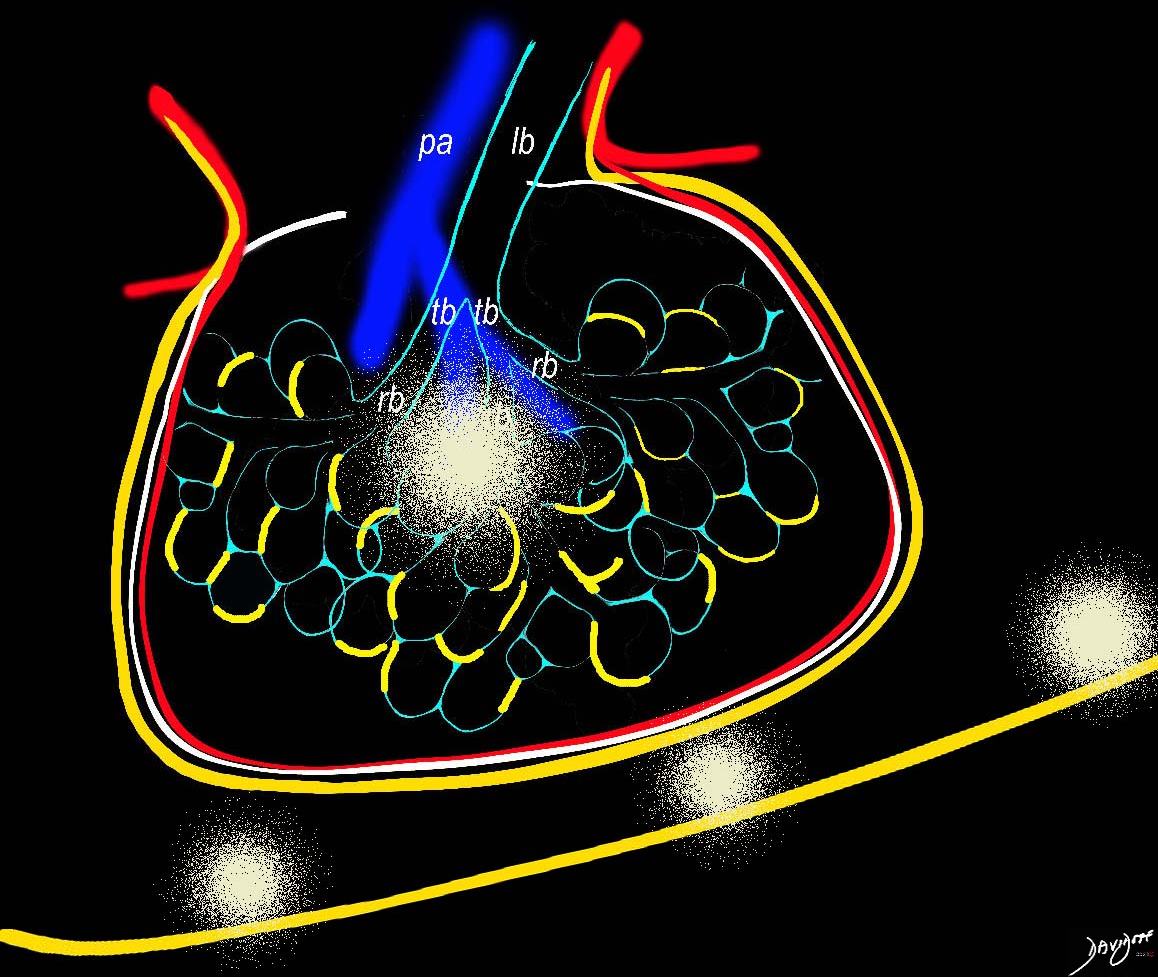
The infiltration of lymphocytes, histiocytes and plasma cells along the lymphatics of the lungs, can sometimes result in ill defined nodules that may be centrilobular or subpleural in location
Ashley Davidoff MD TheCommonVein.net
32645a06L
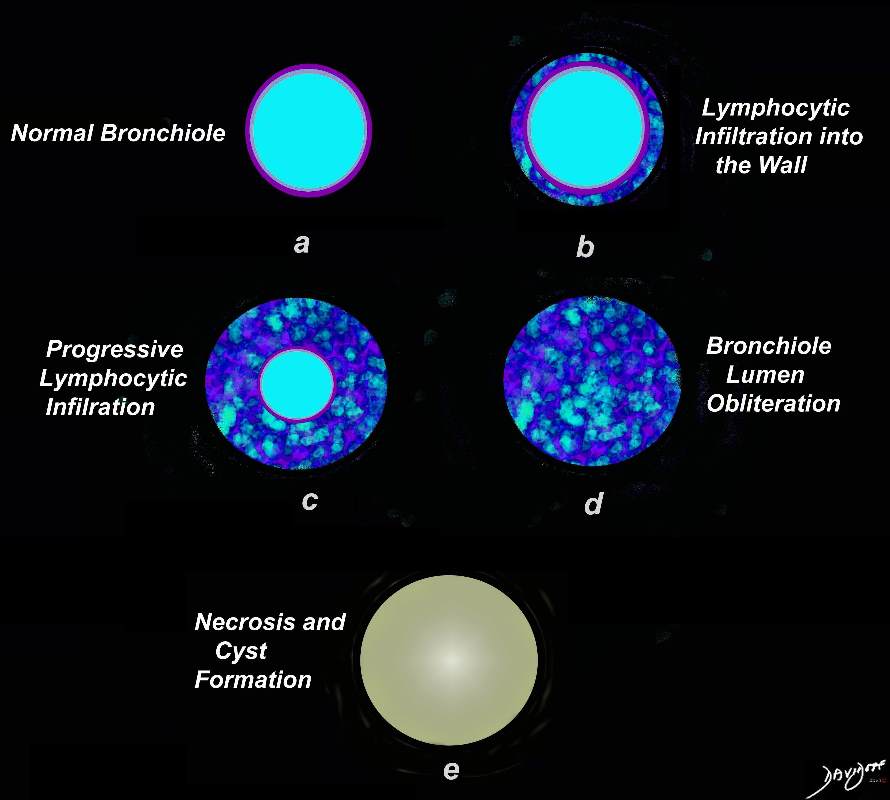
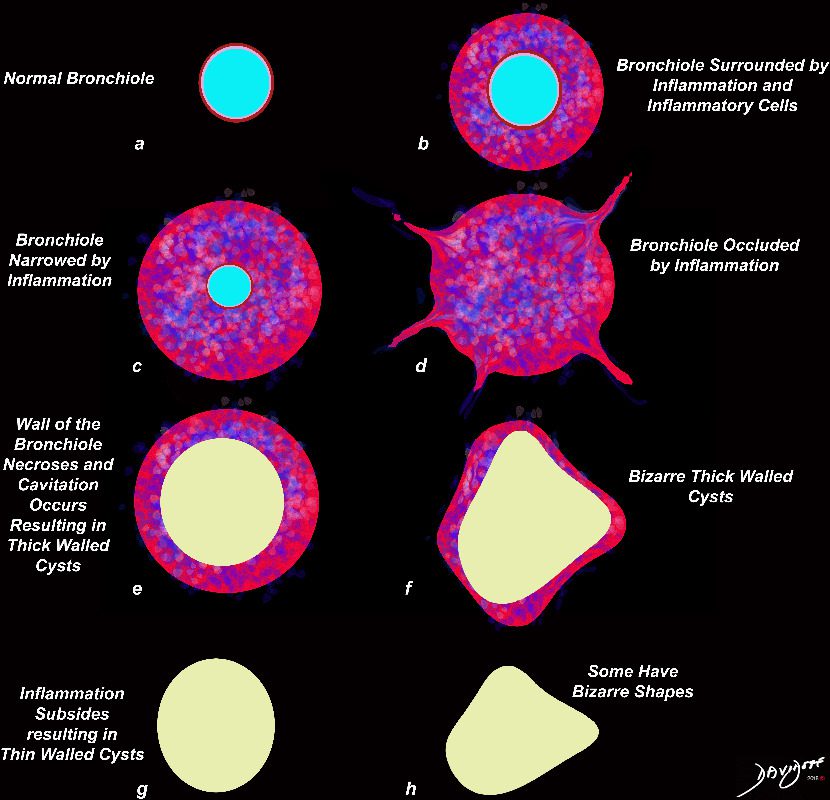
Artistic rendering shows a normal bronchiole (a) with early infiltration into the wall of the airway, (b) withprogressive infiltration with luminal compromise (c) evolving into obliteration (d). This would result in centrilobular nodules radiologically. Subsequently there is necrosis and a thin walled cyst remains
Ashley Davidoff MD TheCommonVein.net 139264.lungs
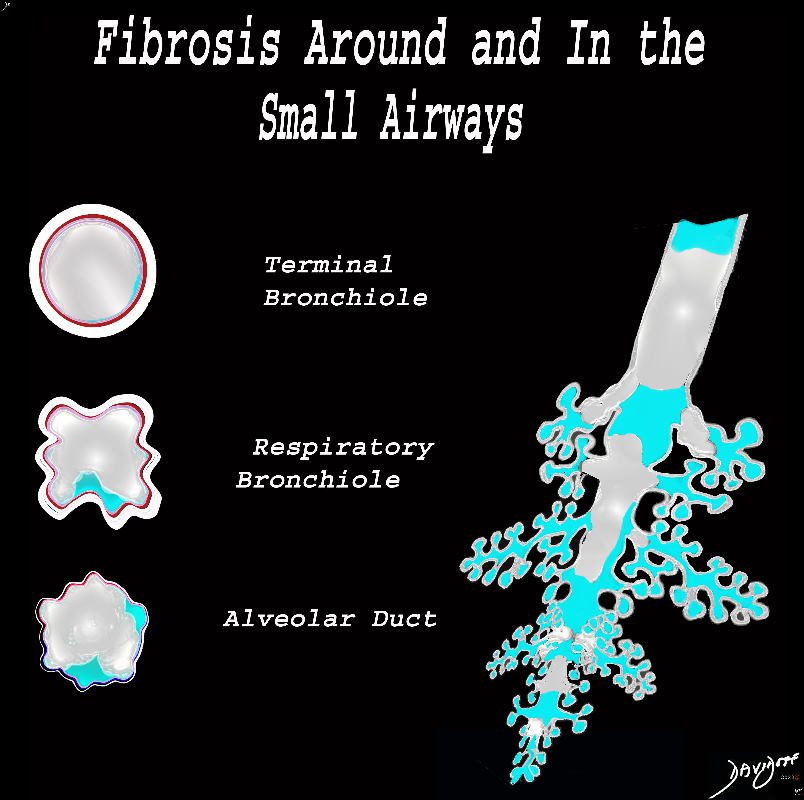
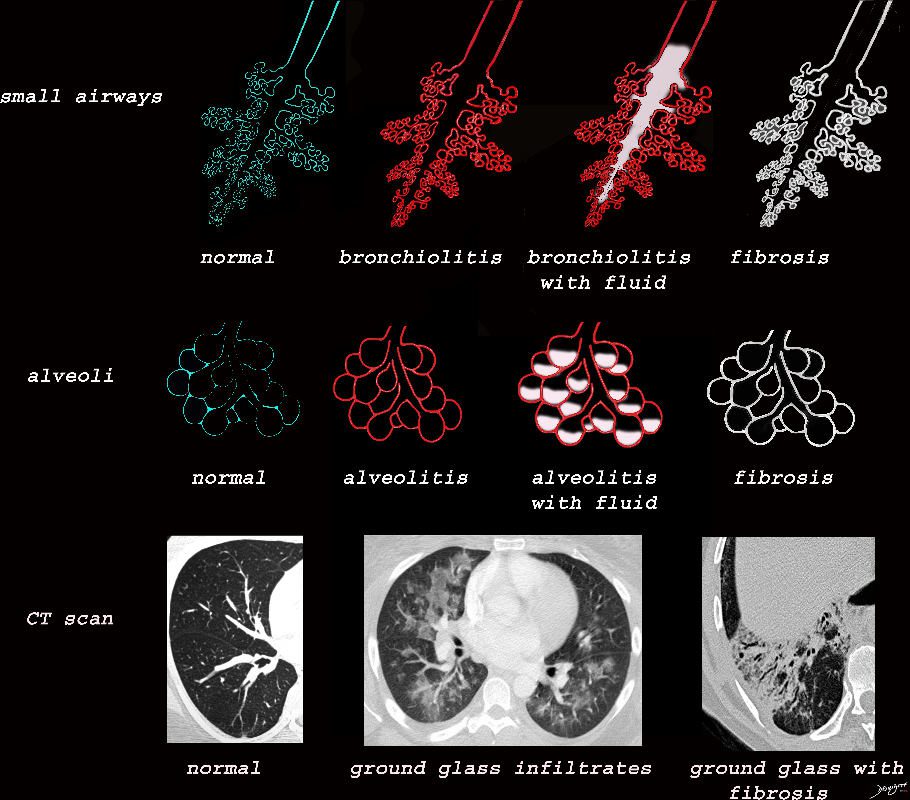
The diagram shows fibrotic changes around and within the small airways including the terminal bronchiole, respiratory bronchiole and the alveolar duct. In this instance the increase density from the fibrotic tissue would result in ground glass changes in the parenchyma and solid centrilobular nodules. Obstruction of the small airways would result in air trapping.
Ashley Davidoff MD TheCommonVein.net lungs-0778
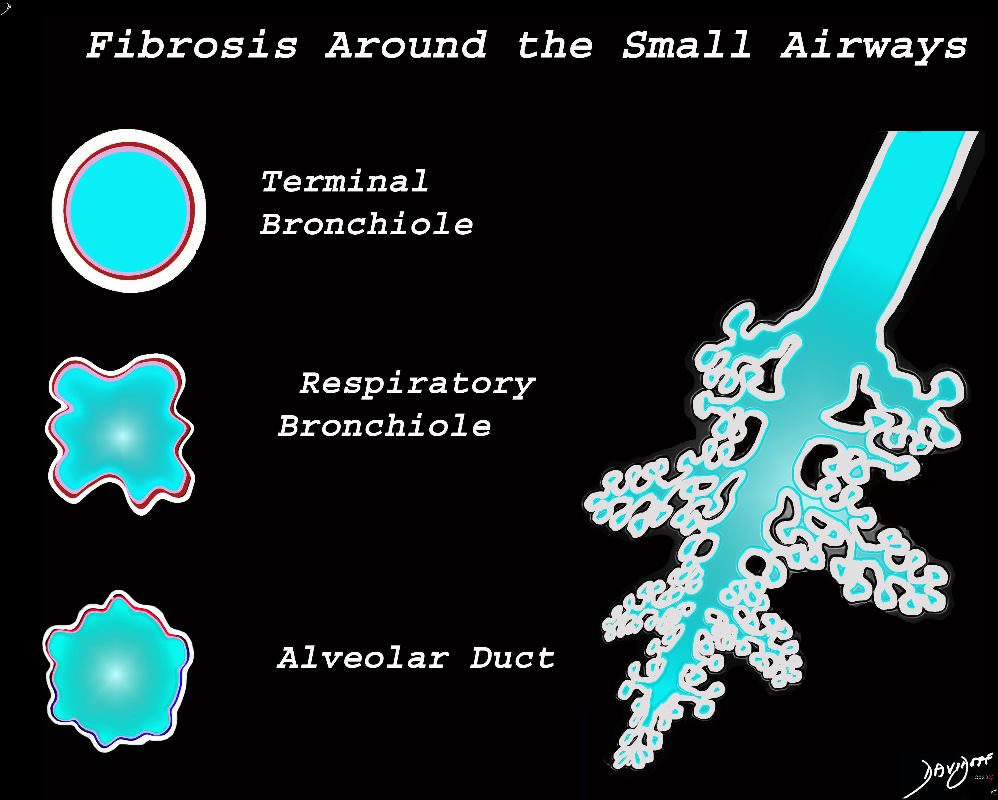
The diagram shows fibrotic changes around the small airways including the terminal bronchiole, respiratory bronchiole and the alveolar duct. In this instance the increase density from the fibrotic tissue would result in ground glass changes in the parenchyma and ground glass centrilobular nodules. Since the airways are patent there would be no air trapping.
Ashley Davidoff MD TheCommonVein.net lungs-0777
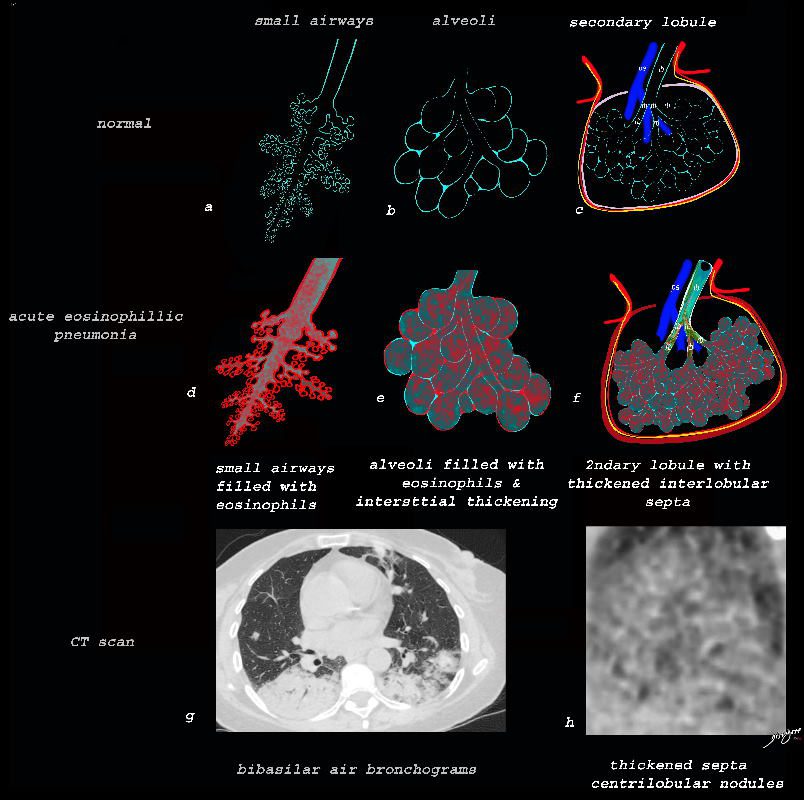
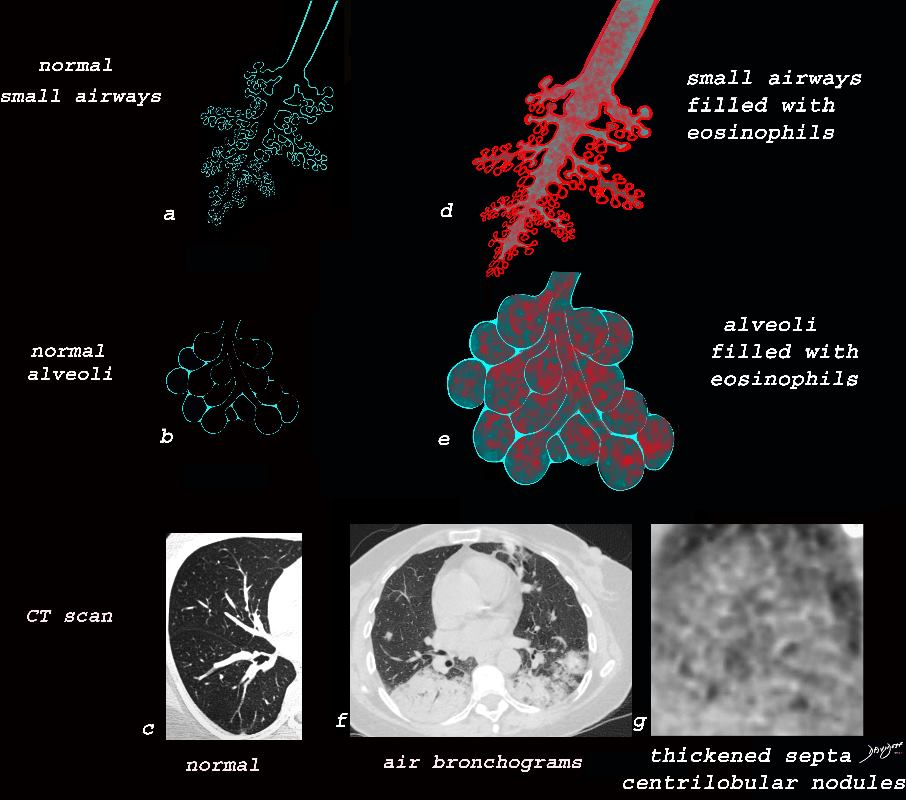
Alveolar and Interalveolar Interstitial Infiltration with Eosinophils and Inflammatory Exudate – Ground Glass Changes
The ground glass changes are a combination of the cellular and exudative inflammatory response in the small airways, alveoli, interalveolar septa and interstitium, and thickened alveolar septum
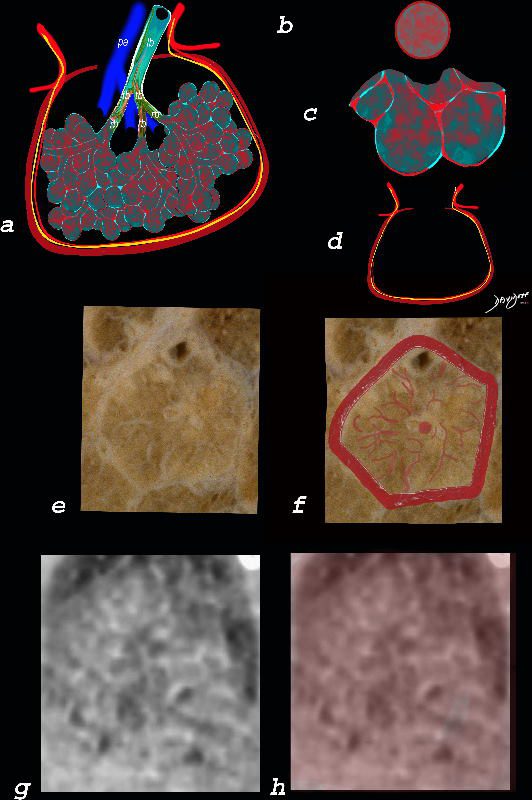
The diagram shows the abnormal secondary lobule (a) The involved components include the small airways(b) alveoli and interalveolar interstitium (c) and the thickened interlobular septum (d) surrounding the secondary lobule due to an inflammatory process, cellular infiltrate and congestion of the venules and lymphatics in the septum. An anatomic specimen of a secondary lobule from a patient with thickened interlobular septa and interstitial thickening is shown in image e, and is overlaid in red (f) . A magnified view of an axial CT of the lungs in a patient with acute eosinophillic pneumonia shows thickened interlobular septa and centrilobular nodules (g) The inflammatory changes in the aforementioned structures result in an overall increase in density of the lung manifesting as ground glass changes (g) and overlaid in red (h)
Ashley Davidoff MD The CommonVein.net lungs-0762
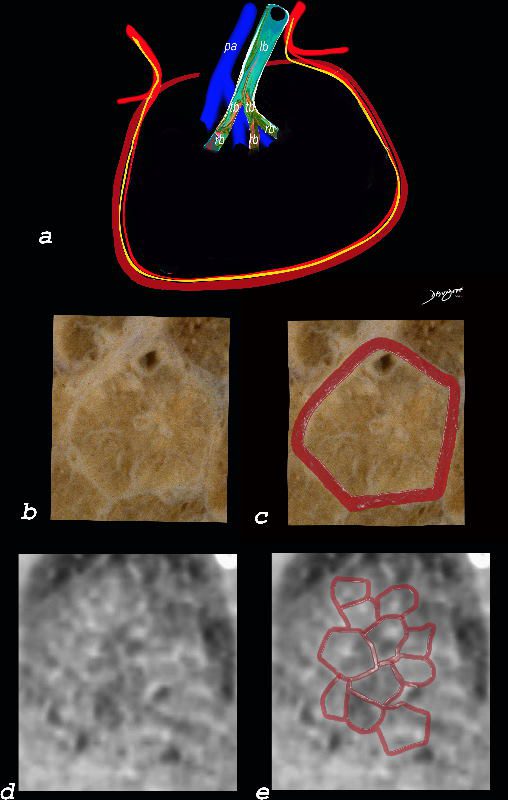
Interlobular Septal Infiltration with Eosinophils and Inflammatory Exudate – Thickening of the Interlobular Septa – Crazy Paving Kerley B lines
The diagram shows the thickened septum surrounding the secondary lobule due to an inflammatory process, cellular infiltrate and congestion of the venules and lymphatics in the septum (a) . An anatomic specimen of a secondary lobule from a patient with thickened interlobular septa is shown in c and overlaid in d. CT of the lungs in a patient with acute eosinophillic pneumonia shows thickened interlobular septa and centrilobular nodules and the thickened septa are overlaid in red (e).
Ashley Davidoff MD The CommonVein.net
lungs-0761
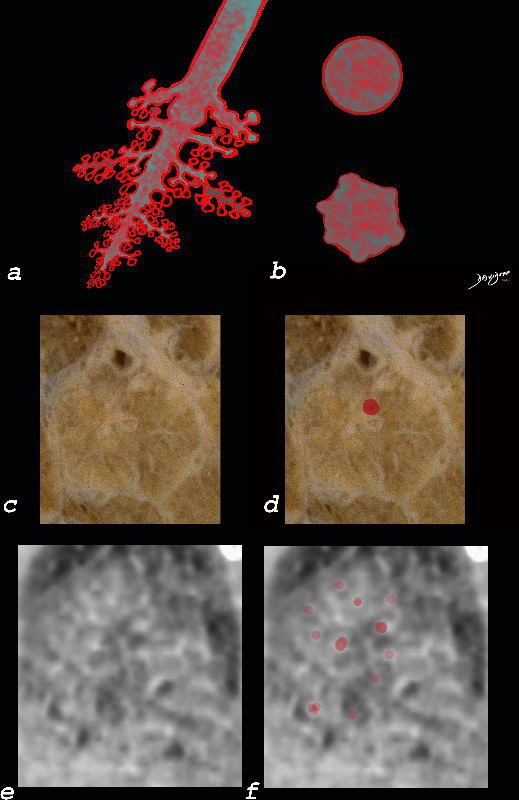
Small Airways Infiltration with Eosinophils and Inflammatory Exudate – Centrilobular Nodules
The diagram shows the small airways of the lung including the respiratory bronchiole, alveolar ducts and alveolar sacs in coronal (a) and in cross section (b) and correlated with an anatomic specimen of a secondary lobule that contains a thickened interlobular septum . The respiratory bronchiole is overlaid in maroon (d), next to the arteriole. Images e and f are magnified views of a CT of the lungs in a patient with acute eosinophillic pneumonia and the centrilobular nodules reflecting small airway disease are highlighted in f.
Ashley Davidoff MD The CommonVein.net lungs-0760b
Ashley Davidoff TheCommonVein.net lungs-0757b
Ashley Davidoff TheCommonVein.net lungs-0757
Ashley Davidoff MD TheCommonVein.net lungs-0733
Ashley Davidoff MD TheCommonVein.net
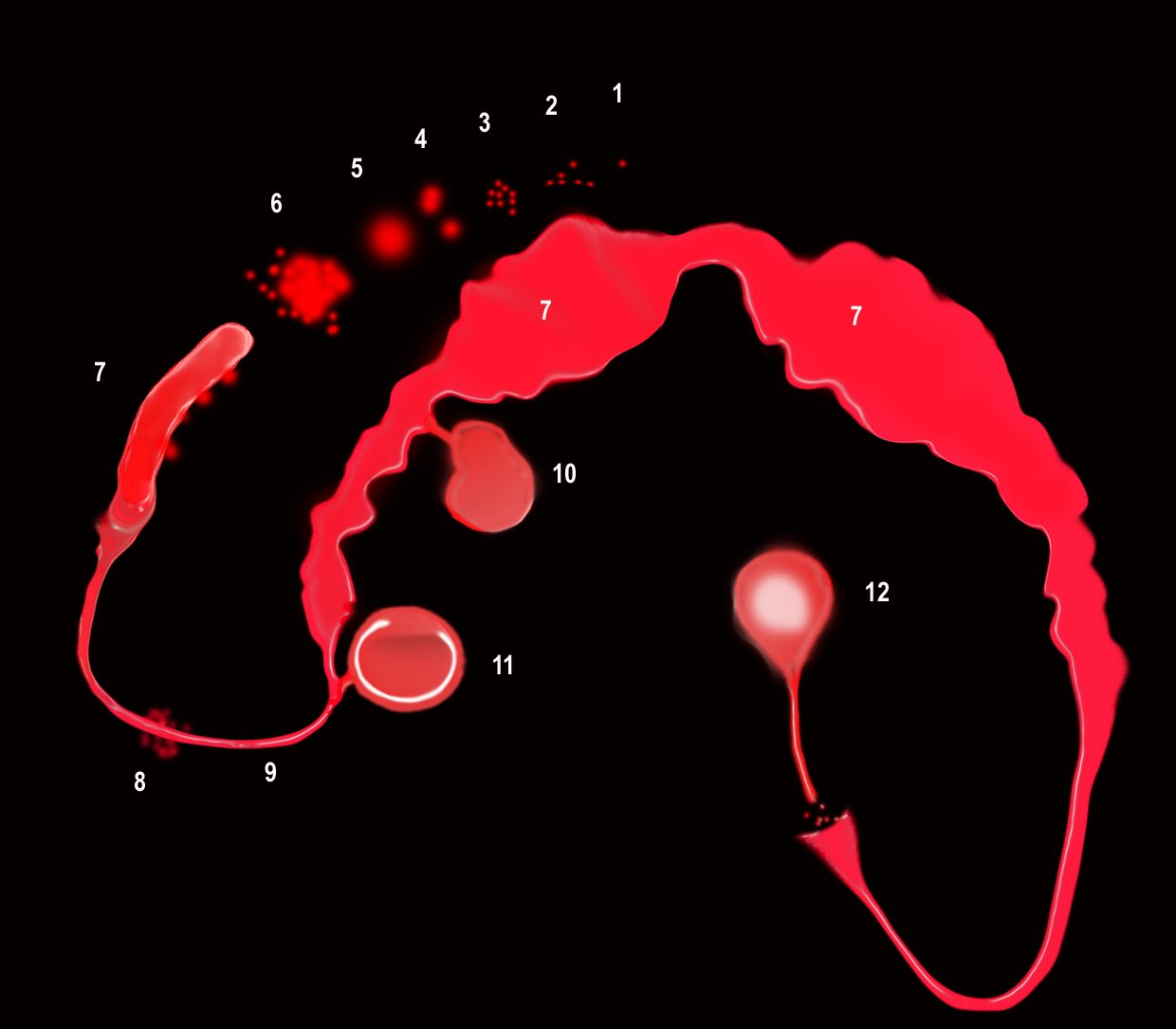
“S” of SARCOIDOSIS
The granulomas start as micronodules in close association with the lymphatics (1) spread in the intralobular septa and centrilobular bronchioles ((2) cluster and conglomerate to form macro nodules (4,5) sometimes manifesting as the galaxy sign (6). As they cluster and conglomerate they can cause conglomerate masses along the pathway (7) most commonly centrally as the lymphatics become confluent in the hila (7)
The lymphovascular bundles may be accompanied by nodularity (8) or just by thickening (9).
The lymph nodes in the mediastinum become significantly enlarged and fleshy (10). They often calcify (12) sometimes on the calcify on the rim of the node (eggshell calcification (11)
Sarcoidosis is a nodular granulomatous disease which predominated in the upper lobes and has its epicenter in the lymphoid tissue of the lungs.
The “S” drawn on the thoracic cage outlines the lymphatic distribution of the lungs, starting in the pleura involving the lymphatic system in the pleura, interlobular septa, bronchovascular bundles and lymph nodes.
The granulomas start out as micronodules and there is a tendency for these to coalesce, sometimes forming large granulomatous masses
When the disease affects the interlobular septa, it causes thickening and nodularity in the septa of the secondary lobule.
When it involves the lymphatics in the pleura or fissures it causes nodularity and thickening.
When it involves the lymphatics around the terminal bronchioles it results in centrilobular micronodules, and when it involves the larger airways it causes thickening and nodularity
Lymph nodes in the hila are characteristically large and flesh like (sarcoid = meat) The Pawnbrokers sign (aka Garland sign or the 1,2,3 sign) describes the enlarged right paratracheal node with bilateral hilar adenopathy.
Parenchymal nodules and micronodules sometimes coalesce to form a central confluent mass with surrounding micronodules, described as the galaxy sign.
Ashley Davidoff MD TheCommonVein.net 132082-S06L
