History
A 32-year-old female presents with chronic dyspnea, progressive muscle weakness, and fatigue over the past year. She reports difficulty climbing stairs and rising from a seated position due to proximal muscle weakness. She also experiences joint pain and stiffness, accompanied by crackles at the lung bases on auscultation.
Examination
- Pulmonary findings: Basilar crackles, consistent with interstitial lung disease (ILD).
- Musculoskeletal findings:
- Proximal muscle weakness, most prominent in the shoulders and hips, suggestive of myositis.
- Tenderness of the proximal muscles without significant atrophy.
- Skin findings (optional, if present): No obvious rash
Blood Tests
- Positive anti-Jo-1 antibody, highly suggestive of antisynthetase syndrome.
- Elevated creatine kinase (CK) and aldolase, consistent with active myositis.
- Mild elevation of inflammatory markers (ESR, CRP).
CXR 1 year Ago
Diffuse Dominant Basilar Changes

History
1 year ago, a 32-year-old female presented with progressive dyspnea and muscle weakness, ultimately diagnosed with antisynthetase syndrome based on clinical, serological, and imaging findings.
Findings
CXR frontal view demonstrates diffuse ground-glass opacities (GGO), most prominent in the basal lung regions, with mild interstitial prominence in the upper lung fields.
The lung volumes are preserved, and there is no evidence of significant consolidation or pleural effusion.
Ashley Davidoff MD TheCommonVein.net (b12386-01a)(312Lu)
Comment
The findings on chest radiograph are limited and nonspecific, showing a diffuse process that could reflect an acute or subacute inflammatory condition. While the clinical history suggests interstitial lung disease (ILD) in the context of antisynthetase syndrome, the differential diagnosis remains broad and includes a variety of inflammatory and infectious diseases.
CXR is limited in its ability to fully characterize interstitial lung disease or identify specific patterns, but it provides clues to the presence of an acute process that warrants further investigation with advanced imaging (e.g., CT).
Radiological Pearls
Limitations of Chest X-ray:
Poor sensitivity for subtle interstitial changes or early ILD.
History
1 year prior, a 32-year-old female presented with progressive dyspnea and muscle weakness. She was diagnosed with antisynthetase syndrome, characterized by interstitial lung disease (ILD) and systemic autoimmune features.
Findings
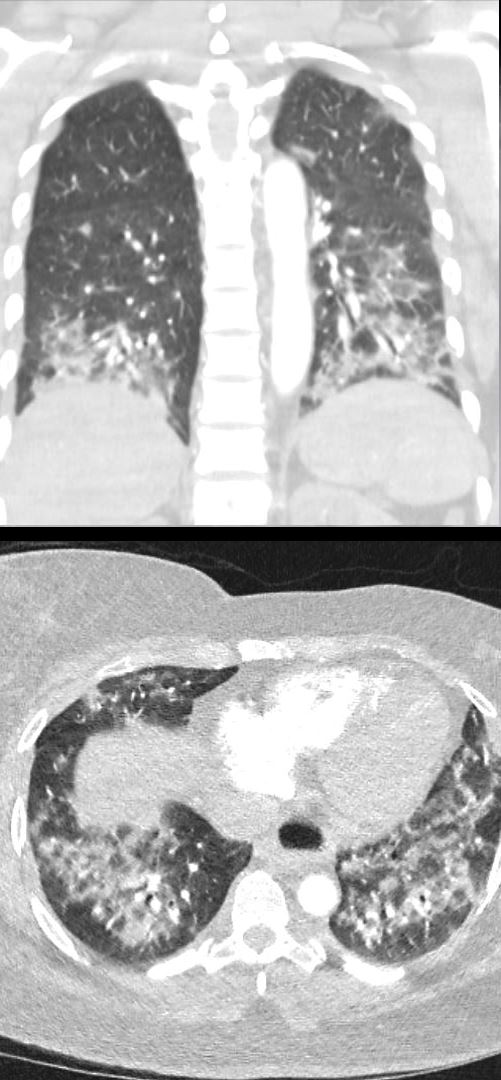
Coronal CT:
NSIP pattern with ground-glass opacities (GGO) predominantly in the basal regions, showing a bronchovascular distribution and subpleural sparing, consistent with the diagnosis of antisynthetase syndrome-associated ILD.
Axial CT:
Similar changes are noted, with bronchovascular GGO and subpleural sparing.
There is no evidence of traction bronchiectasis or bronchiolectasis, suggesting a cellular NSIP subtype, which is more inflammatory and associated with a better prognosis.
Additionally, the esophagus is dilated, with a suggestion of an air-fluid level, which may reflect esophageal dysmotility, a finding commonly associated with scleroderma or mixed collagen vascular disease (MCTD).
Ashley Davidoff MD TheCommonVein.net (b12386-01b)(312Lu)
Comment
The imaging findings, including NSIP pattern ILD and a dilated esophagus with air-fluid level, raise the possibility of an overlap syndrome or mixed collagen vascular disease (MCTD). While the esophageal findings could be incidental, they may suggest an additional autoimmune disorder, such as scleroderma, coexisting with the known antisynthetase syndrome.
Scleroderma diagnosis would require additional clinical and serological correlation, including the presence of esophageal dysmotility or gastroesophageal reflux symptoms, and specific antibody testing, such as anti-centromere antibodies (limited scleroderma) or anti-Scl-70 antibodies (diffuse scleroderma).
Mixed Collagen Vascular Disease (MCTD): This diagnosis is suggested by overlapping features of different connective tissue diseases (e.g., scleroderma, myositis, lupus) and is supported by the presence of anti-U1 RNP antibodies and a combination of systemic clinical findings, such as ILD, Raynaud’s phenomenon, arthritis, and esophageal dysmotility.
What it Takes to Confirm the Diagnosis:
Scleroderma:
Clinical features: Raynaud’s phenomenon, skin thickening, esophageal dysmotility, or digital ulcers.
Serology:
Anti-Scl-70 antibody: Highly specific for diffuse systemic sclerosis.
Anti-centromere antibody: Associated with limited systemic sclerosis.
Imaging: Dilated esophagus on CT supports the diagnosis.
Mixed Collagen Vascular Disease (MCTD):
Clinical features: Overlap of features from systemic sclerosis, polymyositis/dermatomyositis, and lupus.
Serology: Presence of anti-U1 RNP antibodies is diagnostic.
Radiological Pearls
NSIP Pattern on CT:
Basal-predominant GGO with bronchovascular distribution.
Subpleural sparing helps differentiate NSIP from UIP.
Absence of traction bronchiectasis suggests a cellular NSIP subtype.
Esophageal Findings on CT:
A dilated esophagus with an air-fluid level is indicative of dysmotility, frequently seen in scleroderma or MCTD.
Esophageal dysmotility is often associated with systemic sclerosis but may also overlap with other collagen vascular diseases.
Management Implications
If scleroderma or MCTD is confirmed, management would include addressing esophageal dysmotility with proton pump inhibitors (PPIs) or promotility agents and monitoring for other systemic complications.
Comprehensive autoimmune serology and close collaboration with rheumatology would guide further diagnosis and treatment.
History
A 32-year-old female with a diagnosis of antisynthetase syndrome presents with an acute flare characterized by severe hypoxemia, requiring intubation and admission to the ICU. chest X-ray was obtained 1 month later during recovery.
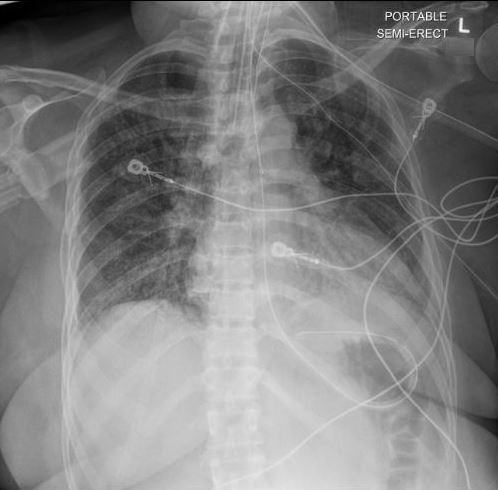
Findings
CXR frontal view demonstrates diffuse bilateral opacities, with a lower lobe predominance.
The opacities show mild air bronchograms, consistent with alveolar involvement.
The lung volumes are preserved, and there is no significant pleural effusion or consolidation suggestive of lobar pneumonia.
Ashley Davidoff MD TheCommonVein.net (b12386-02a)(312Lu)
Comment
The imaging findings reflect an acute exacerbation of antisynthetase syndrome-associated interstitial lung disease (ILD). The diffuse bilateral opacities and lower lobe predominance are consistent with an acute inflammatory process, such as diffuse alveolar damage or a worsening NSIP pattern, which are known complications in severe flares of antisynthetase syndrome.
Differential Diagnosis:
The findings may also overlap with other acute processes, including infection, aspiration, or diffuse alveolar hemorrhage, all of which should be considered in this clinical setting.
The clinical and laboratory context (e.g., markers of infection or bleeding) are critical for distinguishing these causes.
Radiological Pearls
Lower lobe predominance: Common in NSIP pattern ILD but also seen in aspiration or infection.
Air bronchograms: Indicative of alveolar filling processes (e.g., inflammation, infection, or hemorrhage).
Limitations of CXR:
CXR cannot differentiate between NSIP exacerbation, infection, or diffuse alveolar damage.
CT imaging is often required to provide more definitive characterization of the underlying process.
