Esophagram
- Findings: Identifies aspiration by visualizing contrast material entering the trachea or lungs. Detects structural abnormalities such as strictures, fistulas, or diverticula contributing to aspiration.
- Recommendations:
- Barium is not used in the esophagram when aspiration is considered because it can lead to severe lung inflammation, granuloma formation, and fibrosis if aspirated, resulting in chronic pulmonary complications.
- Avoid hyperosmolar contrast agents, including high-osmolar ionic agents such as diatrizoate meglumine or diatrizoate sodium (e.g., Gastrografin). These can rapidly draw fluid into the alveolar spaces, causing life-threatening pulmonary edema if aspirated.
- Use safer alternatives, such as:
- Non-Ionic, Low-Osmolar Contrast Agents (LOCM):
- Iohexol (e.g., Omnipaque)
- Iopamidol (e.g., Isovue)
- Ioversol (e.g., Optiray)
- Iopromide (e.g., Ultravist)
- Iomeprol (e.g., Iomeron)
- Iso-osmolar contrast agents (e.g., iodixanol)
- Iodixanol (e.g., Visipaque)
- These agents are preferred for patients with a risk of aspiration due to their lower irritative potential in the lungs and safer profiles compared to high-osmolar ionic agents. Iso-osmolar agents like iodixanol are particularly safe, as their osmolality closely matches that of human plasma.
- Modified Barium Swallow (MBS)
- Role: Evaluates swallowing mechanics and identifies aspiration during swallowing. Helps pinpoint the phase of swallowing (oral, pharyngeal, or esophageal) that leads to aspiration.
- Procedure: Involves ingestion of various consistencies of food and liquid mixed with barium under fluoroscopic imaging. Safe for patients with suspected aspiration as barium is administered in small, controlled amounts.
- Findings: Real-time visualization of barium entering the trachea or bronchial tree confirms aspiration. Identifies anatomical or functional abnormalities contributing to aspiration (e.g., poor epiglottic closure, delayed swallowing reflex).
- Differential Diagnosis
- Infectious pneumonias of other etiologies.
- Pulmonary edema.
- Hemorrhage.
- Atelectasis.
- Neoplastic processes.
- Recommendations
- Clinical Correlation: Assess history for risk factors such as dysphagia, altered consciousness, or recent vomiting.
- Imaging Follow-Up: Monitor resolution or progression of findings with serial imaging.
- Management:
- Treat underlying causes (e.g., swallowing therapy for dysphagia).
- Antibiotic therapy if bacterial infection is suspected or confirmed.
- Supportive care, including oxygen therapy and pulmonary hygiene.
- Use modified barium swallow for functional swallowing evaluation in appropriate cases.
- Key Points and Pearls
- Aspiration commonly affects dependent lung regions; imaging should focus on these areas.
- Modified barium swallow is an essential tool for identifying and evaluating aspiration risk.
- Avoid hyperosmolar contrast agents like Gastrografin (diatrizoate meglumine, diatrizoate sodium) in esophagrams when aspiration is suspected to prevent complications.
- Use non-ionic, low-osmolar, or iso-osmolar agents (e.g., iohexol, iodixanol) as safer alternatives.
- Early recognition and management are crucial to prevent complications such as abscess formation or chronic lung disease.
Barium Swallow Aspiration into the Trachea
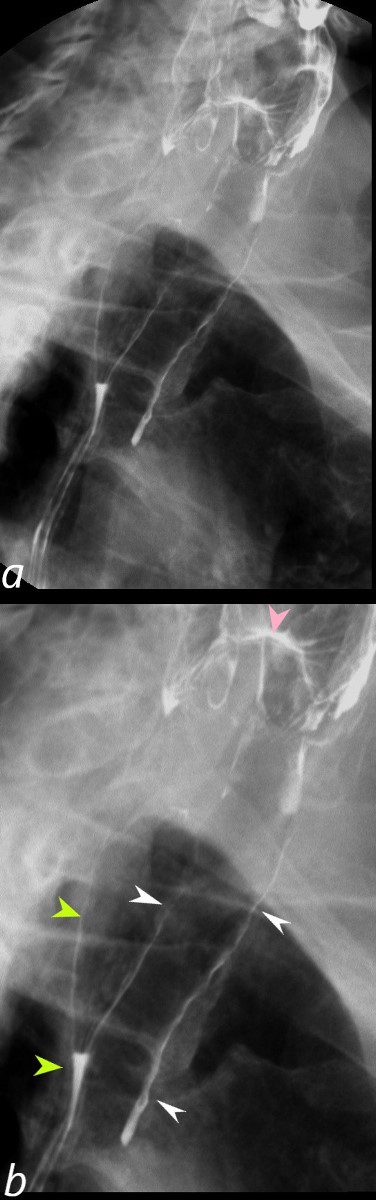
Barium swallow in the LPO projection shows abnormal accumulation of contrast along the walls of the trachea (b, white arrowheads) secondary to aspiration. Contrast also lines the wall of the posteriorly positioned esophagus (b, light green arrowheads) with a small air fluid level in the primary stripping wave of the esophagus (b, lower light green arrowhead). The contrast lined superior aspect of the epiglottis (pink arrowhead) is seen among the vallecula and pyriform sinuses.
Ashley Davidoff MD TheCommonVein.net 46505cL

CT of a 72-year-old male with acute dyspnea shows a focal accumulation of low-density aspirate in the right lower lobe. Distal to the obstruction the posterior segmental and medial segmental airways are patent, but associated atelectasis is noted in those segments of the right lower lobe. The esophagus is displaced to the right, and appears to contain some aerated content. There is atelectasis of the medial and posterior segments of the right lower lobe secondary to the aspiration
Ashley Davidoff MD TheCommonVein.net 136038
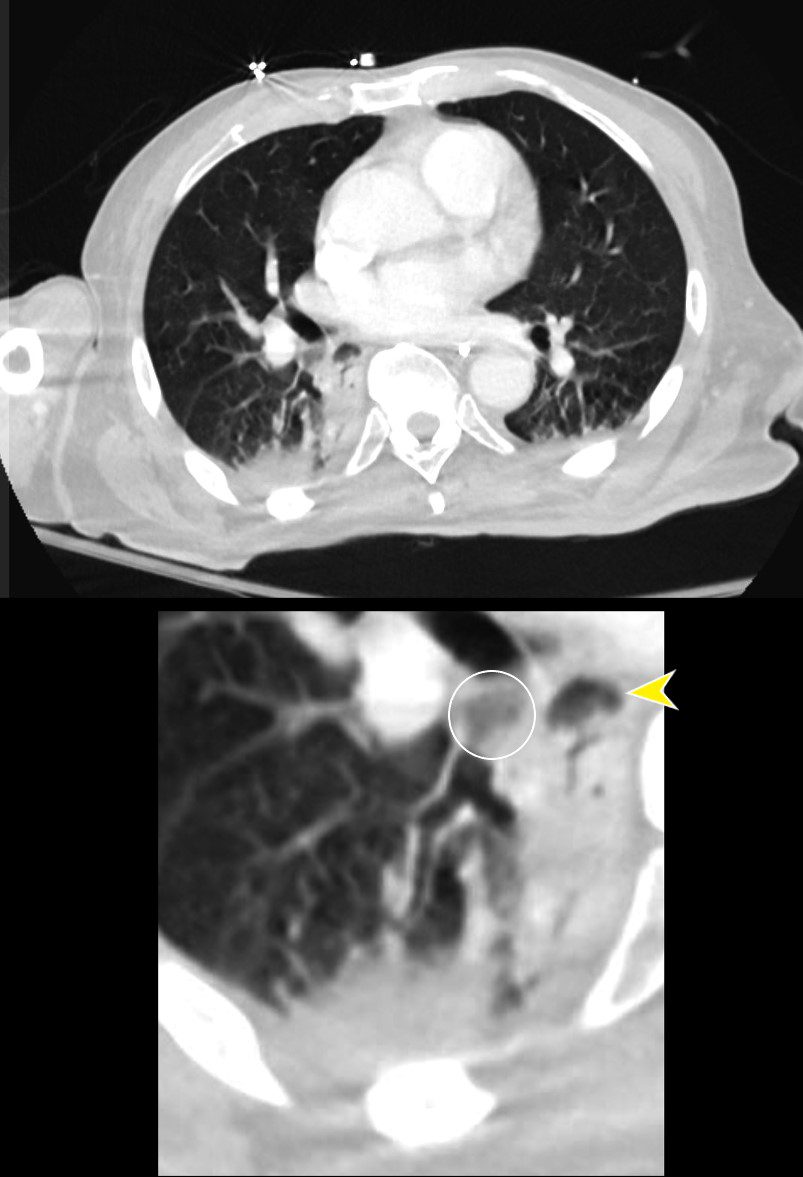
CT of a 72-year-old male with acute dyspnea shows a focal accumulation of low-density aspirate in the right lower lobe (white ring in lower image). Distal to the obstruction the posterior segmental and medial segmental airways are patent, but associated atelectasis is noted in those segments of the right lower lobe. The esophagus is displaced to the right and appears to contain some aerated content.
Ashley Davidoff MD TheCommonVein.net 136038cL
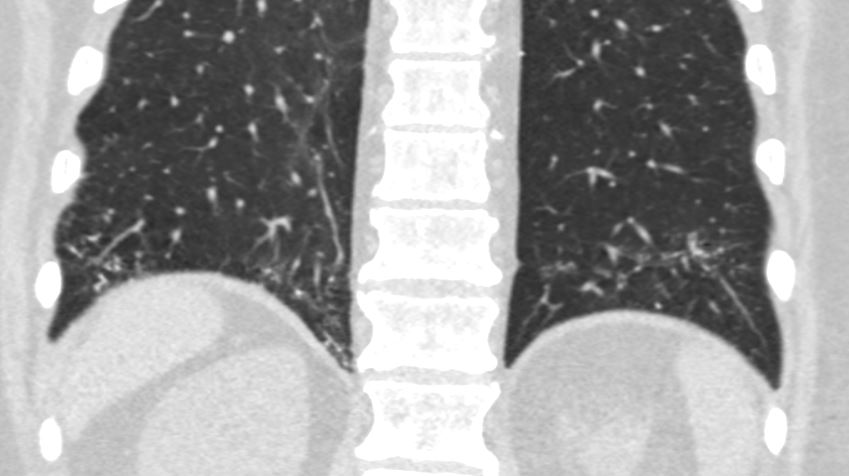
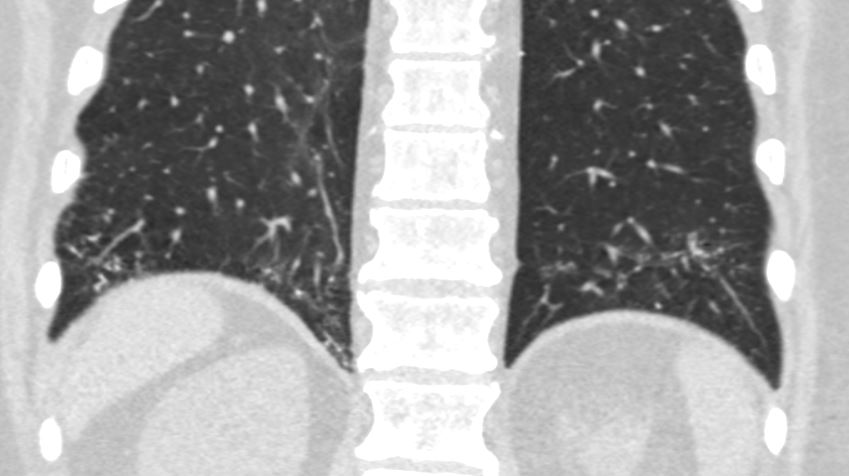
Bibasilar Aspiration Pneumonia with Occluded Right Main Stem Bronchus
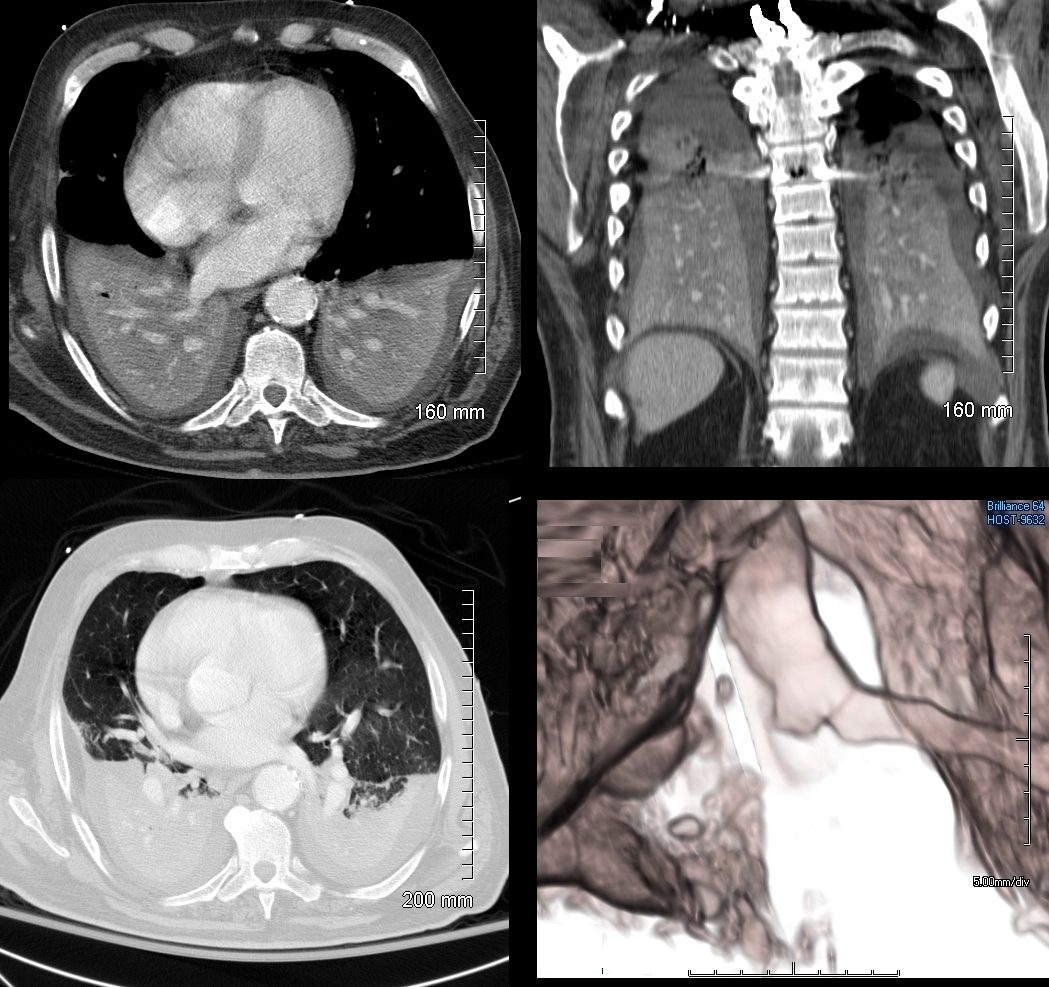
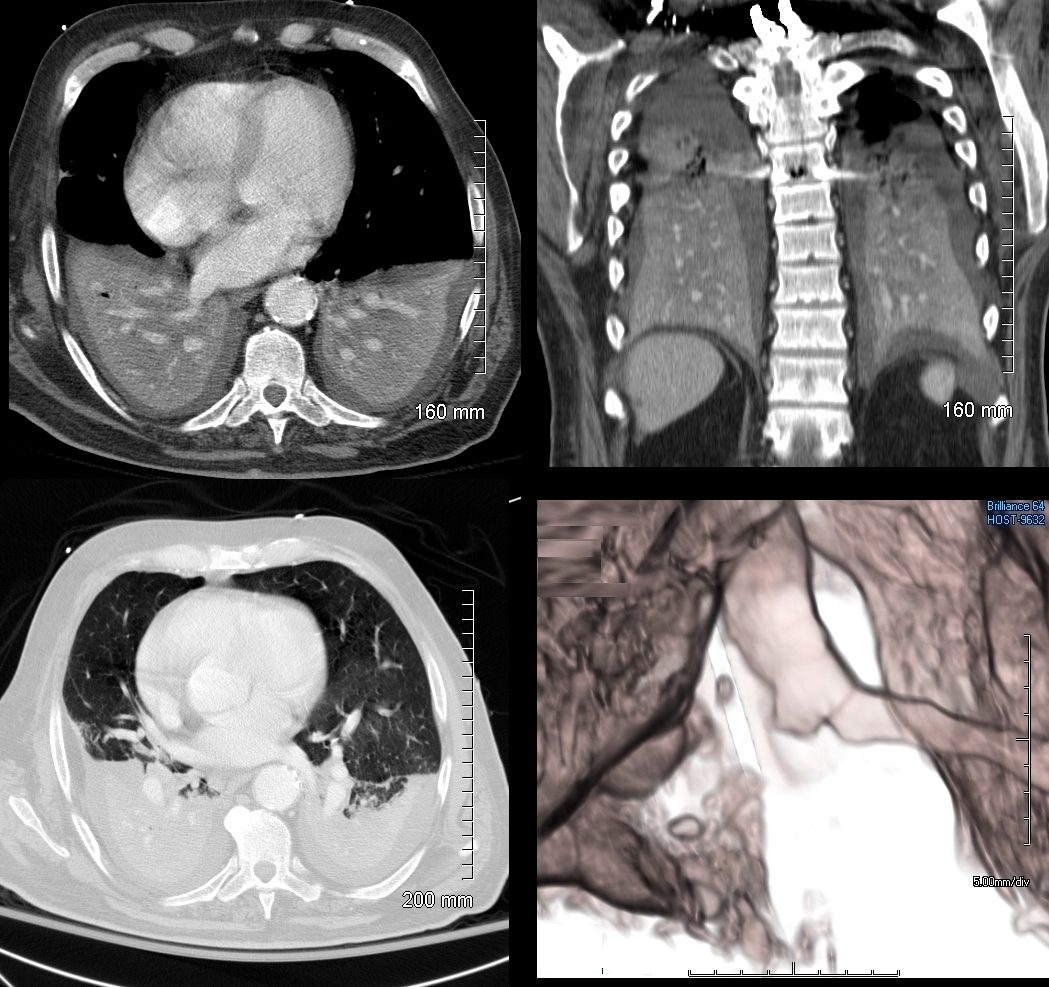
74 year old male alcoholic with bilateral basilar lobar atelectasis caused by bilateral aspiration
CT scan shows airless lower lobes with small bilateral effusions. 3D reconstruction shows total obstruction of the right mainstem bronchus, and patent proximal mainstem bronchus
Ashley Davidoff MD TheCommonVein.net
Bibasilar Consolidation Due to Aspiration
During A Seizure
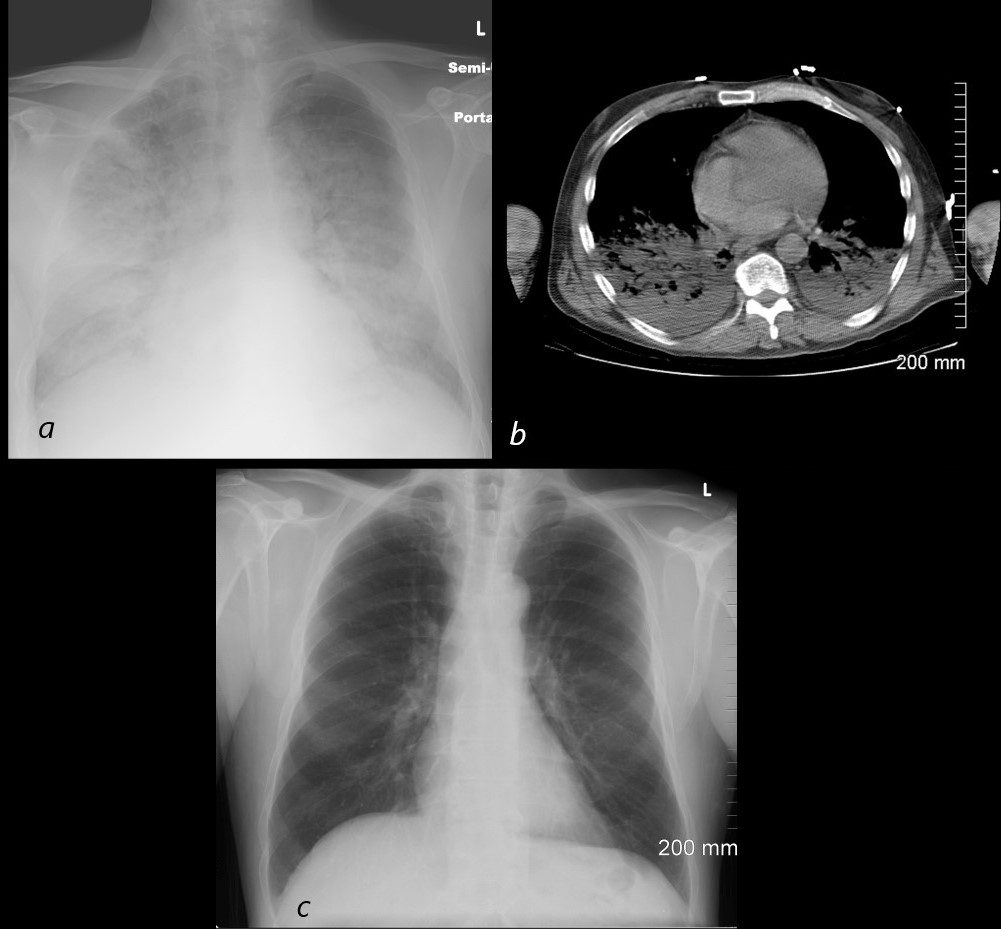
54 year old male alcoholic with seizures presents with diffuse alveolar disease consistent with pulmonary edema (a). CT scan (b) shows bibasilar infiltrates consistent with aspiration.
Follow up CXR 6 months later (c) shows resolution
Ashley Davidoff MD TheCommonVein.net
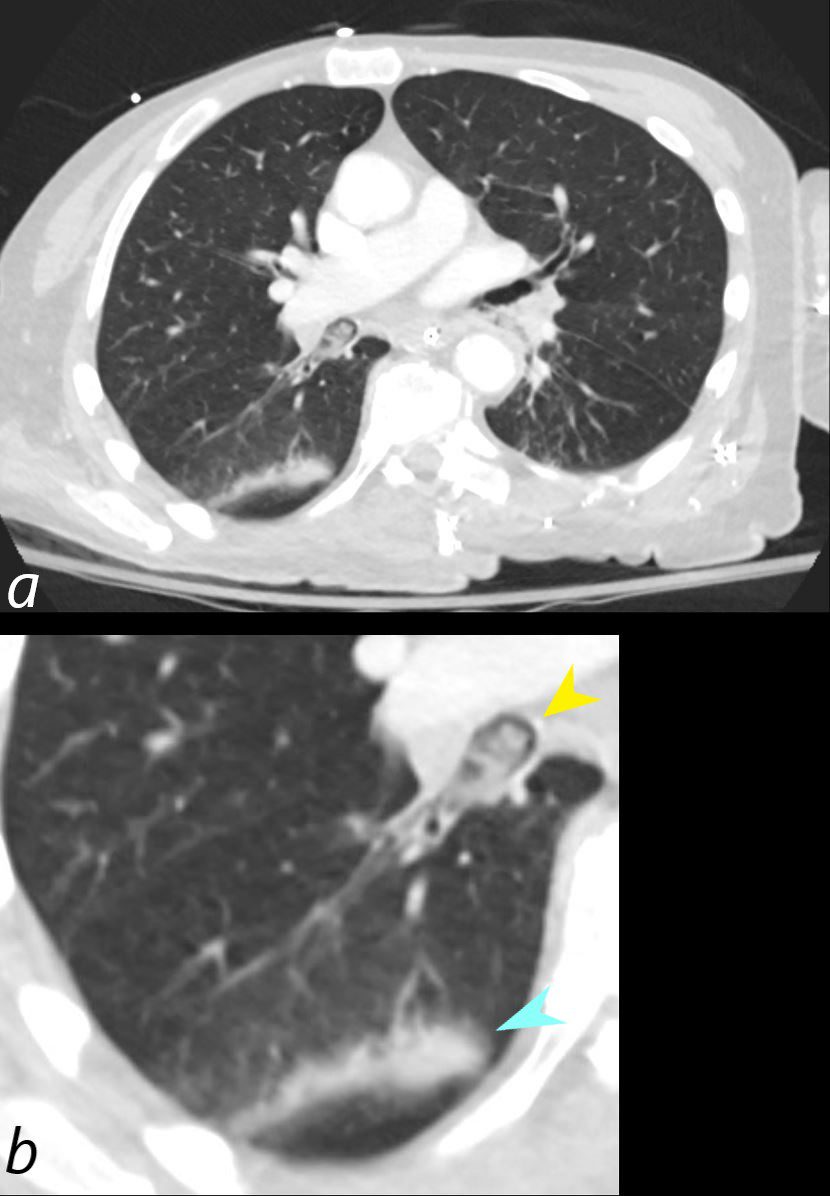
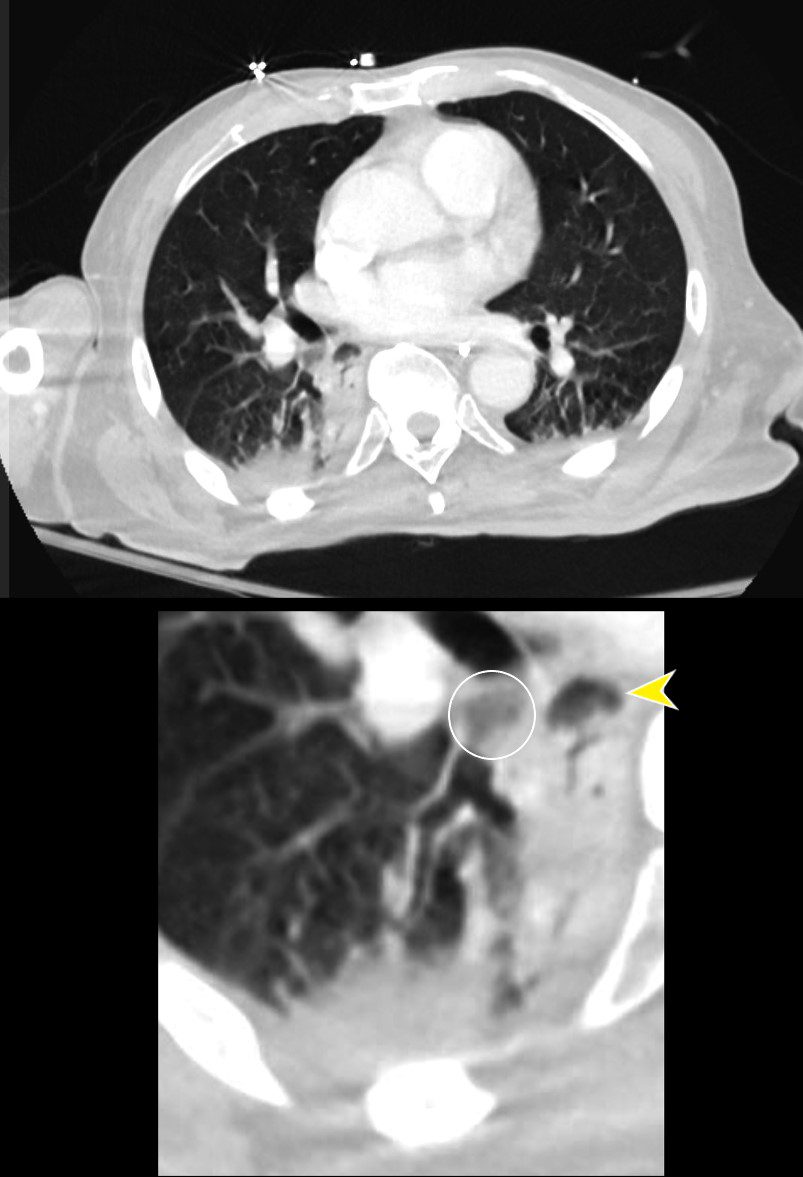
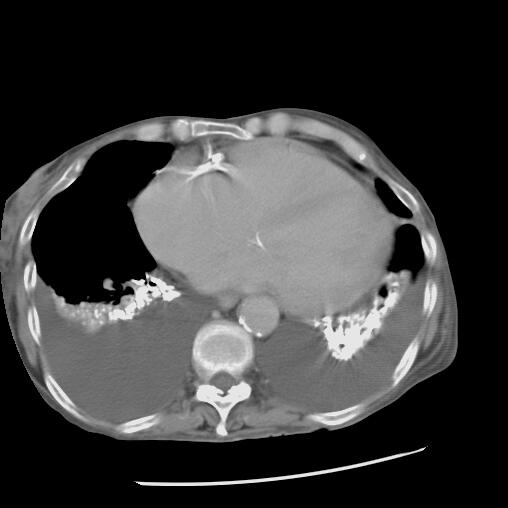
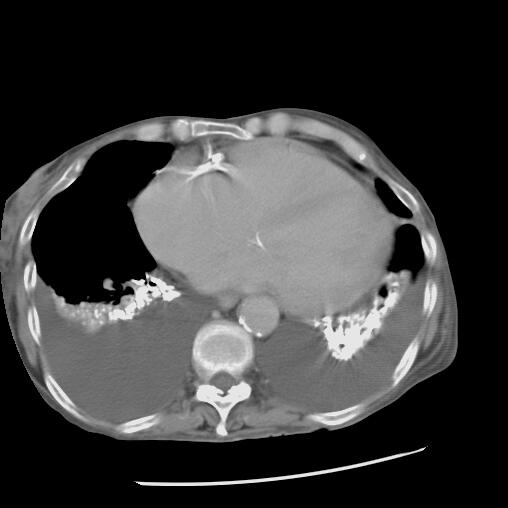
72-year-old male presents with acute dyspnea
Aspirate Occluding the Right Lower Lobe Bronchus


CT of a 72-year-old male with acute dyspnea shows a focal accumulation of low-density aspirate in the right lower lobe (white ring in lower image)
Ashley Davidoff MD TheCommonVein.net 136037c
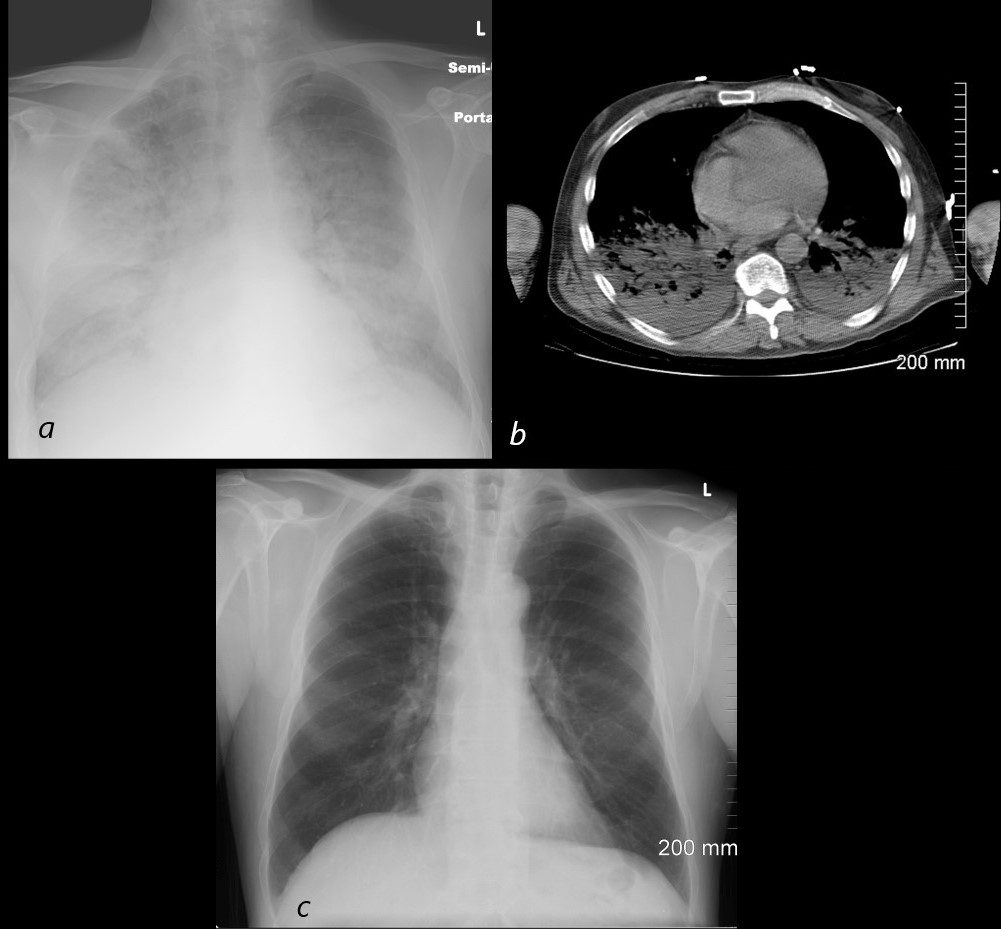
Aspirate Occluding the Right Lower Lobe Bronchus
Superior Segment Consolidation
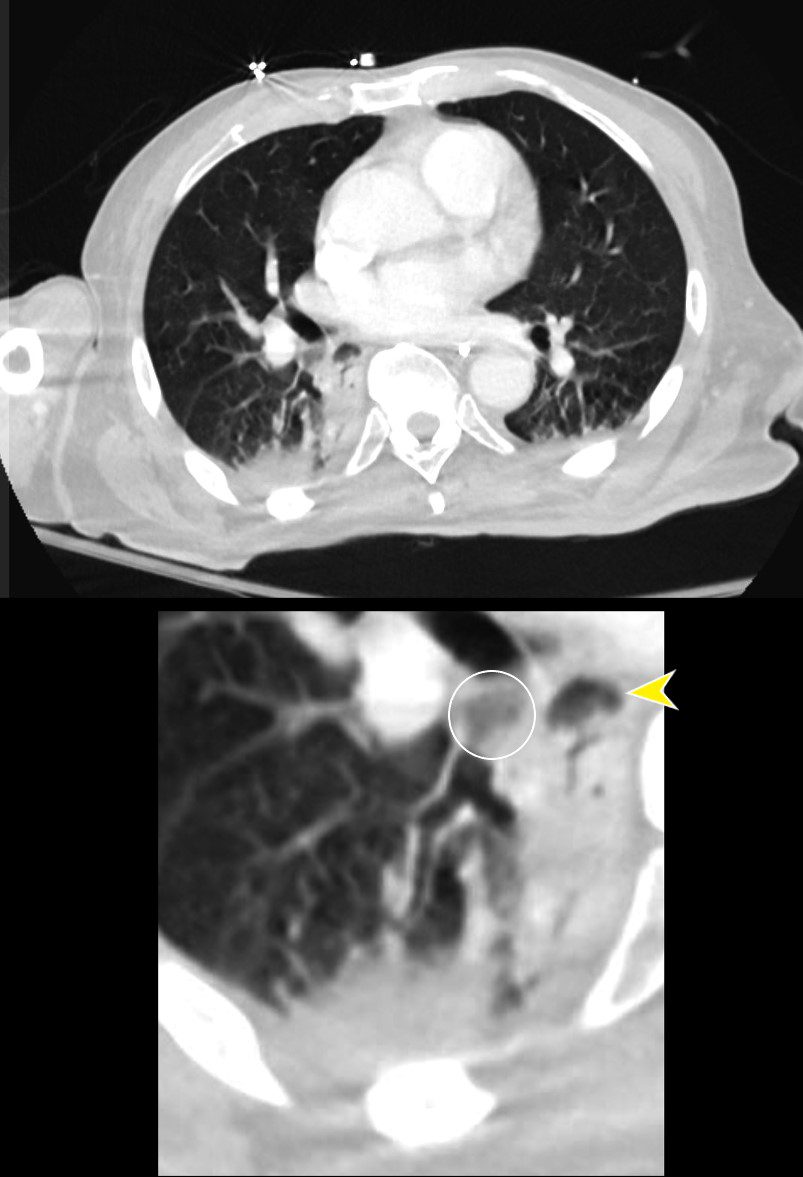
CT of a 72-year-old male with acute dyspnea shows a focal accumulation of low-density aspirate in the right lower lobe (white ring in lower image). Distal to the obstruction the posterior segmental and medial segmental airways are patent, but associated atelectasis is noted in those segments of the right lower lobe. The esophagus is displaced to the right and appears to contain some aerated content.
Ashley Davidoff MD TheCommonVein.net 136038cL
Aspirate Partially Occluding the Right Lower Lobe Bronchus and Extending into the Medial and Posterior Segments with Associated Atelectasis and Consolidation
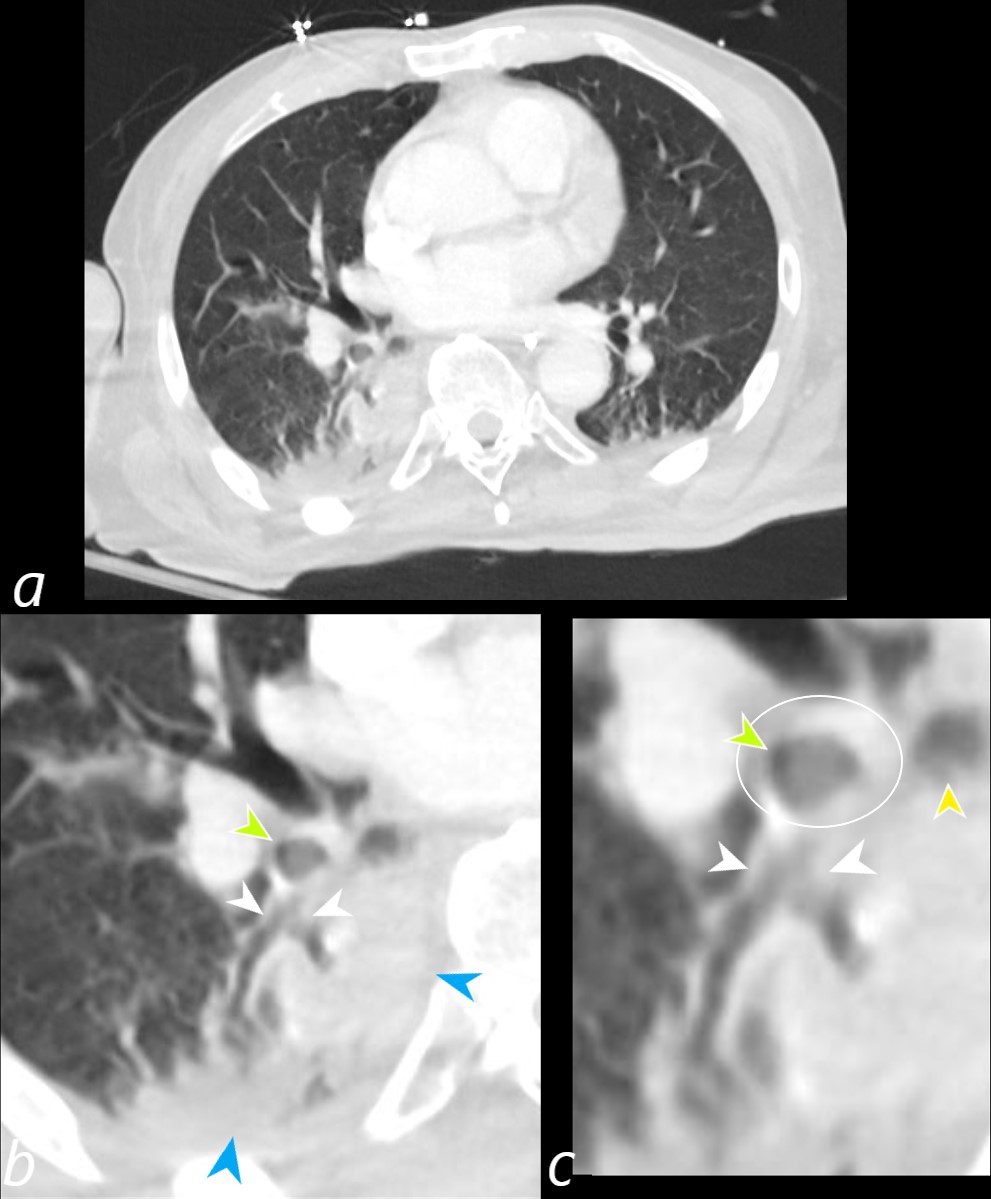
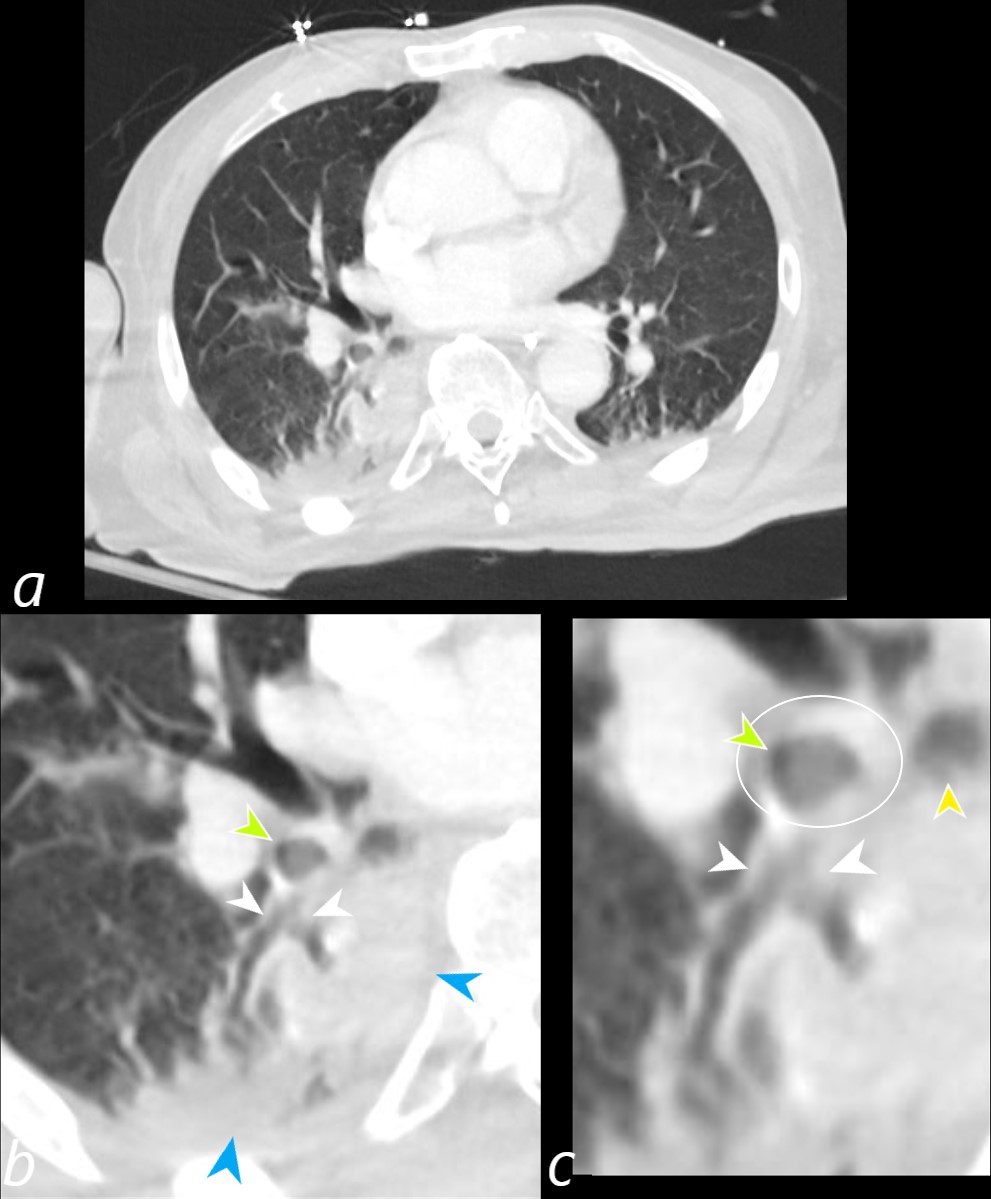
CT of a 72-year-old male with acute dyspnea shows a sub-totally occluded bronchus distal to the more complete obstruction noted in the previous section (green arrowheads b and c, and ringed in white in c). Distally at the branch point of the lower lobe bronchus there is partial filling of the medial and posterior segments (white arrows b and c). Secondary to the aspiration there is post obstructive atelectasis of the medial and posterior segments of the right lower lobe. The esophagus is displaced to the right, and appears to contain some aerated content (yellow arrowhead c).
Ashley Davidoff MD TheCommonVein.net 136041cL
Previously Aspirated Barium
Axial CT through the mid chest shows bibasilar high density barium in atelectatic lung consistent with barium aspiration. There are associated moderately large bilateral pleural effusions causing compressive atelectasis
Ashley Davidoff MD TheCommonVein.net 18243
Aspiration and Tree in Bud


87 year old male with history of cough and suspicion of aspiration shows barium aspiration into the proximal trachea (upper right) The scout view ( upper right) shows an infiltrate at the right base, Thickened airways in the right lower lobe (2nd row left ) is associated with a pneumonic infiltrate in the right lower lobe (lower right) consistent with aspiration. There are thickened airways to the lingula (3rd and 4th row) with magnified view showing tree in bud changes (right sided images 3rd and 4th row)
All these finding likely relate to spiration though lingula involvement is not usual
Ashley Davidoff MD Ashley Davidoff MD TheCommonVein.net 30602d04c01
Tree in Bud


Ashley Davidoff MD TheCommonvein.net


Ashley Davidoff MD TheCommonvein.net
Chronic Recurrent Aspiration
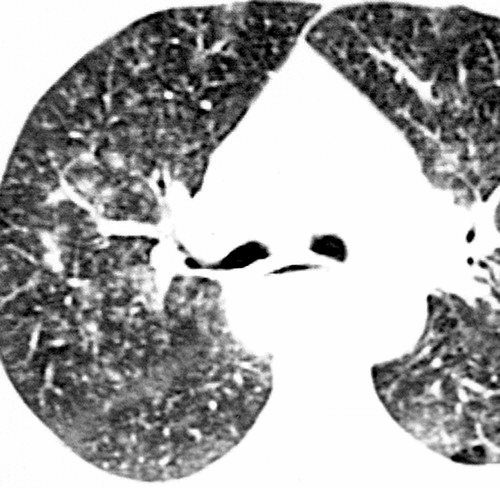
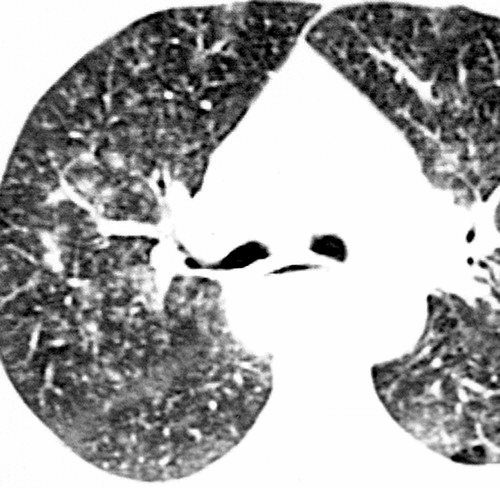
Rossi, SE et al Tree-in-Bud Pattern at Thin-Section CT of the Lungs: Radiologic-Pathologic Overview RadioGraphics Vol. 25, No. 3 2005


Ashley Davidoff MD The CommonVein.net
Ashley Davidoff MD The CommonVein.net
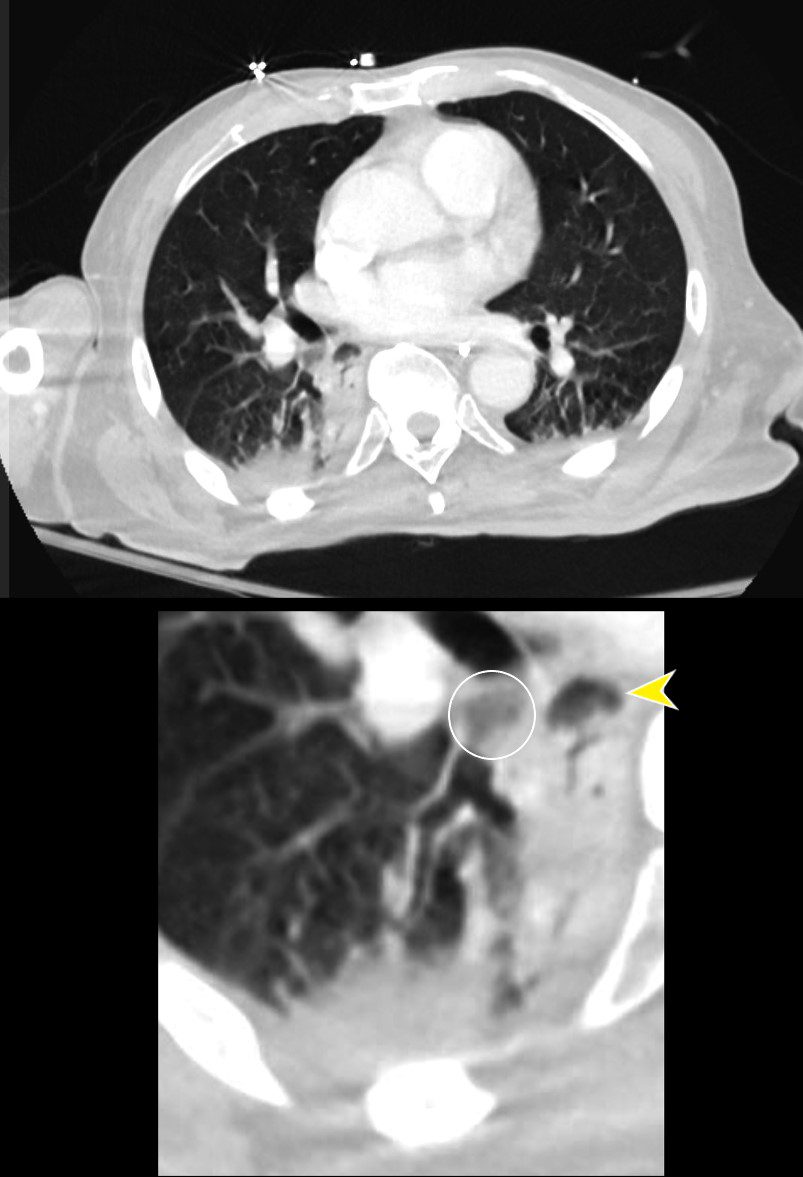
Aspiration from a Esophageal to Bronchial Fistula in a Patient with Esophageal carcinoma and a Stent
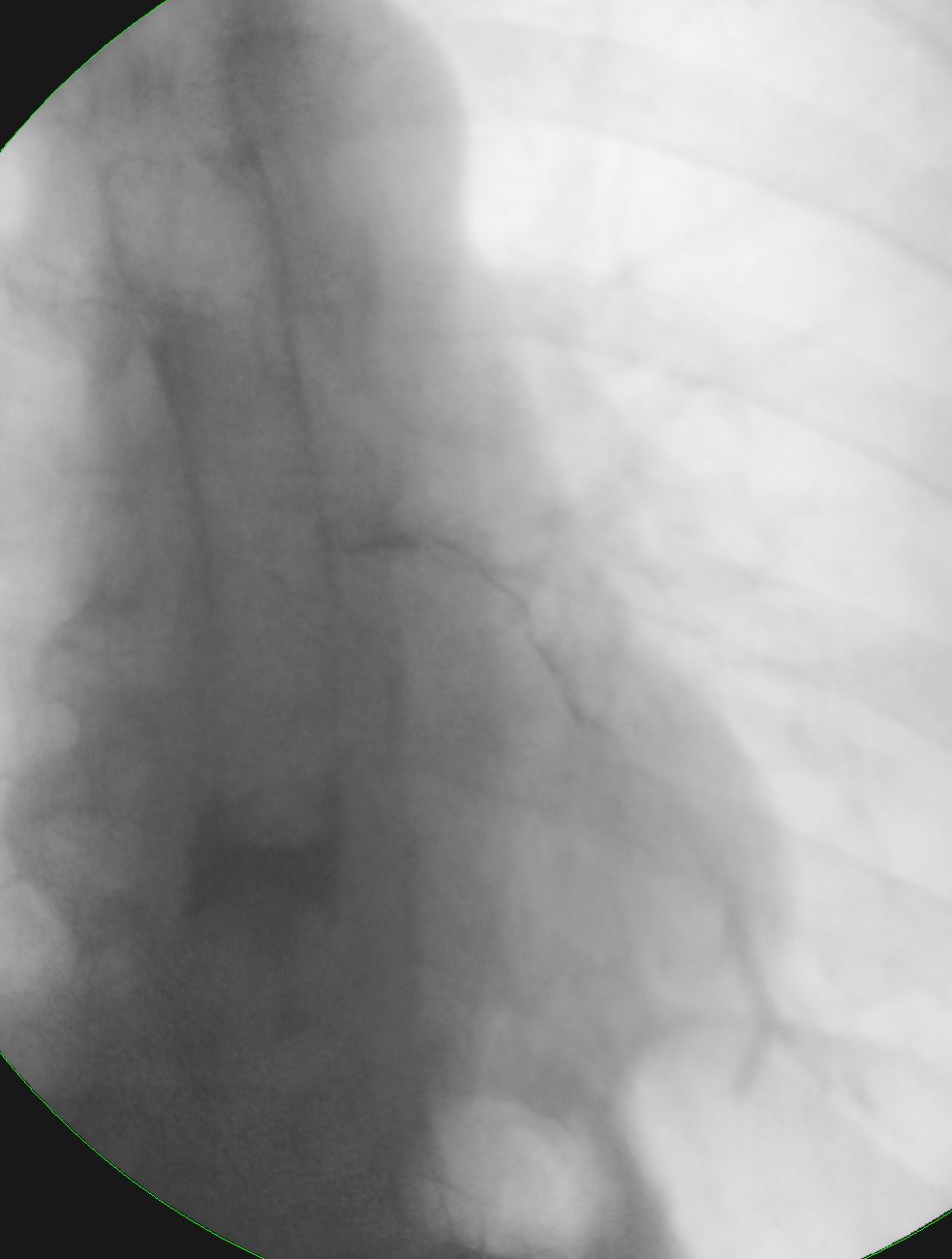
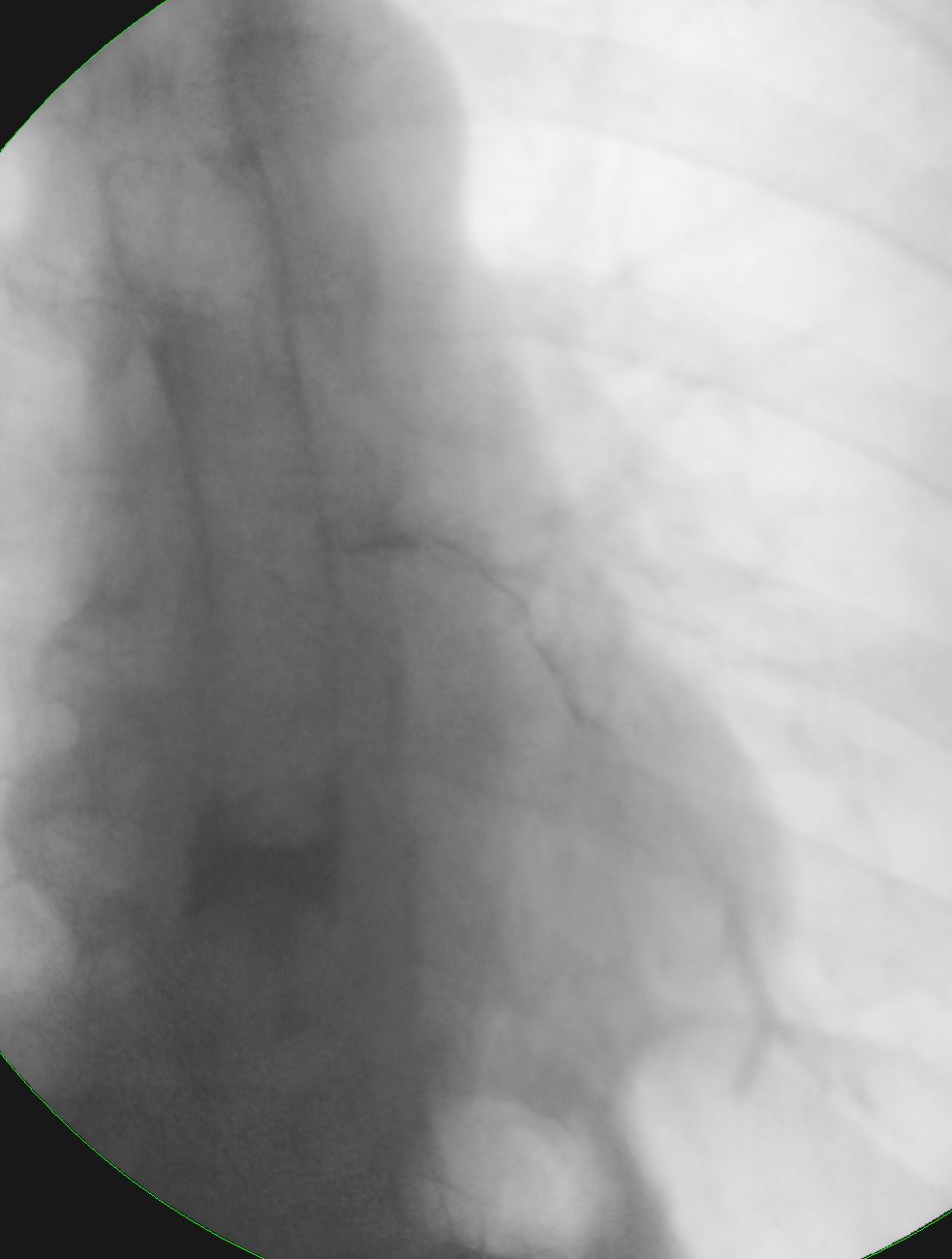
Ashley Davidoff MD TheCommonVein.net squamous-cell-carcinoma-001
Ashley Davidoff MD TheCommonVein.net squamous-cell-carcinoma-002


Ashley Davidoff MD TheCommonVein.net squamous-cell-carcinoma-003