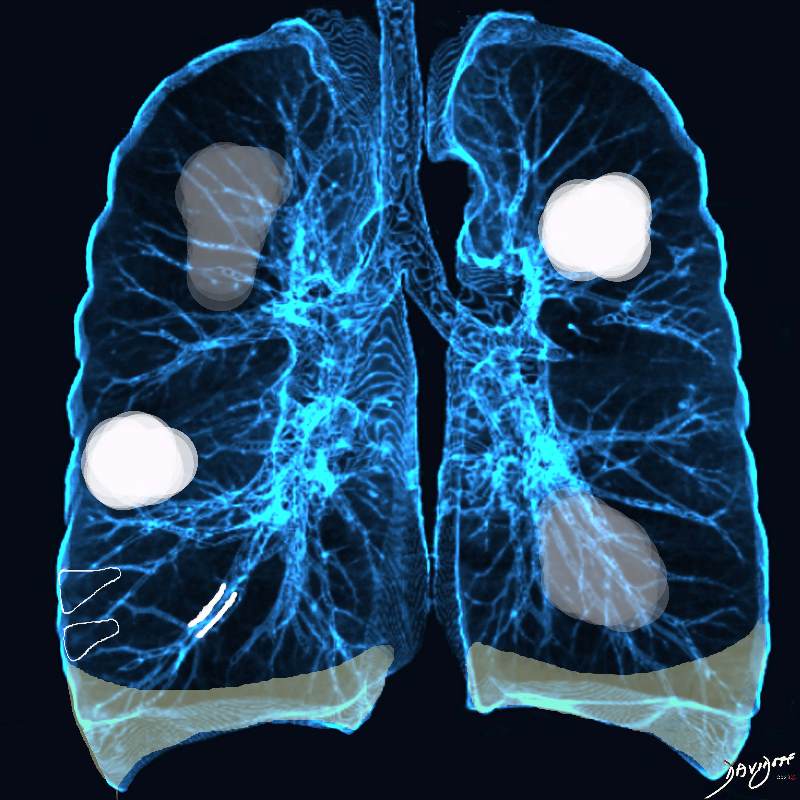
Acute Eosinophilic pneumonia is characterised by ground glass opacities (100%) and sometimes consolidation (55%) most commonly with a random distribution 60%. Septal lines (90%) and thickening of the bronchovascular bundles (66%) and bilateral pleural effusions (75%) were common. Ashley Davidoff MD TheCommonvein.net lungs-0775-b (Reference De Giacomi F et al)
Acute Eosinophilic pneumonia is characterised by ground glass opacities (100%) and sometimes consolidation (55%) most commonly with a random distribution 60%. Septal lines (90%) and thickening of the bronchovascular bundles (66%) and bilateral pleural effusions (75%) were common.
Ashley Davidoff MD TheCommonvein.net lungs-0775-bL (Reference De Giacomi F et al)
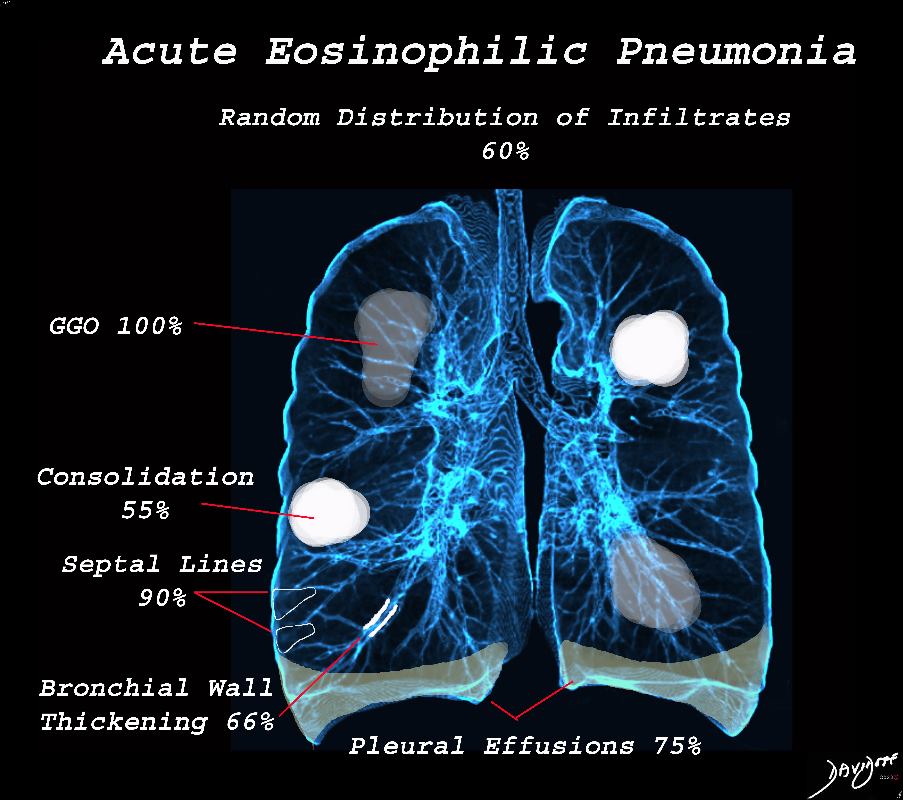
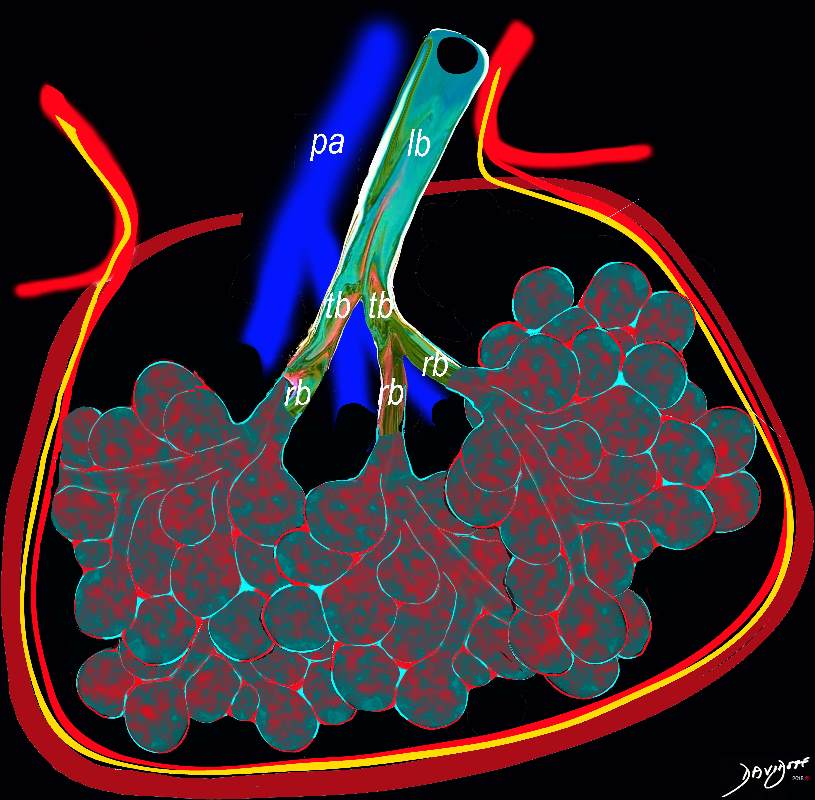
Acute Eosinophillic Pneumonia with Involvement of Small Airways, Alveoli and Interlobular Septa
Ashley Davidoff TheCommonVein.net lungs-0757b
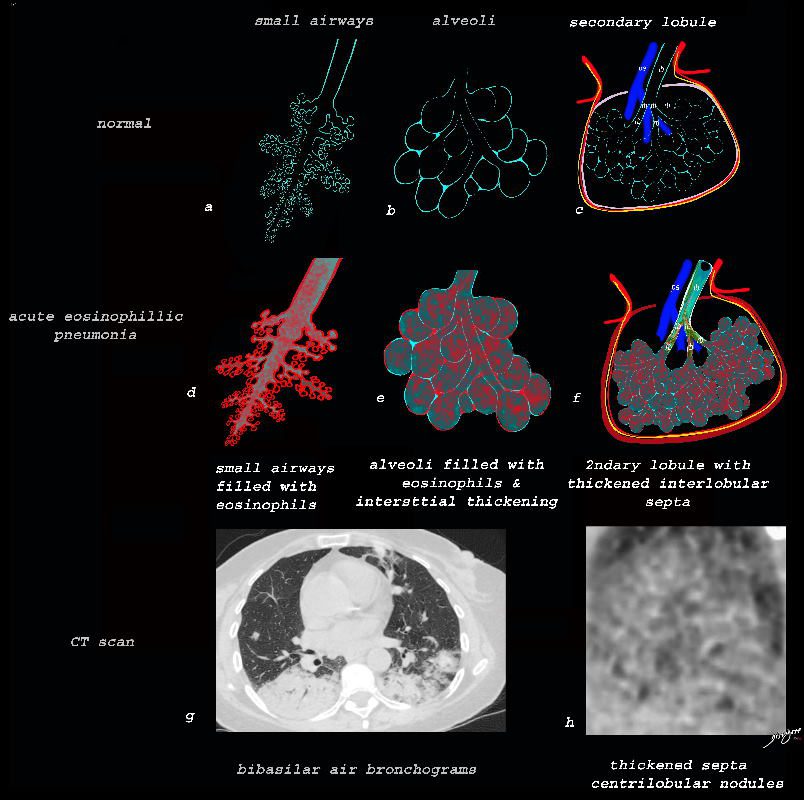
Small Airways Infiltration with Eosinophils and Inflammatory Exudate – Centrilobular Nodules
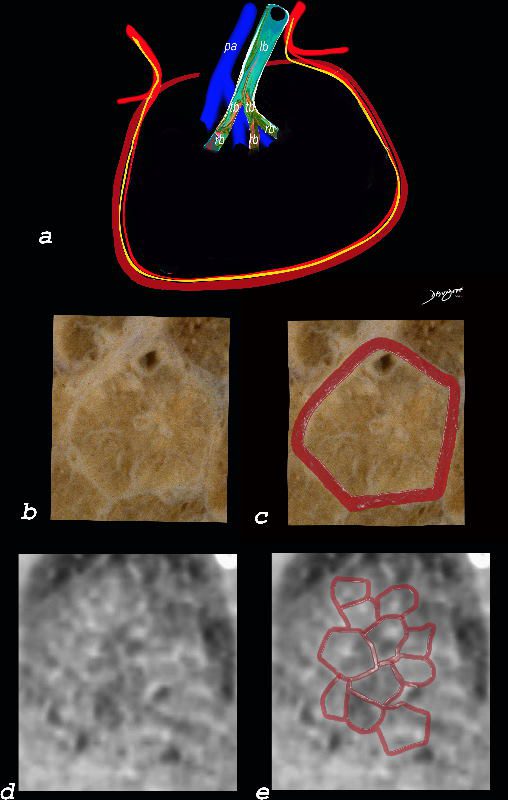
The diagram shows the small airways of the lung including the respiratory bronchiole, alveolar ducts and alveolar sacs in coronal (a) and in cross section (b) and correlated with an anatomic specimen of a secondary lobule that contains a thickened interlobular septum . The respiratory bronchiole is overlaid in maroon (d), next to the arteriole. Images e and f are magnified views of a CT of the lungs in a patient with acute eosinophillic pneumonia and the centrilobular nodules reflecting small airway disease are highlighted in f.
Ashley Davidoff MD The CommonVein.net lungs-0760b
Interlobular Septal Infiltration with Eosinophils and Inflammatory Exudate – Thickening of the Interlobular Septa – Crazy Paving Kerley B lines
The diagram shows the thickened septum surrounding the secondary lobule due to an inflammatory process, cellular infiltrate and congestion of the venules and lymphatics in the septum (a) . An anatomic specimen of a secondary lobule from a patient with thickened interlobular septa is shown in c and overlaid in d. CT of the lungs in a patient with acute eosinophillic pneumonia shows thickened interlobular septa and centrilobular nodules and the thickened septa are overlaid in red (e).
Ashley Davidoff MD The CommonVein.net lungs-0761
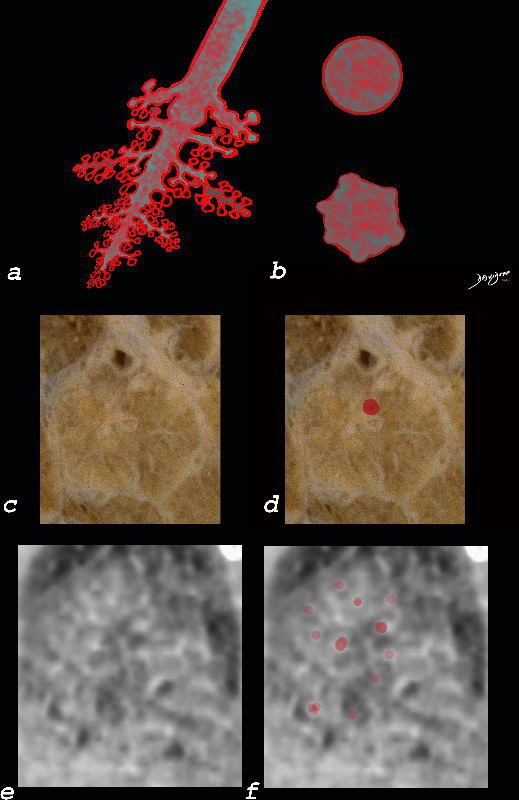
Alveolar and Interalveolar Interstitial Infiltration with Eosinophils and Inflammatory Exudate – Ground Glass Changes
The ground glass changes are a combination of the cellular and exudative inflammatory response in the small airways, alveoli, interalveolar septa and interstitium, and thickened alveolar septum
The ground glass changes are a combination of the cellular and exudative inflammatory response in the small airways, alveoli, interalveolar septa and interstitium, and thickened alveolar septum
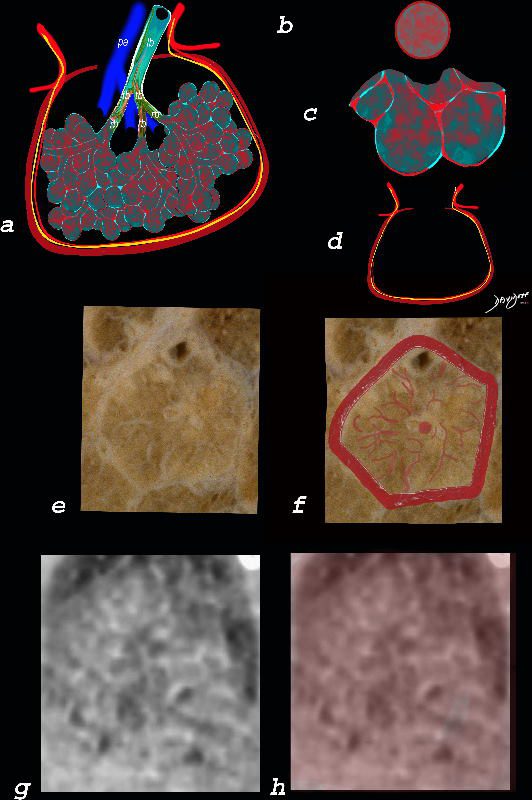
The diagram shows the abnormal secondary lobule (a) The involved components include the small airways(b) alveoli and interalveolar interstitium (c) and the thickened interlobular septum (d) surrounding the secondary lobule due to an inflammatory process, cellular infiltrate and congestion of the venules and lymphatics in the septum. An anatomic specimen of a secondary lobule from a patient with thickened interlobular septa and interstitial thickening is shown in image e, and is overlaid in red (f) . A magnified view of an axial CT of the lungs in a patient with acute eosinophillic pneumonia shows thickened interlobular septa and centrilobular nodules (g) The inflammatory changes in the aforementioned structures result in an overall increase in density of the lung manifesting as ground glass changes (g) and overlaid in red (h)
Ashley Davidoff MD The CommonVein.net lungs-0762
Ashley Davidoff TheCommonVein.net
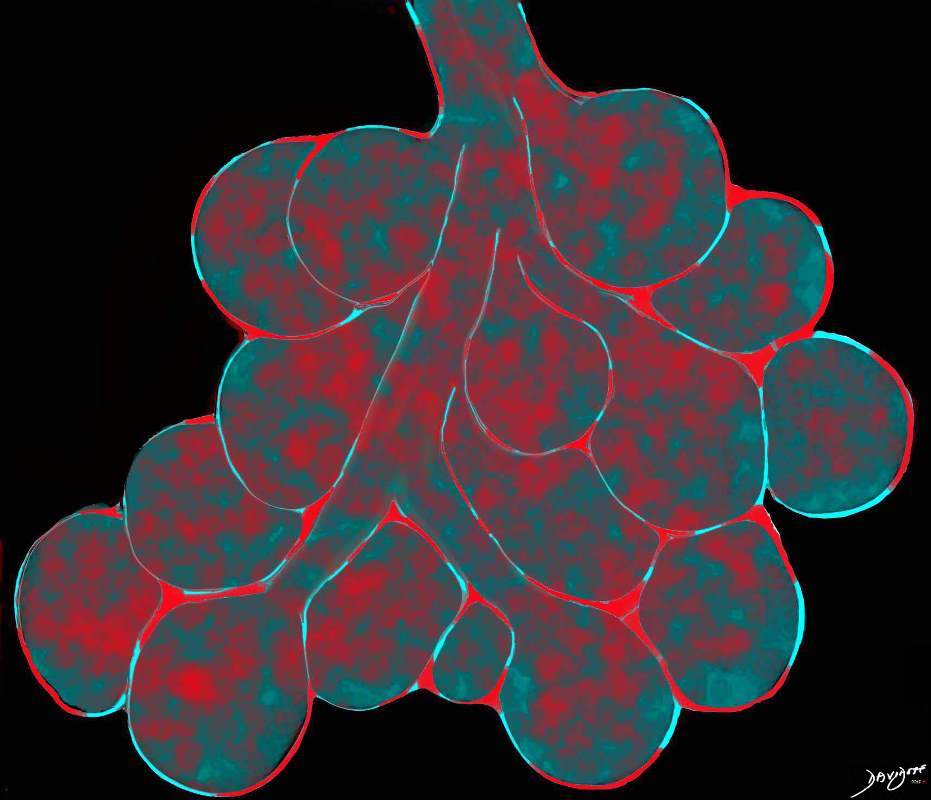
lungs-0756b01
This diagram reveals the important structural changes in the secondary lobule that includes filling of the alveoli with eosinophils and proteinaceous and fibrinous exudate as well as infiltration into the alveolar septa and interstitium (red walls of alveoli) . An important component of the disease is the thickening of the interlobular septa (maroon) which results in Kerley B lines and an interstitial pattern on the CXR and CT that is reminiscent of cardiogenic interstitial edema.
Ashley Davidoff TheCommonVein.net lungs-0758
Advancing Acute Eosinophilic Pneumonia which may go onto Diffuse Alveolar Damage and ARDS
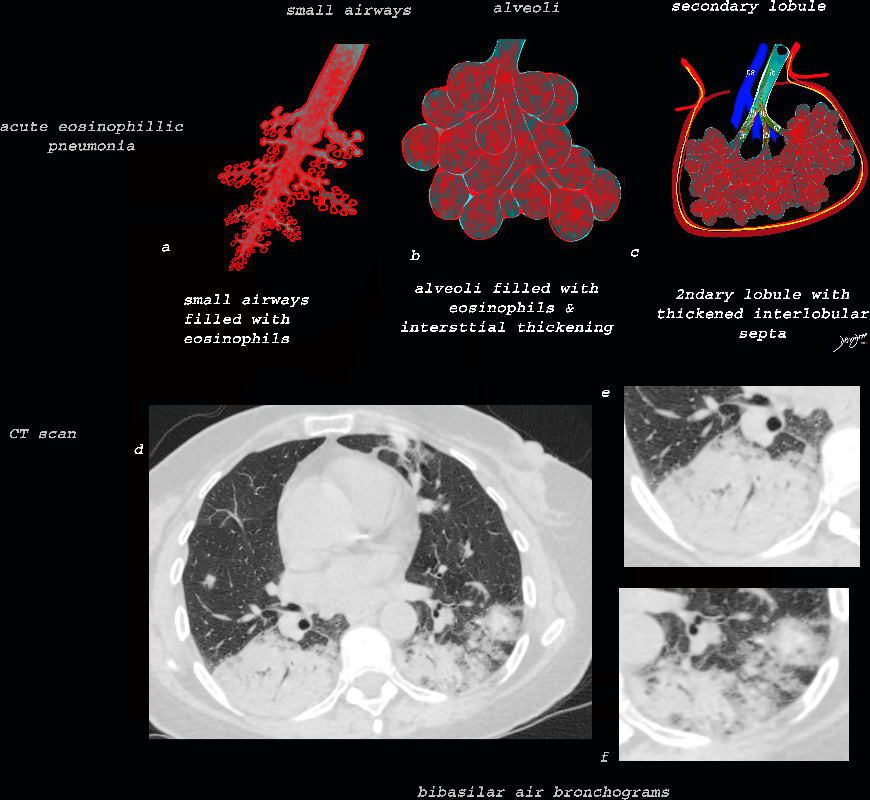
As the disease advances the small airways, and alveoli, get progressively filled with eosinophils, inflammatory cells and fluids resulting in consolidation. This image reveals progressive filling of the small airways, (a) alveoli, (b) and secondary lobules (c) with eosinophils and products of inflammation resulting in multi-segmental consolidations (d), in the lung bases, with air bronchograms at the right base (e), and less dense consolidation at the left base (f)
Ashley Davidoff MD The CommonVein.net lungs-0763
