multiple regions of the lung.
AKA
Multifocal pulmonary abnormalities
What is it?
Multifocal lung findings describe radiologic or pathologic abnormalities occurring in multiple discrete locations within the lung parenchyma. These findings may result from infectious, inflammatory, neoplastic, or vascular processes and are identified on imaging modalities such as chest X-ray (CXR) and computed tomography (CT).
Characterized by:
- Radiologic appearance:
- Multiple areas of abnormal opacities or lesions.
- Distribution may be random, centrilobular, perilymphatic, or peripheral, depending on the underlying etiology.
- Findings may include nodules, ground-glass opacities, consolidations, cavitations, or a mixture of these.
Caused by:
- Most common causes:
- Infectious:
- Bacterial pneumonia (e.g., Staphylococcus aureus, Pseudomonas spp.).
- Fungal infections (e.g., Aspergillosis, Histoplasmosis).
- Mycobacterial infections (e.g., Tuberculosis, nontuberculous mycobacteria).
- Viral infections (e.g., Influenza, COVID-19).
- Neoplastic:
- Metastatic disease (e.g., breast, colorectal, renal cell carcinoma).
- Primary multifocal lung cancer (e.g., multifocal adenocarcinoma in situ).
- Inflammatory/Immune:
- Hypersensitivity pneumonitis.
- Granulomatosis with polyangiitis (Wegener’s).
- Sarcoidosis.
- Connective tissue disease-associated interstitial lung disease (CTD-ILD).
- Other:
- Pulmonary hemorrhage syndromes.
- Drug-induced lung injury.
- Infectious:
Resulting in:
- Impaired gas exchange due to widespread parenchymal involvement.
- Symptoms such as dyspnea, cough, fever, and hemoptysis.
Structural changes:
- Multiple discrete or confluent abnormalities affecting the alveoli, airways, or vasculature.
- Structural changes may include nodular thickening, cavitation, fibrosis, or atelectasis.
Pathophysiology:
- Varies depending on the underlying cause:
- Infection: Pathogen-induced inflammation and alveolar filling.
- Neoplasm: Tumor growth and invasion.
- Inflammation: Immune-mediated damage to lung parenchyma or vasculature.
- Vascular: Hemorrhage or embolization.
Pathology:
- Histopathologic findings depend on the etiology:
- Infectious: Neutrophilic infiltration, necrosis, granulomas.
- Neoplastic: Malignant cells, desmoplastic reaction.
- Inflammatory: Non-necrotizing or necrotizing granulomas, fibrosis.
Diagnosis:
- Clinical correlation:
- Symptoms: Dyspnea, cough, fever, weight loss, or hemoptysis.
- History: Occupational exposures, travel, or malignancy.
- Imaging:
-
Radiology Detail:
- CXR:
- Findings: Multiple opacities or nodules; cavitation in some cases.
- Associated Findings: Mediastinal lymphadenopathy, pleural effusion.
- CT:
- Parts: Involves multiple lobes, segments, or subsegments.
- Size: Variable; may include micronodules or larger masses.
- Shape: Round, irregular, or tree-in-bud pattern.
- Position: Random, centrilobular, perilymphatic, or peripheral.
- Character:
- Nodules: Solid, cavitating, or ground-glass.
- Consolidation: Diffuse or patchy.
- Associated Findings: Bronchiectasis, interlobular septal thickening.
- Time: Acute, subacute, or chronic patterns.
- Other relevant Imaging Modalities:
- MRI: Rarely used but helpful for soft tissue differentiation.
- Nuclear medicine: PET-CT to assess metabolic activity.
- CXR:
-
- Labs:
- Infectious workup (sputum culture, blood culture, PCR).
- Autoimmune panel (e.g., ANA, ANCA).
- Tumor markers if neoplasm is suspected.
-
Pulmonary Function Tests (PFTs):
-
- May show restrictive, obstructive, or mixed patterns depending on etiology.
-
Management:
- Underlying cause treatment:
- Infections: Antimicrobial therapy.
- Inflammatory/Immune: Immunosuppressants or corticosteroids.
- Neoplasm: Chemotherapy, targeted therapy, or surgical intervention.
- Supportive therapy:
- Oxygen supplementation for hypoxemia.
- Pulmonary rehabilitation for chronic cases.
Recommendations:
- Multidisciplinary evaluation for complex cases (pulmonologist, radiologist, oncologist).
- Biopsy for histological confirmation if imaging and clinical findings are inconclusive.
- Serial imaging to monitor progression or response to therapy.
Key Points and Pearls:
-
- Multifocal lung findings are a descriptive term, not a diagnosis.
- Etiology can be infectious, inflammatory, or neoplastic; clinical and imaging correlation is essential.
- PET-CT is valuable in evaluating malignancy-related multifocal findings.
- Consider sampling (e.g., biopsy, bronchoalveolar lavage) in unclear cases for definitive diagnosis.

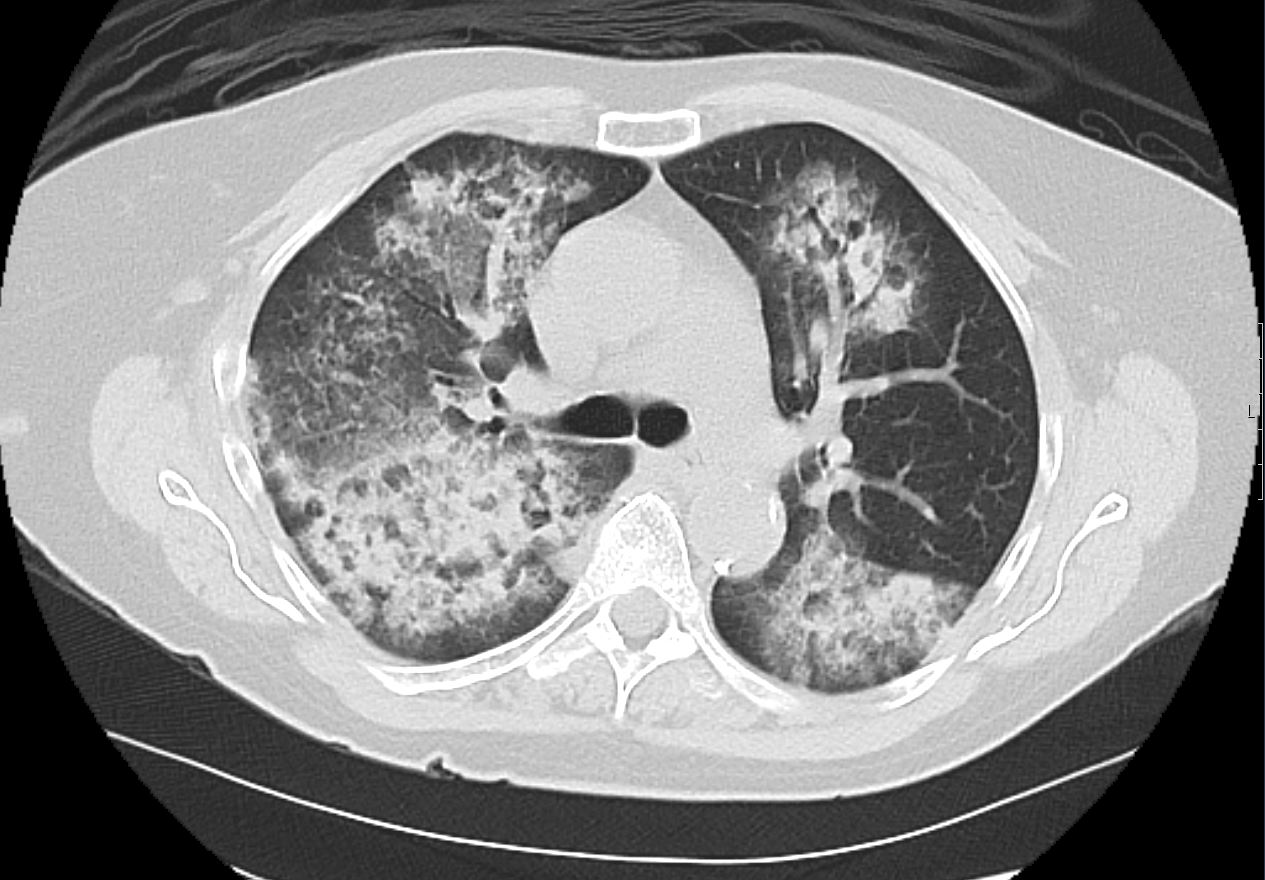
CXR and CT scan shows multifocal pneumonia involving right upper lobe, right lower lobe and to lesser extent the left upper lobe characterised by segmental and subsegmental consolidations and air bronchograms
Ashley Davidoff MD TheCommonVein.net b11521
Key Characteristics
Number:
More than one lesion or abnormality.
Distribution:
Can involve one lung or both lungs.
May be confined to specific regions (e.g., upper lobes, peripheral, or central) or diffusely spread.
Appearance:
Nodules, masses, infiltrates, ground-glass opacities, consolidation, cavitations, or mixed patterns.
Common Causes of Multifocal Lung Findings
Infectious Diseases:
Bacterial Pneumonia: Multifocal consolidations, especially in bronchopneumonia or aspiration.
Fungal Infections: Nodules or cavitations (e.g., aspergillosis, histoplasmosis).
Viral Pneumonia: Multifocal ground-glass opacities (e.g., COVID-19, influenza).
Tuberculosis: Multifocal nodules or cavitating lesions.
Malignancies:
Metastatic Disease: Hematogenous spread from cancers (e.g., breast, renal, thyroid, colorectal).
Primary Lung Cancer: Multifocal tumors in the setting of synchronous primary cancers.
Inflammatory/Autoimmune Conditions:
Sarcoidosis: Perilymphatic nodules, usually bilateral.
Rheumatoid Arthritis-Associated ILD: Multifocal reticulonodular patterns or ground-glass opacities.
Granulomatosis with Polyangiitis (GPA): Multifocal cavitating nodules.
Vascular Causes:
Septic Emboli: Multifocal nodules or cavitations.
Pulmonary Infarcts: Wedge-shaped peripheral opacities.
Pulmonary Hemorrhage Syndromes: Diffuse or multifocal ground-glass opacities.
Vasculitis
35 year old male in acute renal failure and respiratory distress with hemoptysis. CT shows multicentric segmental and subsegmental regions of consolidations and ground glass opacity in the upper and lower lobes with subpleural sparing consistent with pulmonary hemorrhage
Ashley Davidoff MD TheCommonVein.net 137273
Trauma or Iatrogenic:
Fat Embolism Syndrome: Multifocal ground-glass opacities or nodules.
Post-radiation Pneumonitis: Multifocal opacities in radiation fields.
Radiological Features
Imaging Modalities:
Chest X-ray: May show multiple opacities but limited in spatial resolution.
High-Resolution CT (HRCT): The gold standard for characterizing multifocal lung findings, including size, shape, distribution, and associated findings (e.g., cavitation, lymphadenopathy).
Key Patterns to Note:
Nodular: Suggestive of infections (e.g., tuberculosis), metastases, or sarcoidosis.
Ground-glass opacities: Associated with viral pneumonia, autoimmune diseases, or hemorrhage.
Consolidation: Seen in bacterial pneumonia, aspiration, or infarcts.
Cavitation: Possible in infections, GPA, or metastatic disease.
Clinical Correlation
Multifocal findings require integration with clinical data such as:
Symptoms: Fever (infection), hemoptysis (vasculitis, cancer), weight loss (malignancy).
Risk factors: Smoking, occupational exposure, immunosuppression.
Laboratory tests: Cultures, autoimmune panels, or tumor markers.
Differential Diagnosis
The differential depends on the patient’s history, imaging characteristics, and associated systemic findings:
Acute Symptoms:
Infections, pulmonary embolism, trauma.
Chronic Symptoms:
Malignancy, autoimmune diseases, chronic infections (e.g., tuberculosis).
Management
Further Testing:
Biopsy (bronchoscopic or surgical) for unclear causes.
Microbiological tests for infectious causes.
Treatment:
Targeted therapy based on the underlying etiology (e.g., antibiotics for infection, steroids for autoimmune conditions, chemotherapy for cancer).
Multifocal lung findings represent a wide spectrum of conditions, and their management hinges on accurate diagnosis and understanding of the underlying pathology.
