40 y F with hx of smoking (tobacco, marijuana) who also had occupational exposures and developed an ILD initially thought to most likely be hypersensitivity pneumonitis or RB-ILD but acutely worsened and now has a confirmed sarcoidal process. She required O2 but responded well to prednisone and addition of methotrexate (at 20 mg weekly). Strated tret,ment with with a biologic, remicade or equivalent remaining on prednisone 20mg daily and methotrexate 20mg weekly until remicade is started
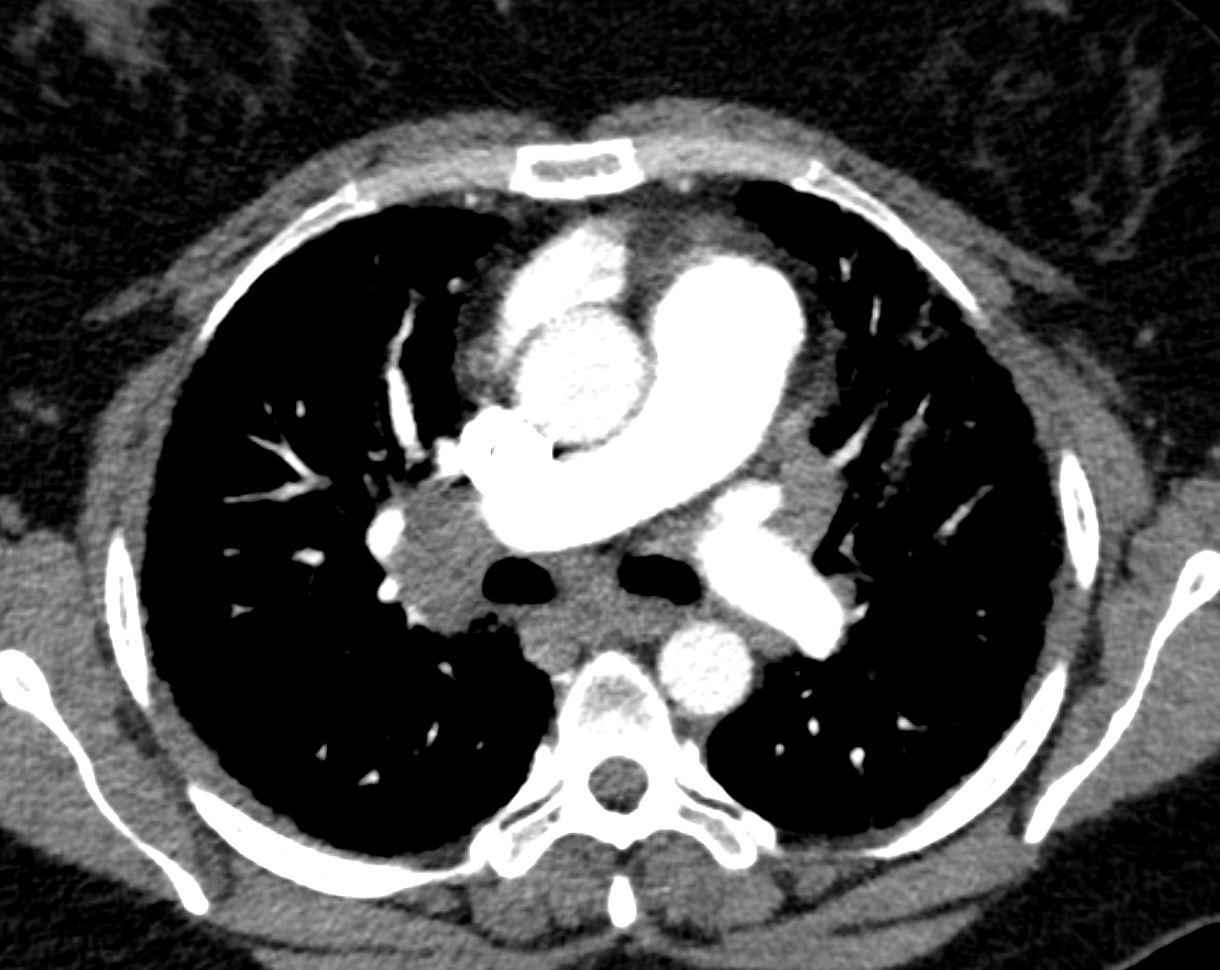
Cardiac MRI is not suggestive of cardiac sarcoid. Her follow up CT chest shows no progression but significant parenchymal lung disease and fibrosis. Has hypercalcemia
Around 2 years ago she was able to walk work and live normally. She says over the following couple of months her health deteriorated and 4 months later developed chest pain. Overall her symptoms have gradually worsened and 4months therafter she was hospitalized at that stage she was thought to have scleroderma associated interstitial lung disease based on the finding of a mildly elevated Scl70 antibody

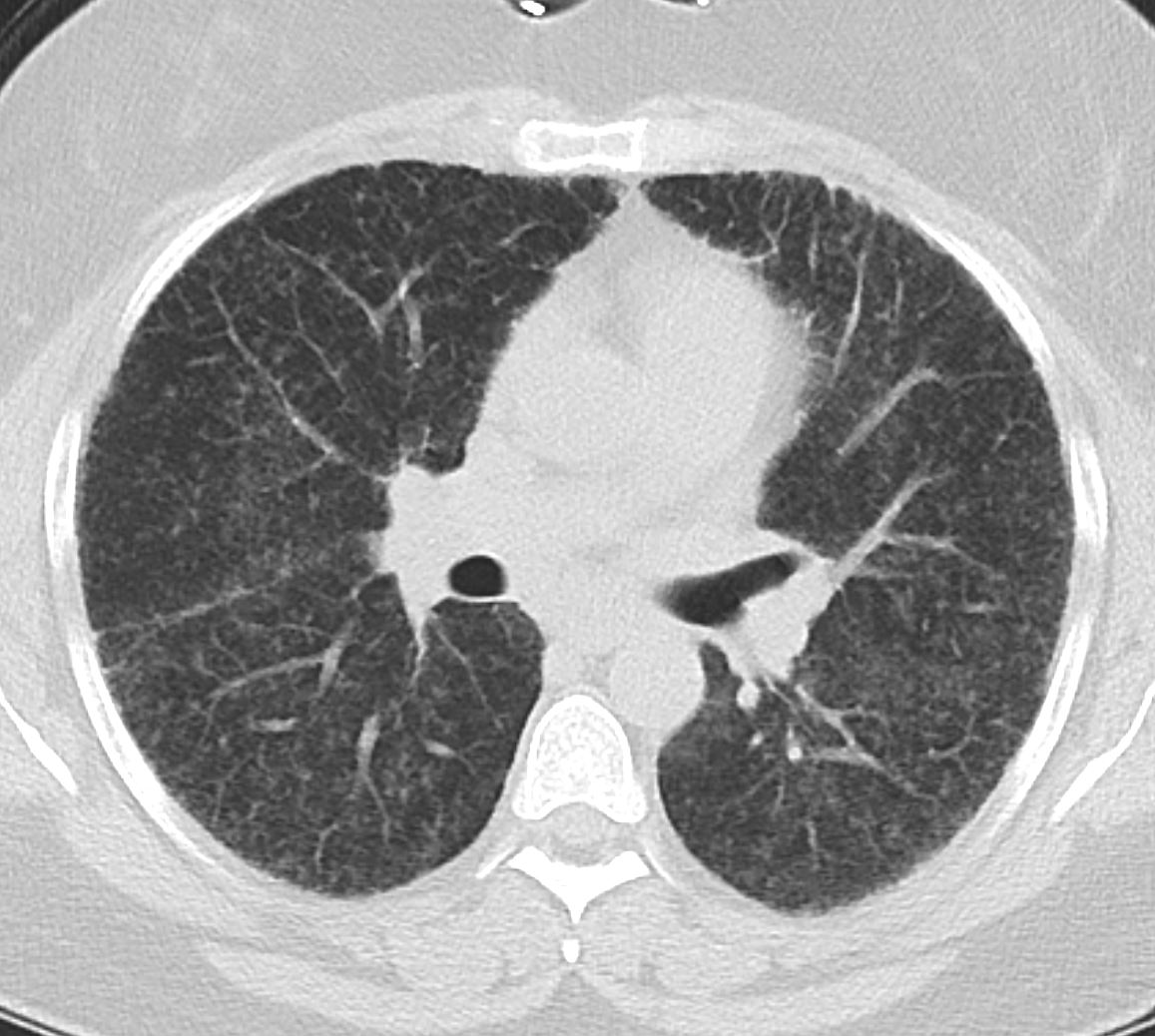

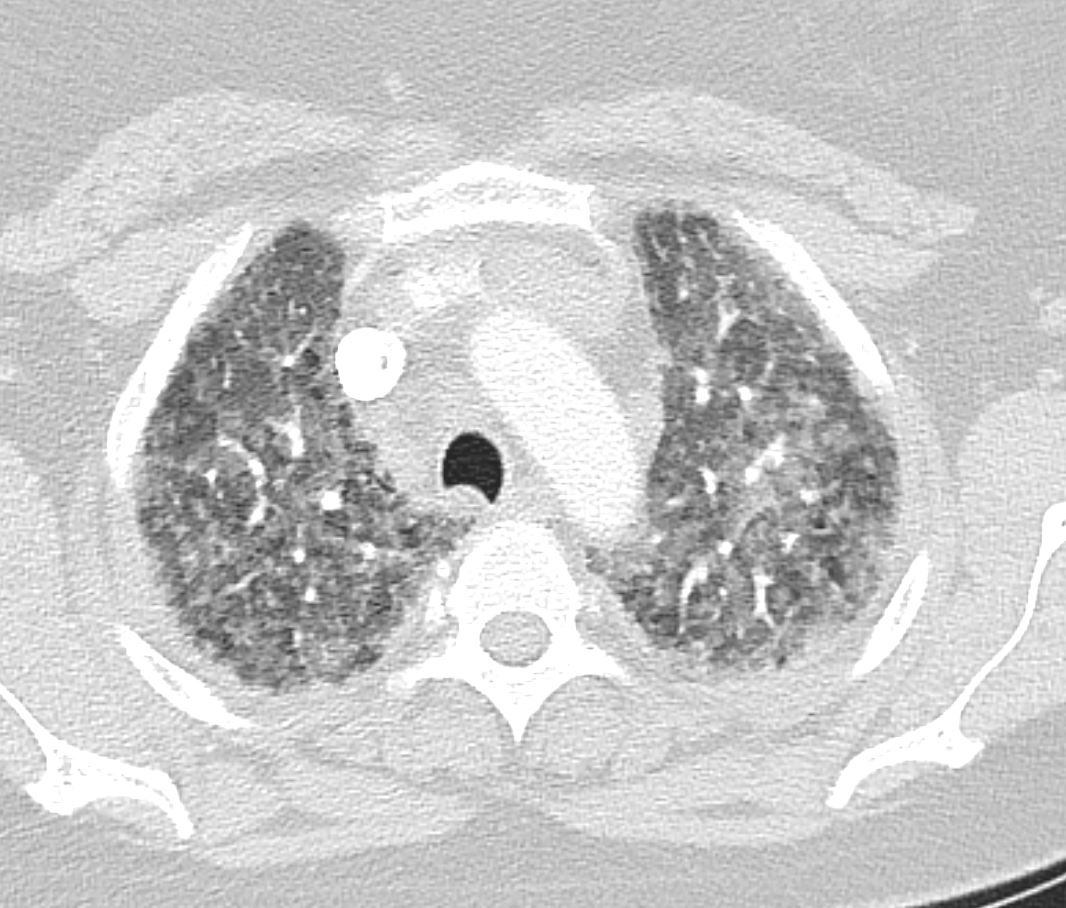
Nodularity of the fissures
Nodularity of the interlobular septa
Nodularity of the interlobular septa
Nodularity of the interlobular septa
Nodularity of the interlobular septa
Nodularity of the interlobular septa
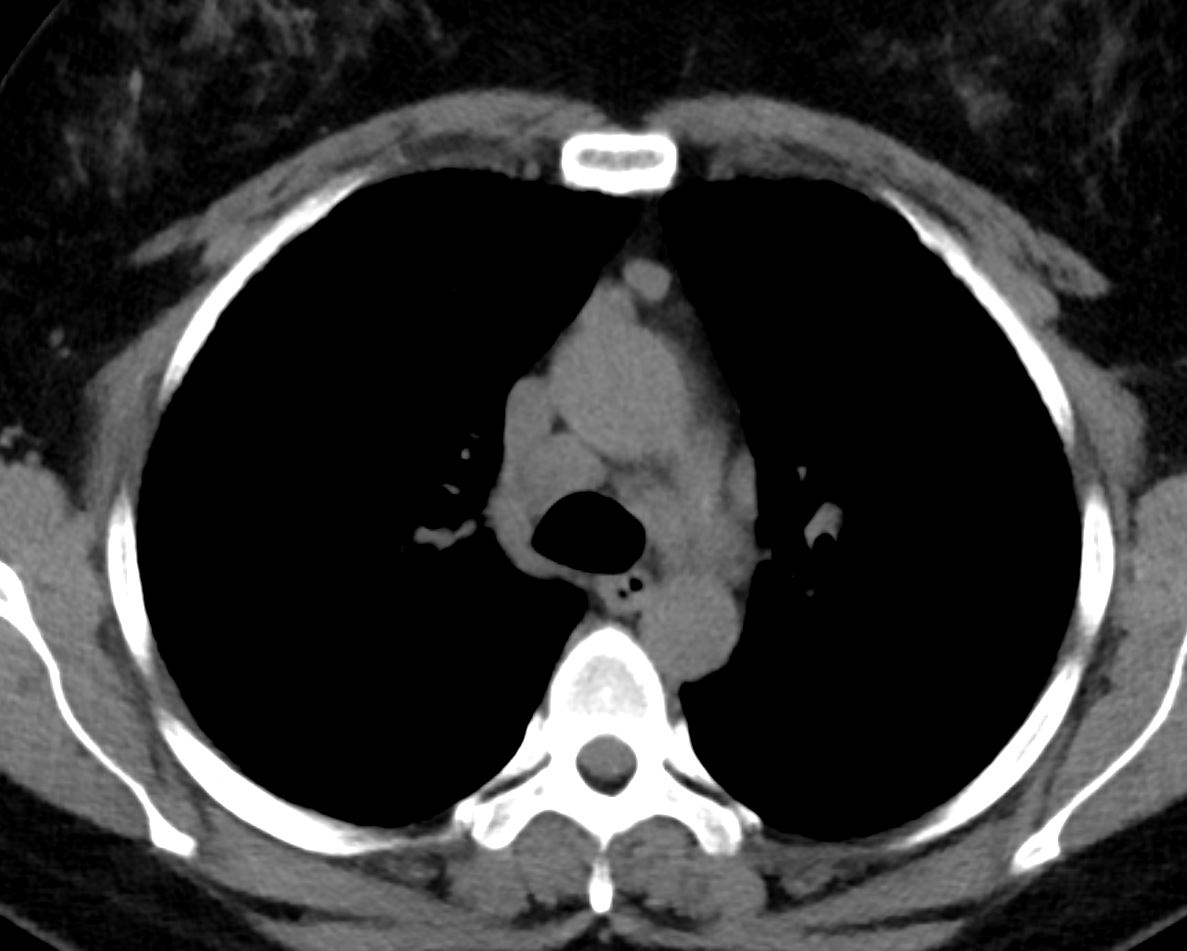
Mild lymphadenopathy

Mild lymphadenopathy
3 months later

3 months later
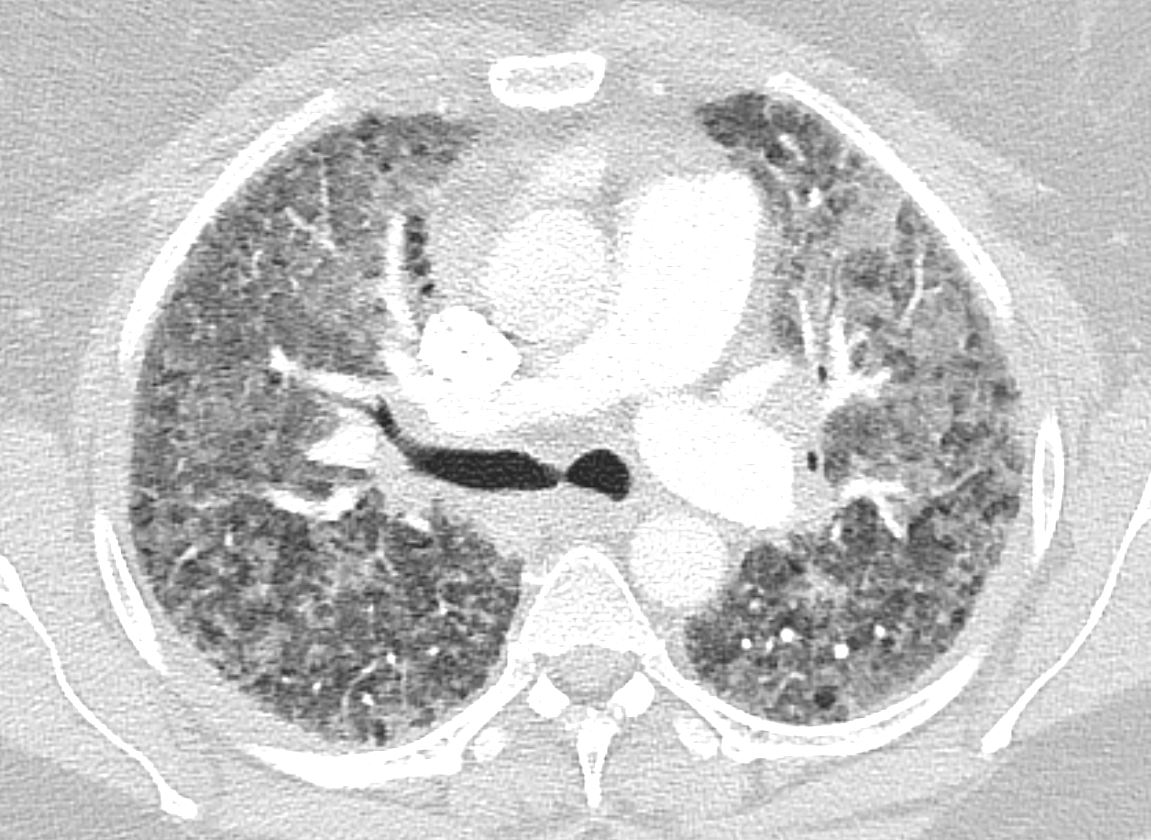
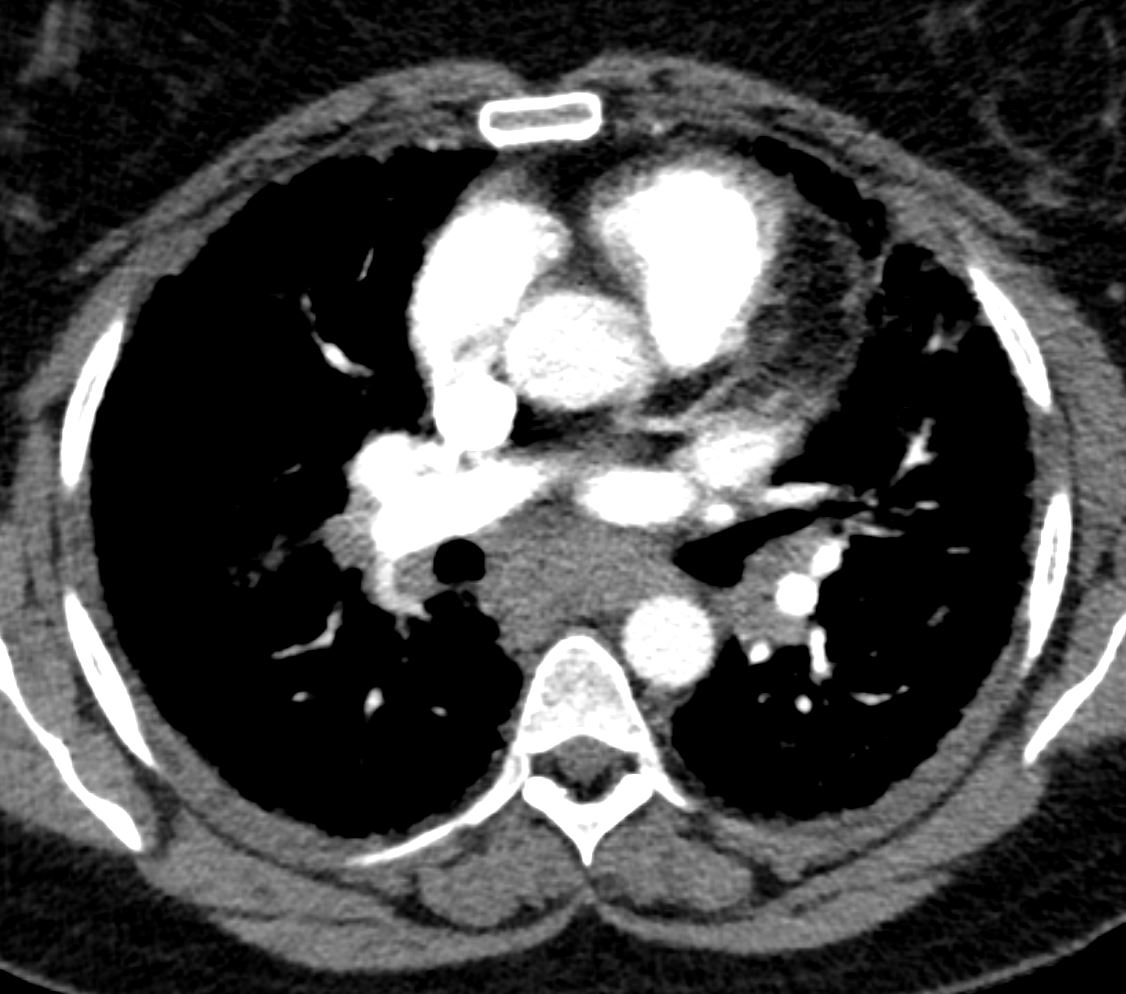
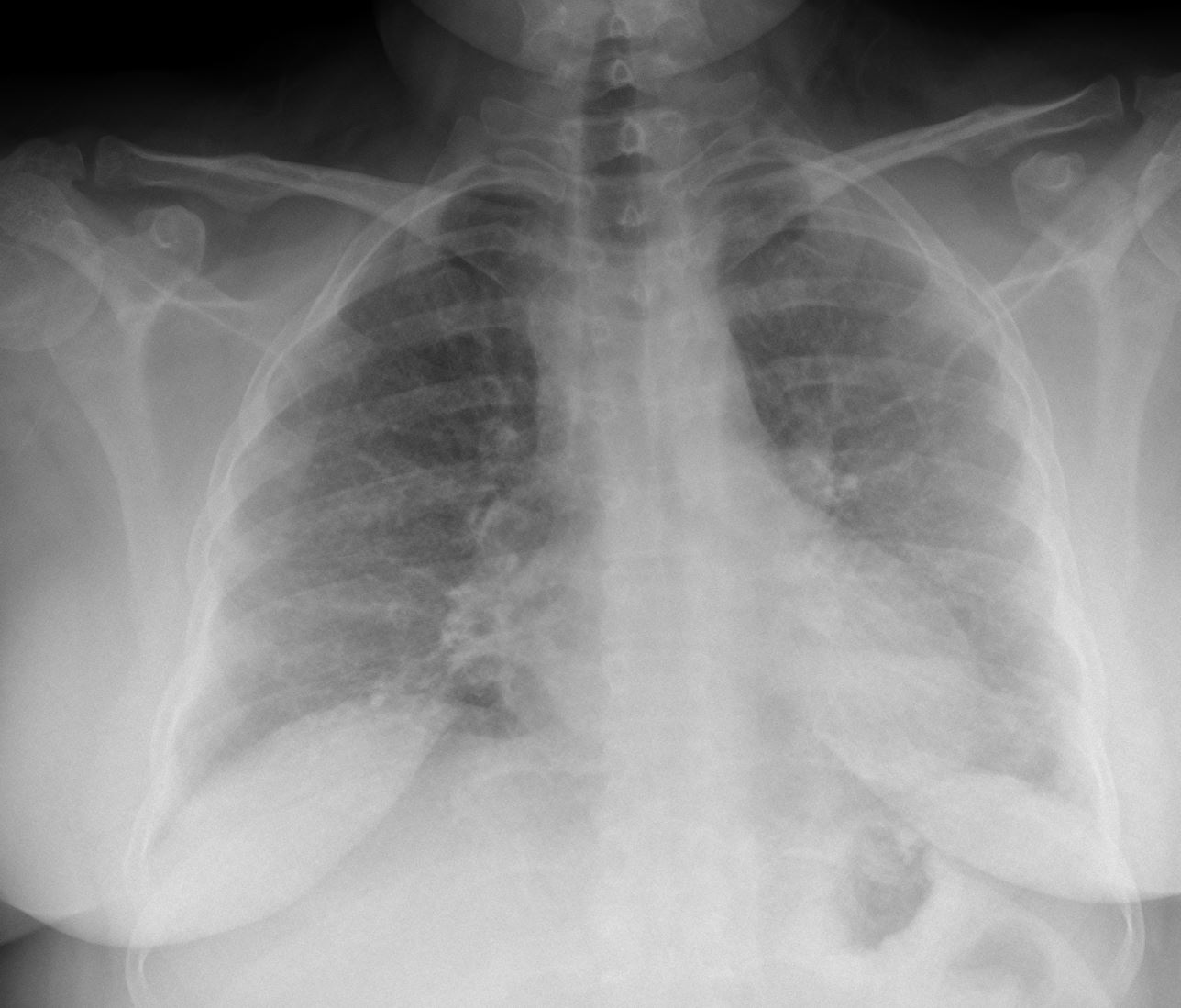
CTA Chest about 1 year ago There are diffuse ground glass opacities, interlobular septal thickening with a background of hundreds of centrilobular nodules. They are not as well seen due to the GGO’s. Significant mediastinal LAD. Overall, much worse than the the prior scan



Bronchoscopy and EBUS performed. Both node and transbronchial biopsy identified well formed granulomas, non-necrotizing, with negative microbial stains. She was started on prednisone 30mg. . Initial imaging was consistent with RB-ILD or HP. Path is consistent with sarcoidosis or sarcoidal reaction. Unusual in the severity of hypoexmia. Recommended adding methotrexate.
TE
Normal EF, mild MR.
CR 3.4, HP panel negative, ANA 1:40, SCl70 1.1 (<1.0)
Negative: anti-centromere, SSA, SSB, HIV, dsDNA, C3, C4, CCP, RF, SM/RNP


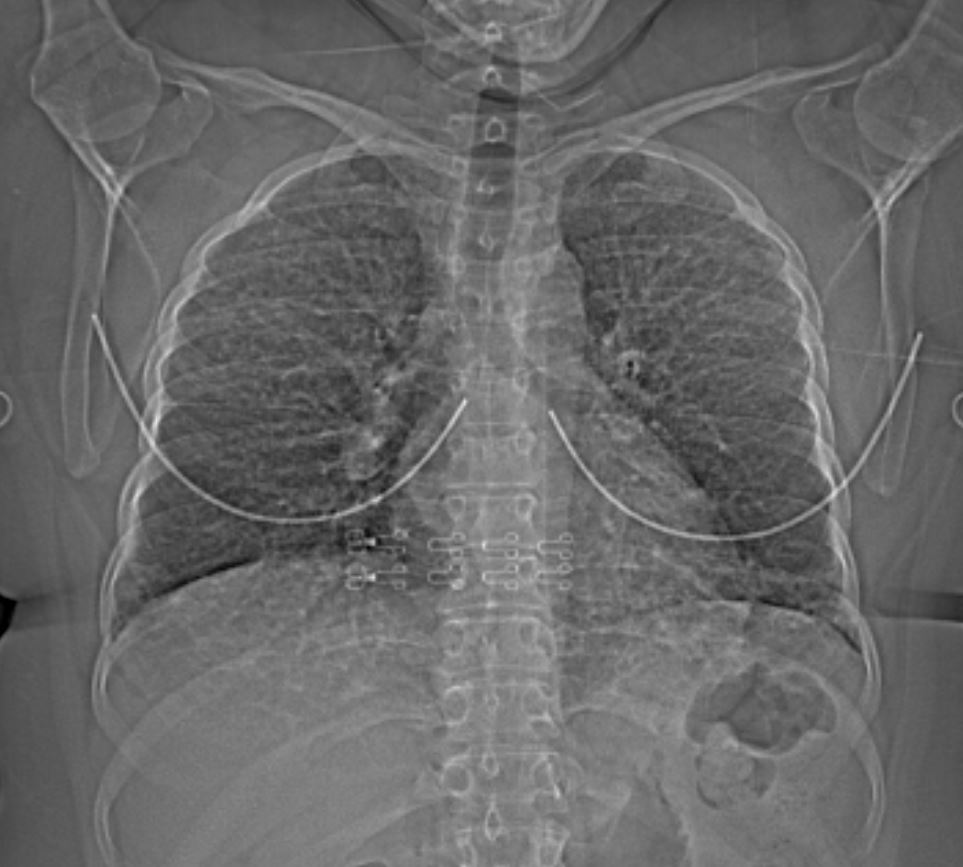
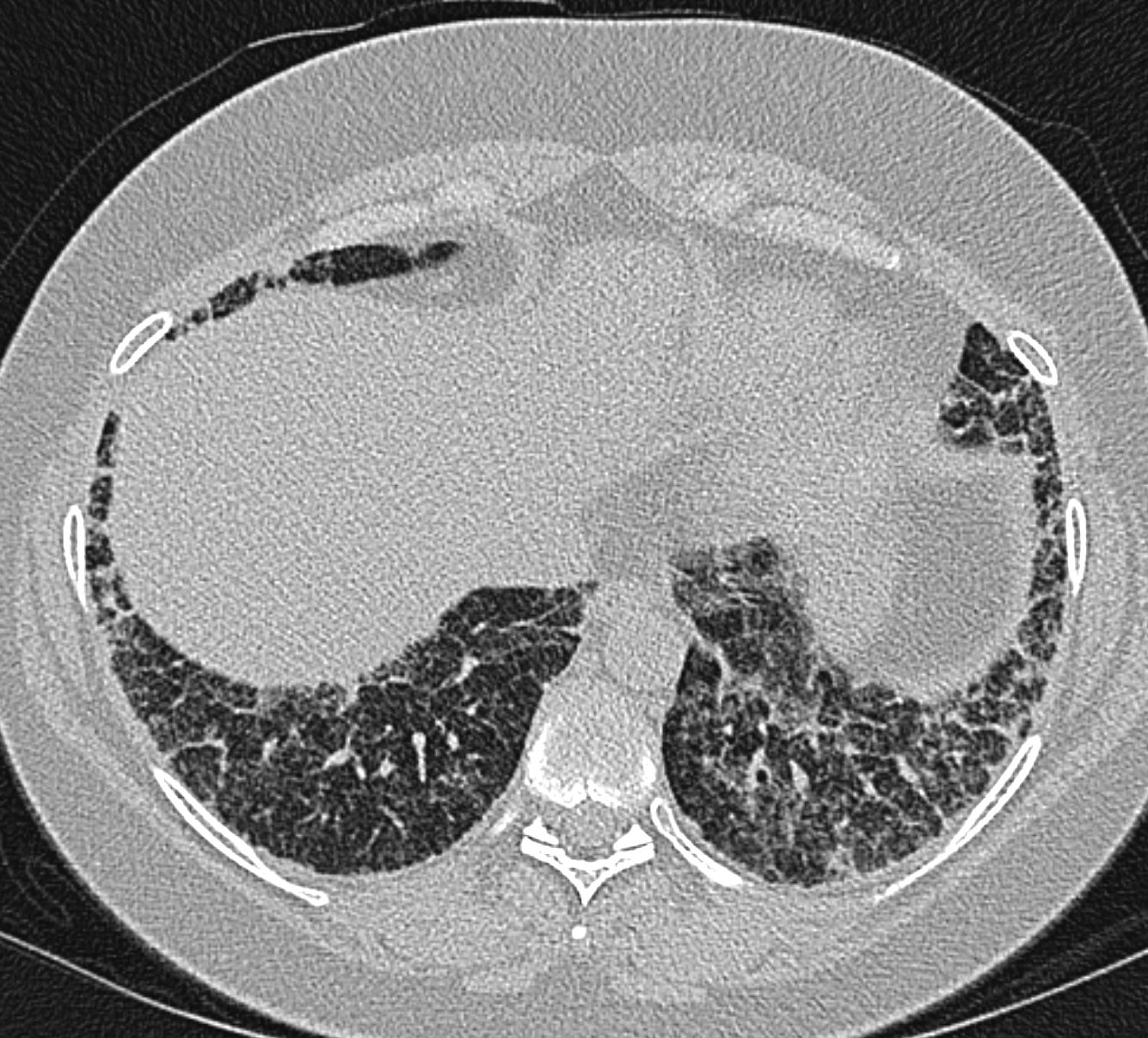
progressive extensive diseae with ground glass changes and micronodularity

progressive extensive disease with ground glass changes and micronodularity and nodularity of the interlobular septa and nodularity of the pleura

progressive extensive disease with ground glass changes and micronodularity and nodularity of the interlobular septa and nodularity of the pleura
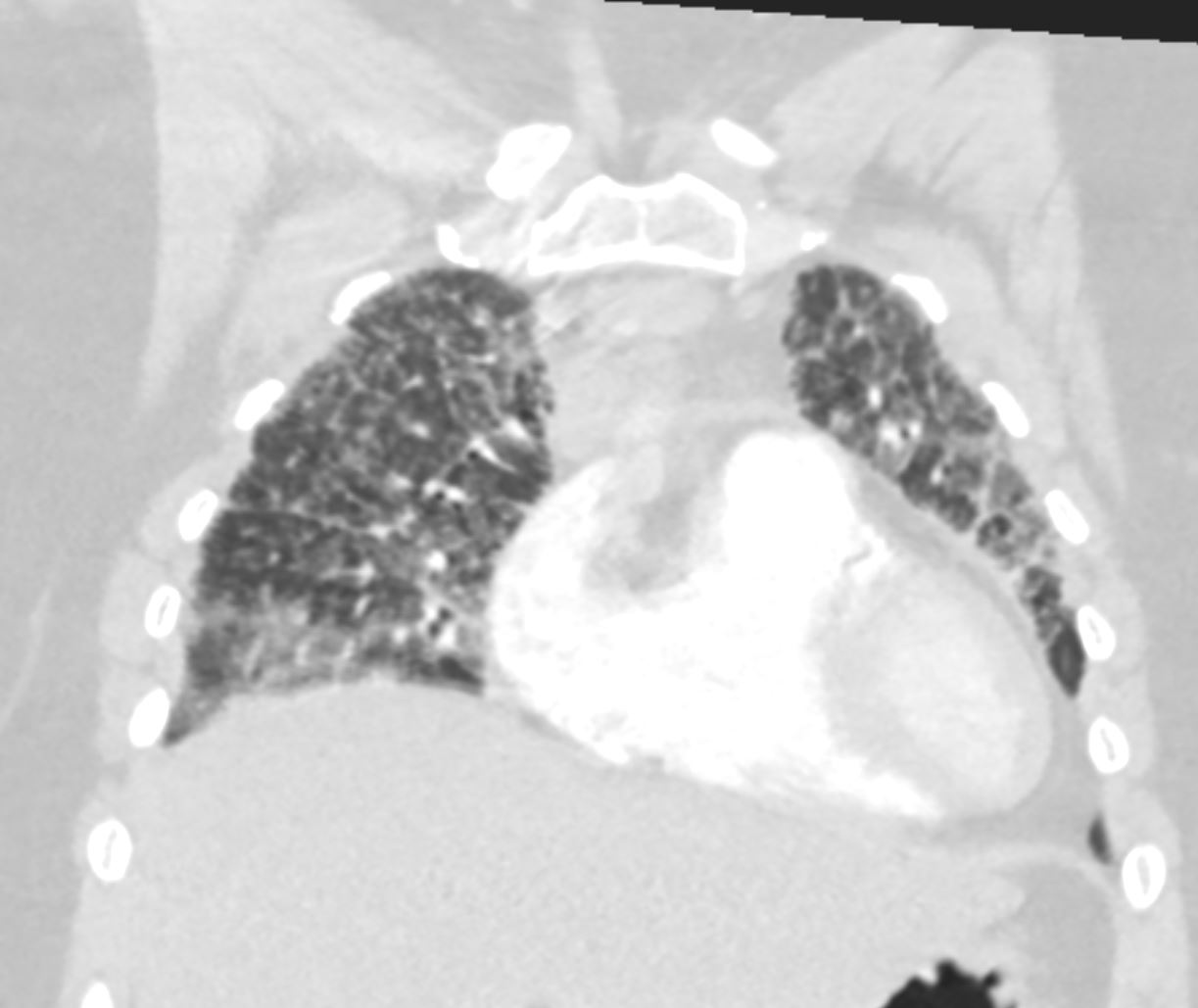
progressive extensive disease with ground glass changes and micronodularity and nodularity of the interlobular septa and nodularity of the pleura

progressive extensive disease with ground glass changes and micronodularity and nodularity of the interlobular septa and nodularity of the pleura
progressive extensive disease with ground glass changes and micronodularity and nodularity of the interlobular septa and nodularity of the pleura
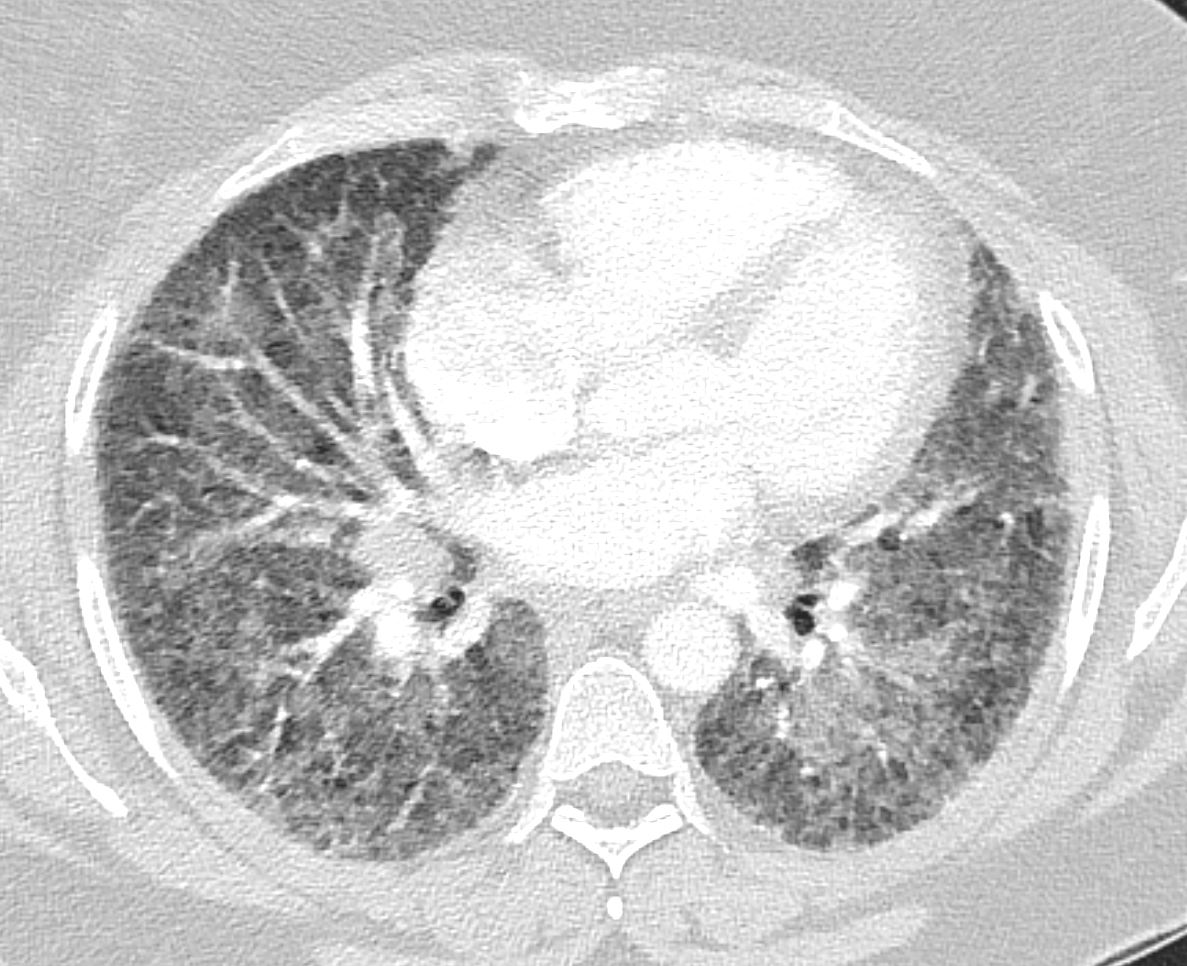
2months later
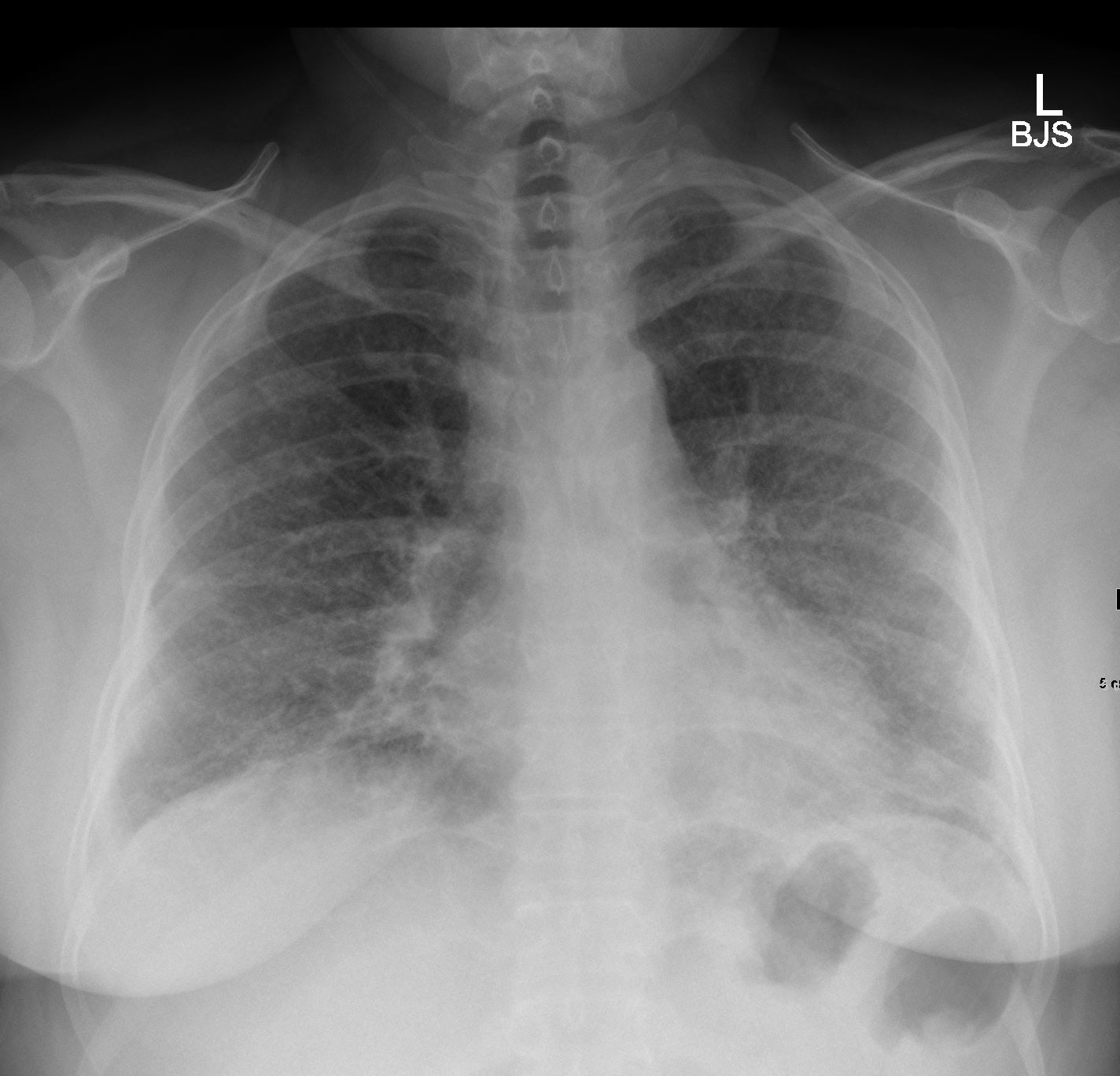
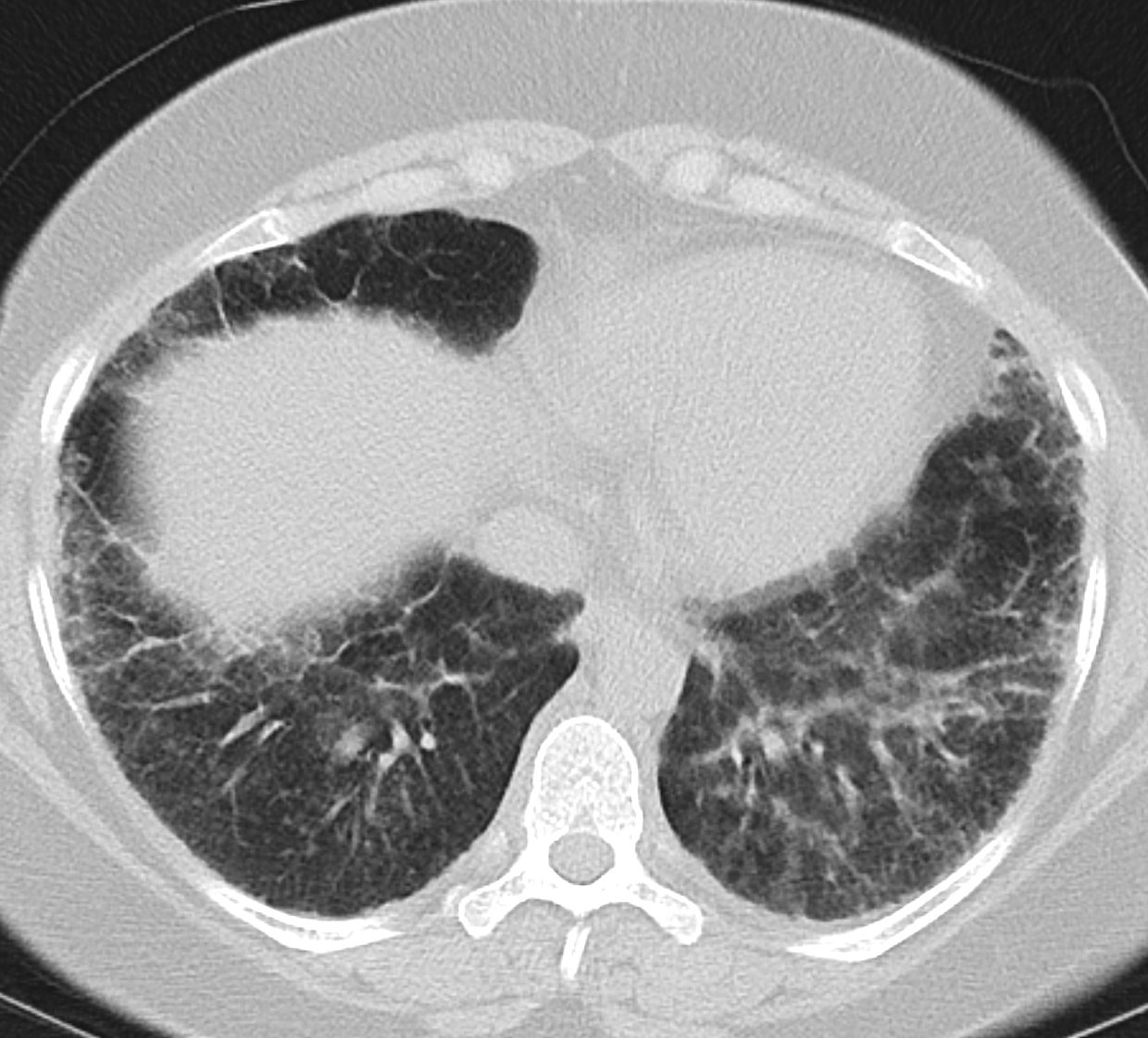
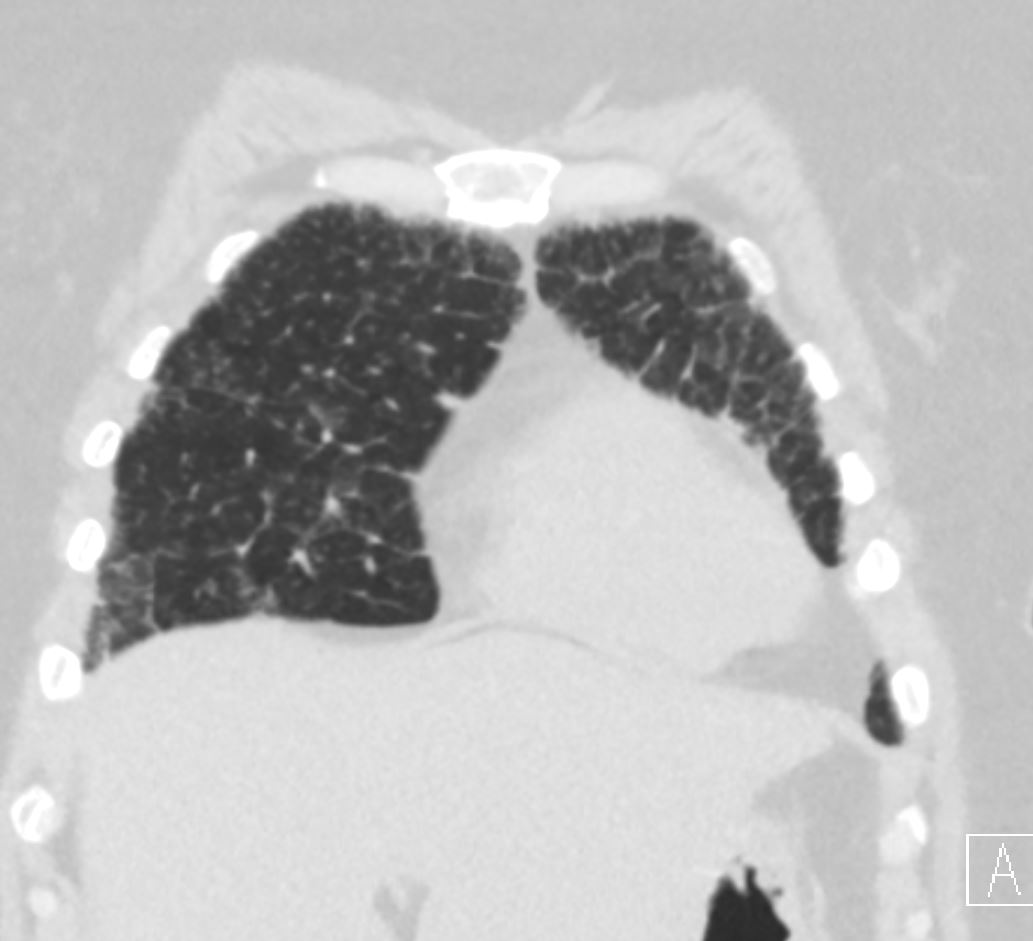
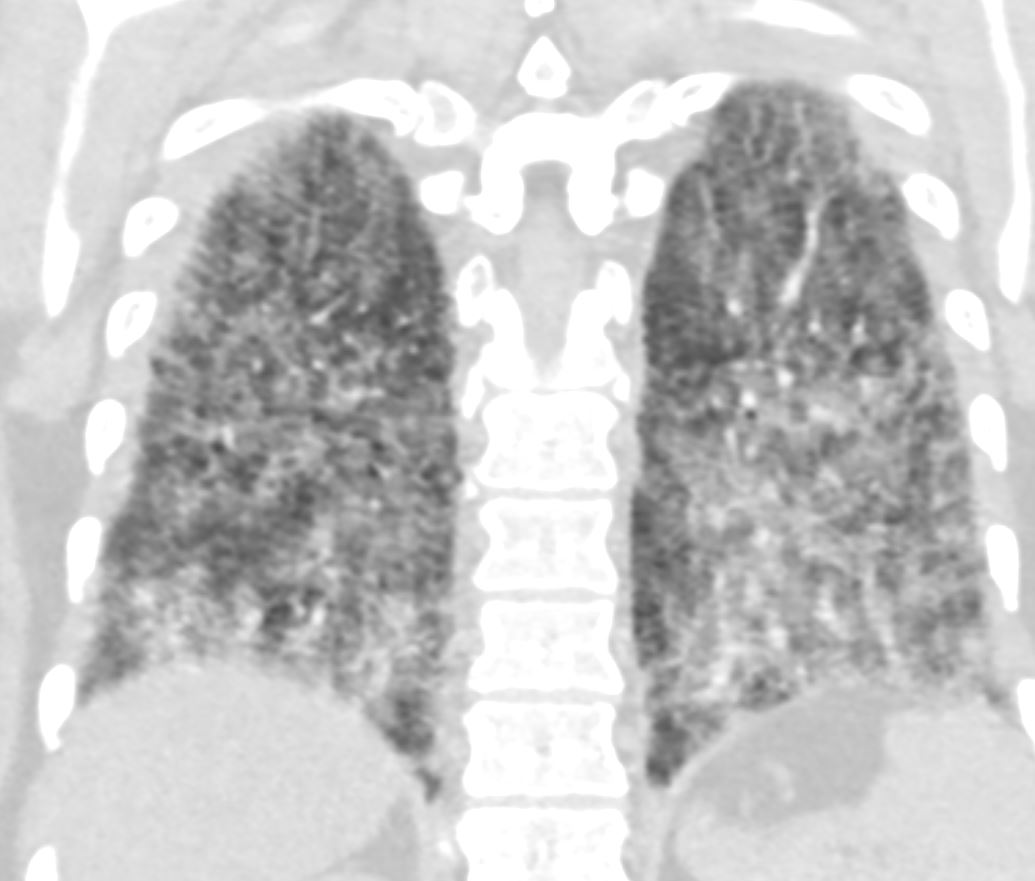
2 months later showing significant improvement
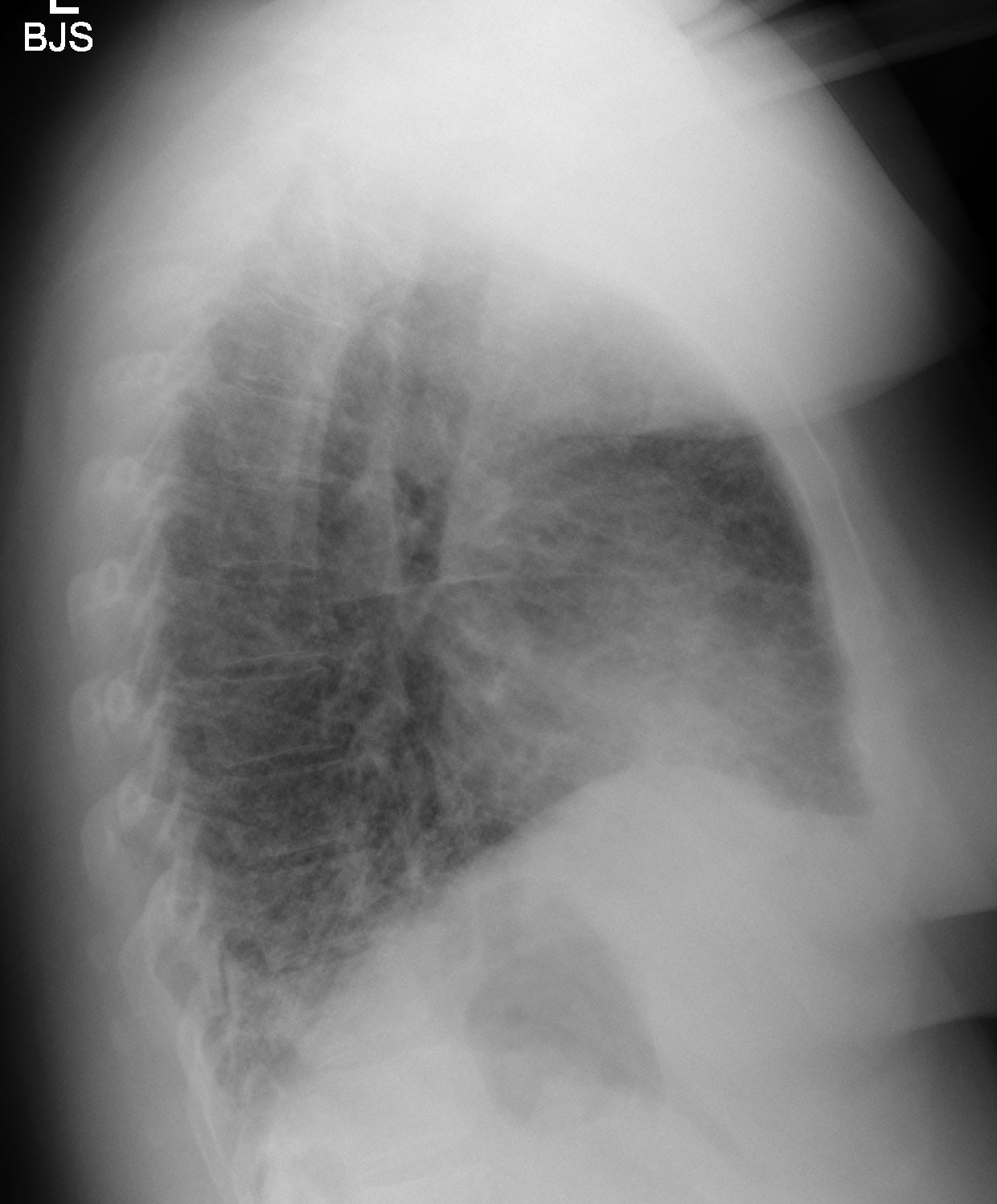
2 months later showing significant improvement
9 months later
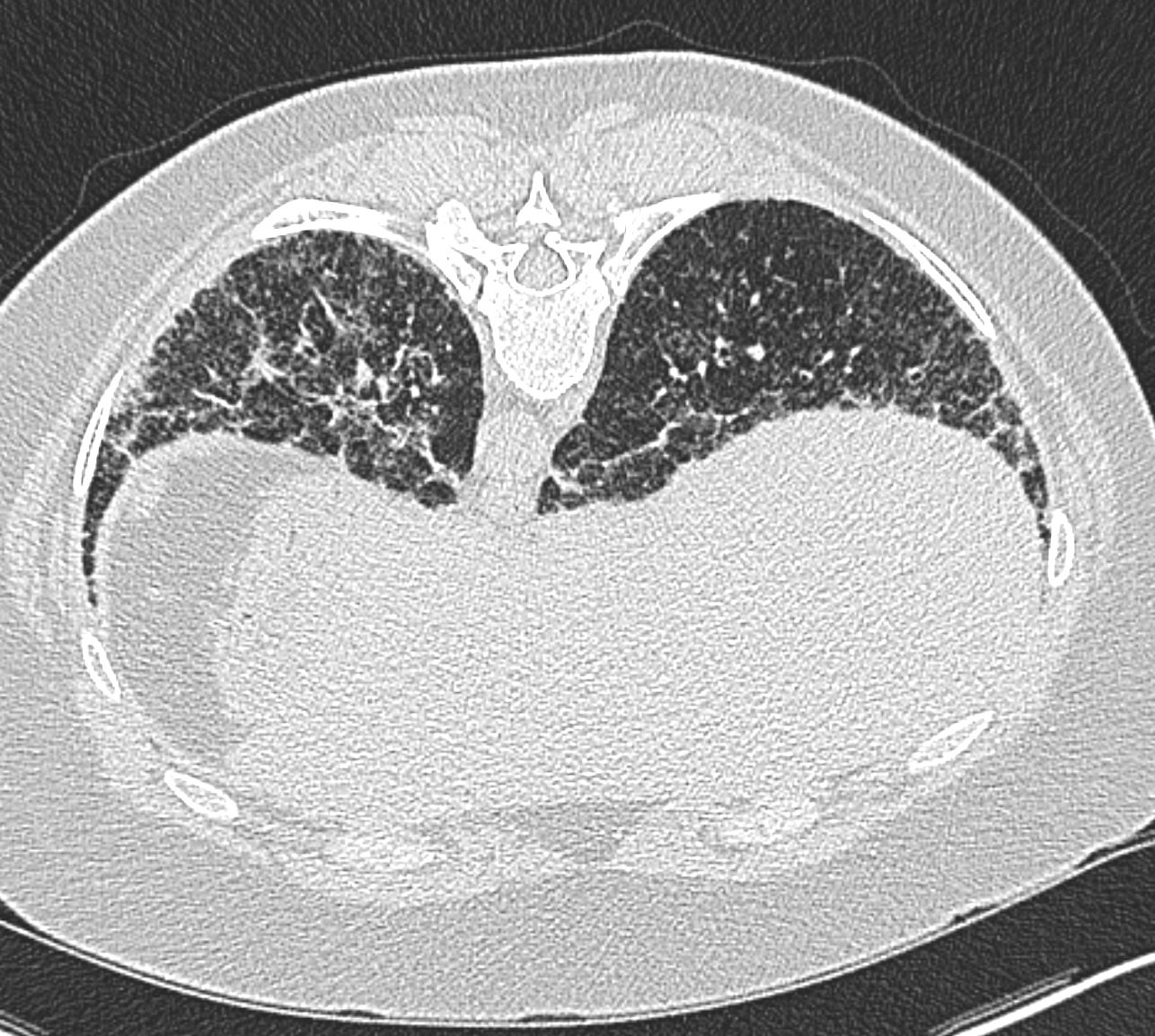
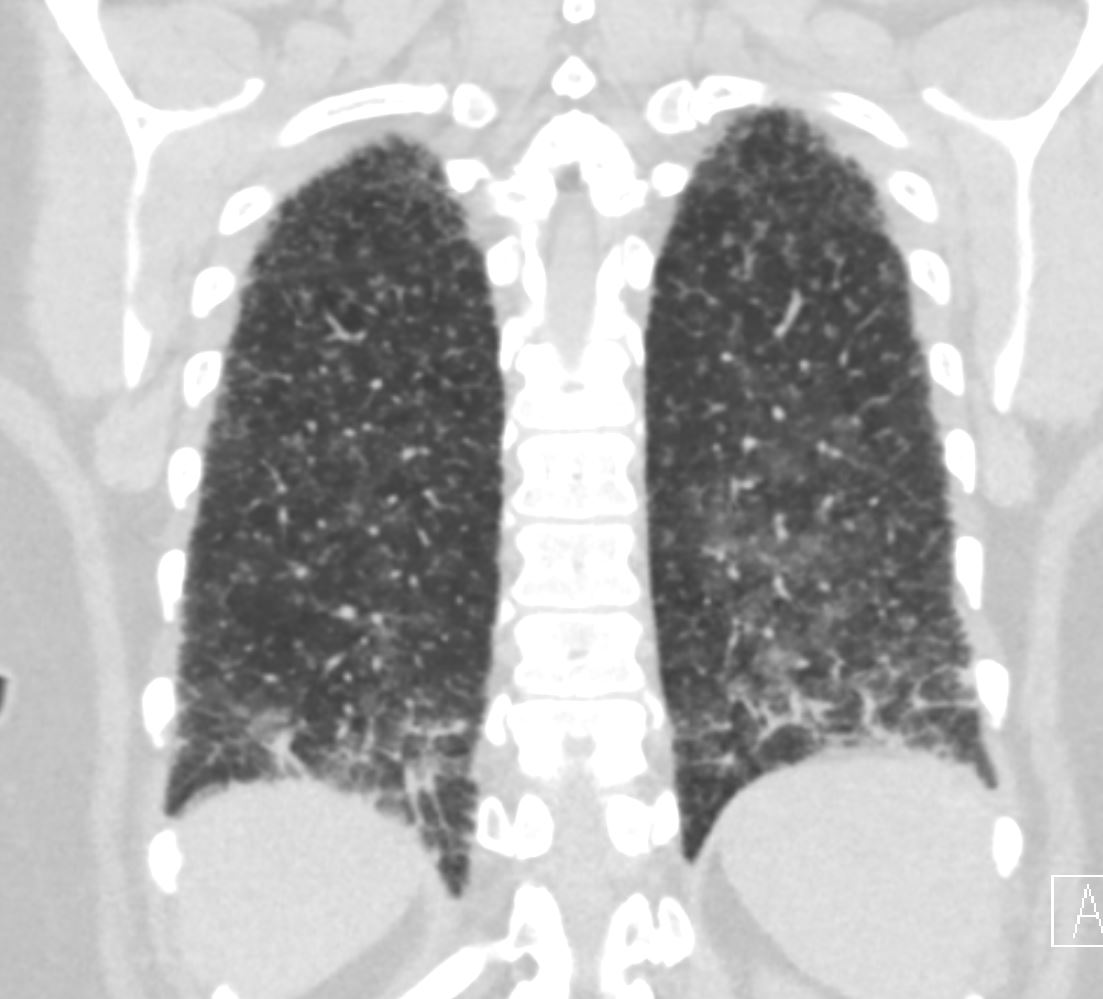
9 months later showing stability
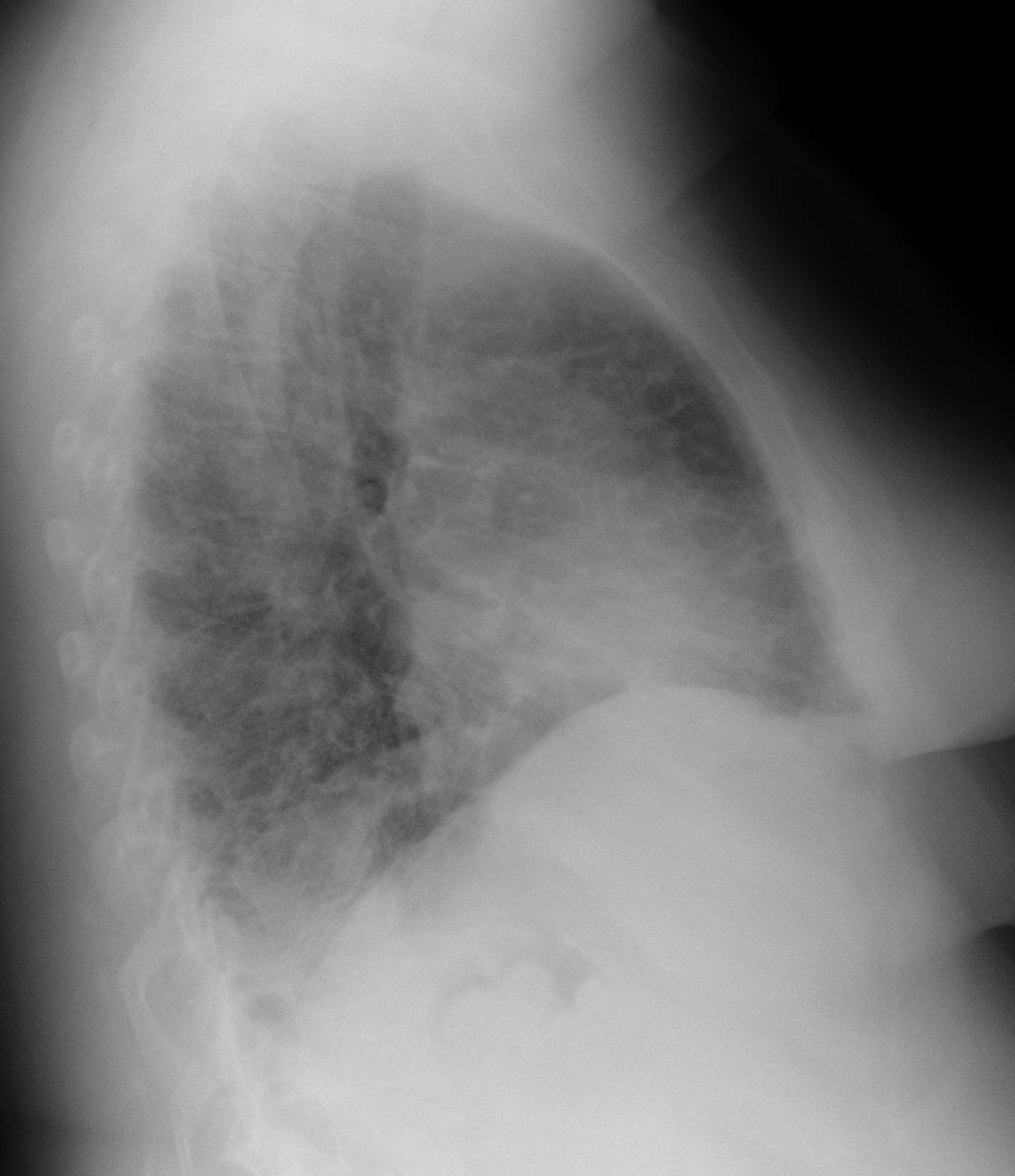
9 months later showing stability

