-
Etymology
- Derived from the word air, referring to gaseous content, and trapping, indicating the retention or inability to expel air.
AKA
- Air retention
- Trapped lung air
Definition
- What is it? Air trapping refers to the abnormal retention of air in the lungs or specific lung regions during expiration, often visible on imaging as areas of reduced lung density that do not empty fully.
- Caused by:
- Obstructive airway diseases such as asthma, chronic obstructive pulmonary disease (COPD), and bronchiolitis.
- Small airway obstruction from inflammation, fibrosis, or foreign bodies.
- Mechanical factors like airway collapse or external compression.
- Resulting in:
- Structural changes: Hyperinflated lung regions, mosaic attenuation on imaging, or lobar volume changes.
- Pathophysiology: Airflow obstruction prevents complete expiration, leading to localized or generalized air retention.
- Pathology: Hyperinflation and trapping of air in alveoli due to partial airway obstruction.
- Diagnosis:
- Clinical: Symptoms such as wheezing, dyspnea, or exercise intolerance, often varying by underlying condition.
- Radiology: Detected on expiratory CT as areas of low attenuation relative to normal lung parenchyma. May also appear as hyperlucent regions on chest X-ray.
- Labs: Generally non-specific but may include arterial blood gas abnormalities in severe cases.
- Treatment: Management focuses on addressing the underlying cause, such as bronchodilators for obstructive airway diseases, anti-inflammatory treatments, or removal of mechanical obstructions.
Radiology
- CXR
- Findings: Hyperlucent lung regions, flattened diaphragms, or increased retrosternal airspace in severe cases.
- Associated Findings: Hyperinflation or signs of associated airway disease (e.g., bronchial wall thickening).
- CT
- Parts: Segmental or lobar regions of reduced attenuation, often seen during expiratory imaging.
- Size: Variable, from small localized areas to extensive lobar or whole-lung involvement.
- Shape: Irregular or lobular regions of low attenuation.
- Position: Often distributed in dependent lung regions but varies by disease.
- Character: Persistent low attenuation on expiratory CT compared to inspiratory scans.
- Time: Chronic in obstructive diseases, transient in reversible conditions.
- Associated Findings: Mosaic attenuation, bronchial wall thickening, or evidence of airway narrowing.
- Other Imaging Modalities
- MRI may demonstrate areas of low signal intensity corresponding to trapped air but is less commonly used.
- Ventilation-perfusion (V/Q) scans may show perfusion defects without corresponding ventilation abnormalities.
-
Pulmonary function tests (PFTs) in air trapping often demonstrate an obstructive pattern, with decreased FEV1, a reduced FEV1/FVC ratio, and elevated residual volume (RV) or total lung capacity (TLC).
Key Points and Pearls
- Air trapping is a hallmark of obstructive airway diseases and is best assessed on expiratory CT.
- Mosaic attenuation on imaging may help distinguish air trapping from vascular causes of hypoperfusion.
- The extent and distribution of air trapping can guide diagnosis and management of underlying conditions.
- Early recognition of small airway disease through imaging can prevent progression to advanced obstructive lung diseases.
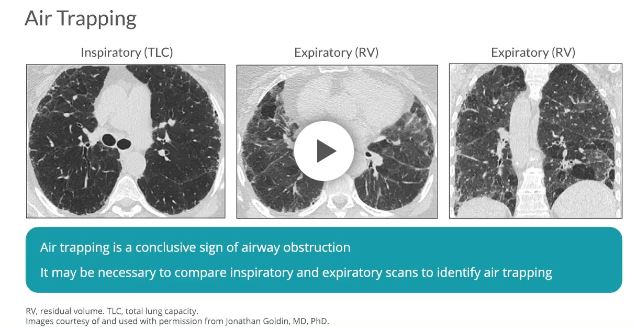
Air Trapping
Artistically rendered depiction of air trapping in the upper lung fields characteristic of emphysema
Ashley Davidoff MD art TheCommonVein.net
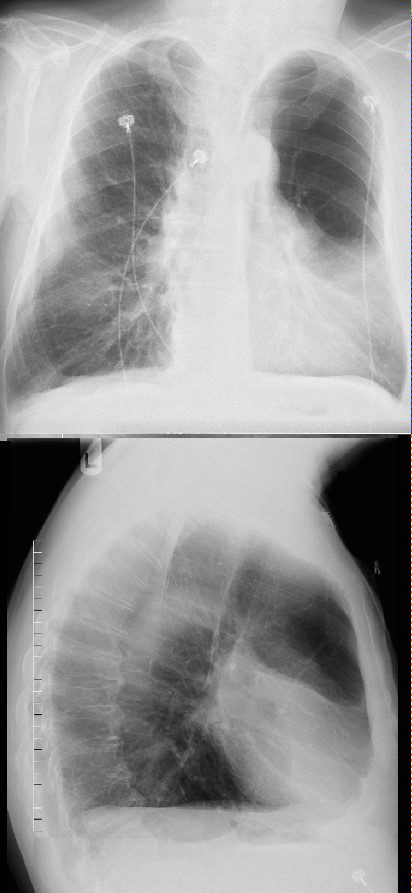
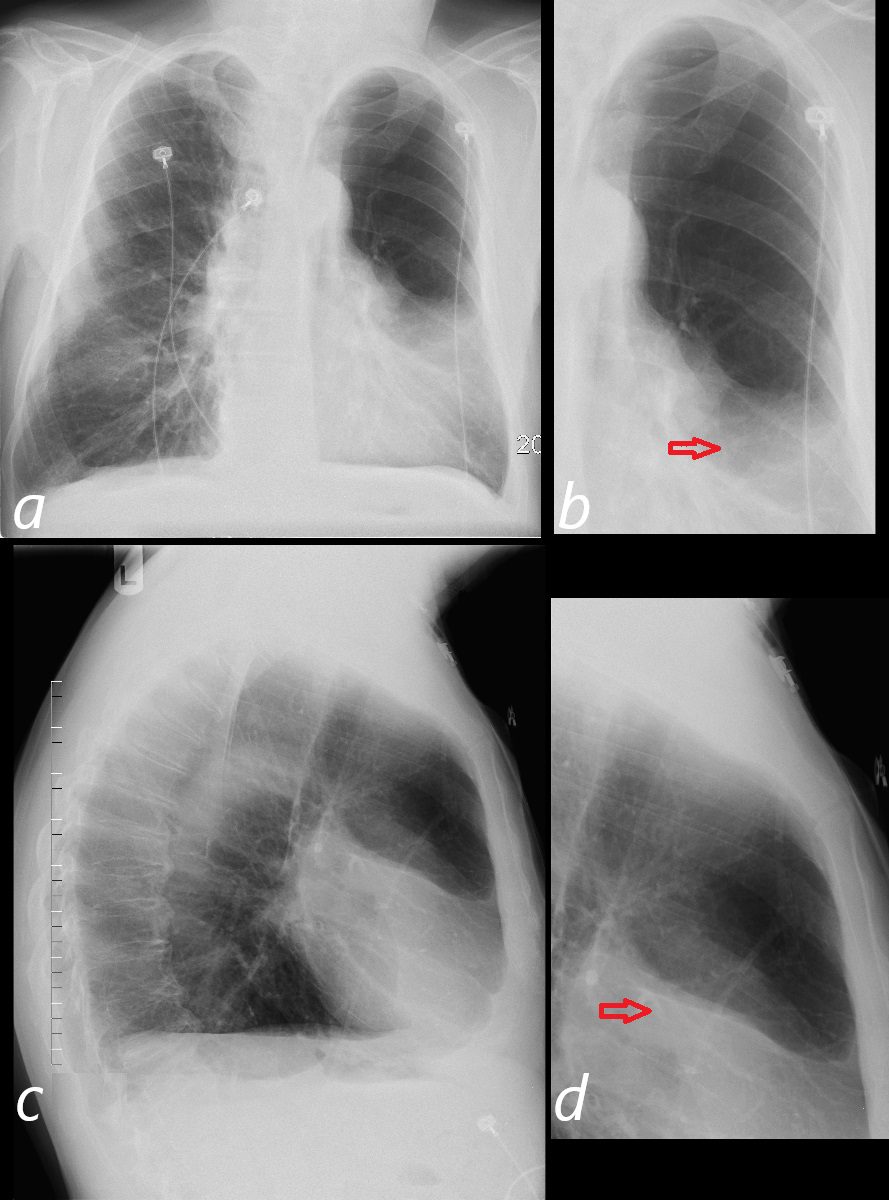
CXR Air Trapping Superior Segment LLL and
Small Subsegment in the RLL above the Diaphragm
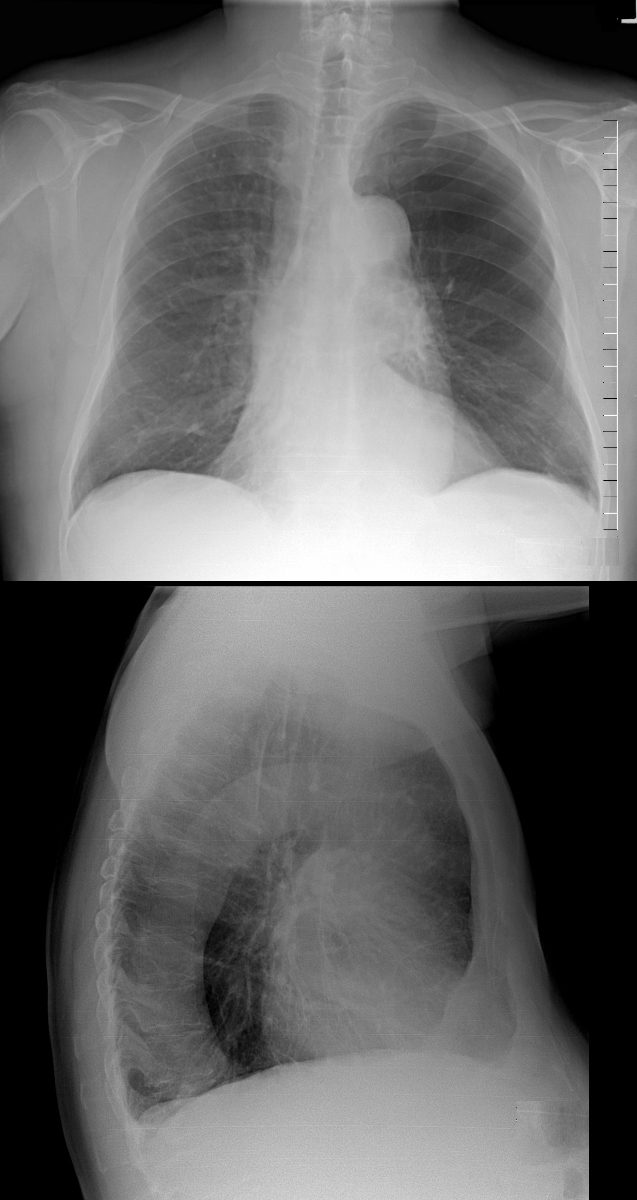
Swyer James Syndrome
55 year-old male with a history of childhood infection presents with dyspnea
On the frontal view, there is an area of lucency in the mid to left upper lung field with additional paucity of blood vessels in the region. There is a smaller region of hyperlucency above the right hemidiaphragm. The lateral examination suggests the lucency is located posteriorly in the superior segment of the left lower lobe. These findings likely reflect manifestation of Swyer James syndrome with segmental involvement
Ashley Davidoff MD TheCommonVein.net 47050c
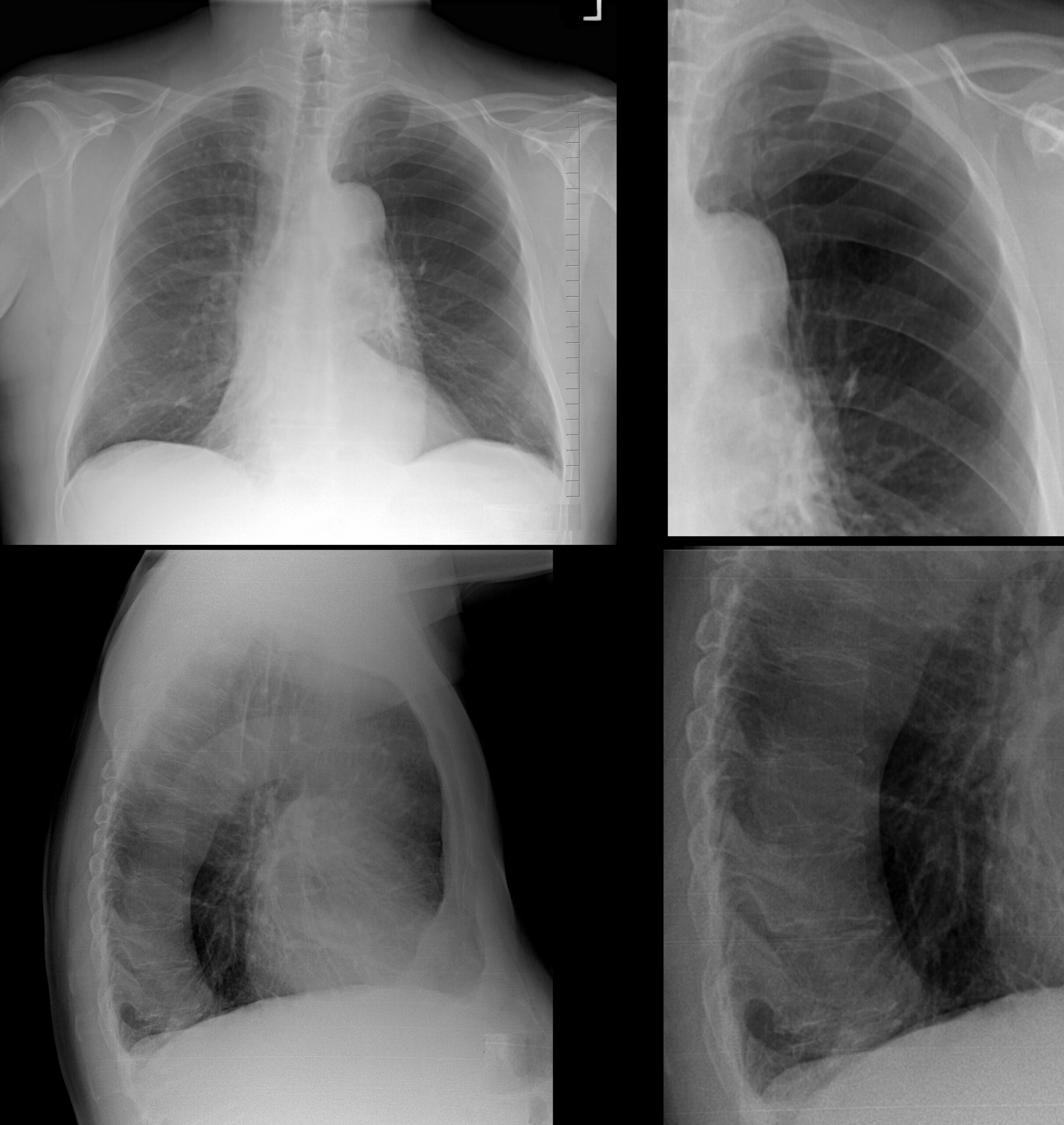
Swyer James Syndrome
55 year-old male with a history of childhood infection presents with dyspnea
On the frontal viewt there is an area of lucency in the mid to left upper lung field with additional paucity of blood vessels in the region. The lateral examination suggests the lacency is located posteriorly in the superior segment of the left lower lobe. These findings likely reflect manifestation of Swyer James syndrome with segmental involvement
Ashley Davidoff MD TheCommonVein.net 47050cL
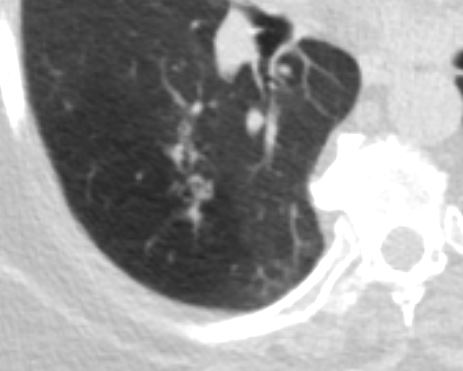
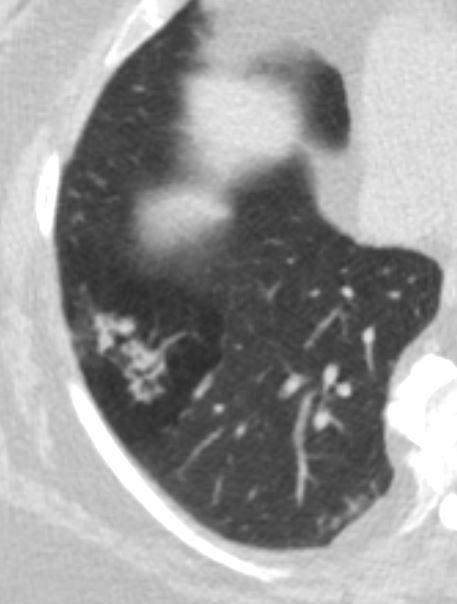
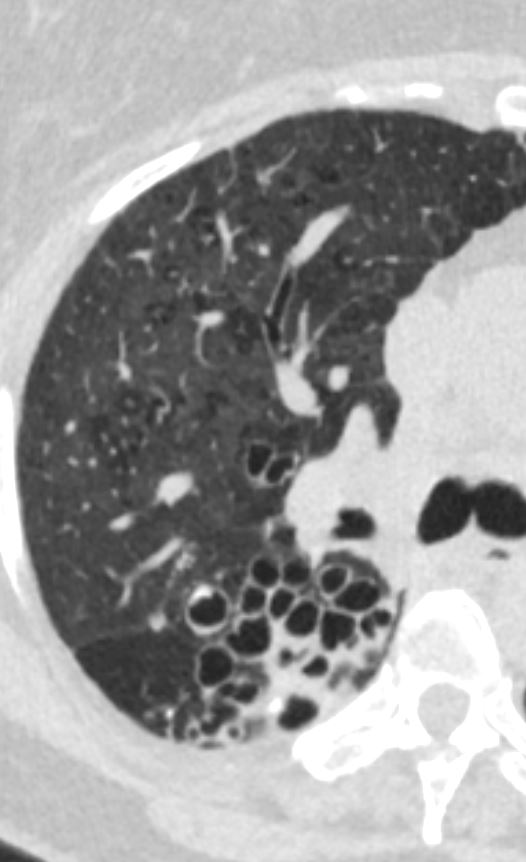
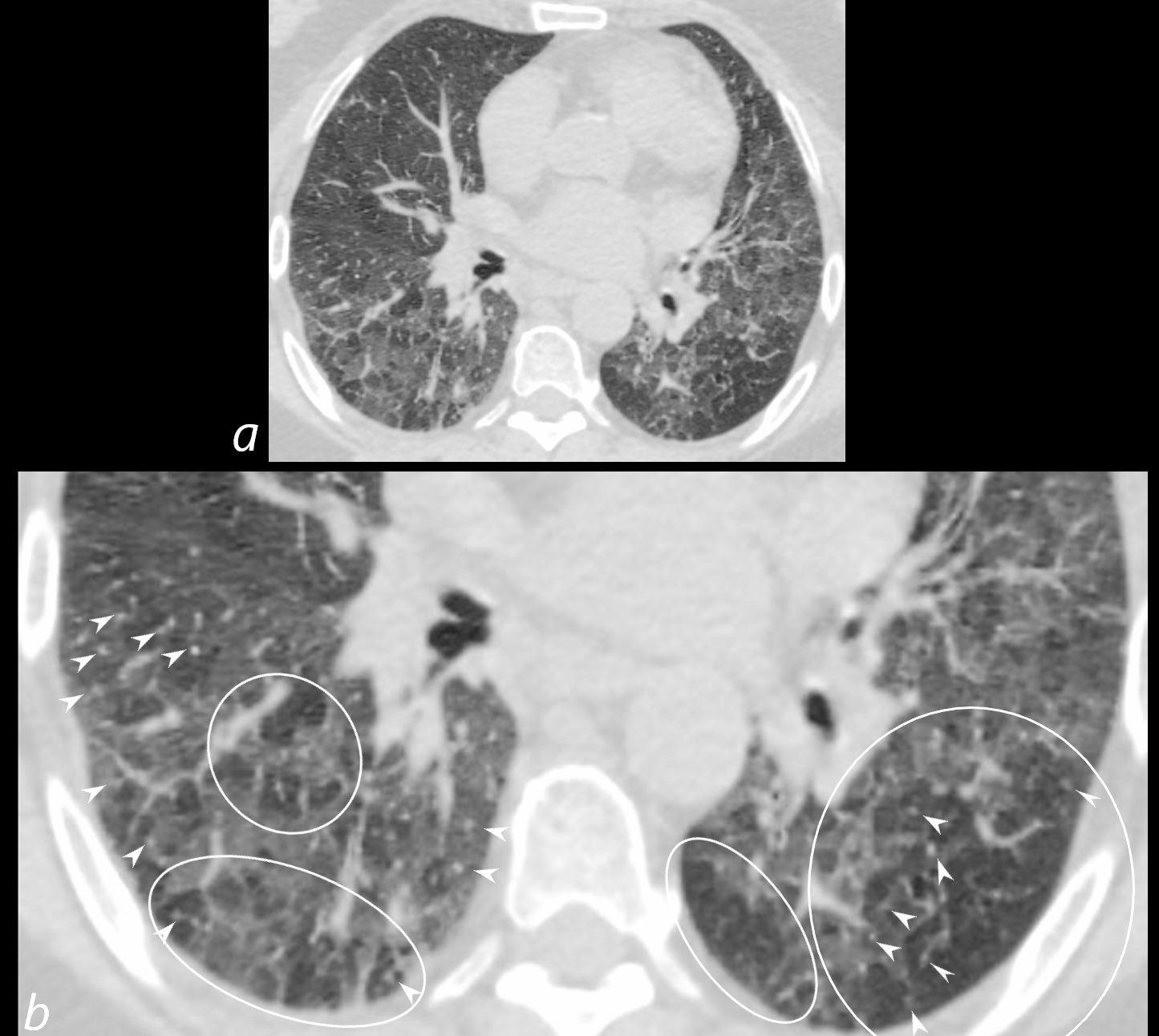
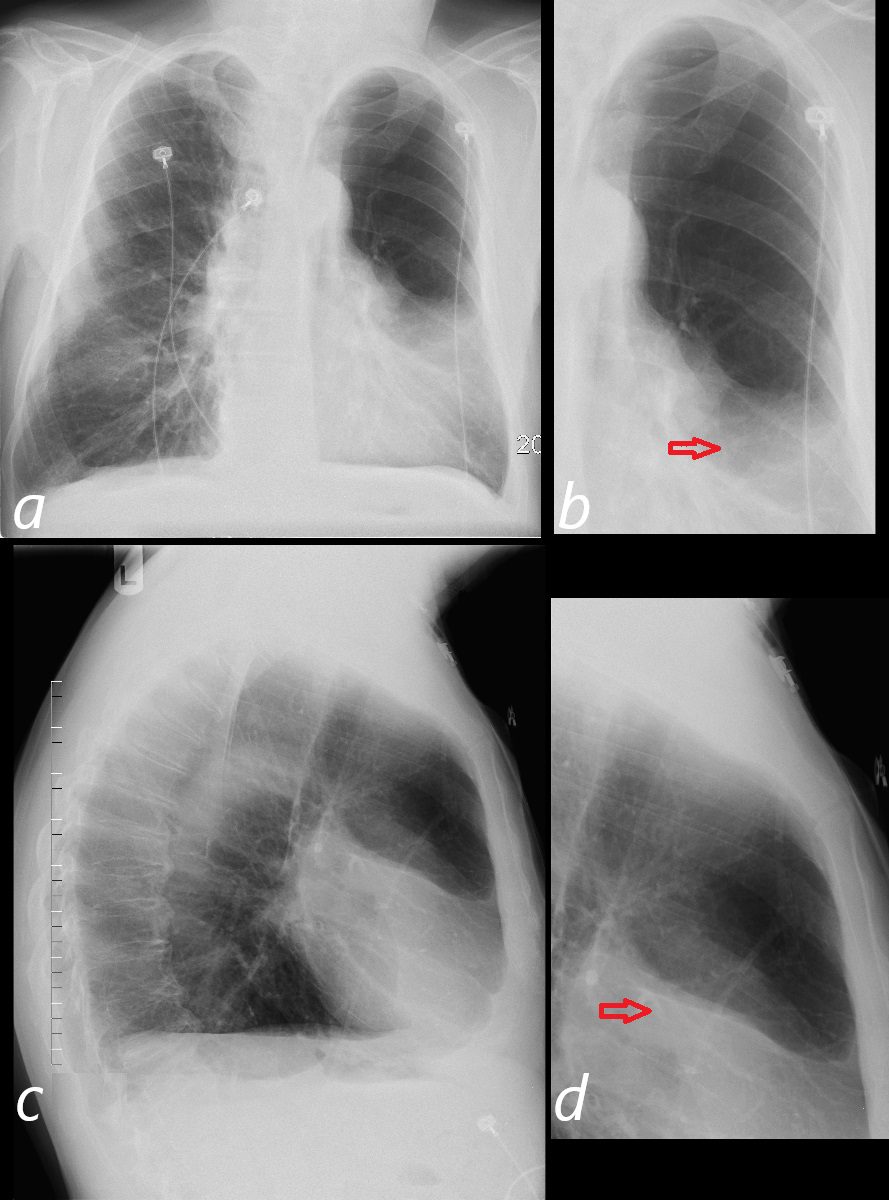
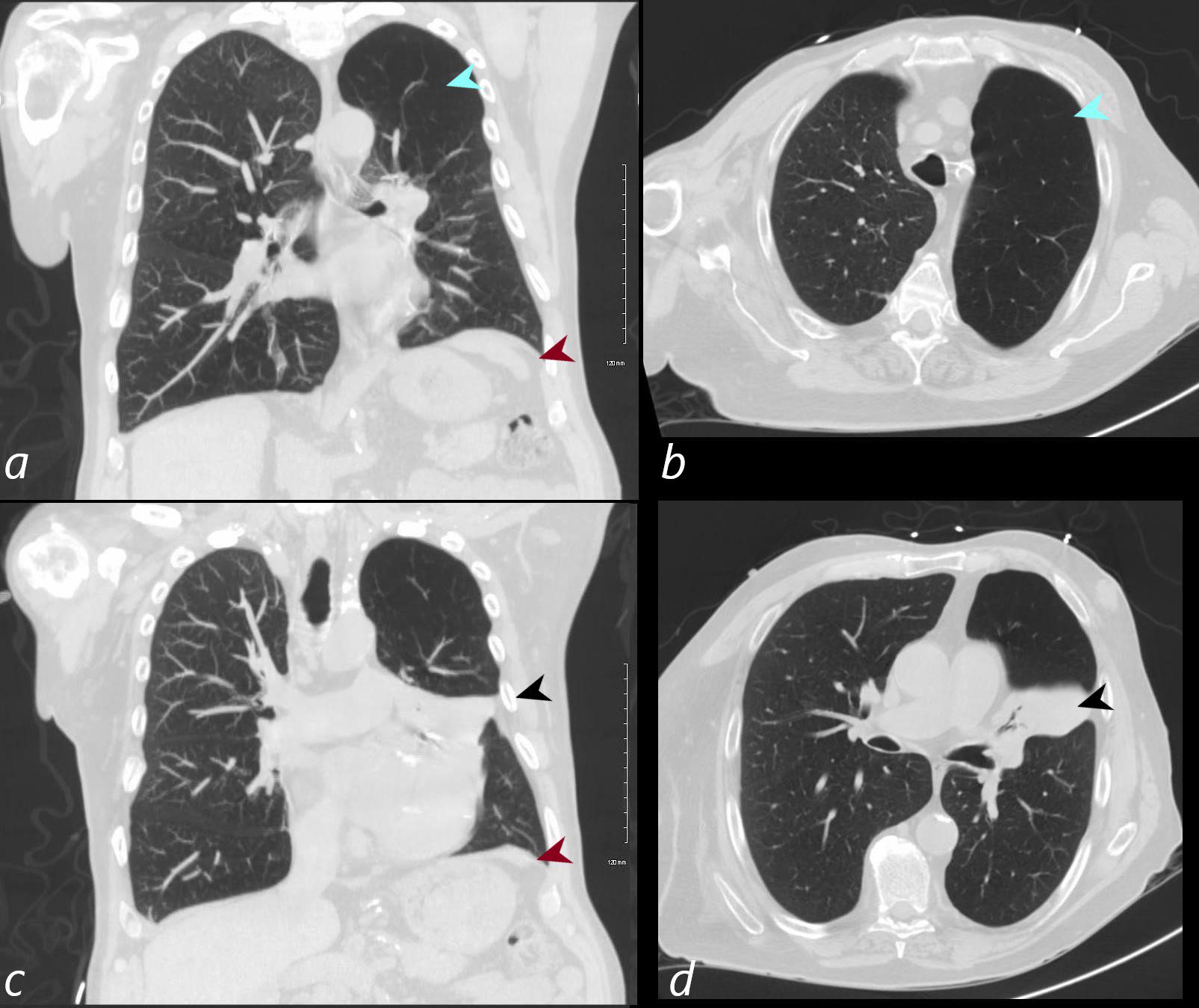
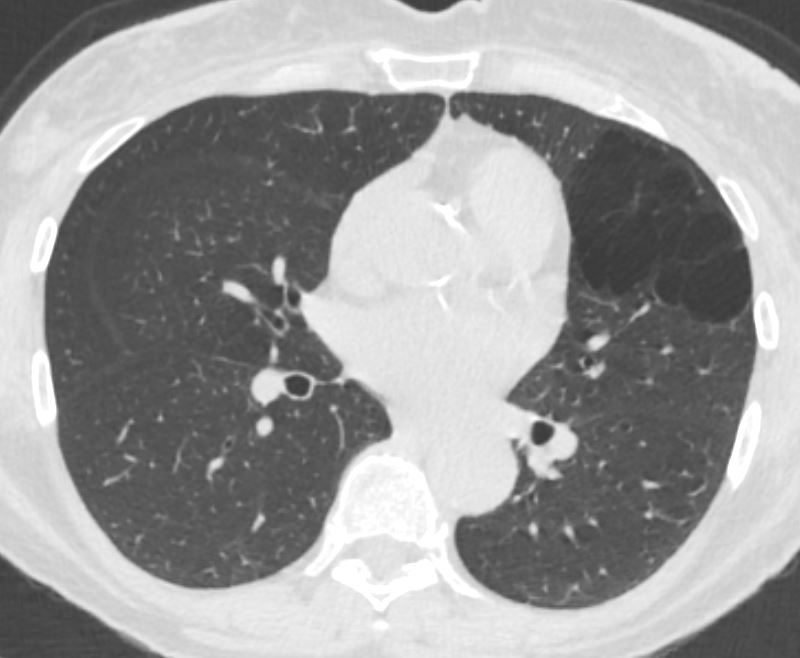
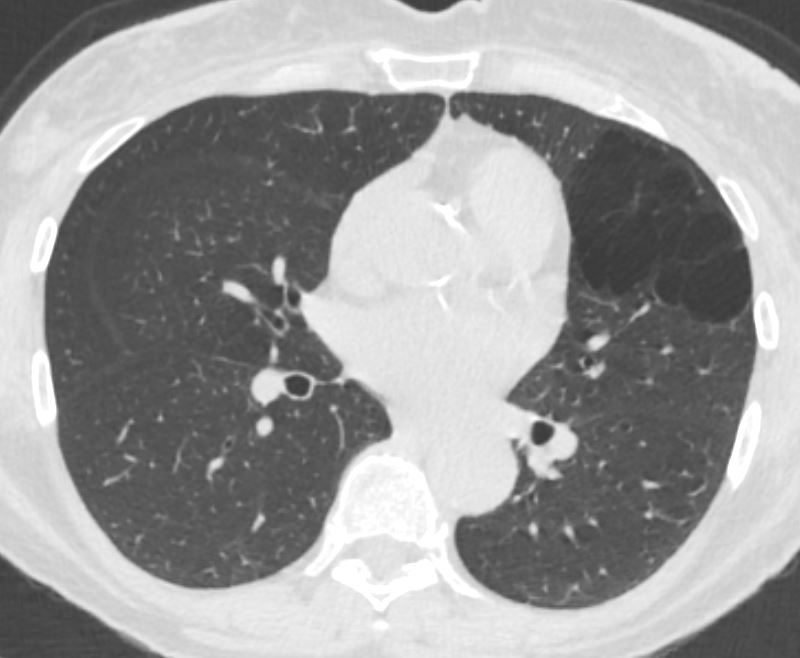
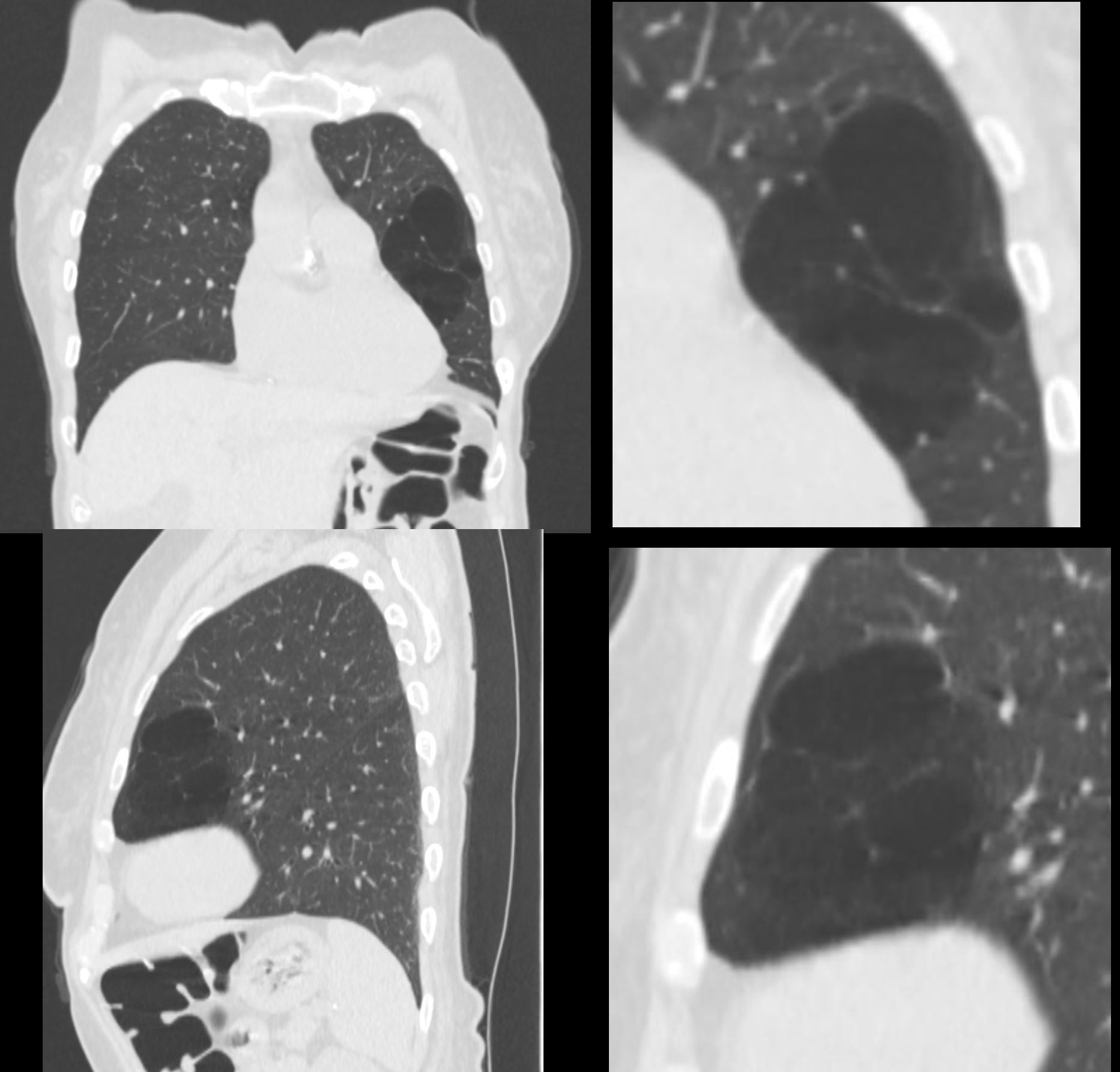
CT Air Trapping Superior Segment LLL and
Small Post Segment in the RLL above the Diaphragm
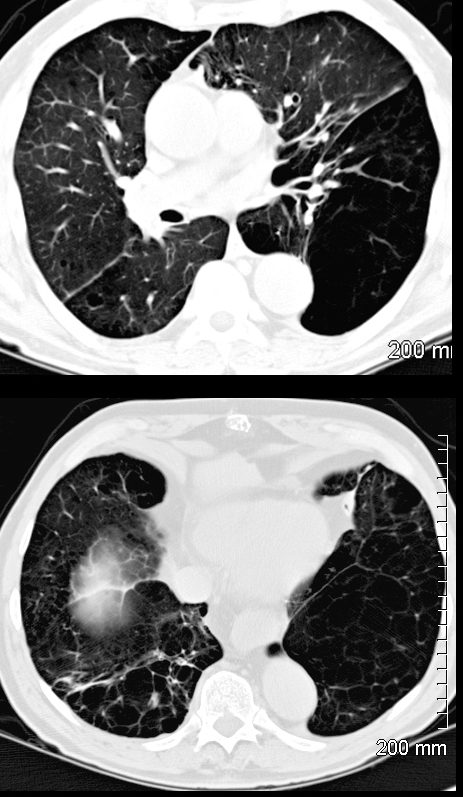
55 year-old male lucent and expanded superior segment of the left lower lobe with paucity of blood vessels in the region (top image) . There is a smaller region of hyperlucency in the posterior segment of the right lower lobe. in the . These findings in the context of childhood infection likely reflect a manifestation of Swyer James syndrome with segmental involvement and subsegmental involvement
Ashley Davidoff MD TheCommonVein.net 47055c
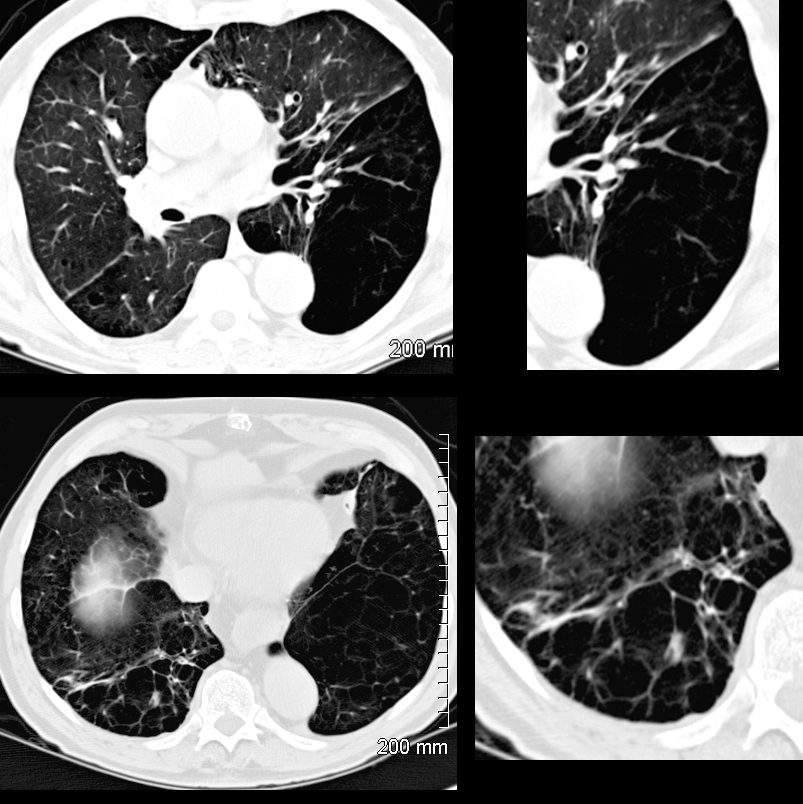
55 year-old male lucent and expanded superior segment of the left lower lobe with paucity of blood vessels in the region (top image) . There is a smaller region of hyperlucency in the posterior segment of the right lower lobe. in the . These findings in the context of childhood infection likely reflect a manifestation of Swyer James syndrome with segmental involvement and subsegmental involvement
Ashley Davidoff MD TheCommonVein.net 47050cL
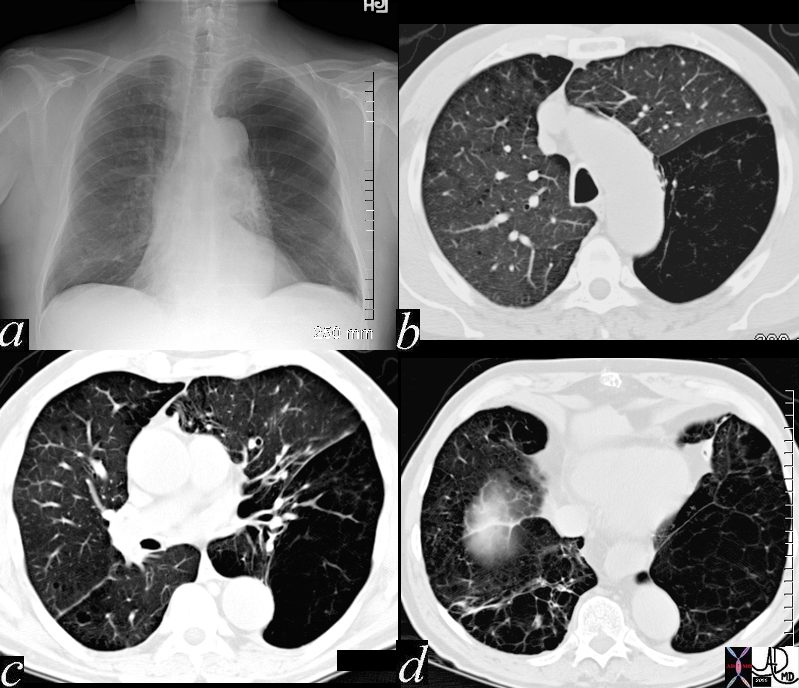
Frontal CXR of a 55 year-old male (a) shows a hyperlucent left upper to mid lung field . CT in the axial projections (b,c,d) show an expanded superior segment of the left lower lobe with paucity of blood vessels in the region ) . There is a smaller region of hyperlucency in the posterior segment of the right lower lobe (d). These findings in the context of childhood infection likely reflect a manifestation of Swyer James syndrome with segmental and subsegmental involvement
Ashley Davidoff MD TheCommonVein.net 47050cL
The pathogenesis involves airway obstruction or collapse during expiration, preventing air from escaping the affected parts of the lungs, resulting in hyperinflation and difficulty with ventilation. Over time, this can impair lung function, leading to symptoms such as shortness of breath, wheezing, and reduced exercise tolerance. Air trapping is typically diagnosed through imaging, where it appears as areas of hyperlucency on a chest X-ray or CT scan, particularly in expiratory views. Pulmonary function tests (PFTs) may also show a decreased expiratory flow rate, further confirming the presence of obstructive processes.
Small Airway Obstruction
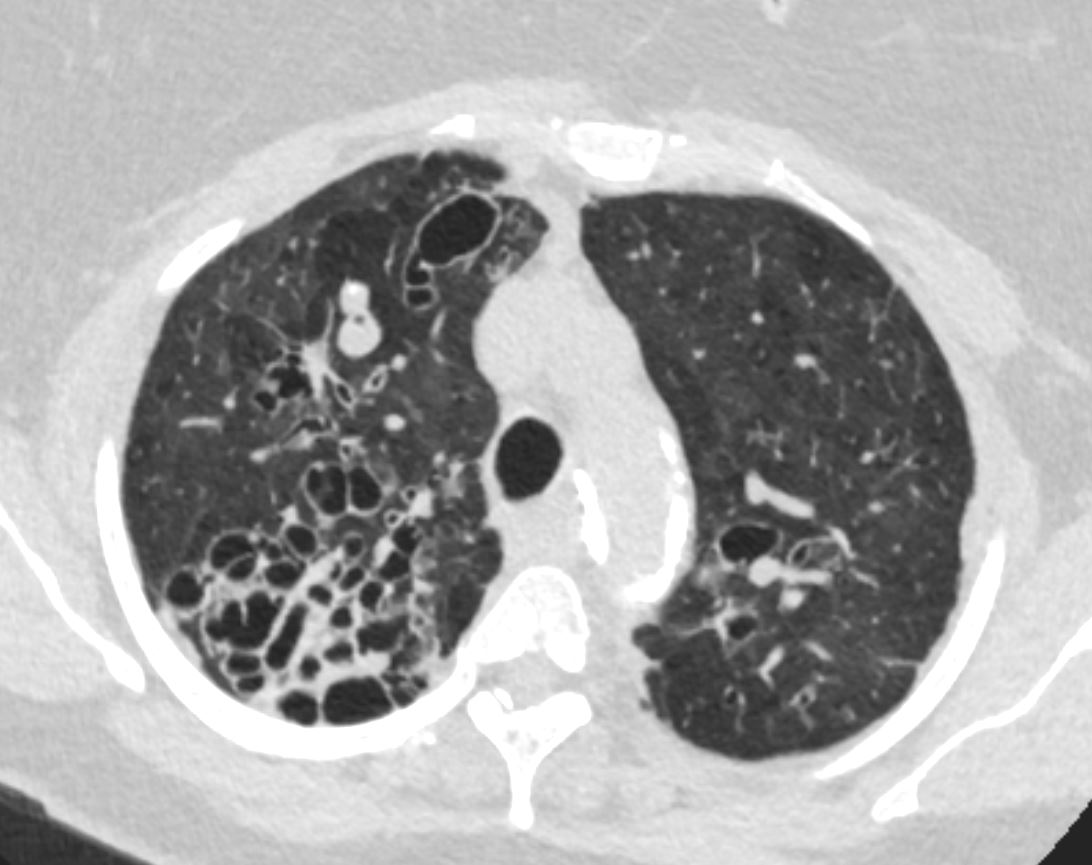
Bronchiolitis and Mosaic Attenuation

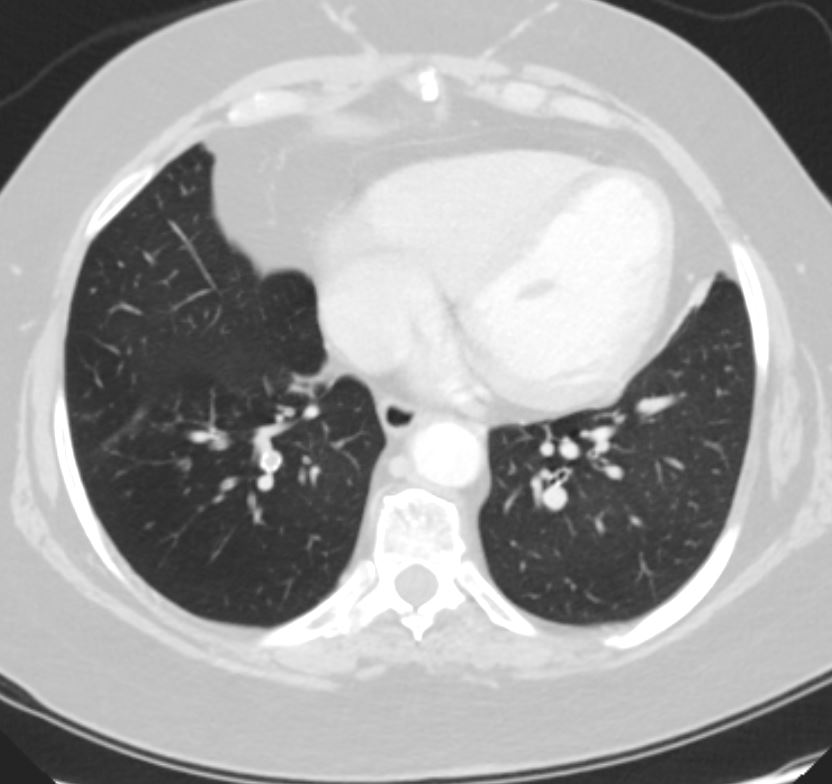
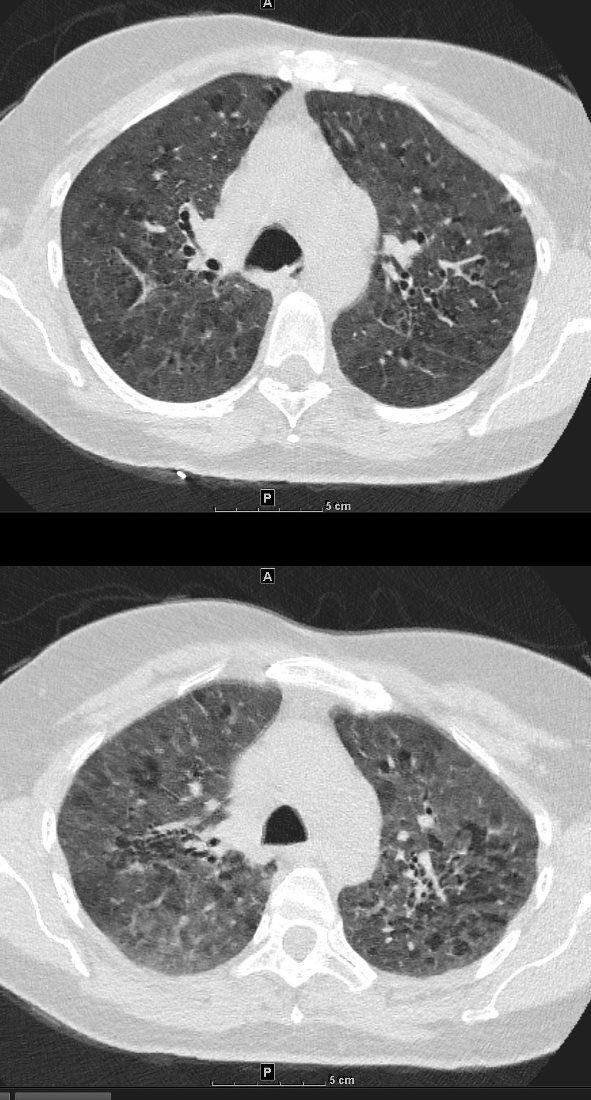
70-year-old female former smoker with long standing history of RA presents with chronic dyspnea.
Axial CT of the chest at the level of the carina reveals centrilobular nodules, ground-glass opacities, and mosaic attenuation (likely due to air trapping in this context) and bronchial wall thickening . In the context of a patient with rheumatoid arthritis a diagnosis of follicular bronchiolitis is likely. However radiologically fibrotic hypersensitivity pneumonitis (HP) is included in the differential diagnosis
Ashley Davidoff MD TheCommonVein.net 132Lu 136654
70-year-old female former smoker with long standing history of RA presents with chronic dyspnea.
Axial CT of the chest at the level of the lower lung fields reveals centrilobular nodules (b white arrowheads), ground-glass opacities, and mosaic attenuation (b, white rings) likely due to air trapping in this context.
In the context of a patient with rheumatoid arthritis a diagnosis of follicular bronchiolitis is likely. However radiologically fibrotic hypersensitivity pneumonitis (HP) is included in the differential diagnosis
Ashley Davidoff MD TheCommonVein.net 132Lu 136657cL
Hypersensitivity Pneumonitis
Mosaic Attenuation with Persistence on Expiration = Air Trapping
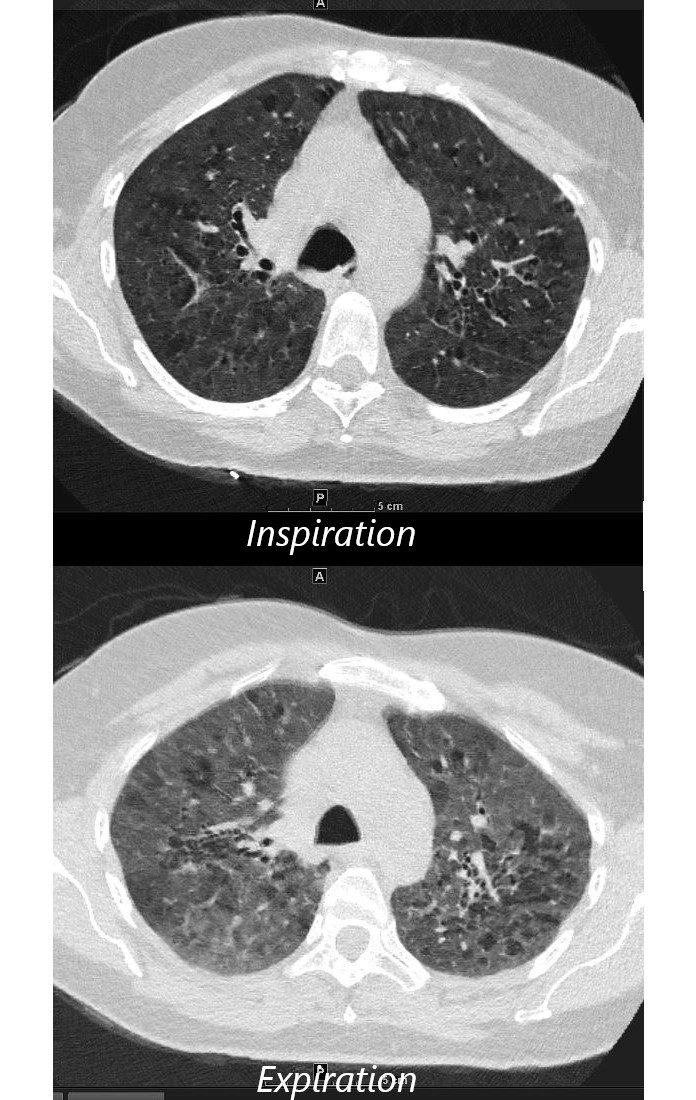
55-year-old female with shortness of breath. She keeps birds for pets Axial CT through the mid lung fields on inspiration, shows diffuse ground glass changes with a combination of mosaic attenuation and normal lung giving the appearance of the head cheese sign.
On the expiration phase the mosaic attenuation remains indicating air trapping and inferring small airway disease
Ashley Davidoff MD TheCommonVein.net 242Lu 13551aL
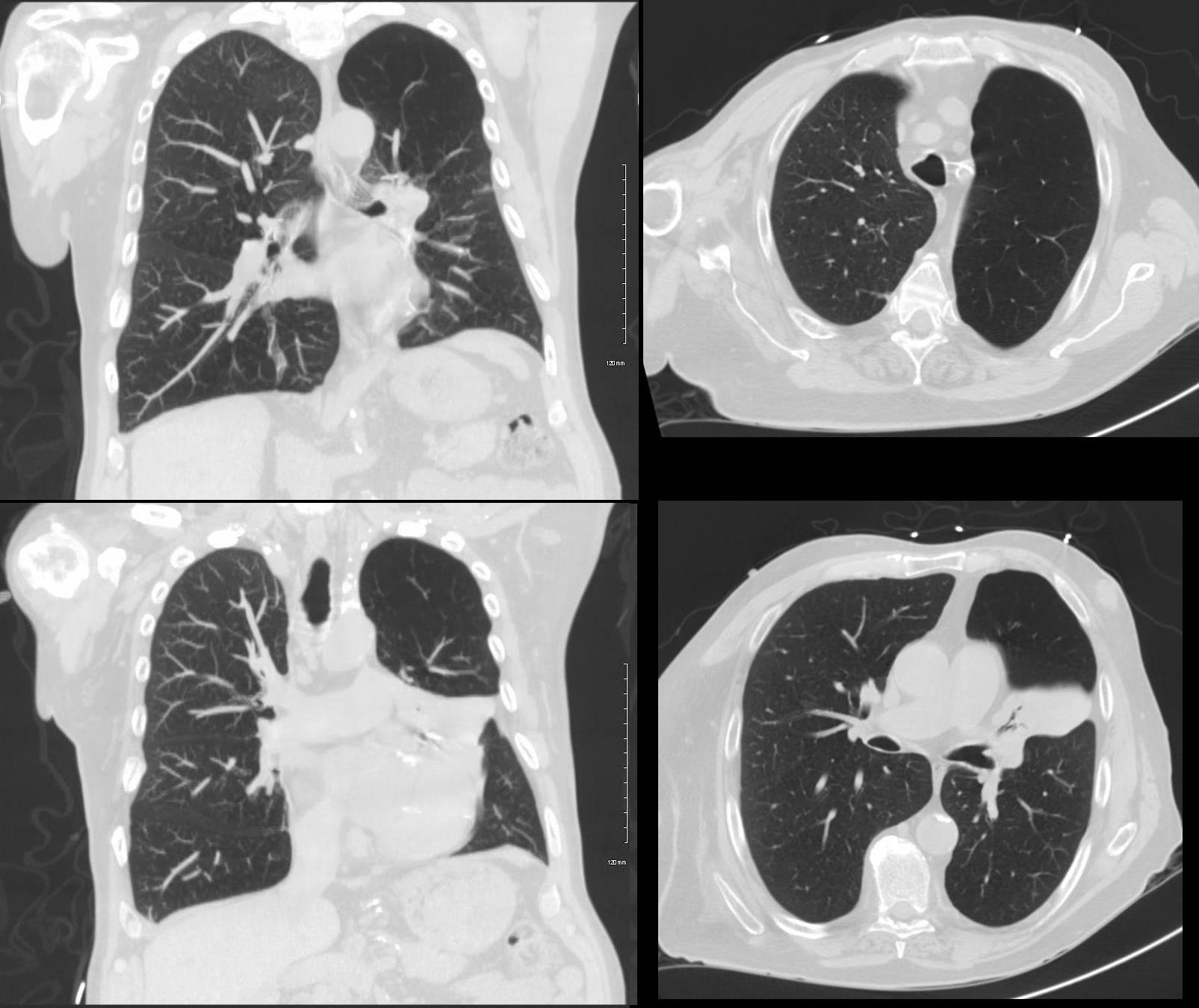
CXR Air Trapping LUL and
Compressive Atelectasis of the Lingula
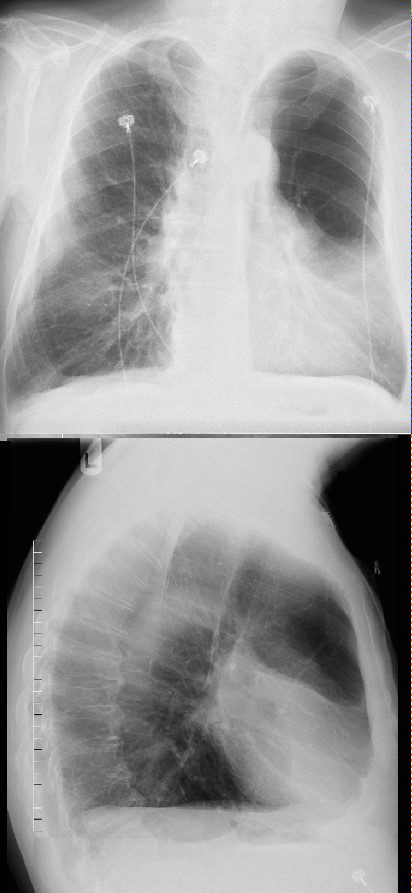
58 year old male presents with dyspnea.
Frontal CXR reveals a lucent left upper lung field with a midlung opacity
The lateral exam shows an opacity in the region of the ligula
There is mild elevation of the left hemidiaphragm
Finding are consistent with air trapping in a patient with Swyer James Syndrome. there is secondary compression of the superior lingula segment secondary to the air trapping and hyperinflated LUL
Ashley Davidoff MD TheCommonVein.net
118064c
58 year old male presents with dyspnea.
Frontal CXR reveals a lucent left upper lung field with a midlung opacity
The lateral exam shows an opacity in the region of the ligula
There is mild elevation of the left hemidiaphragm
Finding are consistent with air trapping in a patient with Swyer James Syndrome. there is secondary compression of the superior lingula segment secondary to the air trapping and hyperinflated LUL
Ashley Davidoff MD TheCommonVein.net
118064cL01
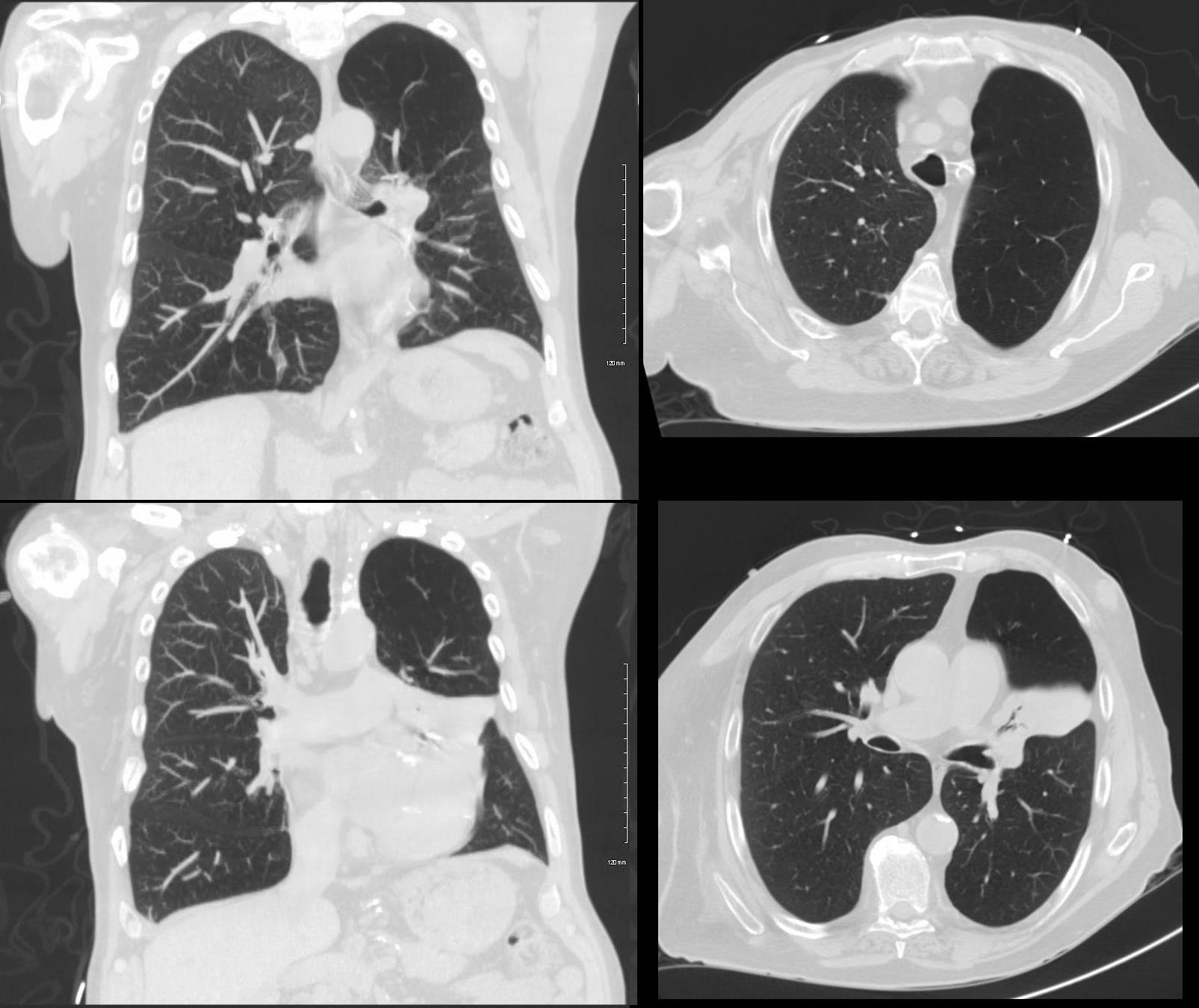
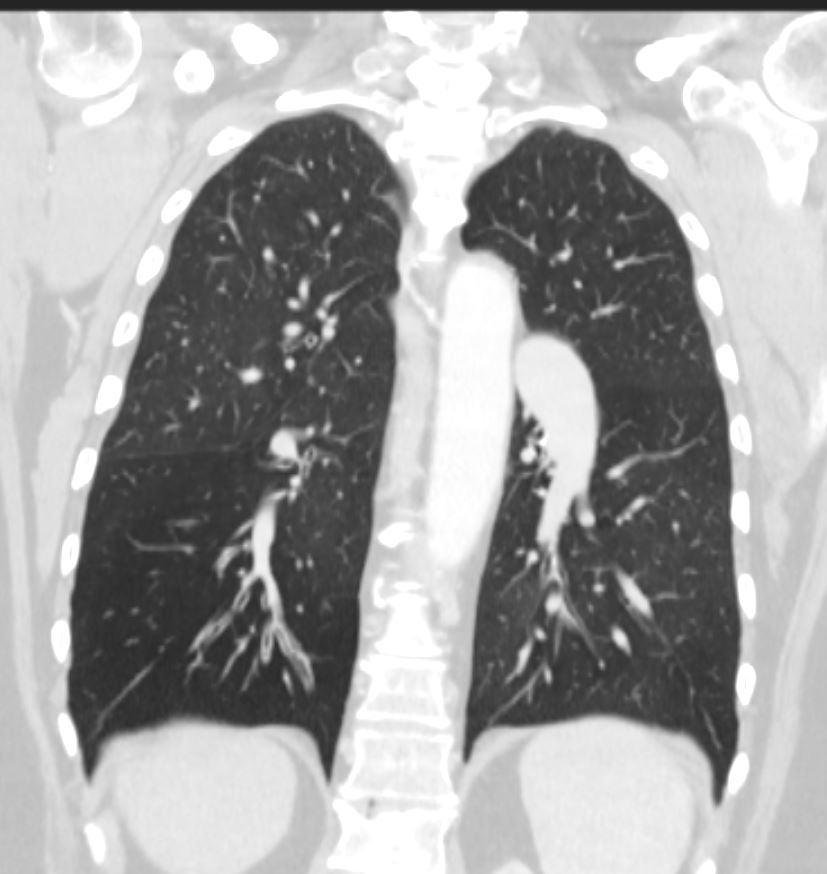
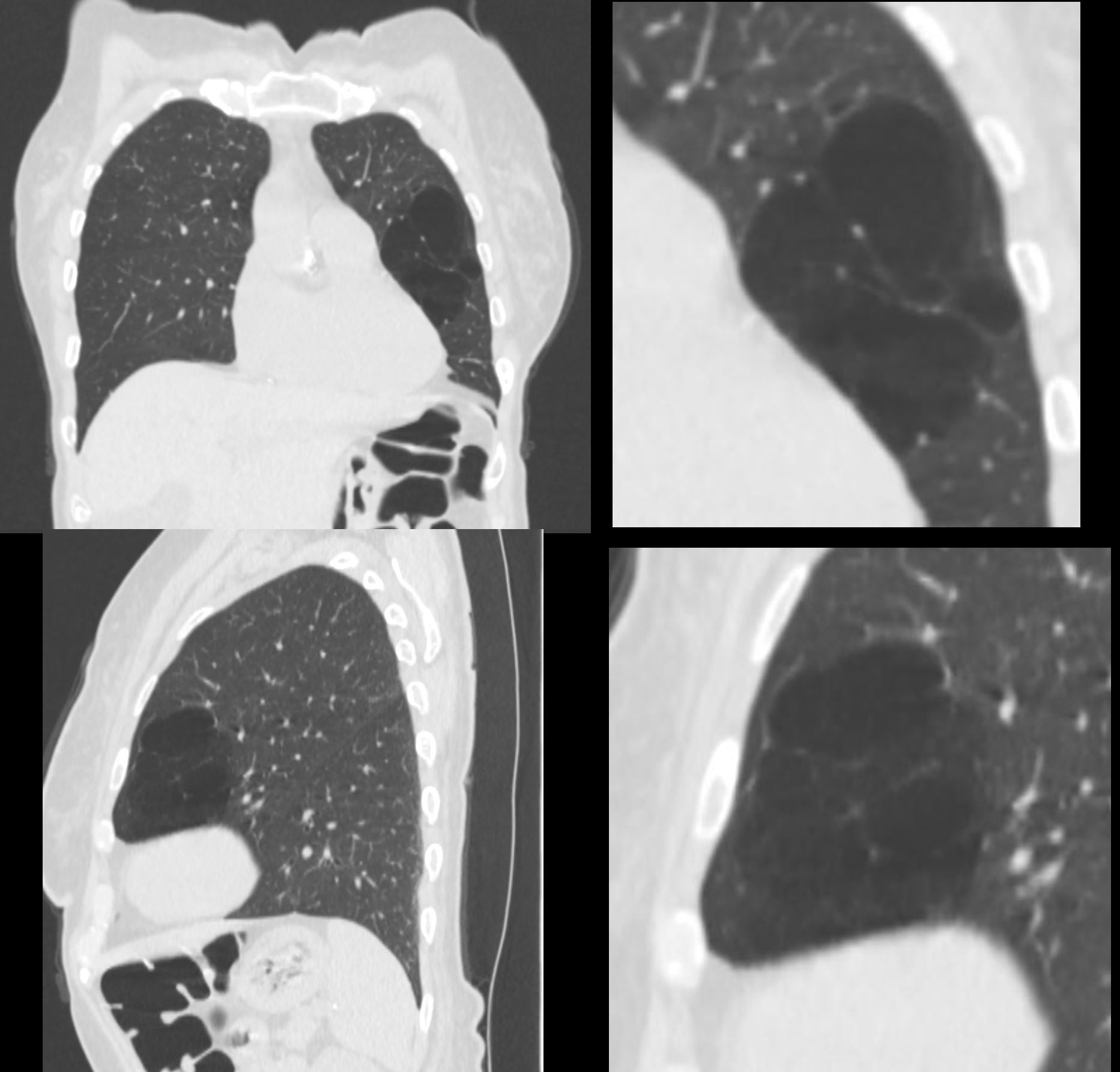
58 year old male presents with dyspnea.
Coronal and axial CT scans reveal a lucent left upper lung field consistent with air trapping There is a midlung opacity consistent with atelectasis of the superior segment of the lingula. The elevated left hemidiaphragm is secondary to the atelectasis and volume loss.
Findings are consistent with air trapping in a patient with Swyer James Syndrome. There is secondary compression of the superior lingula segment, secondary to the air trapping and hyperinflated LUL
Ashley Davidoff MD TheCommonVein.net 118069c01
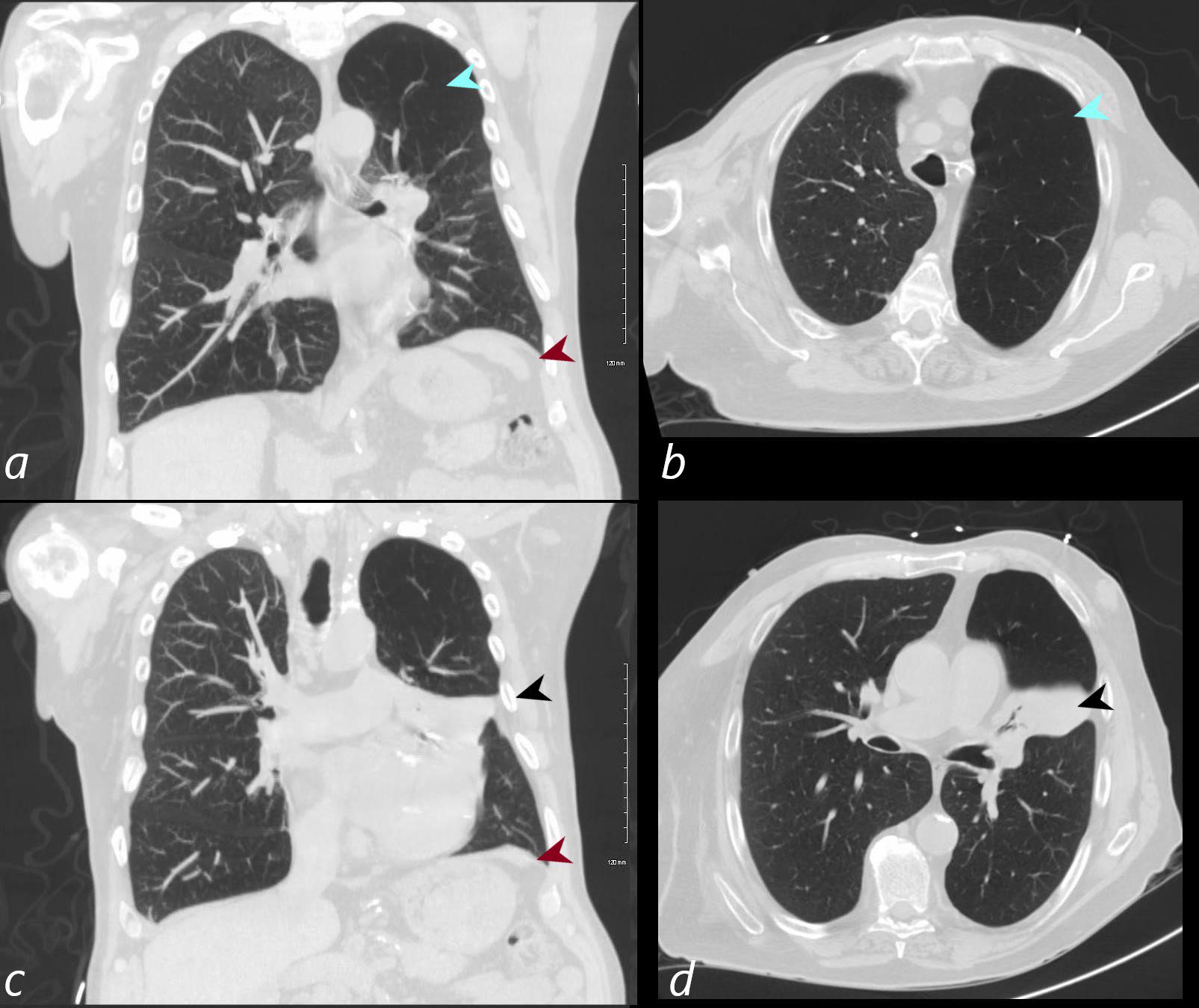
58 year old male presents with dyspnea.
Coronal and axial CT scans reveals a lucent left upper lung field consistent with air trapping (teal arrowheads a and b). There is a midlung opacity (black arrowheads c and d) consistent with atelectasis of the superior segment of the lingula with silhouetting of the left heart border. The elevated left hemidiaphragm (maroon arrows a and c) is secondary to the atelectasis and volume loss.
Findings are consistent with air trapping in a patient with Swyer James Syndrome. There is secondary compression of the superior lingula segment secondary to the air trapping and hyperinflated LUL
Ashley Davidoff MD TheCommonVein.net 118069c01L
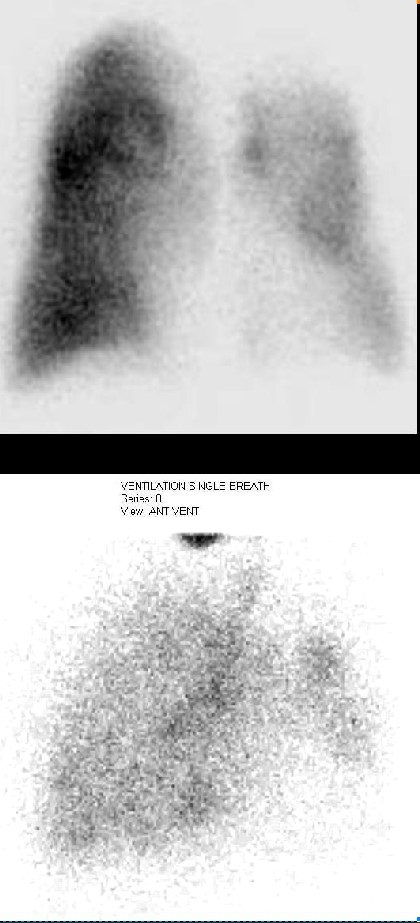
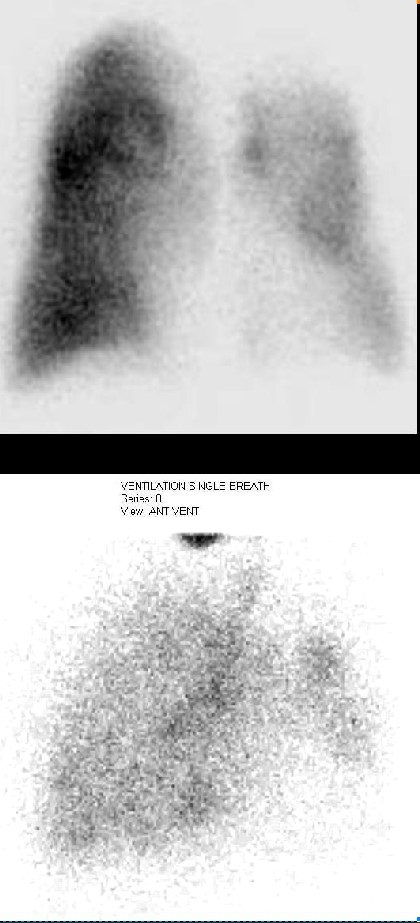
58 year old male presents with dyspnea.
Perfusion scan (upper image) and ventilation scan (lower image) showed decrease in both the perfusion and ventilation of the left upper lobe which had shown air trapping on the CXR and CT scan.
Findings of decrease in both ventilation and perfusion are consistent with air trapping in a patient with Swyer James Syndrome. There is secondary compression of the superior lingula segment secondary to the air trapping which also contributes to the findings.
Ashley Davidoff MD TheCommonVein.net 118079c
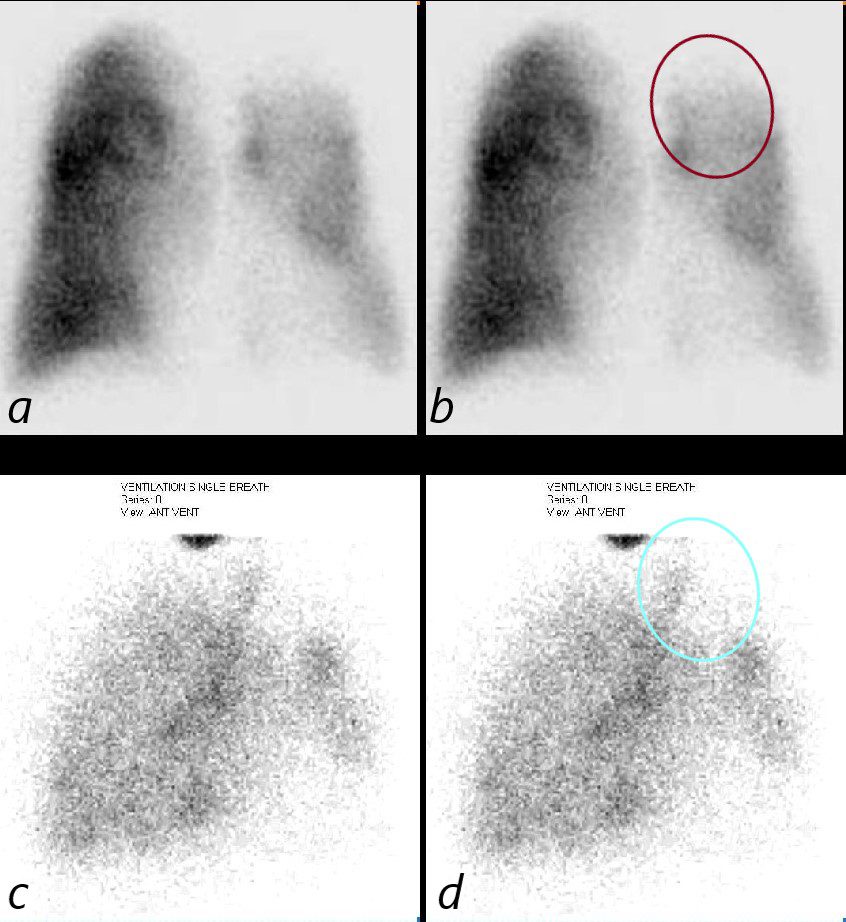
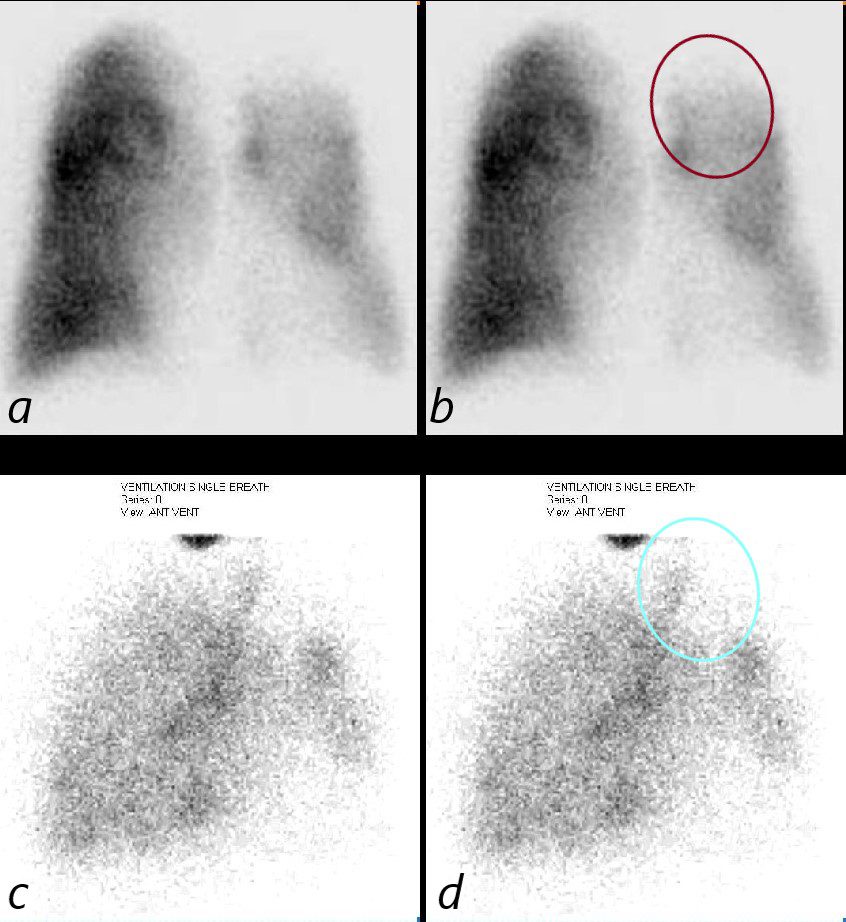
58 year old male presents with dyspnea.
Perfusion scan (upper images a and b) show decreased perfusion of the left upper lobe (maroon circle b). The ventilation scan (lower images c,d) show a decrease in the ventilation of the left upper lobe (teal circle d) The areas of decreased ventilation and perfusion had shown air trapping on the CXR and CT scan in the LUL as well as segmental atelectasis of the lingula .
Findings of decrease in both ventilation and perfusion are consistent with air trapping in a patient with Swyer James Syndrome.
Ashley Davidoff MD TheCommonVein.net 118079cL
Inferior Lingula Air Trapping
63 year old female presents with dyspnea
CT in the axial plane shows a hyperlucent subsegment of the lingula with sparse and constricted vasculature
Findings consistent with air trapping and Swyer James syndrome
Ashley Davidoff MD TheCommonVein.net 137658
63 year old female presents with dyspnea
CT in the coronal and sagittal planes shows a hyperlucent subsegment of the lingula with sparse and constricted vasculature.
Findings are consistent with air trapping and Swyer James syndrome
Ashley Davidoff MD TheCommonVein.net 137656c
- It is commonly associated with obstructive lung diseases such as asthma, chronic obstructive pulmonary disease (COPD), and bronchiolitis. The pathogenesis involves airway obstruction or collapse during expiration, preventing air from escaping the affected parts of the lungs, resulting in hyperinflation and difficulty with ventilation. Over time, this can impair lung function, leading to symptoms such as shortness of breath, wheezing, and reduced exercise tolerance. Air trapping is typically diagnosed through imaging, where it appears as areas of hyperlucency on a chest X-ray or CT scan, particularly in expiratory views. Pulmonary function
tests (PFTs) may also show a decreased expiratory flow rate, further confirming the presence of obstructive processes. - is an imaging and physiologic term to
- retained air in a part or parts of the lung
- more easily identified during expiration
- caused by
- obstruction
- often small airway disease
- chronic bronchitis
- asthma
- Hypersensitivity pneumonitis
- sarcoidosis
- bronchiolitis
- cystic fibrosis/bronchiectasis
- ILD
- obesity
- often small airway disease
- abnormality in lung compliance
- sometimes seen in normal people
- 50% of CT scans
- obstruction
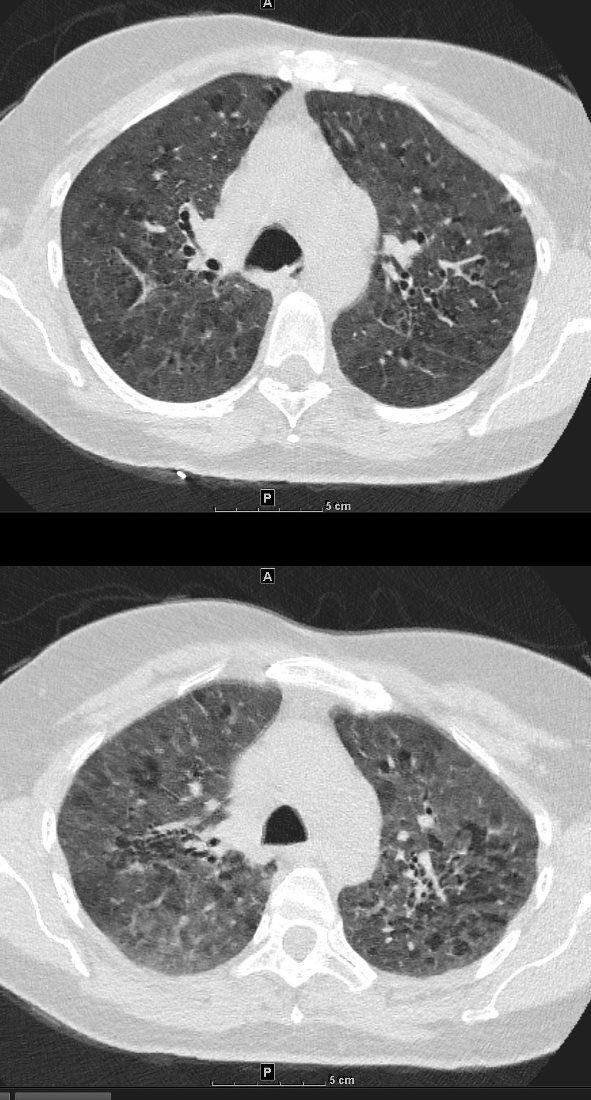
55-year-old female with shortness of breath. She keeps birds for pets Axial CT through the mid lung fields shows diffuse ground glass changes with a combination of mosaic attenuation and normal lung giving the appearance of the head cheese sign.
Ashley Davidoff MD TheCommonVein.net 242Lu 13551a
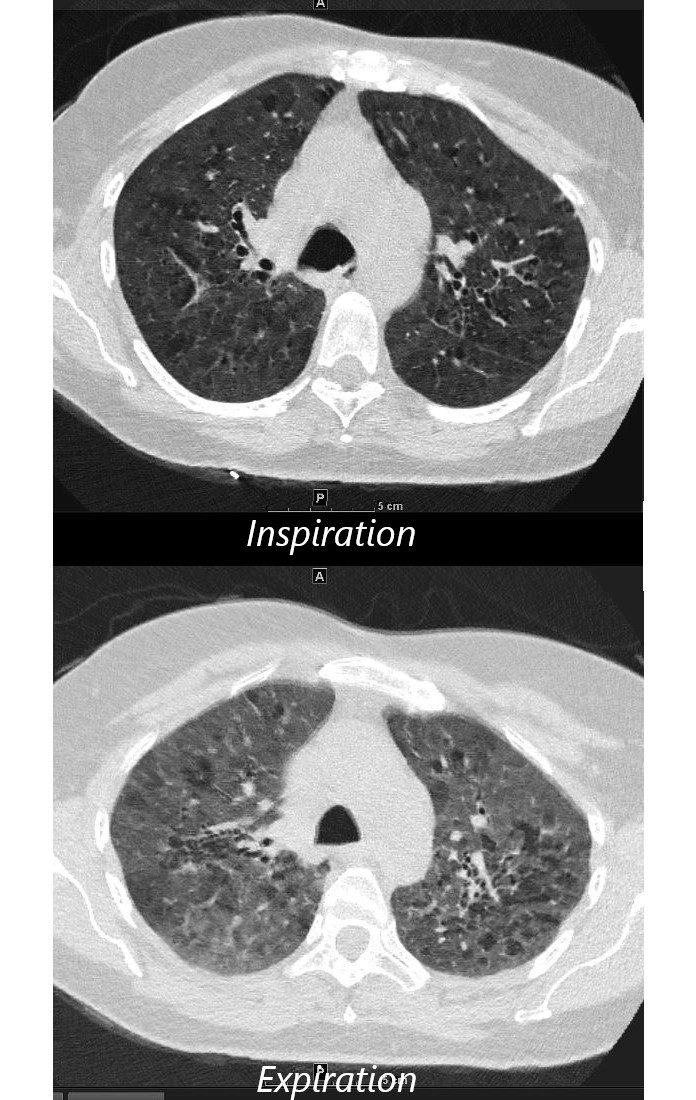
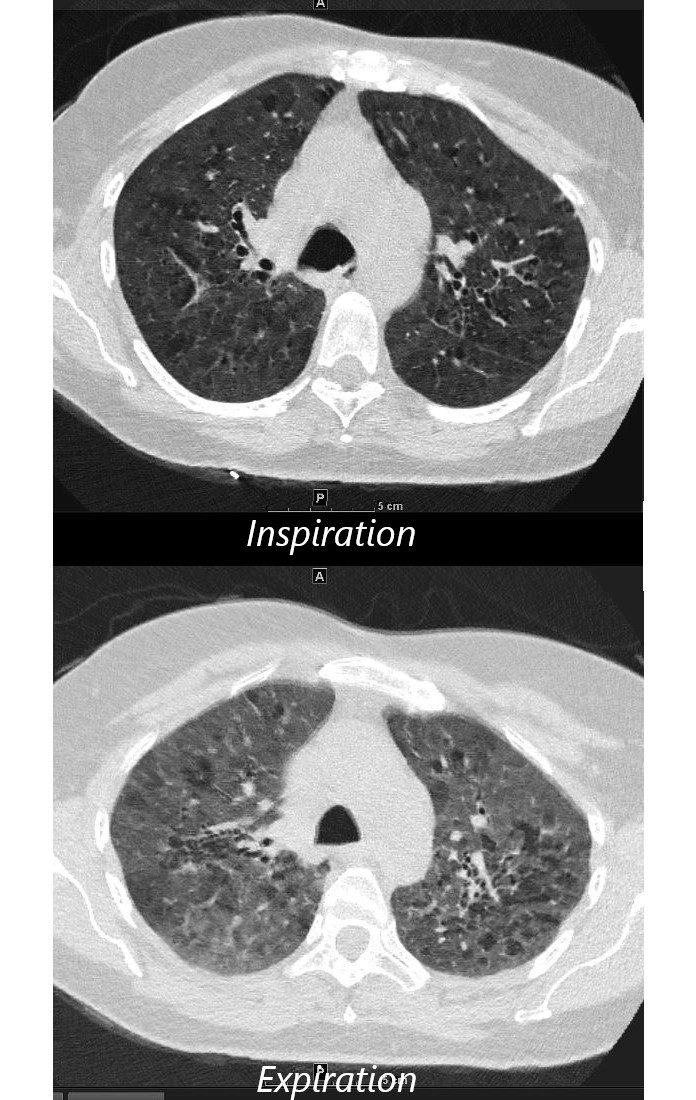
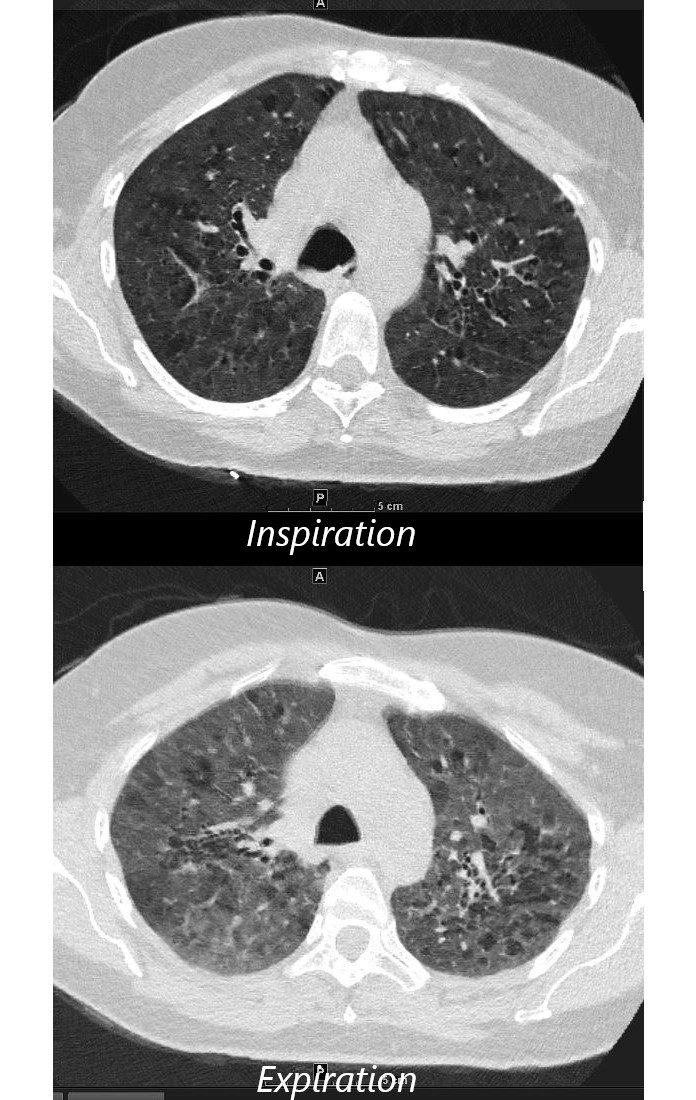
55-year-old female with shortness of breath. She keeps birds for pets Axial CT through the mid lung fields on inspiration, shows diffuse ground glass changes with a combination of mosaic attenuation and normal lung giving the appearance of the head cheese sign.
On the expiration phase the mosaic attenuation remains indicating air trapping and inferring small airway disease
Ashley Davidoff MD TheCommonVein.net 242Lu 13551aL
-

Air Trapping
Air trapping is a conclusive sign of airway obstruction 6 and appears as areas of decreased attenuation resulting from the presence of gas retained in the lung parenchyma.7 It may be necessary to compare between inspiratory and end-expiratory HRCT scans to determine the extent of air trapping, especially if the degree of air trapping is minimal.7 Patients with normal inspiratory scans frequently have signs of air trapping on expiratory scans, suggesting that expiratory scans should be performed as part of a standard evaluation.6
Mosaic Attenuation Caused by Obstruction of Small Airways
Medium Sized Airways and Smaller Airways are Filled with Mucus in a patient with COPD – Note Centrilobular Impaction of Mucus
Medium Sized Airways and Smaller Airways are Filled with Mucus – Note Centrilobular Impaction of Mucus
-
- Mosaic attenuation is an
- imaging pattern
- variable lung attenuation
- results in a heterogeneous appearance of the parenchyma.
- sometimes it is caused by air trapping
- sometimes by perfusion abnormalities
- sometimes normal
- imaging pattern
- Mosaic attenuation is an
Lobar Air Trapping Due to Mucus Impaction
Note Realative Lucency of the RLL compared to the LLL
Links and References
Fleischner Society
air trapping
Pathophysiology.—Air trapping is retention of air in the lung distal to an obstruction (usually partial).
CT scans.—Air trapping is seen on end-expiration CT scans as parenchymal areas with less than normal increase in attenuation and lack of volume reduction. Comparison between inspiratory and expiratory CT scans can be helpful when air trapping is subtle or diffuse (,11,,12) (,Fig 4). Differentiation from areas of decreased attenuation resulting from hypoperfusion as a consequence of an occlusive vascular disorder (eg, chronic thromboembolism) may be problematic (,13), but other findings of airways versus vascular disease are usually present. (See also mosaic attenuation pattern.)