Pleural Fibrofatty Proliferation
Etymology
Derived from “pleura” (membrane surrounding the lungs) and “fibrofatty,” referring to combined proliferation of fibrous tissue and adipose tissue.
AKA
- Pleural fat hyperplasia
- Localized pleural fat proliferation
- Reactive pleural adipose proliferation
What is it?
A localized reparative process involving the proliferation of fatty tissue within the pleura, typically in response to chronic pleural inflammation or infection
History
A 60-year-old male with chronic cough and a history suggestive of chronic aspiration.
Findings
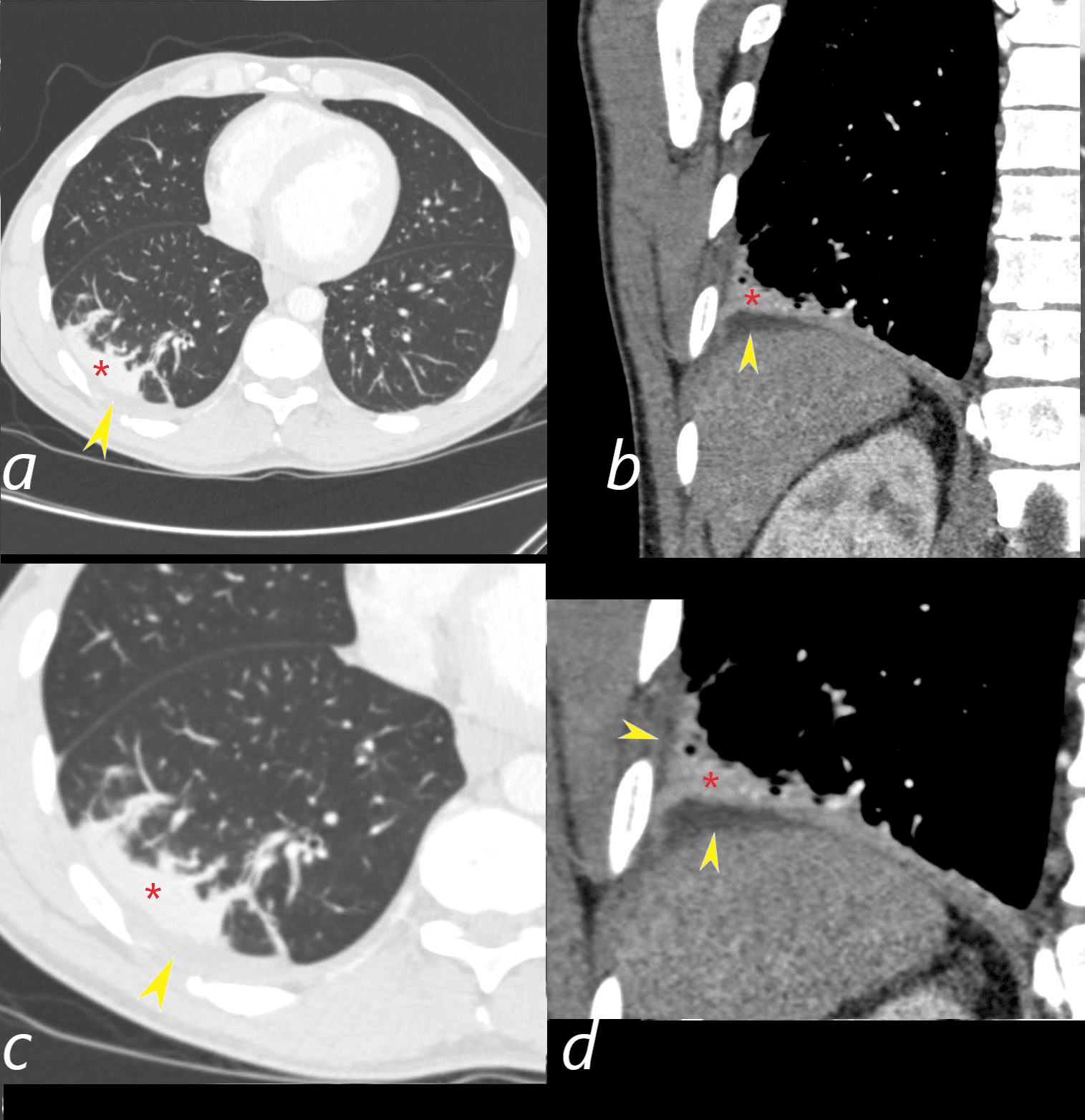
Axial CT (a magnified in c) demonstrates bronchovascular thickening and crescentic atelectasis in the lateral segment of the right lower lobe (RLL) (red asterisk), and fatty proliferation along the pleural surface adjacent to the atelectasis (yellow arrowheads).
Coronal CT (b magnified in d ) reveals a rim of pleural fatty proliferation along the pleural surface adjacent to the atelectasis (red arrowheads) and fatty proliferation along the pleural surface adjacent to the atelectasis (yellow arrowheads).
Ashley Davidoff MD TheCommonVein.net (b12388-03cL)(310Lu)
Comment
The findings in the right lower lobe (RLL) represent chronic crescentic atelectasis, likely due to chronic aspiration, with associated pleural fibrofatty proliferation.
Chronic atelectasis leads to persistent pleural irritation and inflammation, which stimulates localized fibrosis and reactive adipose tissue proliferation in the pleura.
The presence of bronchovascular thickening suggests chronic inflammatory changes, commonly seen in conditions like recurrent aspiration.
Fat proliferation in the pleura (red arrowheads) is a characteristic finding in chronic inflammatory pleural processes and serves as a marker of prolonged pleural injury or irritation.
Radiological Pearls
Fatty proliferation is seen as low-attenuation areas (-50 to -150 HU) adjacent to areas of pleural thickening.
Crescentic atelectasis is a hallmark of chronic subsegmental airway obstruction and recurrent collapse, as seen in this case.
Caused by
Chronic pleural inflammation, such as:
- Tuberculous pleuritis
- Chronic empyema
- Chronic pleural effusions
- Post-inflammatory pleuritis
- Post-surgical or post-traumatic pleural changes
Resulting in
The development of localized fat proliferation within thickened pleural layers.
Structural Changes
Fibrosis combined with fat deposition in pleural tissues.
Parts
Found within the visceral pleura, parietal pleura, or both.
Size
Typically small and localized, depending on the extent of the underlying inflammatory process.
Shape
Irregular or nodular fatty deposits along the pleura.
Position
Localized to areas of prior or ongoing inflammation, often near regions of pleural thickening or calcifications.
Character
Radiologically appears as low-attenuation fat-density areas within the pleura on CT.
Time
Develops over a chronic course, often secondary to prolonged inflammation.
Pathophysiology
Chronic pleural irritation activates fibroblasts and mesenchymal cells, leading to localized fibrosis and adipose proliferation within the pleural layers. May represent a reparative mechanism to stabilize the inflamed or damaged pleura.
Pathology
Histologically shows adipose tissue proliferation interspersed with fibrous tissue, often accompanied by signs of chronic inflammation (e.g., lymphocytic infiltration).
Diagnosis
Primarily diagnosed on imaging (CT), often as an incidental finding.
Clinical
Usually asymptomatic. May serve as a marker of prior pleural inflammation or infection.
Radiology and Imaging
CXR Findings
Nonspecific pleural thickening. Cannot reliably distinguish fat proliferation on plain radiographs.
CT Findings
Localized fat-density regions within the pleura (attenuation values between -50 and -150 HU). Associated pleural thickening or calcifications. Often adjacent to lung parenchymal abnormalities, such as fibrotic bands or prior pleural effusion cavities.
Associated Findings on CT
Pleural calcifications in chronic empyema or tuberculosis. Fibrotic changes in the adjacent lung parenchyma.
Other Relevant Imaging Modalities
MRI
Fat proliferation may appear hyperintense on T1-weighted sequences, with suppression on fat-saturated imaging. Limited utility due to the predominance of CT for pleural evaluation.
Ultrasound (US)
May show hyperechoic areas representing fatty tissue, though differentiation from fibrosis is challenging.
Nuclear Medicine (NM)
Not typically used for this condition.
Angiography
No role.
Labs
Generally nonspecific, reflecting the underlying inflammatory process (e.g., elevated ESR or CRP).
Management
No specific treatment is required for pleural fibrofatty proliferation itself. Focus on managing the underlying condition (e.g., tuberculosis, chronic empyema).
Recommendations
Radiological follow-up is typically unnecessary unless clinically indicated.
Key Points and Pearls
Pleural fibrofatty proliferation is a localized reaction to chronic inflammation, characterized by fat deposition within thickened pleura. It is best visualized on CT, appearing as low-attenuation fat-density regions. Often associated with conditions like tuberculous pleuritis, chronic empyema, or chronic pleural effusion. Subpleural fat proliferation helps localize prior areas of pleural injury and chronic inflammation.
