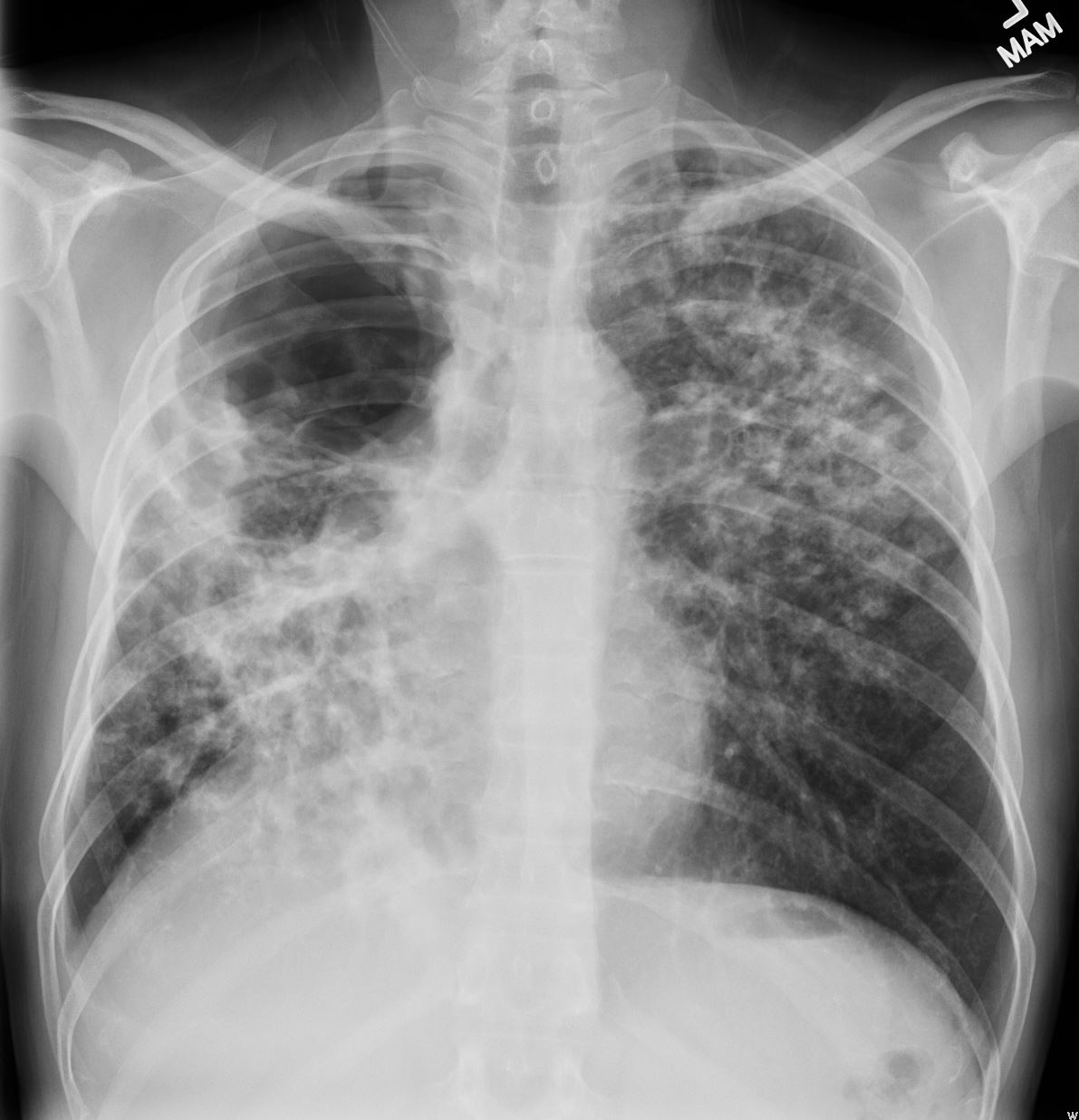
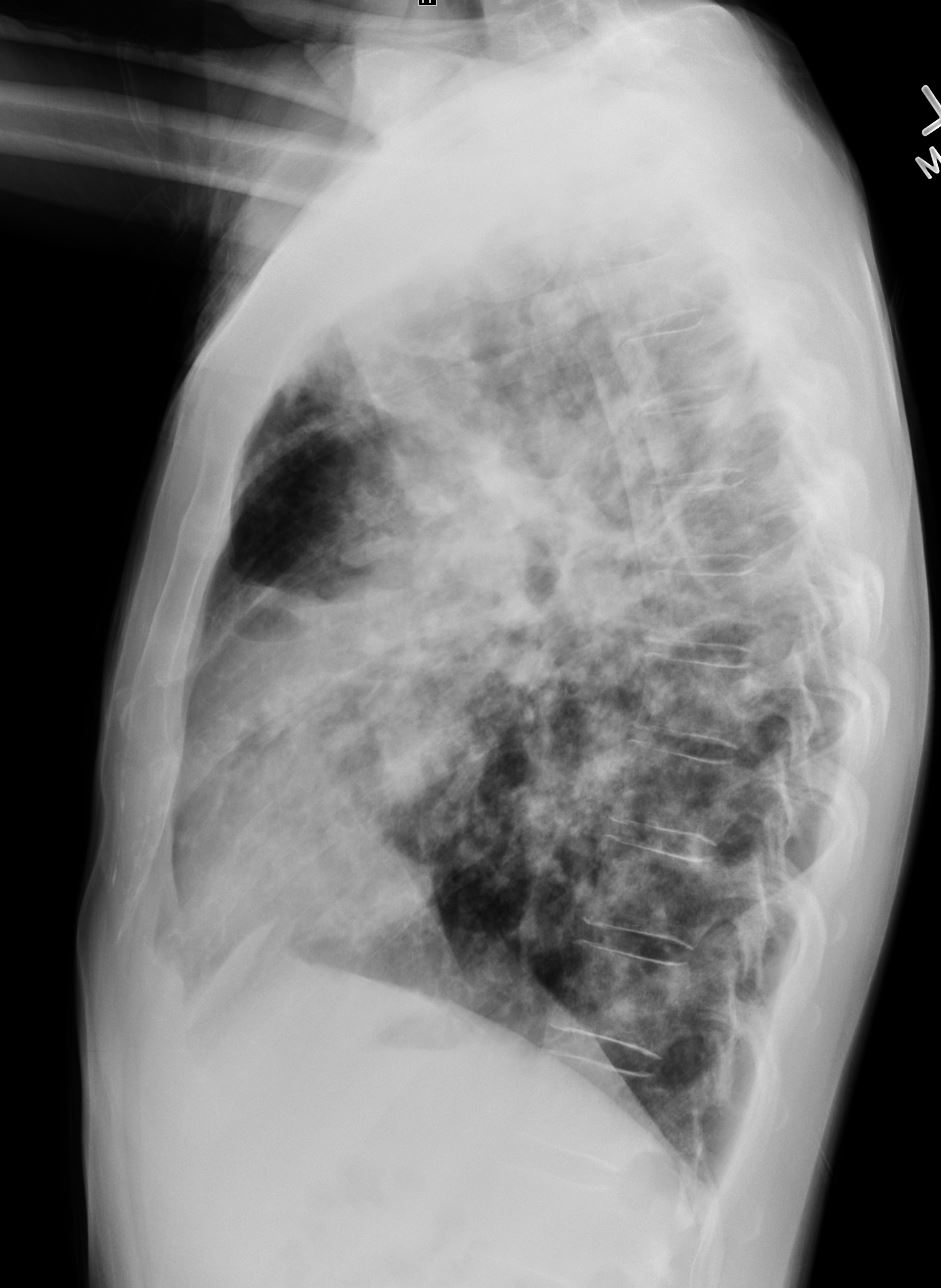
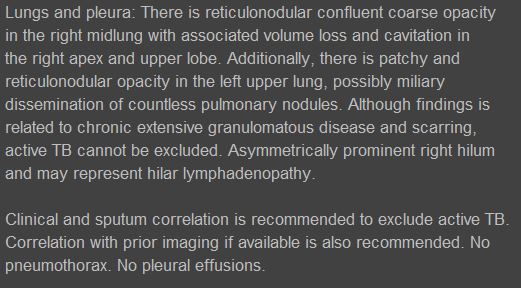
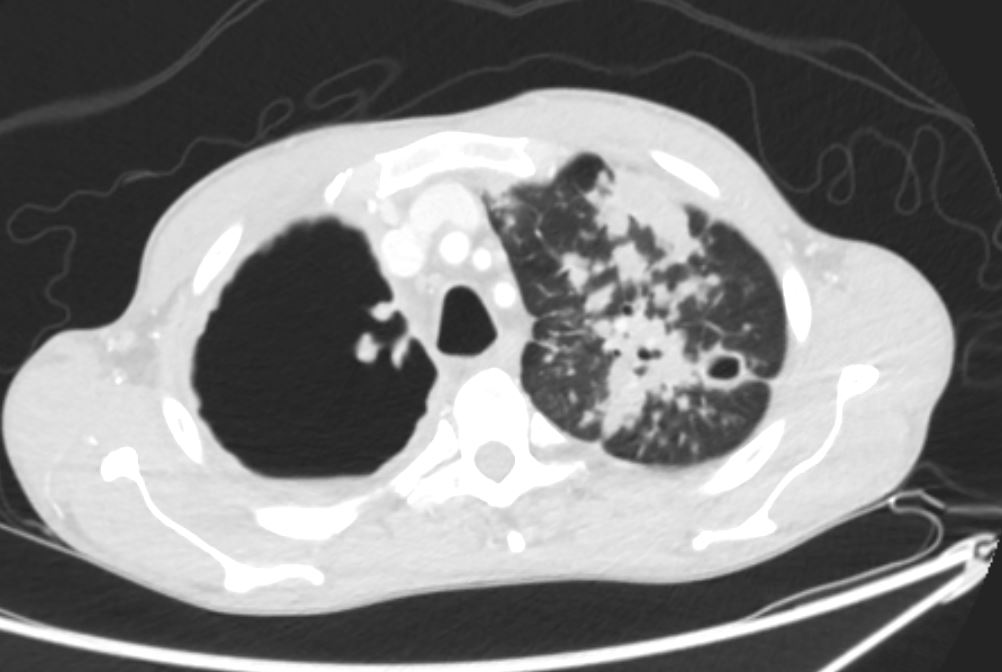
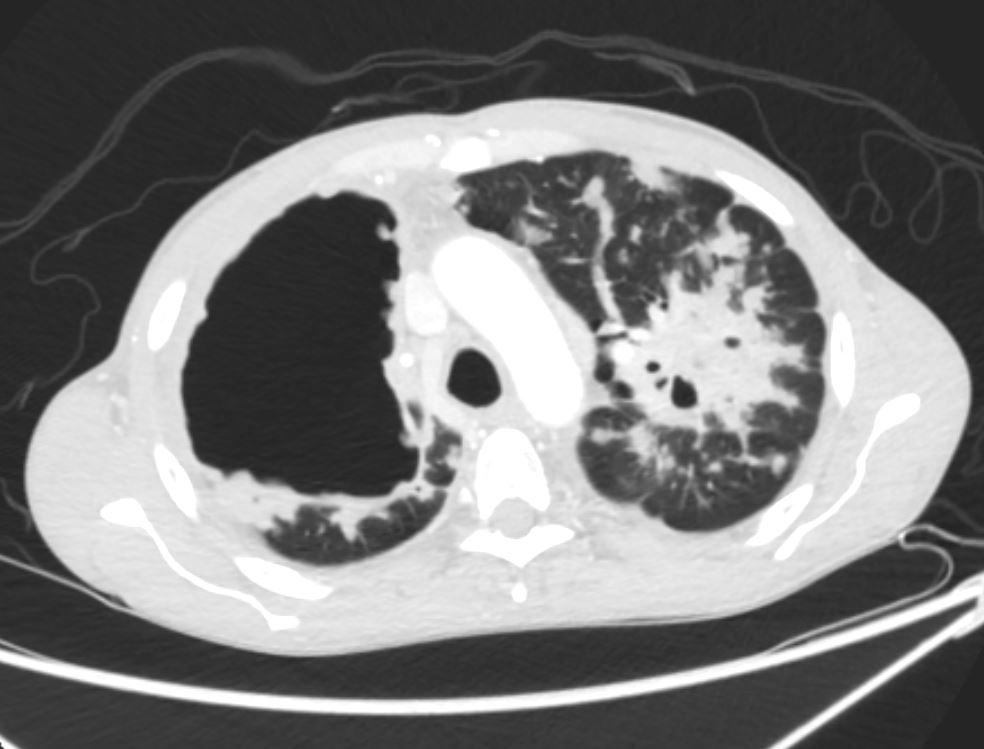
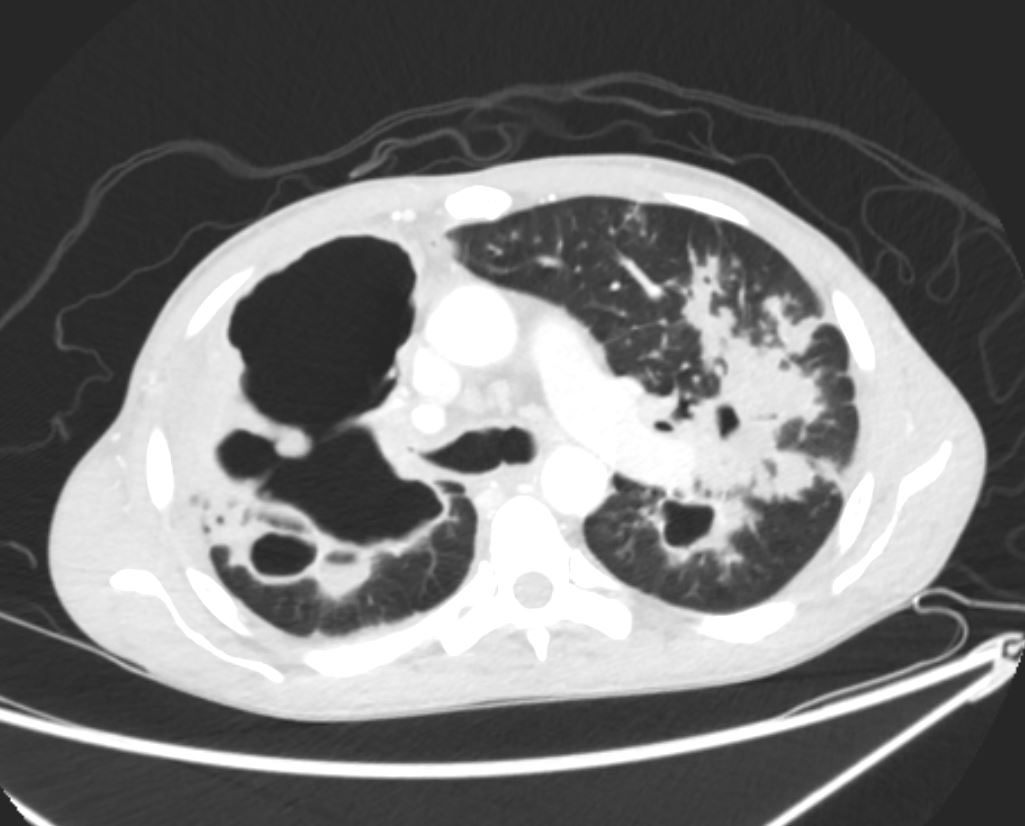
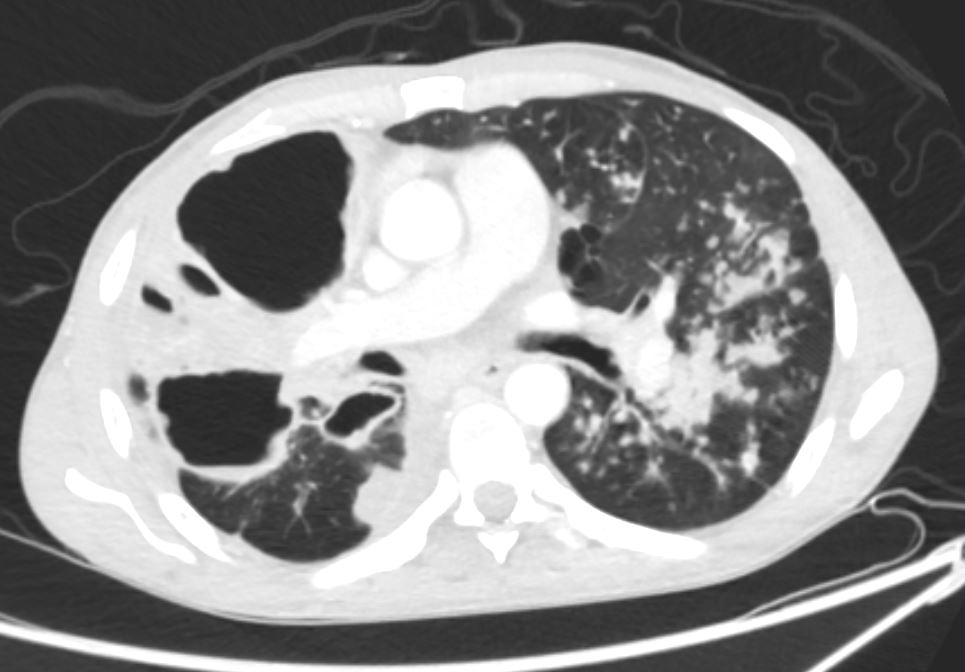
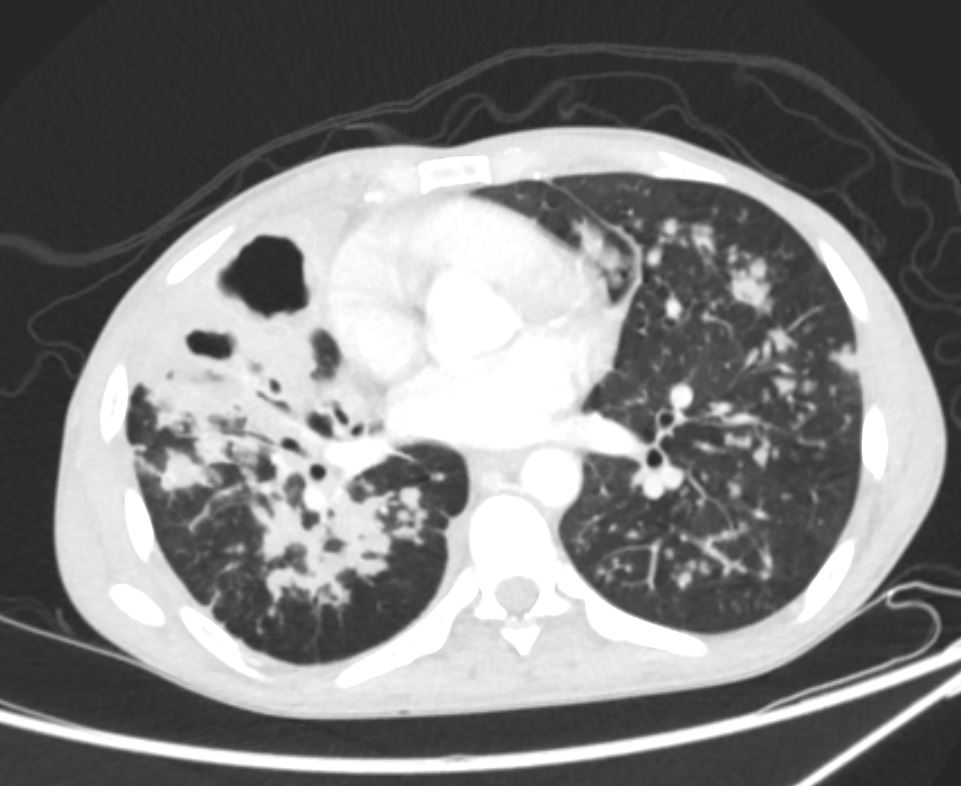
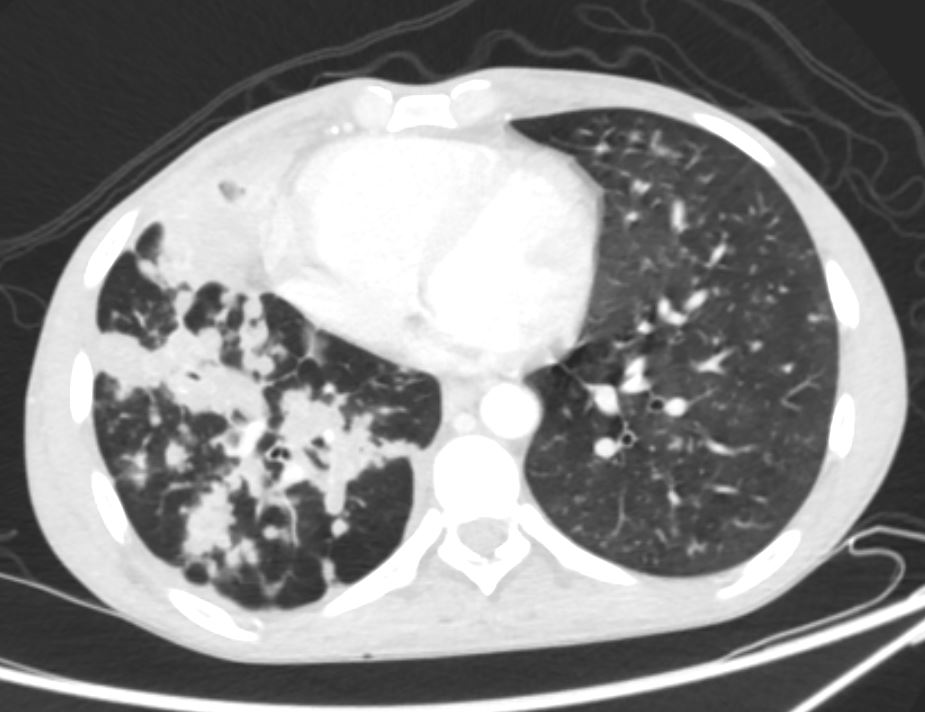
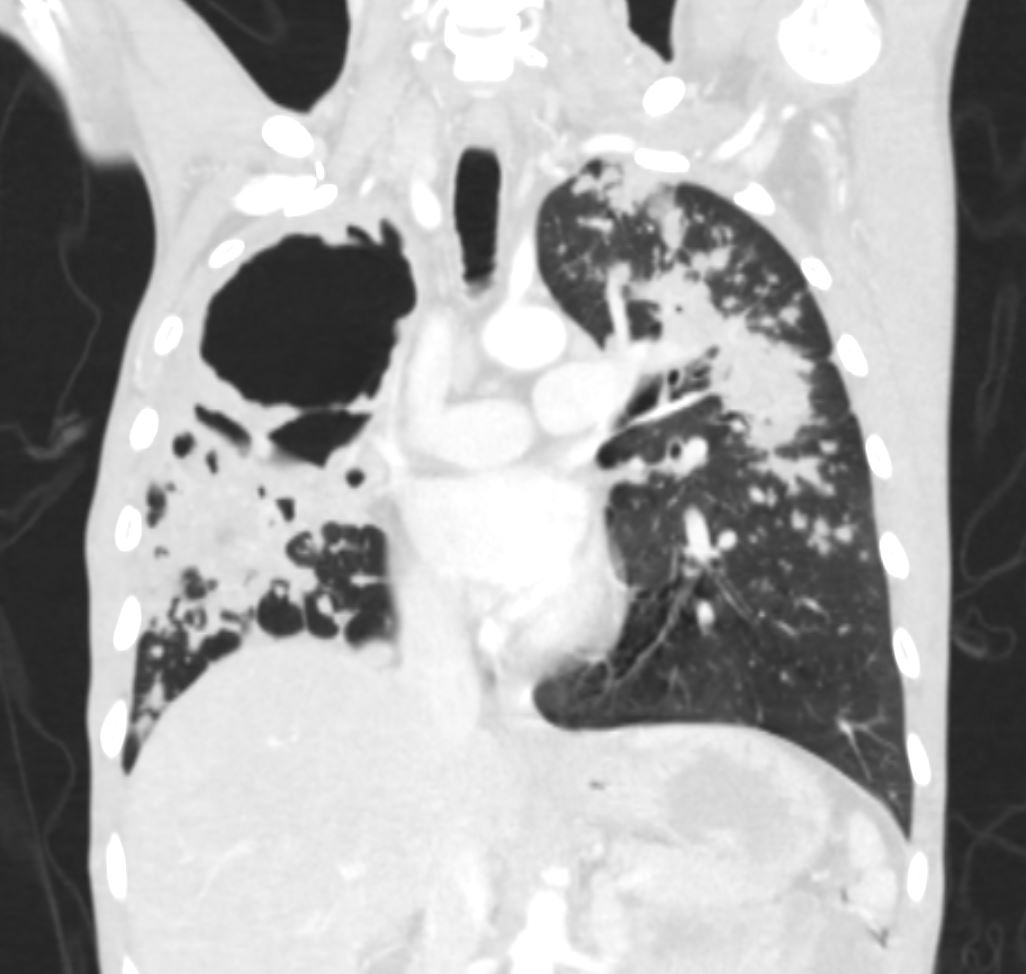
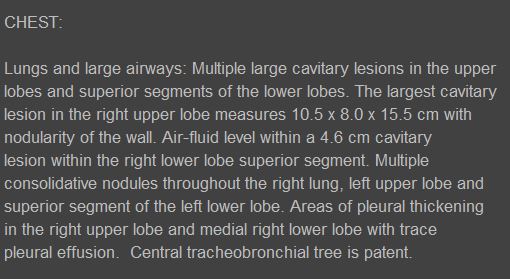
Cavitary lung lesions, c/f relapsed TB
vs superinfection
58 y.o. male with a past medical history
significant for active TB (diagnosed 2 years ago) s/p multiple
drug therapy and treatment of ~12 months as below, PE (not on AC)
 who presented to the hospital for scheduled bronchoscopy on
who presented to the hospital for scheduled bronchoscopy on
for evaluation of progressive cavitary/necrotic
pulmonary lesions with post-bronch course c/b acute hypoxemia
respiratory failure, currently intubated in the MICU with a
pressor requirement. BAL AFB smears x2 with 1+ AFB, MTB PCR
positive (rpoB gene neg), and BAL culture + Enterobacter Cloacae
complex. ID consulted for help with antibiotics.
Patient’s TB history with treatment:
1 year ago – 5/20/2019 INH, RIF, PZA, ETB (unclear compliance)
7 months ago – 6/1/2019 INH, RIF, PZA, linezolid, amikacin
2months ago INH, PZA, Rifampin (r/o resistance)
He was then hospitalized 15 months agoand at that time he underwent a bronchoscopy and AFB smear 2/2 with 3+ AFB but no growth on culture. Samples were also
sent to the CDC for sequencing and no resistance pattern found.
At that time, he continued 3 drug regimen for 6 months. During
this admission, he also underwent CTPA and was found to have a
RUL PE for which evaluated by PERT but not started on AC given
chronicity.
More recently, the patient reports ongoing dyspnea since May and
DOE. He reports dyspnea with minimal exertion. He also reports a
cough productive of green phlegm mostly in the AM. He denies any
F/C/night sweats, no hemoptysis. He has lost ~5lbs in last month.
Of note, patient smoked 1/2ppd x 35 yrs and quit in 2019. He was
born in Vietnam and move to US 30 years ago. He worked in construction
x20 yrs.
He was seen in Pulmonary Clinic on 2 weeks ago – reviewed CT chest
that demonstrated new RLL cavitary lesions and worsening
necrosis of the RLL and RML as well as extension of the RUL PE.
Part of Pulmonary work up included negative ANCA, neg
immunoglobulins, and aspergillus galactomannan which was neg.
Here the patient initially presented for bronchoscopy on 1/29
with BAL to LUL, with scattered mucopurulent secretions
throughout L bronchial tree. After the bronchoscopy while in the
PACU, the patient had tachycardia, tachypnea and worsening