2 Years Prior to Current Admission
55-year-old male with
substance use disorder presents with dyspnea.
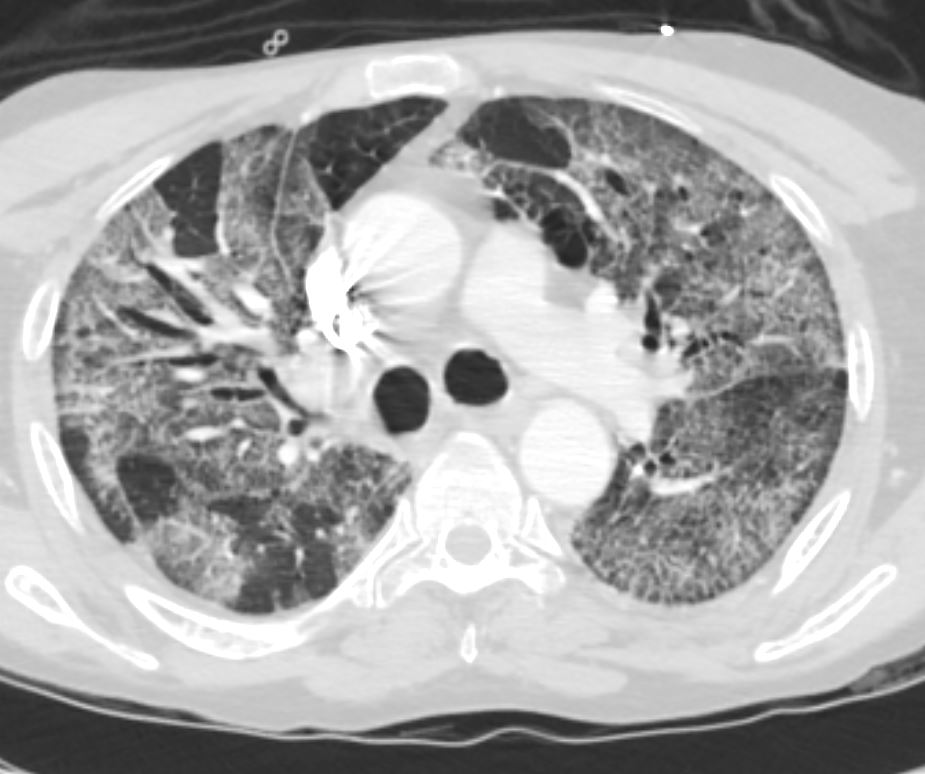
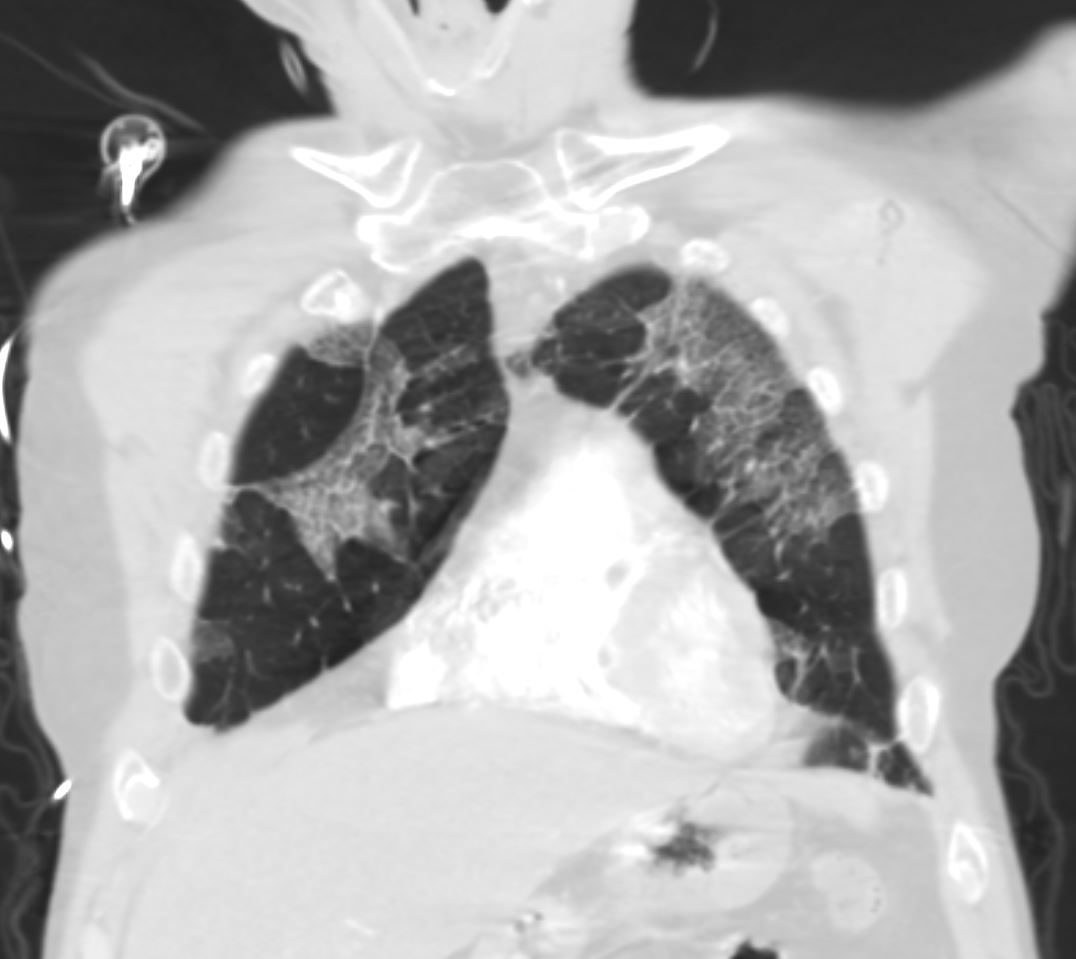
Mild Upper Lobe ground Glass Changes
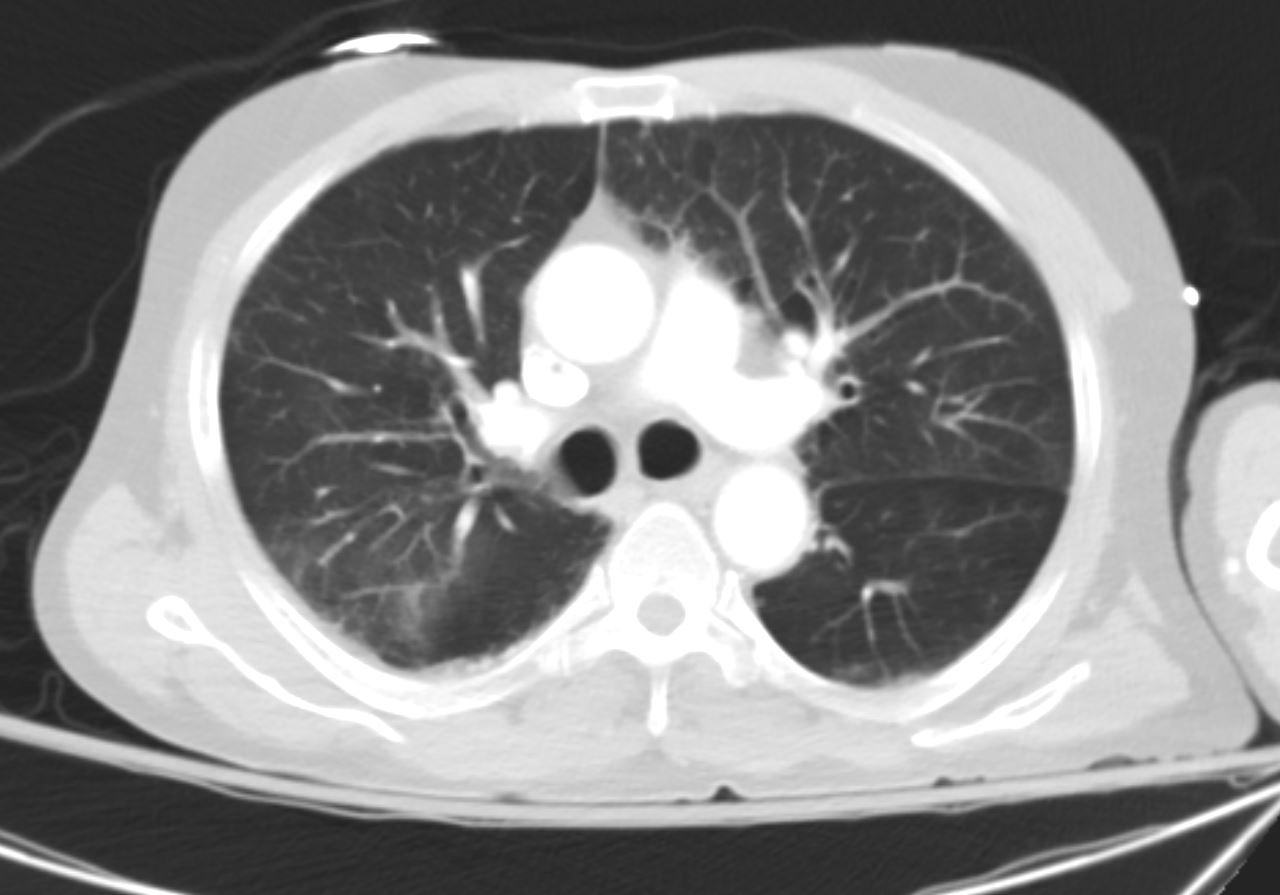
55 year old male with substance use disorder presented 2years prior with dyspnea. CT in the axial plane shows minor ground glass changes in the upper lobes. Inhalational alveolitis was suspected
Ashley Davidoff MD TheCommonVein.net 251Lu 135914

55 year old male with substance use disorder presented 2years prior with dyspnea. CT in the axial plane shows minor ground glass changes in the upper lobes. Inhalational alveolitis was suspected
Ashley Davidoff MD TheCommonVein.net 251Lu 135915
CT 18 months Later
- 55 y.o. male w
- PMH of AUD c/b chronic pancreatitis, HTN, obstructive lung disease (COPD, asthma) tobacco use disorder,
- Presents with
- 1 day of abdominal pain and nausea
- found to have presumed alcohol induced pancreatitis. During hospitalization, patient noted to have elevated CK,
- Lipase 345, acute on chronic pancreatitis,
- Elevated transaminases in pattern of hepatocellular injury, AST 870, ALT 541. Normal bilirubin
- worsening SOB and new hypoxemia.
- worsening GGOs on imaging.
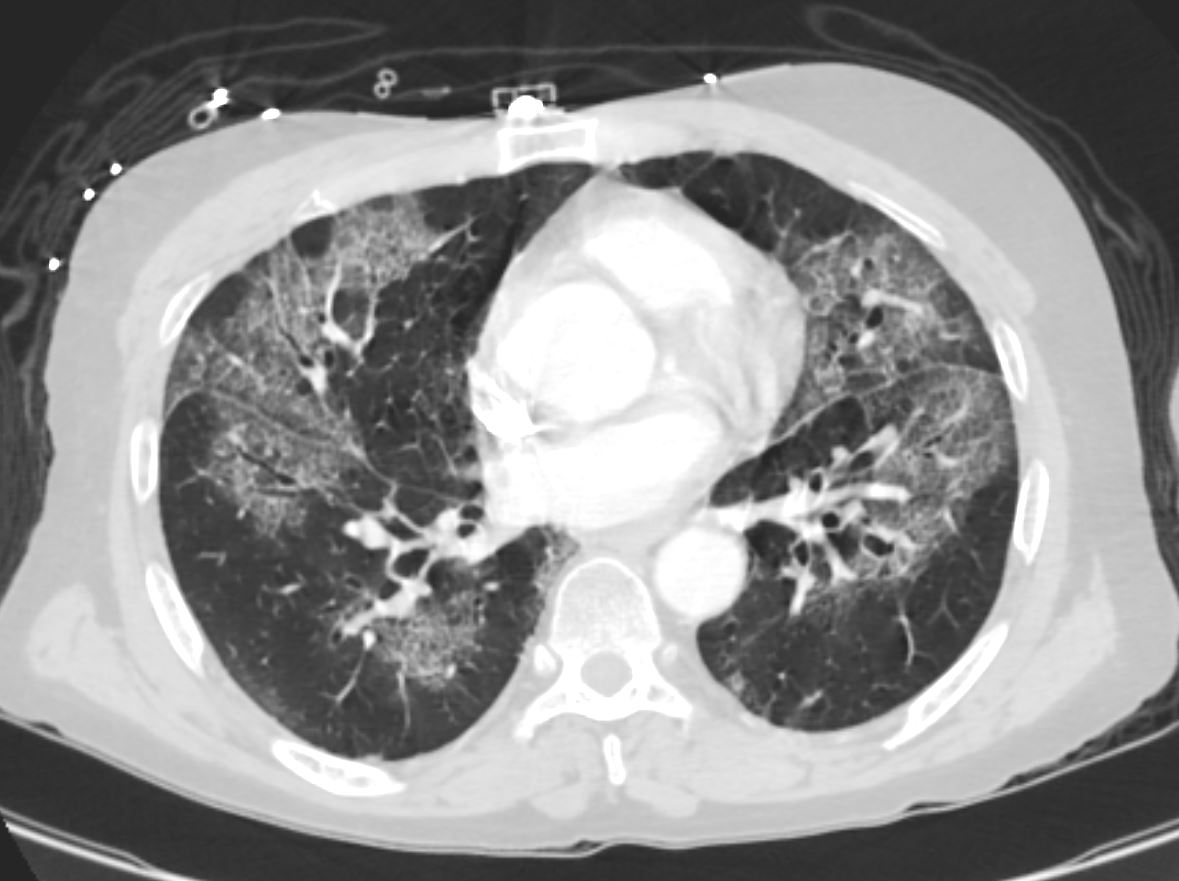
CT – more prominent
Central, perihilar upper lobe ground glass changes.
Inhalational pneumonitis

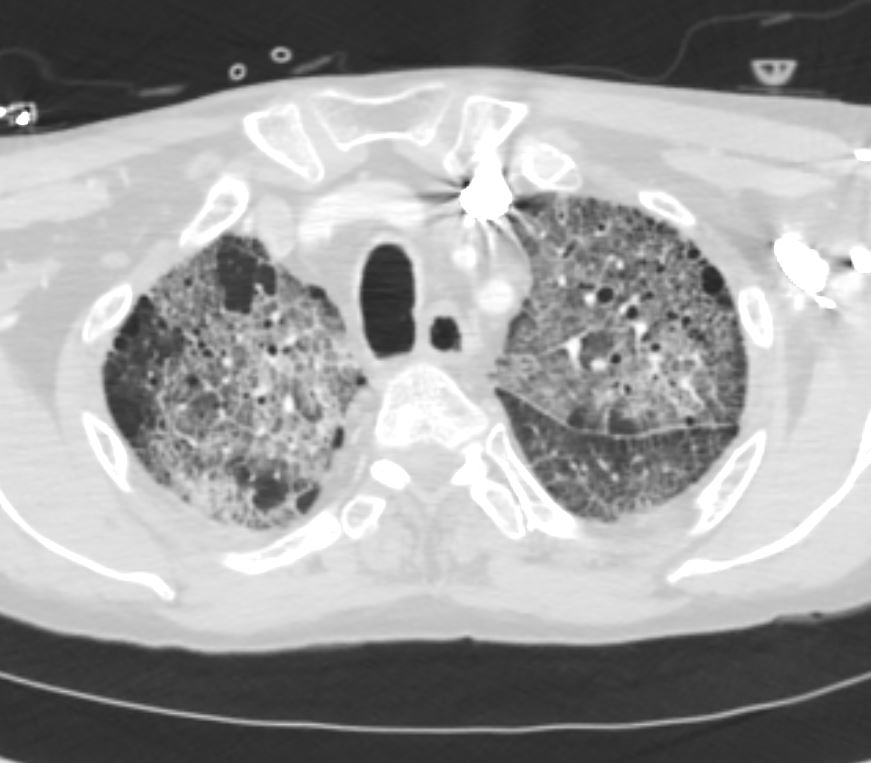
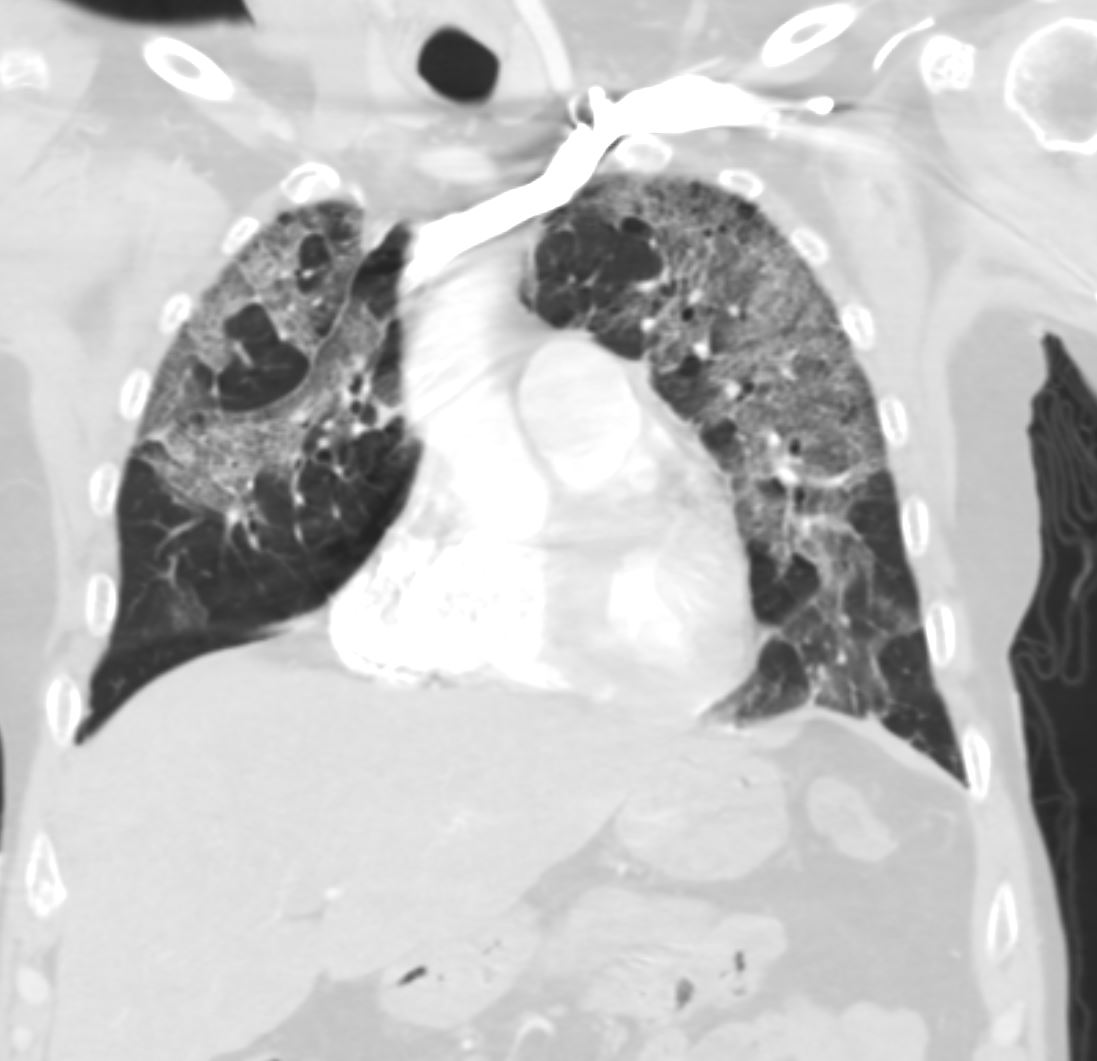
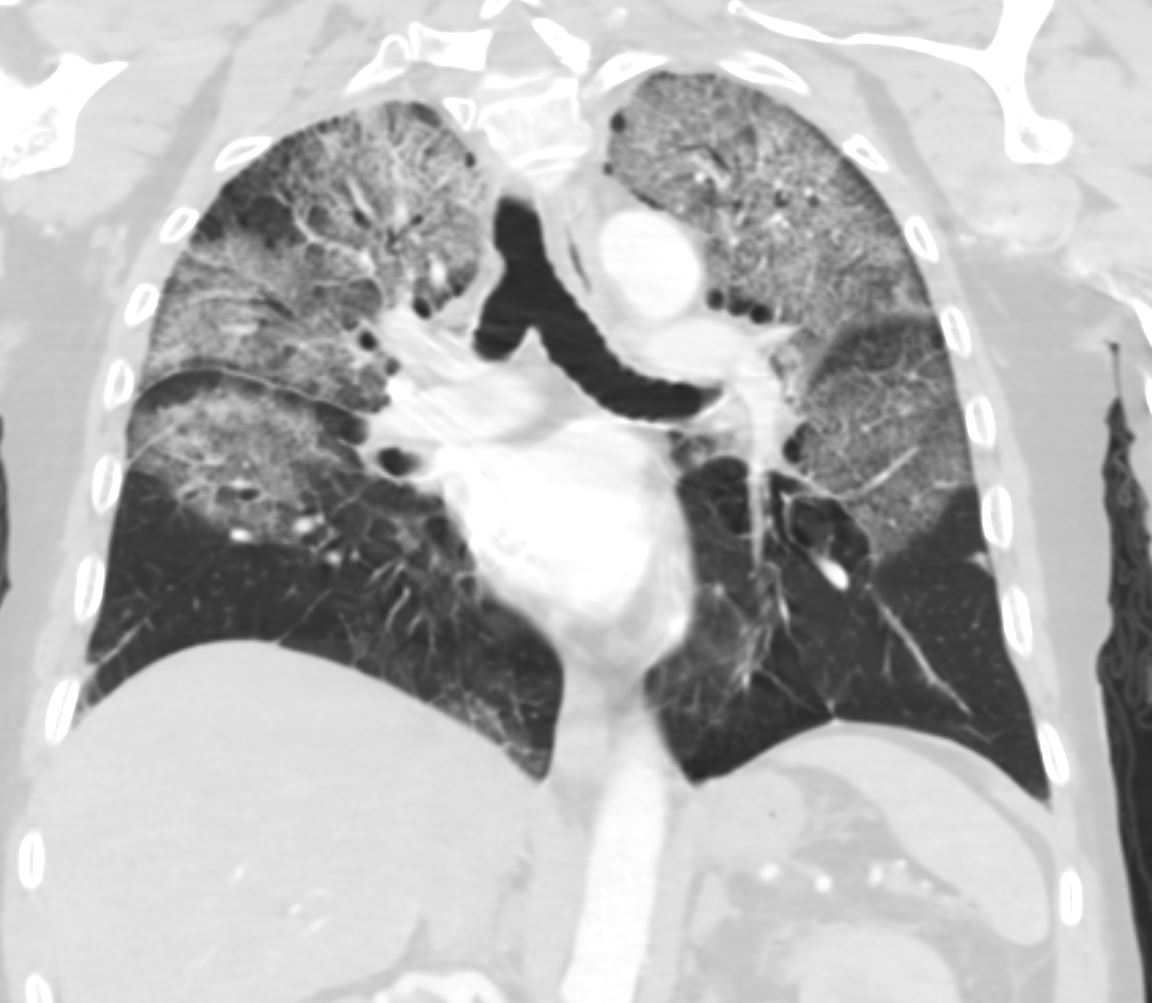
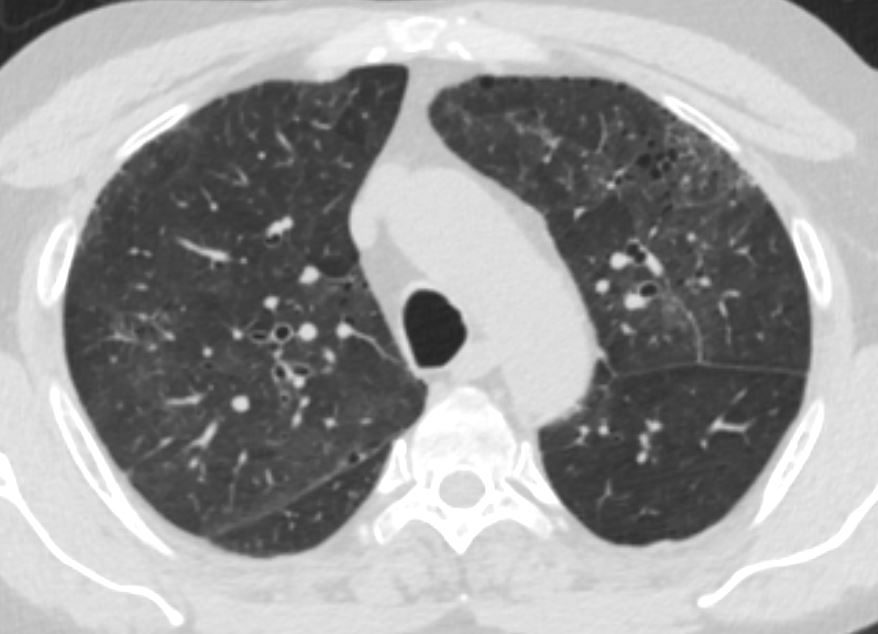
55-year-old male with substance use disorder presents with progressive dyspnea. Axial CT shows more prominent central, and upper lobe ground glass changes. Inhalational pneumonitis was suspected from cigarette smoking or from inhaled cocaine . Included in the differential diagnosis was DIP and hypersensitivity pneumonitis
Ashley Davidoff MD TheCommonVein.net 251Lu 135917
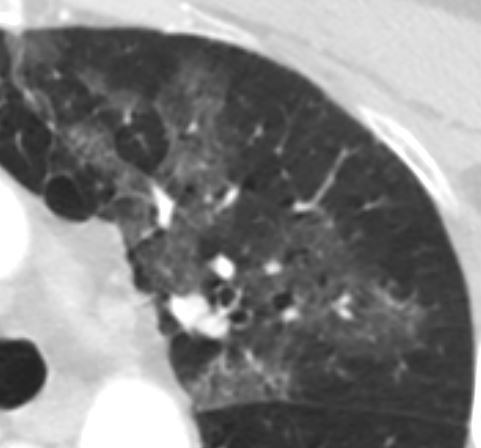
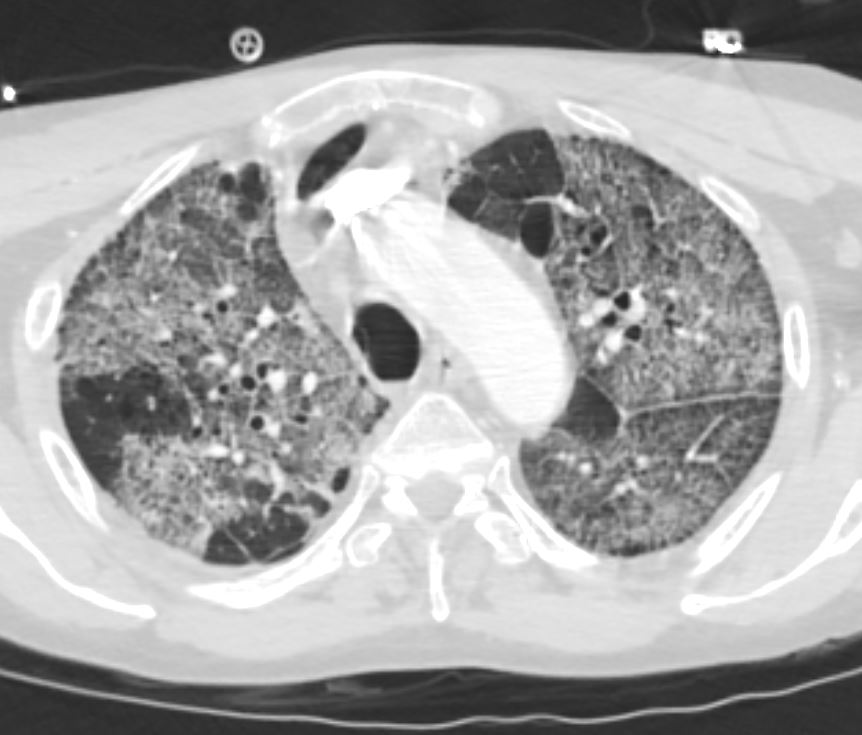
55-year-old male with substance use disorder presents with progressive dyspnea. Magnified view of an axial CT shows panlobular central ground glass changes, with the left upper lobe more prominent than right Inhalational pneumonitis was suspected, from cigarette smoking or cocaine. Included in the differential diagnosis was DIP and hypersensitivity pneumonitis
Ashley Davidoff MD TheCommonVein.net 251Lu 135918
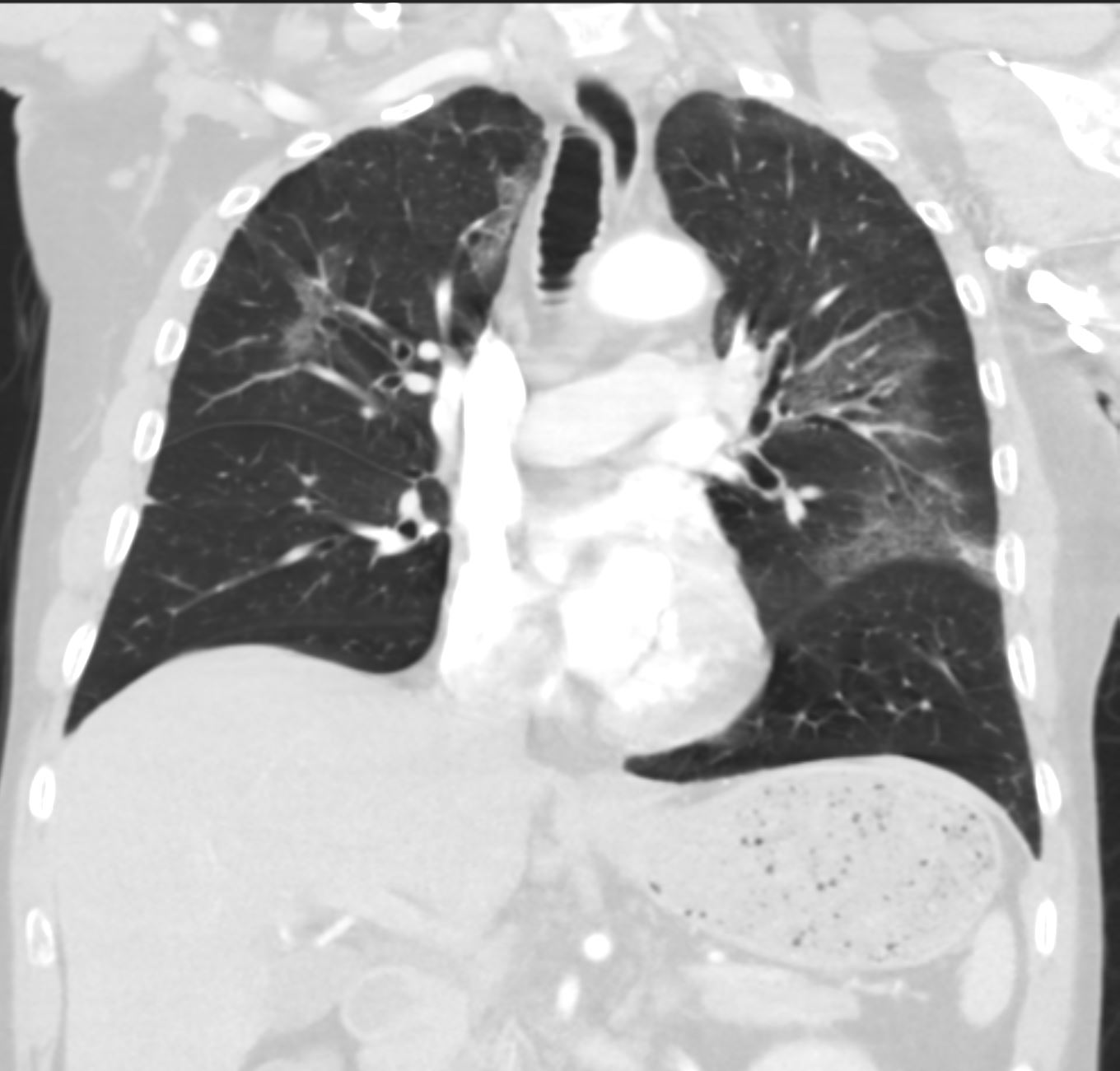
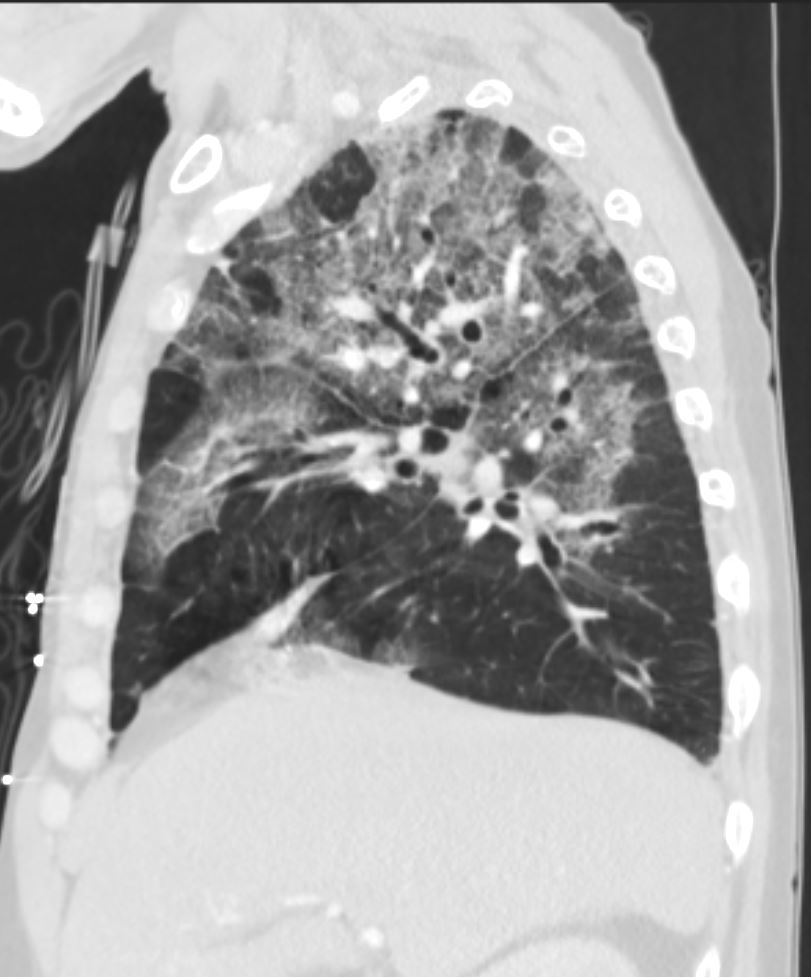
55-year-old male with substance use disorder presents with progressive dyspnea. Coronal CT shows panlobular central ground glass changes, with the left upper lobe more prominent than right. Inhalational pneumonitis was suspected, from cigarette smoking or cocaine. Included in the differential diagnosis was DIP and hypersensitivity pneumonitis
Ashley Davidoff MD TheCommonVein.net 251Lu 135919
1month Later Prominent Upper Lobe
Ground Glass Parenchymal Changes
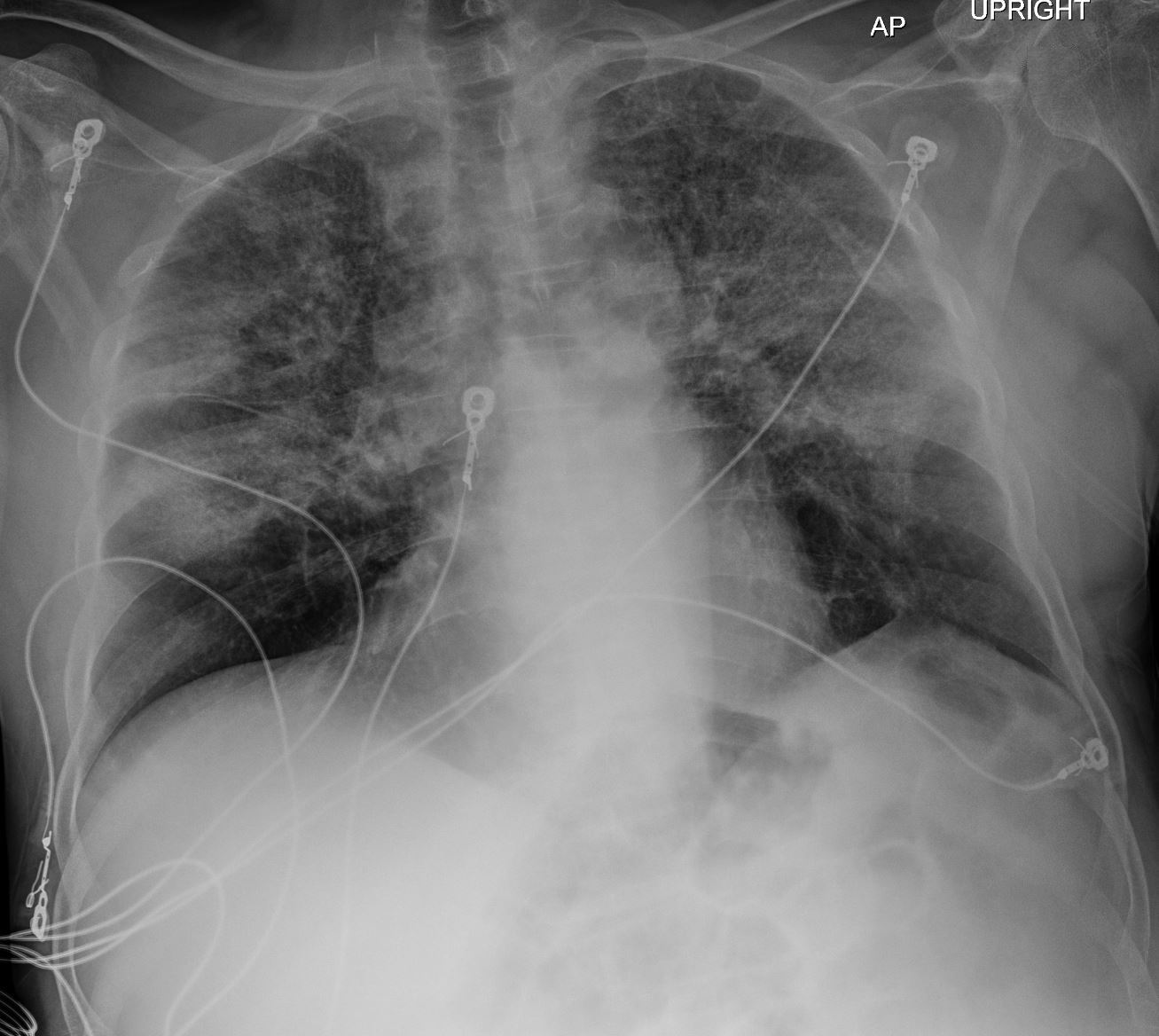
55 year old male with substance use disorder presents with progressive and now more severe dyspnea. Frontal CXR shows extensive upper lobe ground glass changes in the upper lobes. Inhalational pneumonitis was suspected with multifocal regions of consolidation.
Progressive inhalational pneumonitis from smoking or cocaine inhalation was suspected
Ashley Davidoff MD TheCommonVein.net 251Lu 135918
Prominent Upper Lobe Ground Glass Parenchymal Changes with Subpleural Sparing
55 year old male with substance use disorder presents with progressive and now more severe dyspnea. CT through the upper lung fields shows extensive upper lobe ground glass changes with thickening of the interlobular septa giving the appearance of “crazy paving”.
Progressive inhalational pneumonitis from smoking or cocaine inhalation was suspected. DIP and hypersensitivity pneumonitis remained in the differential diagnosis
Ashley Davidoff MD TheCommonVein.net 251Lu 135921
55 year old male with substance use disorder presents with progressive and now more severe dyspnea. CT through the upper lung fields shows extensive upper lobe ground glass changes with thickening of the interlobular septa giving the appearance of “crazy paving”. Thickening and irregularity of the left major fissure is also noted
Progressive inhalational pneumonitis from smoking or cocaine inhalation was suspected. DIP and hypersensitivity pneumonitis remained in the differential diagnosis
Ashley Davidoff MD TheCommonVein.net 251Lu 135922
CT 1month Later Prominent Upper Lob
Ground Glass Parenchymal Changes Crazy Paving and Subpleural Sparing
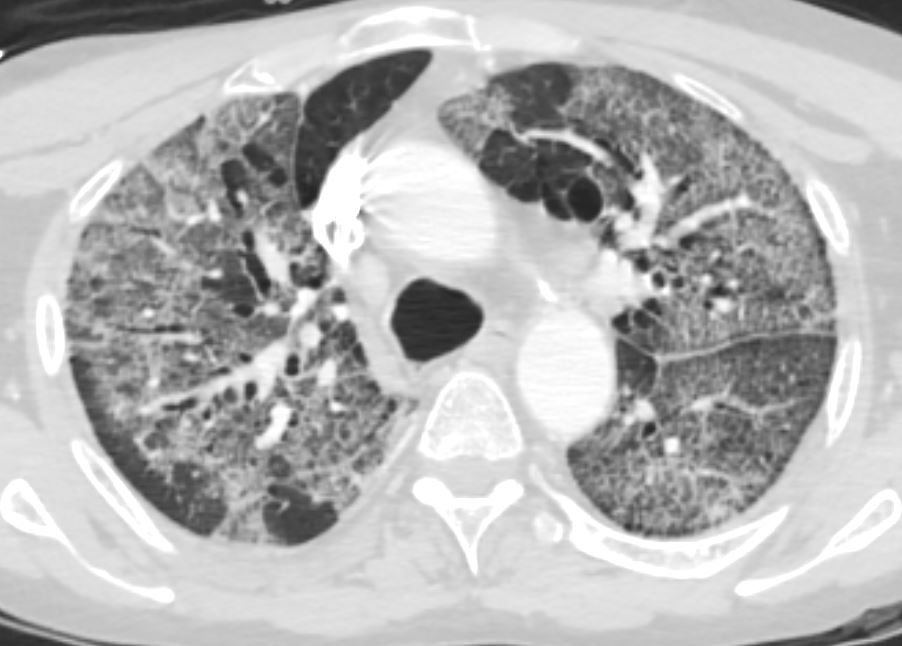
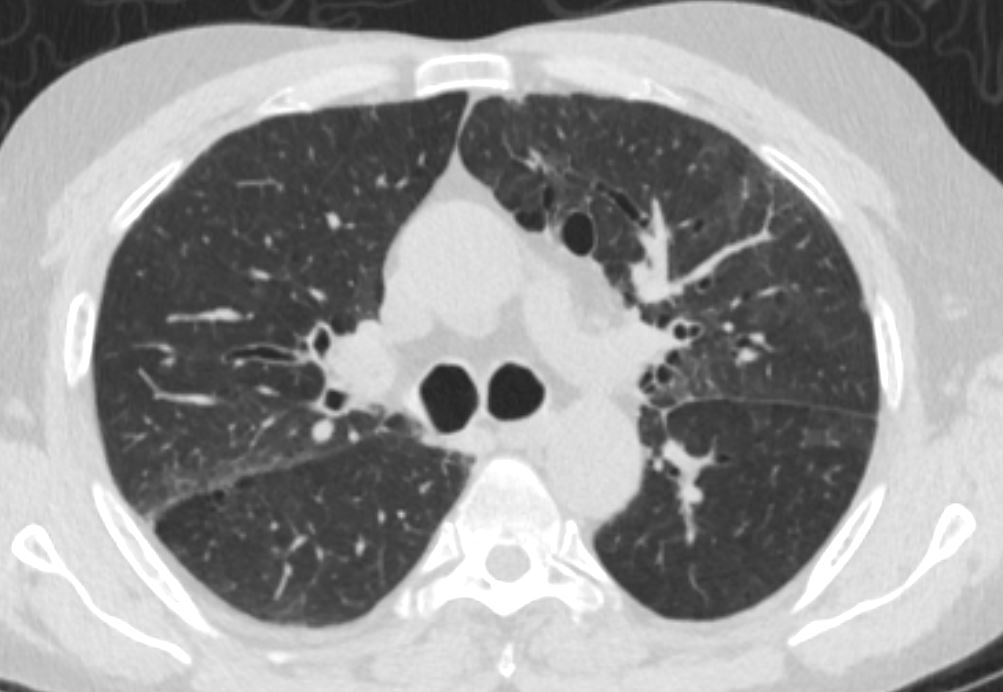
55 year old male with substance use disorder presents with progressive and now more severe dyspnea. CT through the upper lung fields shows extensive upper lobe ground glass changes with thickening of the interlobular septa giving the appearance of “crazy paving”. Thickening and irregularity of the left major fissure is also noted There is bilateral peripheral sparing.
Progressive inhalational pneumonitis from smoking or cocaine inhalation was suspected. DIP and hypersensitivity pneumonitis remained in the differential diagnosis
Ashley Davidoff MD TheCommonVein.net 251Lu 135923
55 year old male with substance use disorder presents with progressive and now more severe dyspnea. CT through the upper lung fields shows extensive upper lobe ground glass changes with thickening of the interlobular septa giving the appearance of “crazy paving”. Thickening and irregularity of the left major fissure is also noted There is bilateral peripheral sparing.
Progressive inhalational pneumonitis from smoking or cocaine inhalation was suspected. DIP and hypersensitivity pneumonitis remained in the differential diagnosis
Ashley Davidoff MD TheCommonVein.net 251Lu 135924
55 year old male with substance use disorder presents with progressive and now more severe dyspnea. CT through the upper lung fields shows extensive upper lobe ground glass changes with thickening of the interlobular septa giving the appearance of “crazy paving”. Thickening and irregularity of the left major fissure is also noted. There is bilateral peripheral sparing and mosaicism.
Progressive inhalational pneumonitis from smoking or cocaine inhalation was suspected. DIP and hypersensitivity pneumonitis remained in the differential diagnosis
Ashley Davidoff MD TheCommonVein.net 251Lu 135925
Prominent Upper Lobe and
Superior Segments of the Lower Lobes
Central Ground Glass Changes

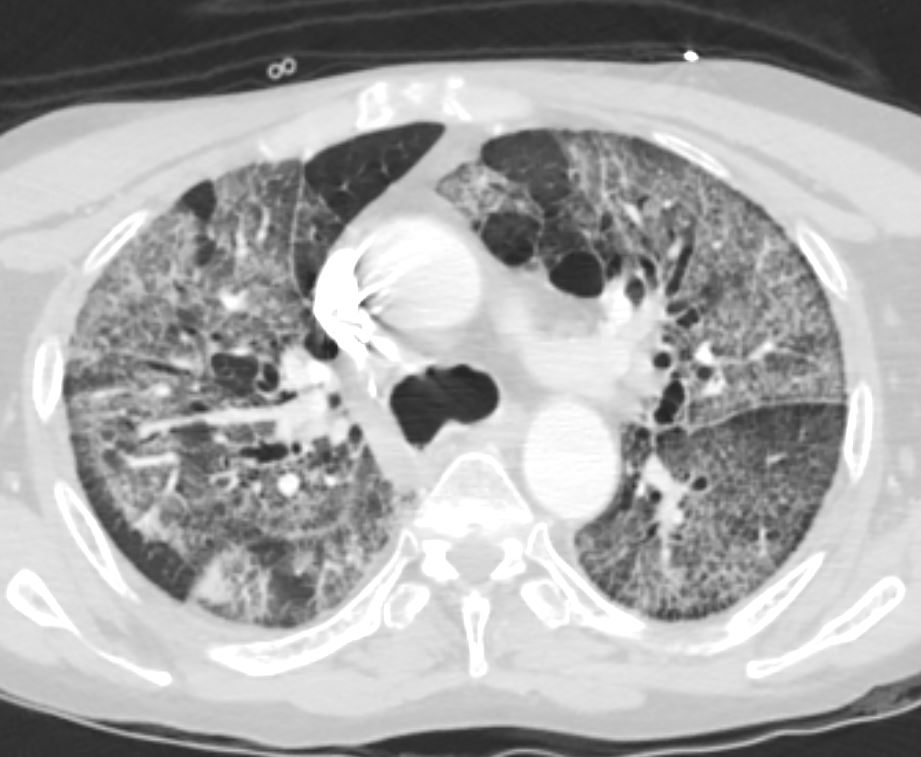
55 year old male with substance use disorder presents with progressive and now more severe dyspnea. CT through the mid lung fields shows extensive upper lobe and superior segmental lower lobe ground glass changes with thickening of the interlobular septa giving the appearance of “crazy paving”. Thickening and irregularity of the major and middle fissures are also noted. There is bilateral peripheral sparing with a batwing distribution
Progressive inhalational pneumonitis from smoking or cocaine inhalation was suspected. DIP and hypersensitivity pneumonitis remained in the differential diagnosis
Ashley Davidoff MD TheCommonVein.net 251Lu 135926

55 year old male with substance use disorder presents with progressive and now more severe dyspnea. CT through the mid lung fields shows extensive upper lobe and superior segmental lower lobe ground glass changes with thickening of the interlobular septa giving the appearance of “crazy paving”. Thickening and irregularity of the major and middle fissures are also noted. There is bilateral peripheral sparing with a batwing distribution
Progressive inhalational pneumonitis from smoking or cocaine inhalation was suspected. DIP and hypersensitivity pneumonitis remained in the differential diagnosis
Ashley Davidoff MD TheCommonVein.net 251Lu 135927
55 year old male with substance use disorder presents with progressive and now more severe dyspnea. CT through the mid lung fields shows extensive upper lobe and superior segmental lower lobe ground glass changes with thickening of the interlobular septa giving the appearance of “crazy paving”. Thickening and irregularity of the major and middle fissures are also noted. There is bilateral peripheral sparing with a batwing distribution
Progressive inhalational pneumonitis from smoking or cocaine inhalation was suspected. DIP and hypersensitivity pneumonitis remained in the differential diagnosis
Ashley Davidoff MD TheCommonVein.net 251Lu 135928
Close to Normal Lung Bases

55 year old male with substance use disorder presents with progressive and now more severe dyspnea. CT through the lower lung fields shows sparing of disease except for minor changes in the subsegmental airways which are mildly thickened.
Progressive inhalational pneumonitis from smoking or cocaine inhalation was suspected. DIP and hypersensitivity pneumonitis remained in the differential diagnosis
Ashley Davidoff MD TheCommonVein.net 251Lu 135929
Normal Sized Heart
No CHF
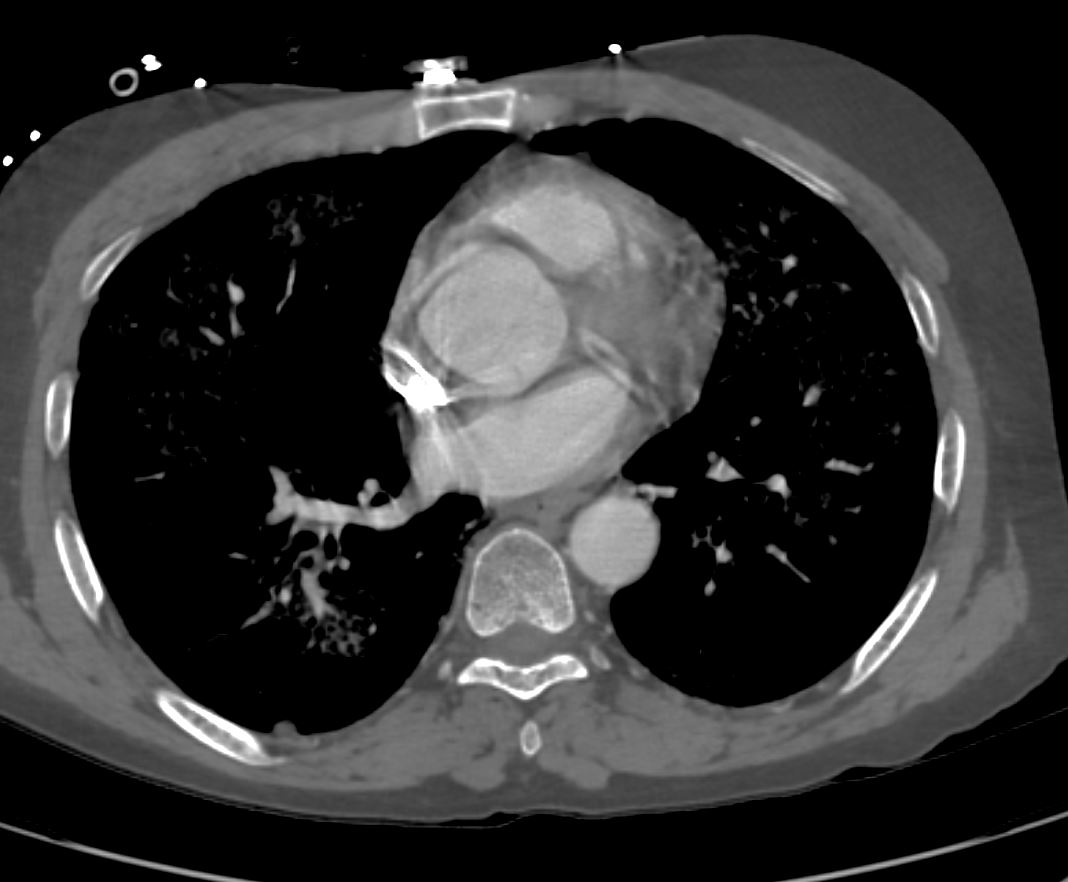
55-year-old male with substance use disorder presents with progressive and now more severe dyspnea. Axial CT through the heart shows no evidence of cardiomegaly to suggest heart failure. Specifically the left atrium is enlarged
Ashley Davidoff MD TheCommonVein.net 251Lu 135944
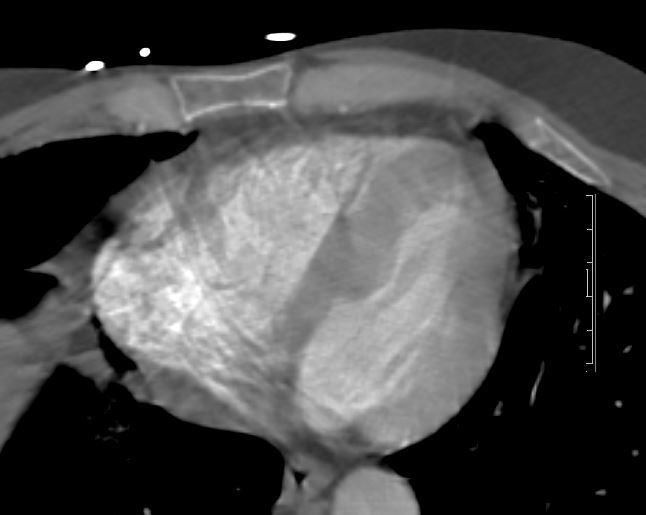
55-year-old male with substance use disorder presents with progressive and now more severe dyspnea. Axial CT through the heart suggests left ventricular hypertrophy which sometimes is associated with cocaine use
Ashley Davidoff MD TheCommonVein.net 251Lu 135945
Enlarged Liver Steatosis

55 year old male with substance use disorder presents with progressive and now more severe dyspnea. CT through the upper abdomen shows an enlarged and mildly fatty liver.
Ashley Davidoff MD TheCommonVein.net 251Lu 135930
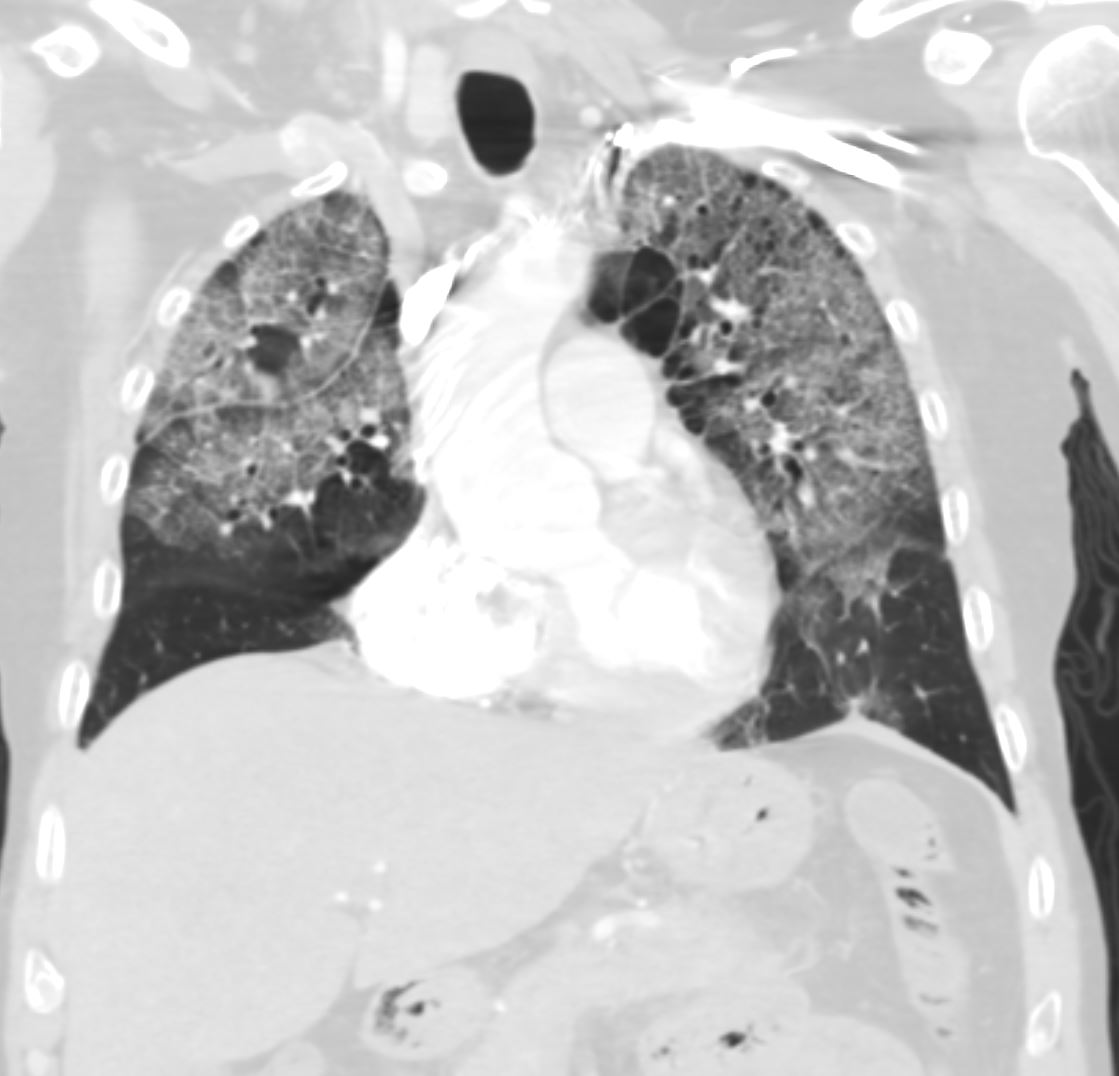
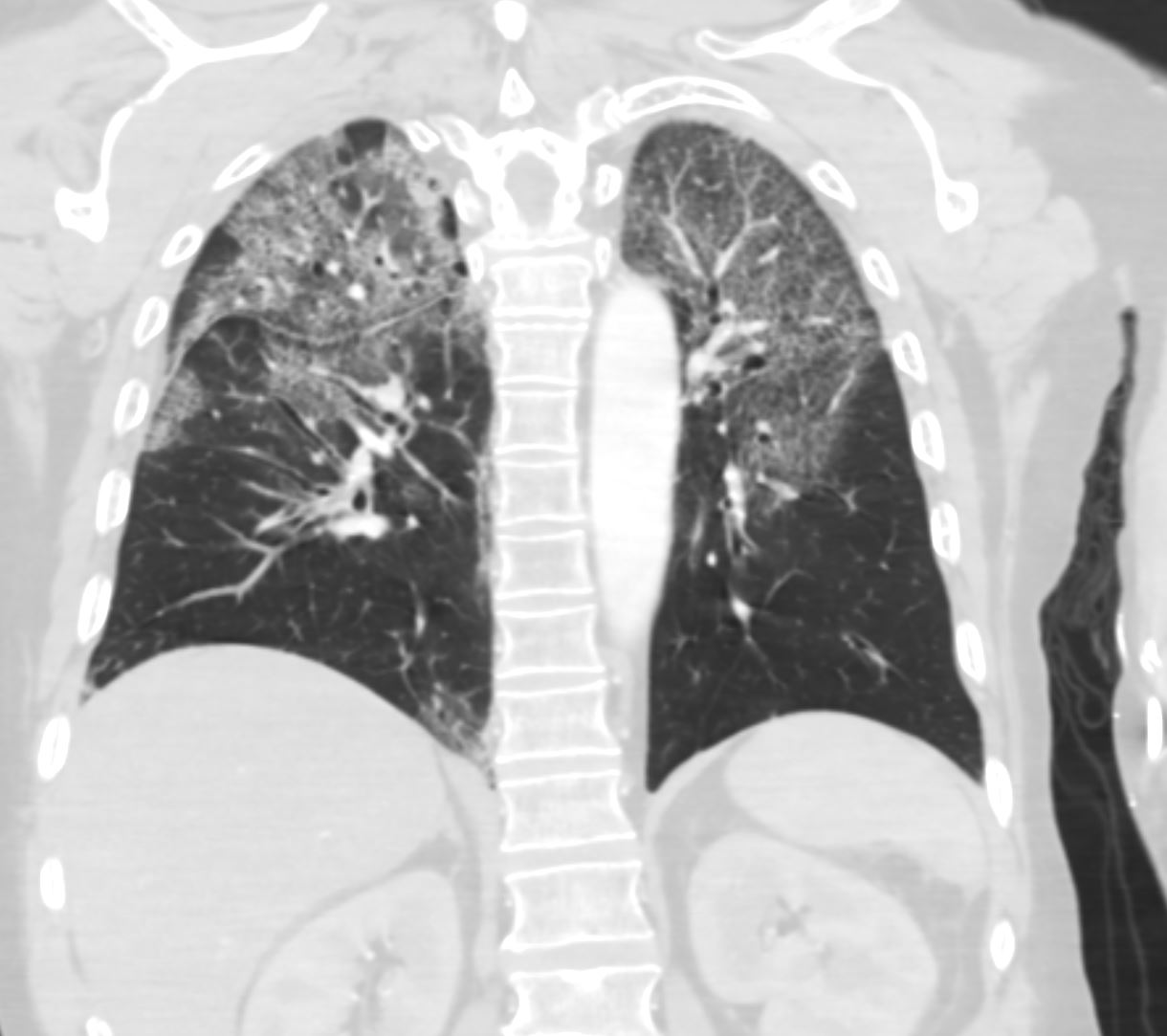
55-year-old male with substance use disorder presents with progressive and now more severe dyspnea. Coronal CT through the anterior lung fields shows upper lobe predominant ground glass changes with thickening of the interlobular septa giving the appearance of “crazy paving”. Thickening and irregularity of the right major fissures is noted.
Progressive inhalational pneumonitis from smoking or cocaine inhalation was suspected. DIP and hypersensitivity pneumonitis remained in the differential diagnosis
Ashley Davidoff MD TheCommonVein.net 251Lu 135931
55-year-old male with substance use disorder presents with progressive and now more severe dyspnea. Coronal CT through the anterior lung fields shows upper lobe predominant ground glass changes with thickening of the interlobular septa. Thickening and irregularity of the right major fissures is noted.
Progressive inhalational pneumonitis from smoking or cocaine inhalation was suspected. DIP and hypersensitivity pneumonitis remained in the differential diagnosis
Ashley Davidoff MD TheCommonVein.net 251Lu 135932
55-year-old male with substance use disorder presents with progressive and now more severe dyspnea. Coronal CT through the anterior lung fields shows upper lobe predominant ground glass changes with thickening of the interlobular septa and a “crazy paving” appearance is suggested. The superior segment of the right lower lobe is also involved. Thickening and irregularity of the right major fissures is noted. LVH is suggested.
Progressive inhalational pneumonitis from smoking or cocaine inhalation was suspected. DIP and hypersensitivity pneumonitis remained in the differential diagnosis
Ashley Davidoff MD TheCommonVein.net 251Lu 135933
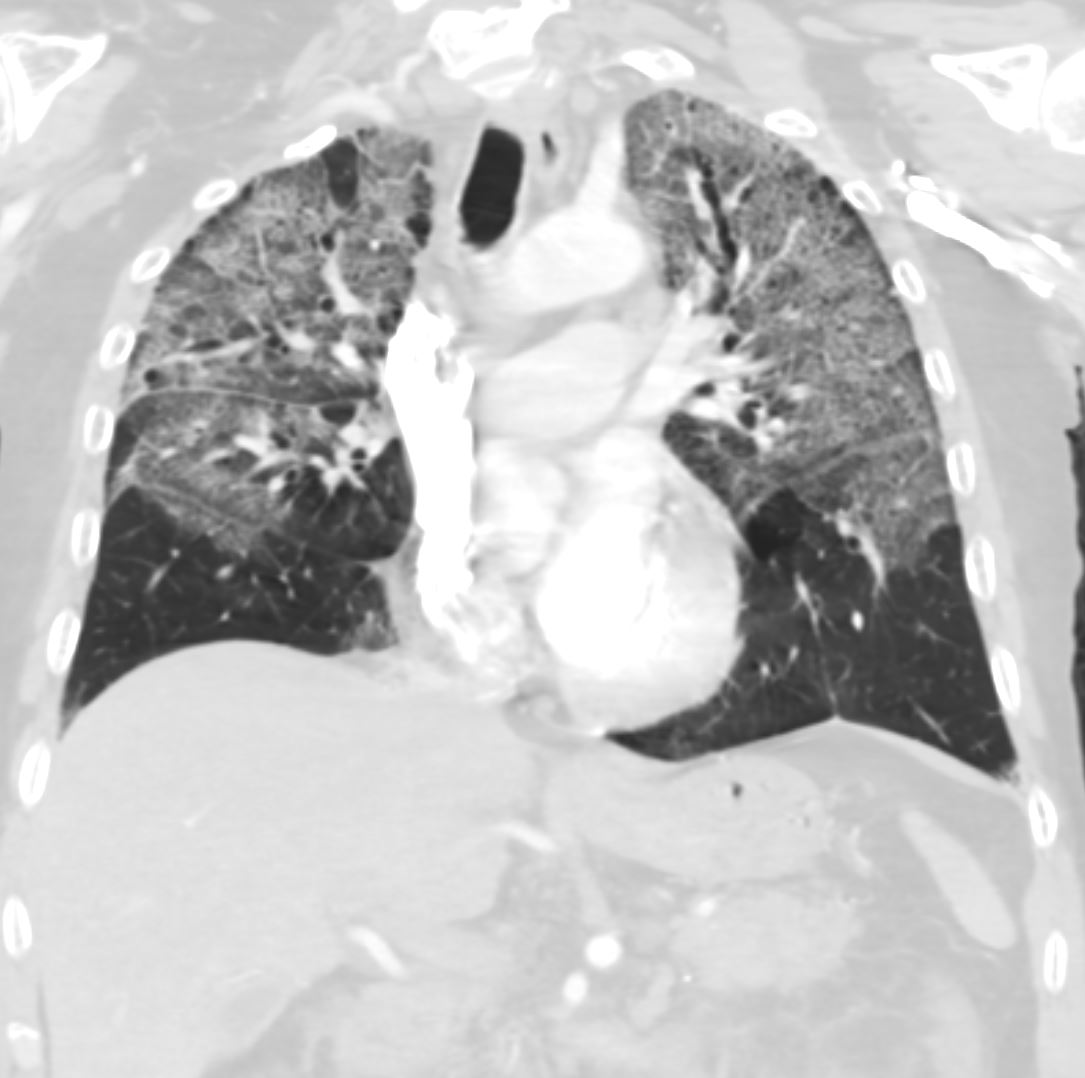
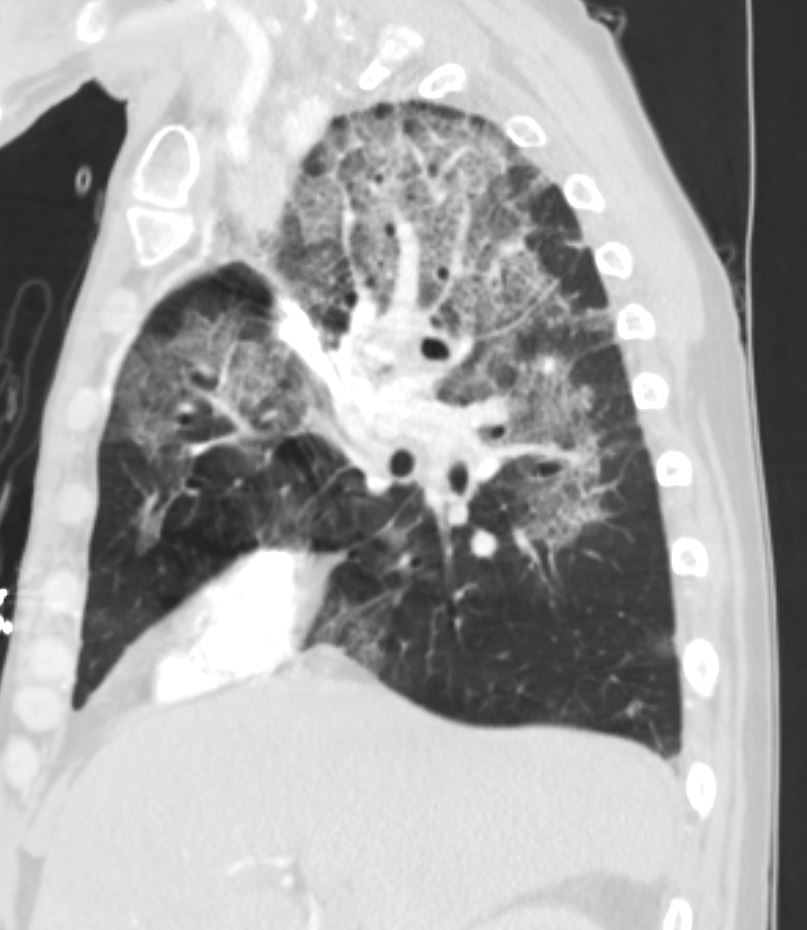
55-year-old male with substance use disorder presents with progressive and now more severe dyspnea. Coronal CT through the mid lung fields shows upper lobe predominant ground glass changes with thickening of the interlobular septa and a “crazy paving” appearance is suggested. The superior segments of the lower lobes are also involved. Thickening and irregularity of the right and left major fissures and the transverse fissure are noted. LVH is suggested.
Progressive inhalational pneumonitis from smoking or cocaine inhalation was suspected. DIP and hypersensitivity pneumonitis remained in the differential diagnosis
Ashley Davidoff MD TheCommonVein.net 251Lu 135934
55-year-old male with substance use disorder presents with progressive and now more severe dyspnea. Coronal CT through the mid lung fields shows upper lobe predominant ground glass changes with thickening of the interlobular septa and a “crazy paving” appearance is suggested. The superior segments of the lower lobes are also involved. Subpleural sparing is suggested. Thickening and irregularity of the right and left major fissures and the transverse fissure are noted.
Progressive inhalational pneumonitis from smoking or cocaine inhalation was suspected. DIP and hypersensitivity pneumonitis remained in the differential diagnosis
Ashley Davidoff MD TheCommonVein.net 251Lu 135935
55-year-old male with substance use disorder presents with progressive and now more severe dyspnea. Coronal CT through the posterior lung fields shows upper lobe predominant ground glass changes with thickening of the interlobular septa and a “crazy paving” appearance is suggested. The superior segments of the lower lobes are also involved. Subpleural sparing is suggested.
Progressive inhalational pneumonitis from smoking or cocaine inhalation was suspected. DIP and hypersensitivity pneumonitis remained in the differential diagnosis
Ashley Davidoff MD TheCommonVein.net 251Lu 135936
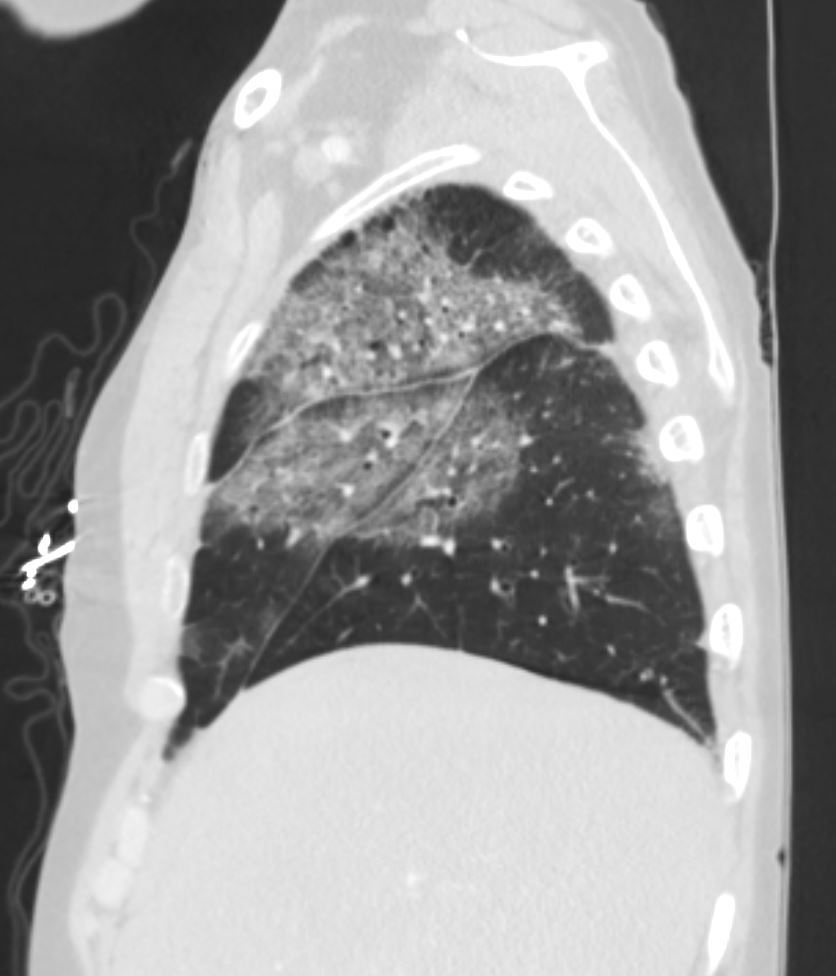
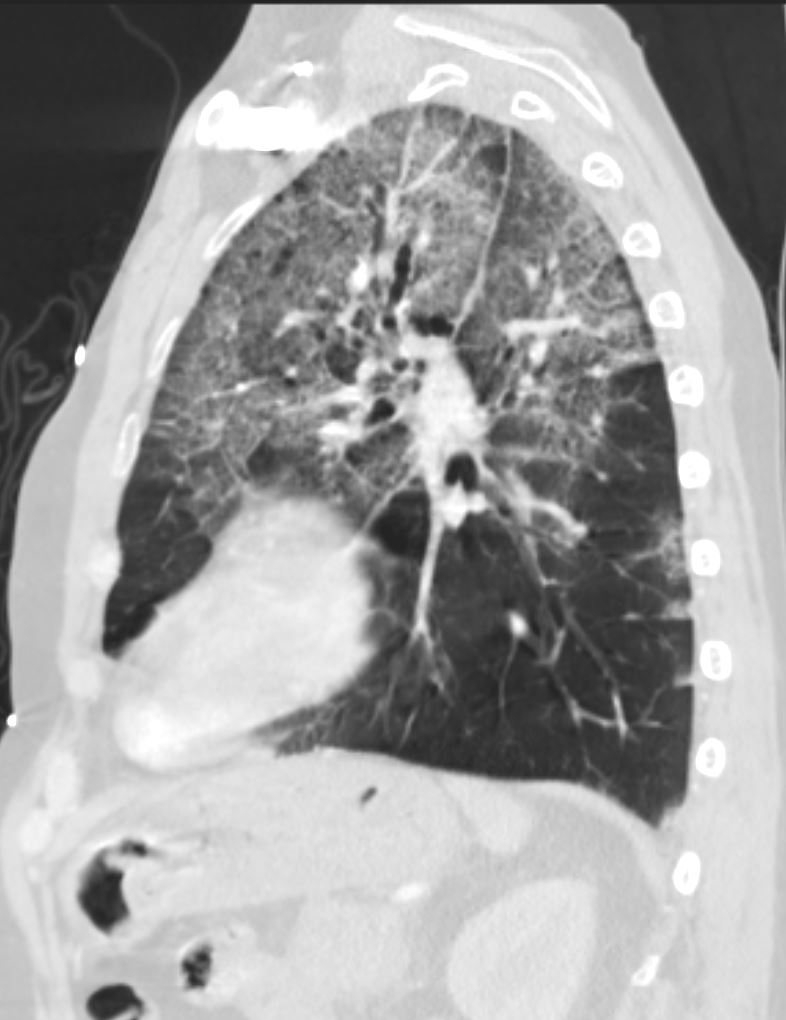
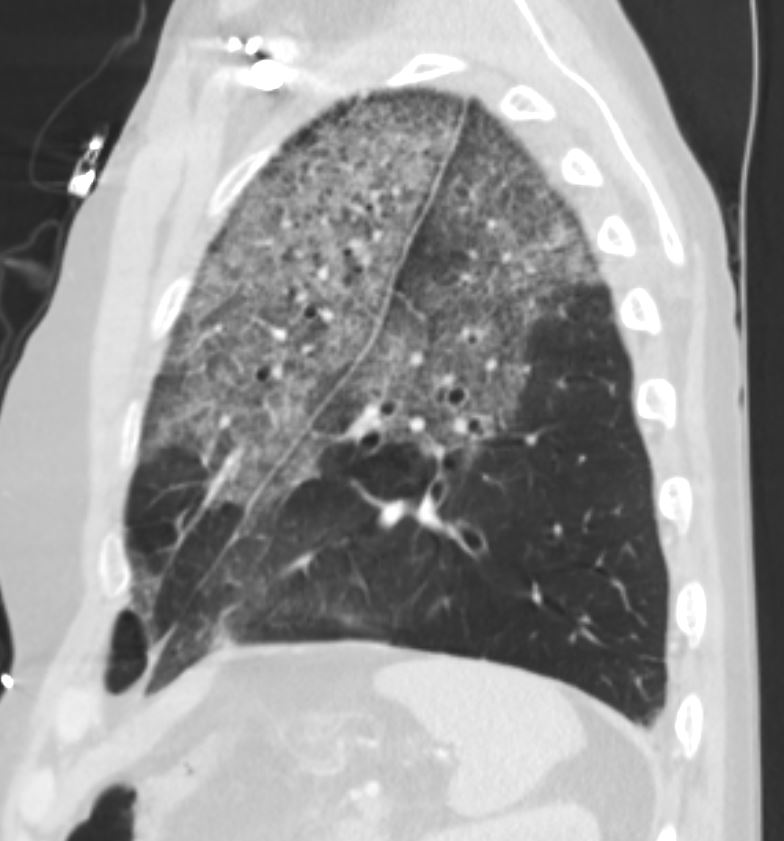
55-year-old male with substance use disorder presents with progressive and now more severe dyspnea. Sagittal CT through the right lung field shows ground glass changes in the upper mid and superior segment of the lower lobe. Subpleural sparing is suggested anteriorly. The fissures of the areas of involved lung are focally thickened
Progressive inhalational pneumonitis from smoking or cocaine inhalation was suspected. DIP and hypersensitivity pneumonitis remained in the differential diagnosis
Ashley Davidoff MD TheCommonVein.net 251Lu 135937
55-year-old male with substance use disorder presents with progressive and now more severe dyspnea. Sagittal CT through the right lung field shows ground glass changes in the upper mid and superior segment of the lower lobe. The fissures of the areas of involved lung are focally thickened
Progressive inhalational pneumonitis from smoking or cocaine inhalation was suspected. DIP and hypersensitivity pneumonitis remained in the differential diagnosis
Ashley Davidoff MD TheCommonVein.net 251Lu 135938
55-year-old male with substance use disorder presents with progressive and now more severe dyspnea. Sagittal CT through the right lung field shows ground glass changes in the upper mid and superior segment of the lower lobe. The fissures of the areas of involved lung are focally thickened
Progressive inhalational pneumonitis from smoking or cocaine inhalation was suspected. DIP and hypersensitivity pneumonitis remained in the differential diagnosis
Ashley Davidoff MD TheCommonVein.net 251Lu 135939
55-year-old male with substance use disorder presents with progressive and now more severe dyspnea. Sagittal CT through the right lung field shows ground glass changes in the upper mid and superior segment of the lower lobe. The fissures of the areas of involved lung are focally thickened. There is subpleural sparing
Progressive inhalational pneumonitis from smoking or cocaine inhalation was suspected. DIP and hypersensitivity pneumonitis remained in the differential diagnosis
Ashley Davidoff MD TheCommonVein.net 251Lu 135940
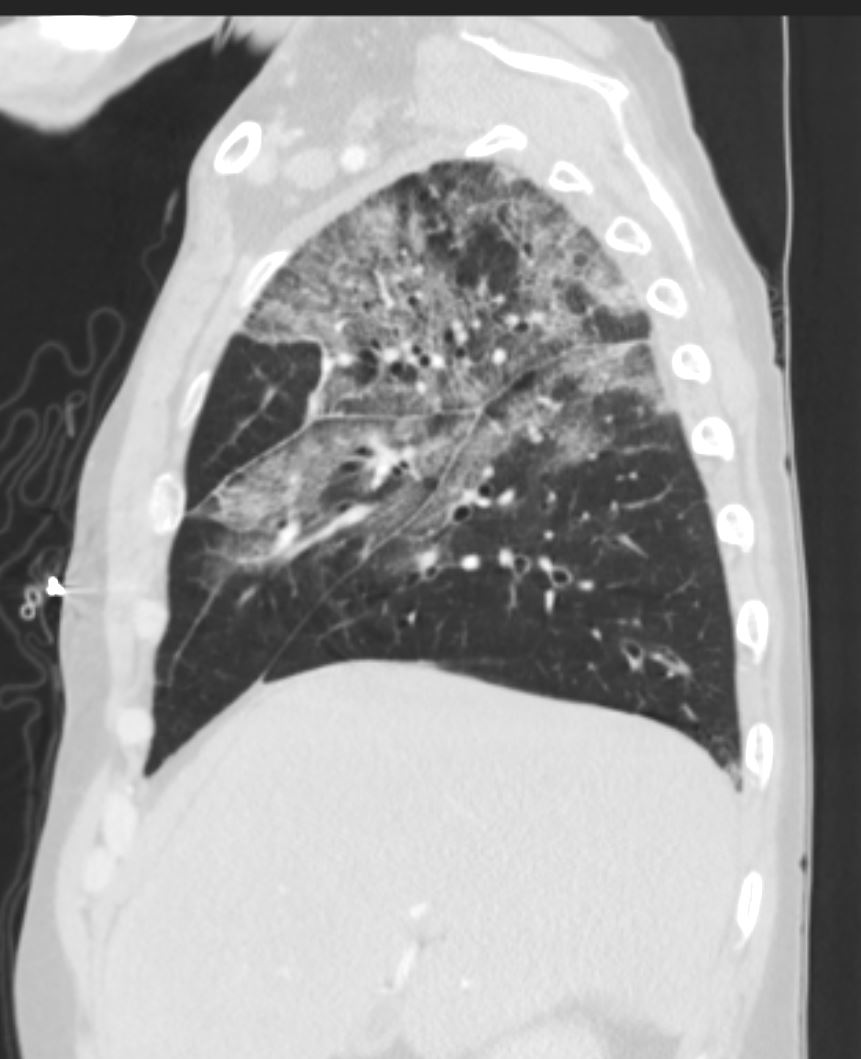
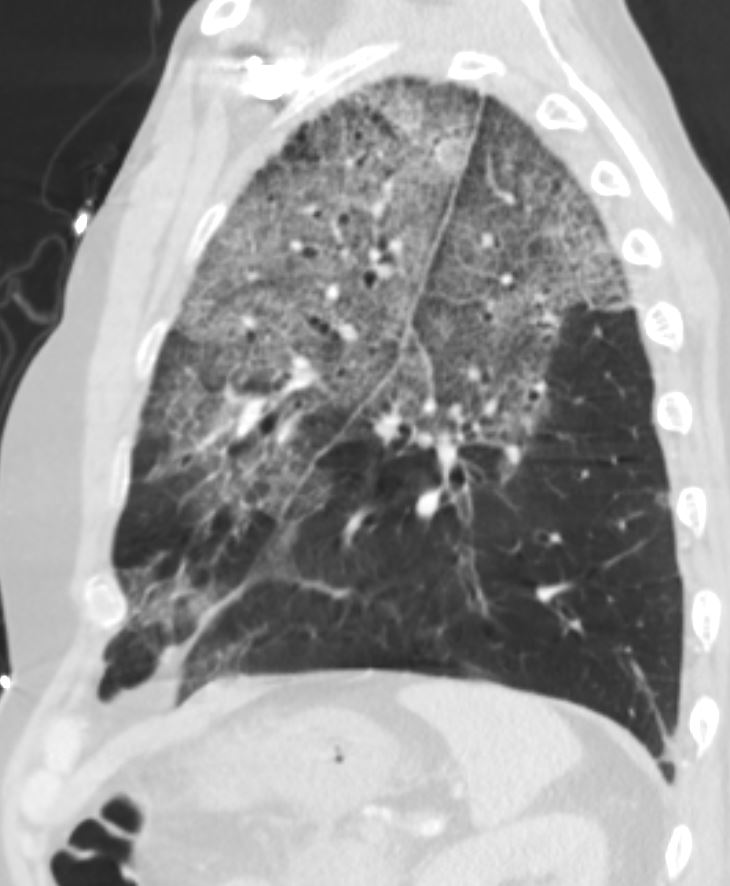
55-year-old male with substance use disorder presents with progressive and now more severe dyspnea. Sagittal CT through the left lung field shows ground glass changes in the upper mid and superior segment of the lower lobe. The fissures of the areas of involved lung are focally thickened. There is subpleural sparing.
Progressive inhalational pneumonitis from smoking or cocaine inhalation was suspected. DIP and hypersensitivity pneumonitis remained in the differential diagnosis
Ashley Davidoff MD TheCommonVein.net 251Lu 135941
55-year-old male with substance use disorder presents with progressive and now more severe dyspnea. Sagittal CT through the left lung field shows ground glass changes in the upper mid and superior segment of the lower lobe. The fissures of the areas of involved lung are focally thickened. There is subpleural sparing.
Progressive inhalational pneumonitis from smoking or cocaine inhalation was suspected. DIP and hypersensitivity pneumonitis remained in the differential diagnosis
Ashley Davidoff MD TheCommonVein.net 251Lu 135942
55-year-old male with substance use disorder presents with progressive and now more severe dyspnea. Sagittal CT through the left lung field shows ground glass changes in the upper mid and superior segment of the lower lobe. The fissures of the areas of involved lung are focally thickened. There is subpleural sparing and “crazy paving” pattern suggested with thickened interlobular septa.
Progressive inhalational pneumonitis from smoking or cocaine inhalation was suspected. DIP and hypersensitivity pneumonitis remained in the differential diagnosis
Ashley Davidoff MD TheCommonVein.net 251Lu 135943
Improved CT after 2 Months of Steroids

55-year-old male with substance use disorder presents with a history of inhalational pneumonitis likely from cocaine presents 2 months after treatment with steroids. Scout CT shows clear lungs
Ashley Davidoff MD TheCommonVein.net 251Lu 135946
55-year-old male with substance use disorder presents with a history of inhalational pneumonitis likely from cocaine presents 2 months after treatment with steroids. Axial CT through the upper lung fields show significant improvement with mild residual patchy ground glass change particularly in the left upper lobe
Ashley Davidoff MD TheCommonVein.net 251Lu 135948
55-year-old male with substance use disorder presents with a history of inhalational pneumonitis likely from cocaine presents 2 months after treatment with steroids. Axial CT through the upper lung fields show significant improvement with mild residual patchy ground glass change particularly in the left upper lobe
Ashley Davidoff MD TheCommonVein.net 251Lu 135948
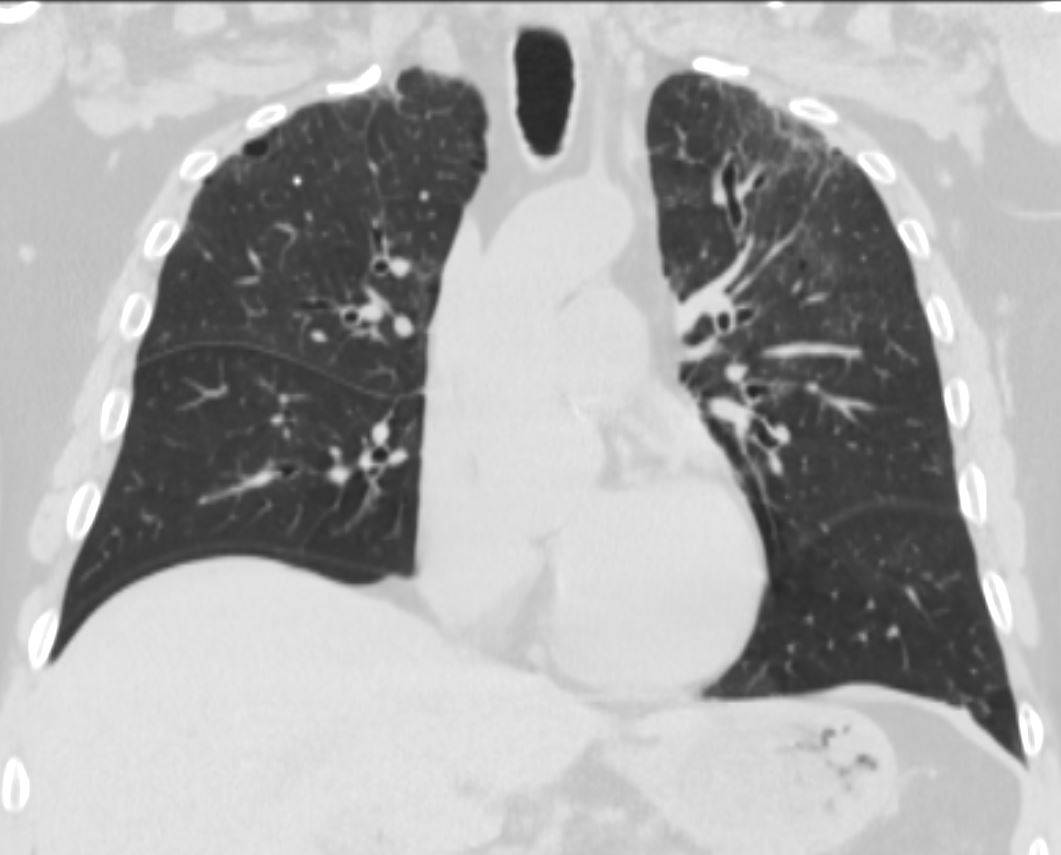
55-year-old male with substance use disorder presents with a history of inhalational pneumonitis likely from cocaine presents 2 months after treatment with steroids. Coronal CT through the anterior lung fields show significant improvement with mild residual patchy ground glass change particularly in the left upper lobe with a single focus of mild bronchiectasis
Ashley Davidoff MD TheCommonVein.net 251Lu 135949

55-year-old male with substance use disorder presents with a history of inhalational pneumonitis likely from cocaine presents 2 months after treatment with steroids. Coronal CT through the carina shows significant improvement
Ashley Davidoff MD TheCommonVein.net 251Lu 135950
