TCV Anatomy: Aortopulmonary Window
Etymology
- Derived from “aorto-” (relating to the aorta) and “pulmonary” (relating to the pulmonary artery), the aortopulmonary window refers to the anatomical space between these two structures.
AKA
- AP window
What is it?
- The aortopulmonary window is a mediastinal space located between the ascending aorta and the pulmonary artery. It is bounded by key vascular and structural components and serves as a conduit for lymphatic, vascular, and nervous structures.
Classified as
- Part of the superior mediastinum.
Parts
- Anterior Boundary: Ascending aorta.
- Posterior Boundary: Left pulmonary artery.
- Superior Boundary: Aortic arch.
- Inferior Boundary: Left main bronchus.
- Lateral Boundaries: Mediastinal pleura.
Size and Shape
- Typically a triangular or oblong space on imaging.
- Variable size depending on the individual anatomy and pathological conditions.
Position
- Located in the superior mediastinum.
- Lies just above the left pulmonary artery and anterior to the tracheobronchial tree.
Character
- Contains lymph nodes, the ligamentum arteriosum, vagus and recurrent laryngeal nerves, and small vessels.
- Rich in lymphatic structures, making it clinically significant for oncological evaluation.
Blood Supply
- Supplied by branches of the aorta and pulmonary arteries.
Lymphatic Drainage
- Lymph nodes within the aortopulmonary window drain the lungs, pleura, and upper mediastinum.
Nerve Supply
- Contains the left recurrent laryngeal nerve, a branch of the vagus nerve, which loops around the ligamentum arteriosum.
Embryology
- Develops from the space left as the aortic arch and pulmonary arteries form during fetal development.
Histology
- Consists primarily of connective tissue, lymphatic tissue, and neurovascular structures.
Physiology and Pathophysiology
- Physiology:
- Acts as a passage for lymphatic and neurovascular structures.
- Pathophysiology:
- Enlarged lymph nodes or masses can compress surrounding structures, leading to symptoms such as hoarseness (via recurrent laryngeal nerve involvement), cough, or superior vena cava obstruction.
Applied Anatomy to Radiology
CXR
- Seen as a clear space on frontal chest radiographs.
- Obliteration of the aortopulmonary window can indicate lymphadenopathy or masses.
- Important for detecting mediastinal widening.
CT
- Radiologic Principles:
- Best visualized on contrast-enhanced CT scans.
- Lymphadenopathy appears as enlarged nodes (>10 mm short-axis diameter).
- Masses or pathologies involving this space can affect adjacent structures, such as the aortic arch or pulmonary artery.
- Applied Anatomy:
- Parts: Ascending aorta, pulmonary artery, left bronchus, lymph nodes.
- Size: Enlarged nodes or masses alter the normal dimensions.
- Shape: Pathological masses distort the triangular shape.
- Position: Deviations or compression of surrounding structures indicate pathology.
- Character: Evaluate for tissue density and contrast enhancement to differentiate masses from nodes.
- Time: Temporal changes in size or density can indicate progression or resolution of disease.
MRI
- Rarely used but can provide detailed soft-tissue contrast for evaluating masses or lymphadenopathy.
PET-CT
- Useful for assessing metabolic activity of lymph nodes or masses in the window.
- Differentiates active disease from fibrotic or inactive nodes.
Other
- Ultrasound (Endobronchial Ultrasound, EBUS):
- Can assess and sample lymph nodes in the aortopulmonary window.
Pathological Implications
- Lymphadenopathy: Seen in malignancies (e.g., lung cancer, lymphoma) or inflammatory diseases (e.g., sarcoidosis, tuberculosis).
- Masses: Mediastinal tumors, vascular aneurysms.
- Vascular Abnormalities: Aortic aneurysms, pulmonary artery dilation.
- Nerve Involvement: Compression of the recurrent laryngeal nerve causing hoarseness (Ortner’s syndrome).
Key Points and Pearls
- A clear aortopulmonary window on imaging is a normal finding.
- Obliteration of this space warrants further investigation for lymphadenopathy or mass lesions.
- Contrast-enhanced CT is the gold standard for evaluation.
- PET-CT is essential for assessing metabolic activity in suspected malignancies.
- EBUS provides a minimally invasive method for biopsy of lymph nodes in this region.
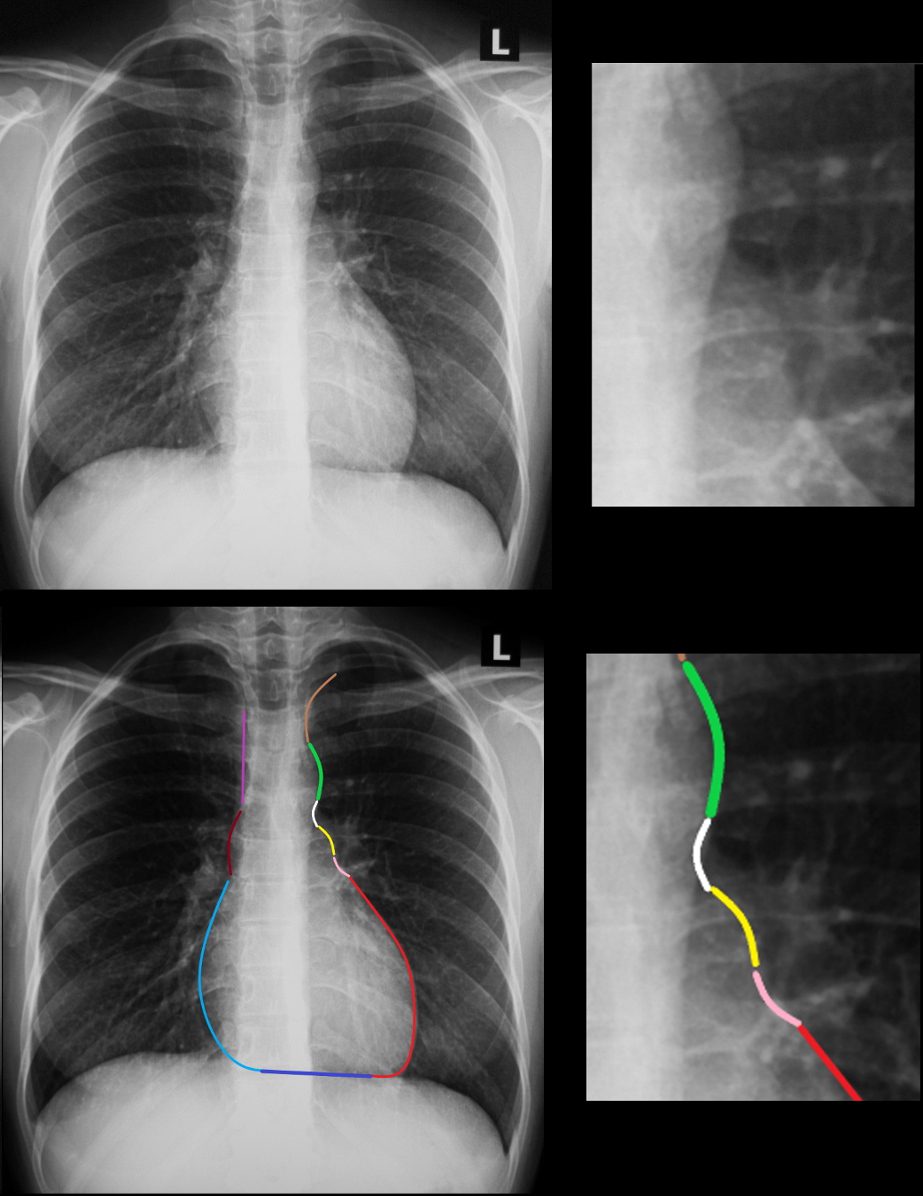
Normal frontal CXR shows the location of the aortopulmonary (A-P) window (magnified in b and d – white arrowhead) and lying between the aortic knob above (d, green curve) and the pulmonary artery below (c and d yellow curve). The “curves” are often described as moguls of the left heart border by creating an imaginary ski slope with the silhouette of each convex outward left sided structure representing a mogul, and the left ventricular silhouette representing the final mogul free ski slope
Ashley Davidoff MD TheCommonVein.net 33679c
