-
Etymology
- Derived from the Greek words ateles, meaning “incomplete,” and ektasis, meaning “expansion,” referring to incomplete expansion or collapse of the lung.
AKA
- Collapsed lung (partial or complete)
Definition
What is it?
- Atelectasis refers to the partial or complete collapse of lung tissue, resulting in reduced or absent air in the affected alveoli and compromised gas exchange.
Caused by
- Obstruction of the airways (e.g., mucus plug, tumor).
- Compression of lung tissue (e.g., pleural effusion, pneumothorax).
- Loss of surfactant in conditions like acute respiratory distress syndrome (ARDS).
- Reduced ventilation due to shallow breathing or prolonged immobility.
Resulting in
- Alveolar collapse and reduced lung volume.
- Hypoxemia due to ventilation-perfusion mismatch.
Structural Changes
- Collapsed alveoli and thickened interstitial spaces.
- Mediastinal or diaphragmatic shifts toward the collapsed region in significant cases.
Pathophysiology
- Atelectasis occurs when alveoli lose the ability to remain inflated, leading to their collapse.
- Obstructive atelectasis: Airway blockage prevents air from reaching alveoli, which subsequently collapse as trapped air is absorbed.
- Compressive atelectasis: External pressure on the lung (e.g., pleural effusion, mass) forces alveoli to collapse.
- Adhesive atelectasis: Loss of surfactant reduces alveolar surface tension, causing collapse.
- Cicatricial atelectasis: Fibrosis of lung tissue leads to irreversible shrinkage and collapse.
- Relaxation (Passive) Atelectasis:Caused by a loss of contact between the visceral and parietal pleura (e.g., pneumothorax, large pleural effusion).
- Rounded (Subpleural) Atelectasis:Typically associated with pleural thickening or fibrosis, often seen in asbestos-related disease.
- Linear or Discoid Atelectasis:Characterized by thin, plate-like areas of subsegmental collapse, often seen in the dependent lung regions, typically caused by hypoventilation or postoperative states.
Pathology
- Collapsed alveoli with varying degrees of interstitial thickening and inflammation, depending on the cause.
Radiology in Detail
Air Bronchograms in Atelectasis
Presence and Absence of Air Bronchograms
- Present when:
- The bronchi remain patent (not obstructed) and surrounded by collapsed alveoli.
- Obstructive atelectasis occurs distal to a blockage but spares the proximal airways.
- Conditions such as passive (compressive) atelectasis and adhesive atelectasis.
- Absent when:
- The bronchi themselves are obstructed, such as in complete proximal airway blockage (e.g., tumor or mucus plug).
- The collapsed region is filled with fluid, pus, or tumor cells (e.g., in a completely consolidated lung or massive pleural effusion).
- Advanced fibrosis obliterates the airway architecture (e.g., cicatricial atelectasis).
Distinction from Consolidation
- In Atelectasis:
- Air bronchograms result from collapsed alveoli around patent airways.
- The air bronchograms often have a sharp, hyperacute angles because the collapse pulls surrounding structures, leading to distortion of the bronchial orientation and sharper angles.
- The lung volume is reduced, leading to displacement of fissures and mediastinal shift toward the affected side.
- In Consolidation:
- Air bronchograms appear when the alveoli are filled with fluid, pus, or blood, and the airways remain patent.
- The bronchial geometry is preserved because there is no volume loss.
- The surrounding lung volume is typically normal or slightly increased.
Role of Geometry and Angles in CXR
- On CXR, the orientation of the airways provides clues to distinguish between atelectasis and other pathologies:
- In atelectasis, angles between bronchi become more acute due to compression caused by volume loss. Bronchi may appear narrowed or angular, reflecting the lung collapse.
- In consolidation, angles between bronchi are preserved, indicating the absence of volume loss.
CXR
Findings
- Increased opacity in the affected area.
- Volume loss with mediastinal or diaphragmatic shift toward the collapsed region.
- Air bronchograms:
- Present if bronchi remain patent.
- Angled or distorted in atelectasis due to surrounding structural shifts.
- Absent if the bronchi are obstructed or if the collapse is due to complete fluid or fibrotic obliteration.
Associated Findings
- Atelectasis may coexist with pleural effusions or masses contributing to collapse.
CT
Parts
- Affected alveoli, bronchi, and pleura.
Size
- Varies with the extent of atelectasis (segmental, lobar, or whole lung).
Shape
- Wedge-shaped or linear opacity in smaller atelectasis.
Position
- Dependent lung regions are often affected (e.g., lower lobes in bedridden patients).
- Involvement of specific regions (e.g., lingula, middle lobe) depending on the underlying cause.
Character
- Collapsed lung parenchyma with sharp demarcation in obstructive atelectasis.
- Rounded appearance in subpleural atelectasis.
- Linear or plate-like areas in discoid atelectasis.
Time
- Acute onset in conditions like mucus plugging or pneumothorax.
- Chronic in cicatricial or rounded atelectasis.
Associated Findings
- Pleural effusion or fibrosis in compressive atelectasis.
Other Imaging Modalities
MRI/PET CT/NM/US/Angio
- Ultrasound: Useful in identifying pleural effusion or diaphragmatic motion abnormalities.
- PET-CT: Evaluates metabolic activity to exclude malignancy in chronic atelectasis.
Key Points and Pearls
- Air bronchograms are variable in atelectasis and depend on the patency of the bronchi and the mechanism of collapse.
- In atelectasis, air bronchograms may appear angular or distorted due to volume loss and structural shifts, unlike in consolidation, where geometry is preserved.
- Recognizing the geometric distortion of airways on CXR is essential for differentiating atelectasis from consolidation or other opacities.
- The right middle lobe and lingula are commonly affected in obstructive atelectasis due to their narrow bronchial anatomy.
- Prevention with incentive spirometry, early mobilization, and airway clearance techniques is critical in at-risk patients.
Clarifying Consolidation vs. Ground-Glass Opacity (GGO) and Atelectasis
1. Ground-Glass Opacities (GGOs) and Consolidation
- Key distinction
Ground-glass opacities (GGOs) and consolidations are related but distinct imaging findings:- Consolidation: Complete filling of alveoli with material such as fluid, pus, blood, or cells, leading to loss of normal aeration. It results in a homogeneous increase in lung attenuation on CT, where the underlying lung architecture is obscured, and air bronchograms are typically visible.
- GGO: A partial filling of alveoli with fluid, inflammatory exudate, or interstitial thickening. On CT, GGOs appear as hazy areas of increased attenuation, where the underlying lung architecture remains visible.
- Air bronchograms in GGOs
GGOs can exhibit air bronchograms, especially when partial alveolar filling occurs, but this does not make GGOs synonymous with consolidation. The persistence of visible pulmonary vessels and interstitial structures within GGOs distinguishes them from true consolidation. - Key takeaway
GGOs are not considered consolidations because they represent incomplete alveolar filling and preserved underlying architecture, whereas consolidation represents complete alveolar filling with loss of architectural visibility.
2. Atelectasis and Consolidation
- Key distinction
Atelectasis and consolidation are also distinct processes, although they may share overlapping features such as air bronchograms:- Atelectasis: Collapse or loss of lung volume due to airway obstruction, compression, or decreased surfactant. Atelectasis results in increased lung density but is accompanied by volume loss, evidenced by displacement of fissures, crowding of vessels and bronchi, and mediastinal shift (if extensive).
- Consolidation: Involves alveolar filling without volume loss, usually caused by pathological substances rather than mechanical collapse.
- Air bronchograms in atelectasis
Air bronchograms may occur in atelectasis if the airways remain patent while the surrounding alveoli collapse. However, the presence of volume loss (e.g., retracted fissures) and other indicators distinguishes atelectasis from consolidation. - Key takeaway
Atelectasis is not considered consolidation. While both can show air bronchograms, consolidation is characterized by alveolar filling without volume loss, whereas atelectasis involves volume loss due to lung collapse.
Summary of Differences
- Ground-glass opacity: Partial alveolar filling; underlying architecture visible; not consolidation.
- Atelectasis: Volume loss due to lung collapse; not consolidation despite potential air bronchograms.
- Consolidation: Complete alveolar filling; increased attenuation with obscured architecture.
Key Points and Pearls
- Air bronchograms are not specific to consolidation and can appear in GGOs or atelectasis if airways remain patent.
- Differentiation between these entities relies on evaluating secondary features like lung architecture (visible in GGOs), volume changes (present in atelectasis), and extent of alveolar filling (complete in consolidation).

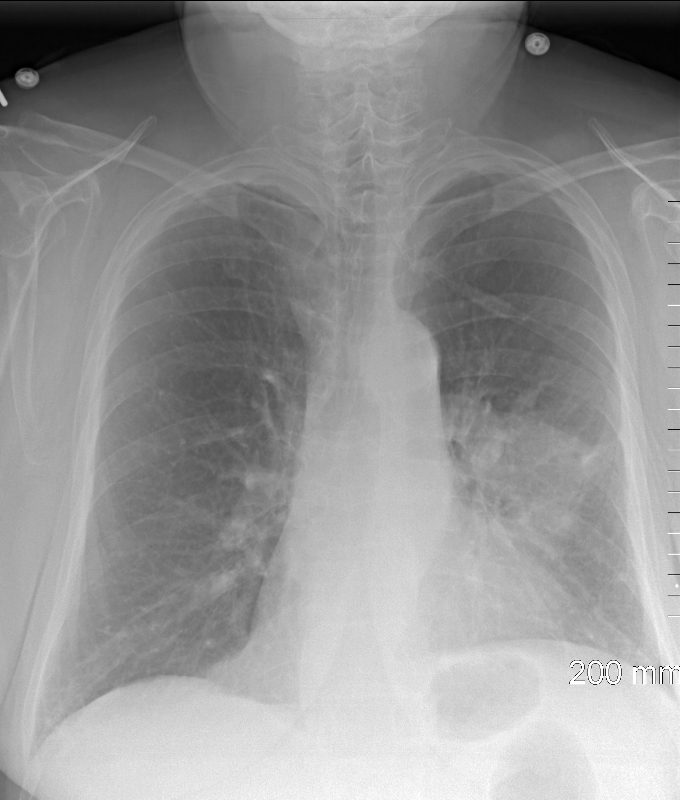
88 year old male with bilateral effusions shown on the CXR. Axial CT shows thickened pleura on the left with compressive atelectasis of the lower lobe and a smaller region of crescentic compressive atelectasis on the right. 3D reconstruction shows atelectasis of the left lower lobe and portion of the lingula
Ashley Davidoff MD TheCommonVein.net 74242b01d
- Caused by
- resulting in absence of air in the affected
- sub-segment
- segment,
- lobe
- lung
- When air does not fill the alveoli, the alveoli collapse.
- Diagnosed by
- stethoscope, percussion, x-ray, CT and bronchoscopy.
Radiological Features
- Chest X-Ray (CXR):
- Increased Opacity:
- Dense, homogenous opacification in the collapsed region.
-

Atelectasis of the Superior Segment of the Left Lower Lobe
72 year old female with left upper lobe mass 1 day after bronchoscopy which was complicated by lung collapse (atelectasis). The CXR has returned to baseline with segmental atelectasis caused by a left hilar mass. Note elevation of the left hemidiaphragm and crowding of the ribs reflecting the volume loss and confirming atelectasis
Ashley Davidoff MD TheCommonVein.net 134476.8
- Volume Loss Indicators:
- Shift of the mediastinum, trachea, or heart toward the affected side.
- Elevation of the hemidiaphragm on the affected side.
- Rib crowding over the collapsed region.
- Displacement of Structures:
- Hilum moves inferiorly (lower lobe atelectasis) or superiorly (upper lobe atelectasis).
- Air Bronchograms:
- Visible air-filled bronchi within the collapsed lung tissue.
- Increased Opacity:
- CT (High-Resolution CT – HRCT):
- Direct Signs:
- Crowded, collapsed lung parenchyma with increased attenuation.
- Wedge-shaped opacity, especially in lobar atelectasis.
- Indirect Signs:
- Volume loss and compensatory hyperinflation of adjacent lung segments.
- Displacement of fissures (e.g., major or minor fissures collapsing toward the atelectatic region).
- Pleural effusion or masses contributing to atelectasis.
- Air Bronchograms:
- Confirms that the airways remain open despite alveolar collapse.
- Direct Signs:
Types of Atelectasis
-
Post Obstructive (Resorbtive)
- Caused by
- complete obstruction
- neoplasm,
- mucus plugging
- foreign bodies
- complete obstruction
- Result
- air
- no new air can enter lung distal to the obstruction
- trapped air that is absorbed into the capillaries, l
- pleura
- cannot separate
- vacuum and
- traction of mediastinal structures and diaphragm
- mediastinal shift and elevated diaphragm
- air
-

CXR Right Upper Lobe Collapse Squamous Cell Carcinoma
55-year-old male presenting with dyspnea
Frontal CXR shows right upper lobe (RUL) atelectasis characterized by rightward deviation of the trachea elevation of the right hemidiaphragm and opacification of the right upper lobe. Final diagnosis was a central RUL proximal squamous cell carcinoma with extensive filling of the distal bronchi-ectatic segmental and subsegmental airways
Ashley Davidoff TheCommonVein.net 212Lu 136430
Lateral CXR Right Upper Lobe Collapse Squamous Cell Carcinoma
55-year-old male presenting with dyspnea
Lateral CXR confirms atelectasis of the RUL characterized by pie shaped consolidation of the anteriorly position right upper lobe, hyperinflation of the right lower lobe mild elevation of the right hemidiaphragm. Final diagnosis was a central RUL proximal squamous cell carcinoma with extensive filling of the distal bronchi-ectatic segmental and subsegmental airways
Ashley Davidoff TheCommonVein.net 212Lu 136430
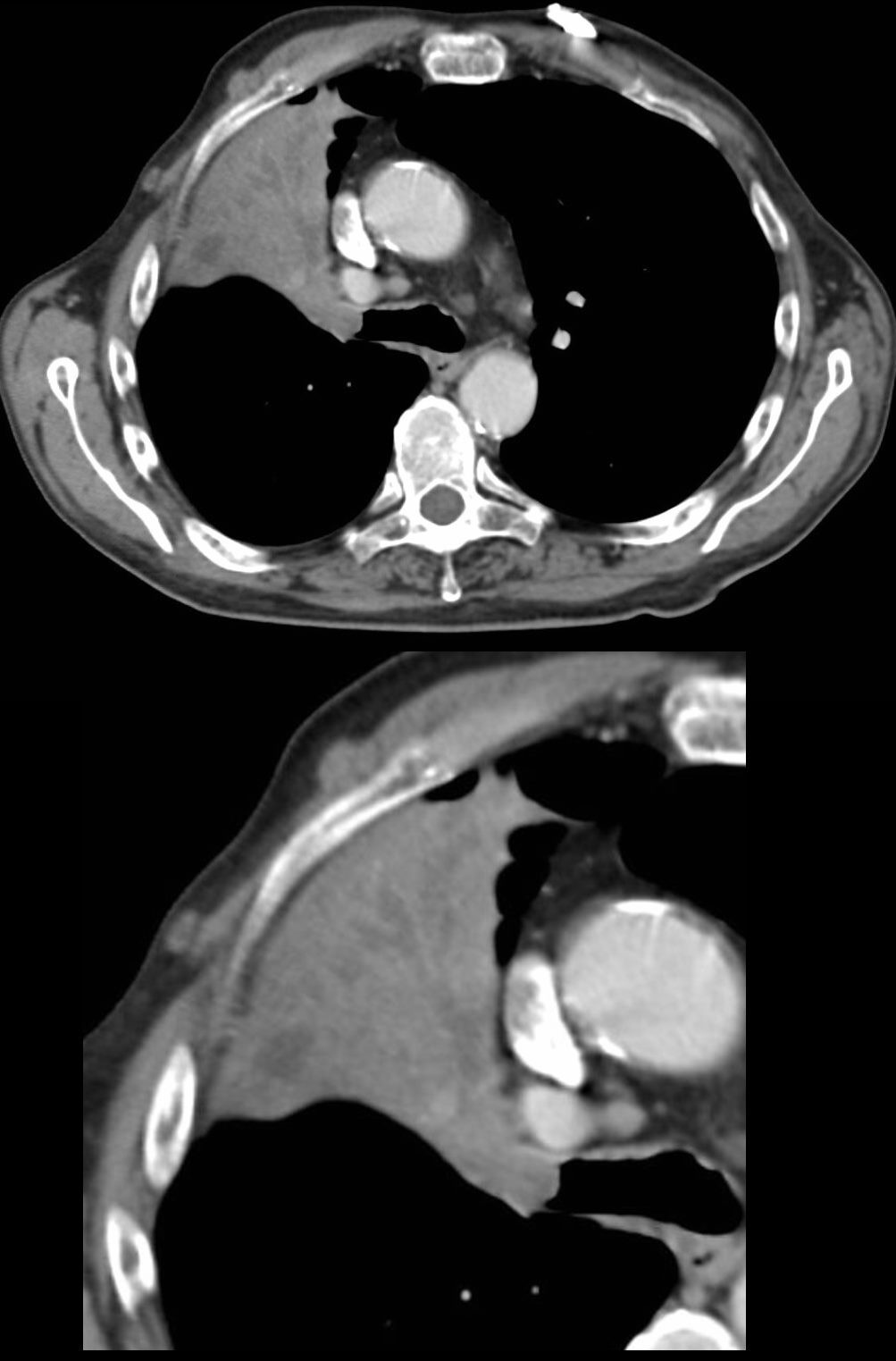
CT – Right Upper Lobe Collapse Central Squamous Cell Carcinoma
55-year-old male presenting with dyspnea
Axial CT at the level of the carina shows atelectasis of the RUL caused by a central obstructing lesion in the right upper lobe bronchus resulting in atelectasis of the RUL characterized by a wedge-shaped consolidation of the anteriorly positioned right upper lobe. The major fissure is displaced anteriorly. There is extensive filling of the distal bronchiectatic segmental and subsegmental airways of the RUL. Final diagnosis was a central RUL proximal squamous cell carcinoma.
Ashley Davidoff TheCommonVein.net 212Lu 136432c
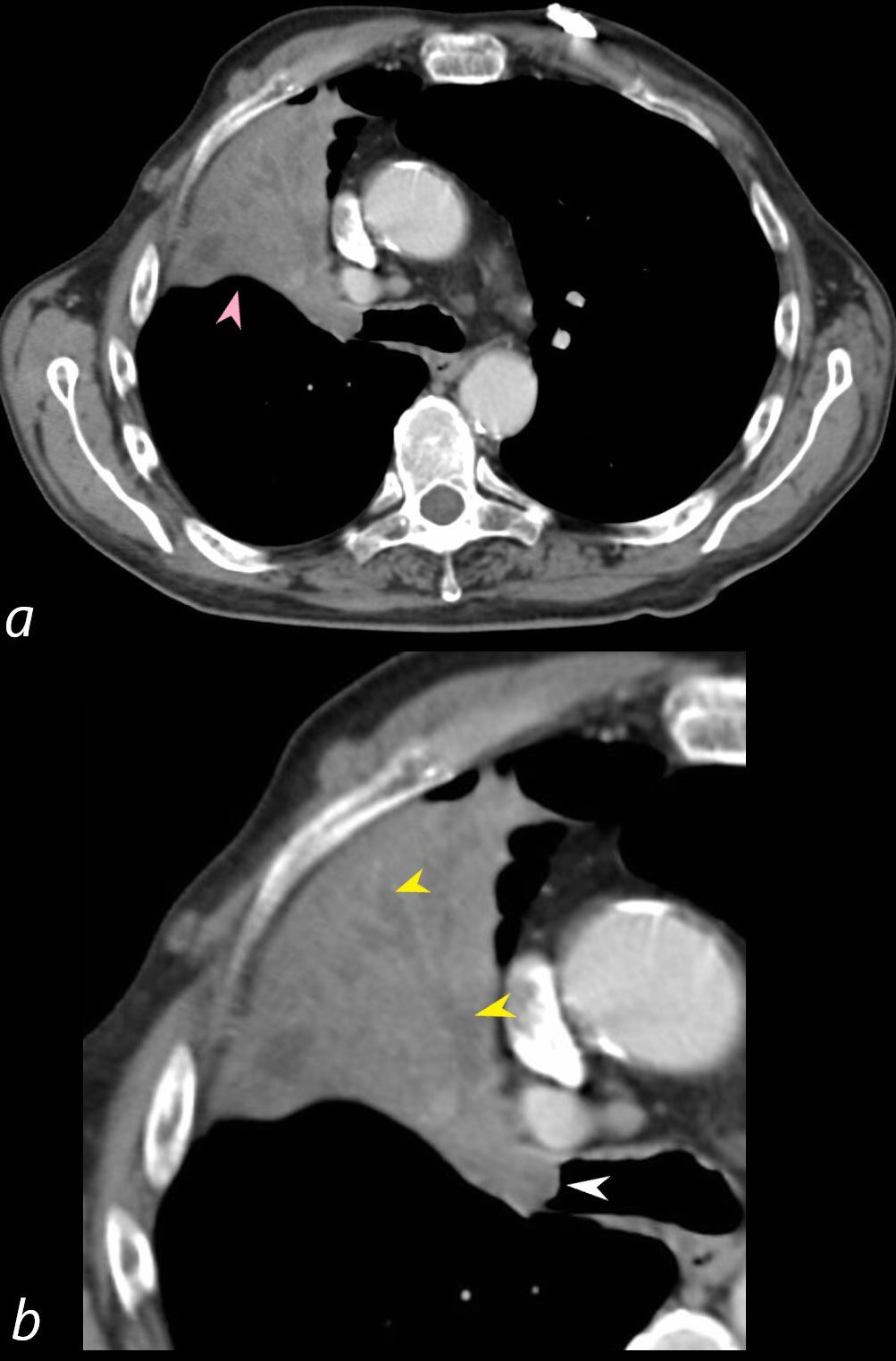
CT – Right Upper Lobe Collapse Central Squamous Cell Carcinoma
55-year-old male presenting with dyspnea
Axial CT at the level of the carina shows atelectasis of the RUL caused by a central obstructing lesion in the right upper lobe bronchus (b, white arrowhead) resulting in atelectasis of the RUL characterized by a wedge-shaped consolidation of the anteriorly positioned right upper lobe. The major fissure is displaced anteriorly (a, pink arrowhead). There is extensive filling of the distal bronchiectatic segmental and subsegmental airways of the RUL (b, yellow arrowheads). Final diagnosis was a central RUL proximal squamous cell carcinoma.
Ashley Davidoff TheCommonVein.net 212Lu 136432cL
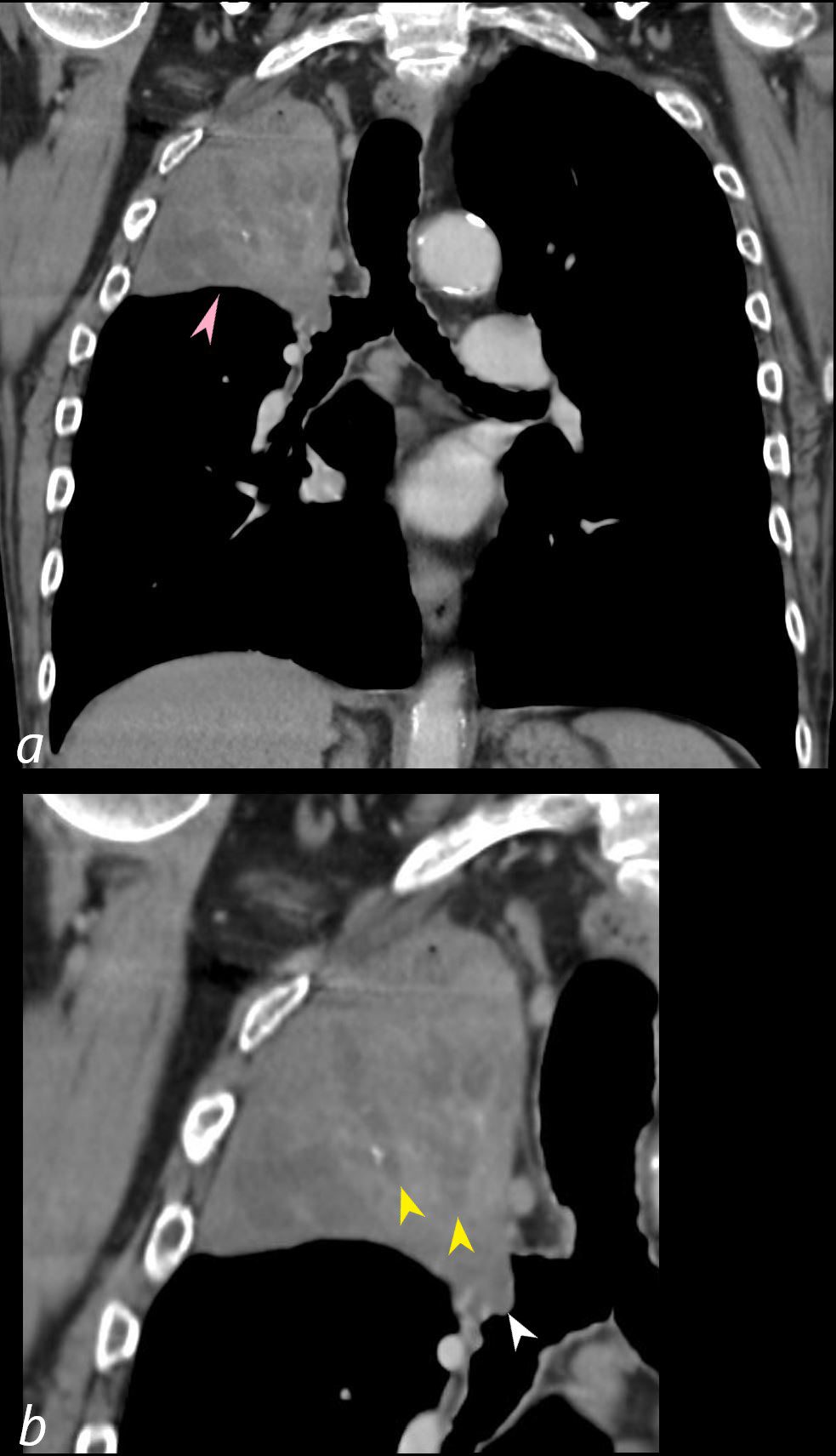
CT – Right Upper Lobe Collapse Central Squamous Cell Carcinoma
55-year-old male presenting with dyspnea
Coronal CT at the level of the trachea and mainstem bronchi, shows atelectasis of the RUL caused by a central obstructing lesion in the right upper lobe bronchus (b, white arrowhead) resulting in atelectasis of the RUL characterized by a wedge-shaped consolidation of the right upper lobe with superiorly displaced major fissure (a, pink arrowhead). There is extensive filling of the distal bronchiectatic segmental and subsegmental airways of the RUL (b, yellow arrowheads). Final diagnosis was a central RUL proximal squamous cell carcinoma.
Ashley Davidoff TheCommonVein.net 212Lu 136433cL
Endoscopy Central Obstructing Mass in the Right Upper Lobe Bronchus
Endoscopic image of a central squamous cell carcinoma (SCC) with extensive
Ashley Davidoff TheCommonVein.net 212Lu 136434
- Compressive Atelectasis
- Caused by
- pleural effusion,
- pneumothorax and
- diaphragmatic abnormality
- Result
- air
- squeezed out of lung
- pleura
- separated
- potentially only minor or no vacuum
-

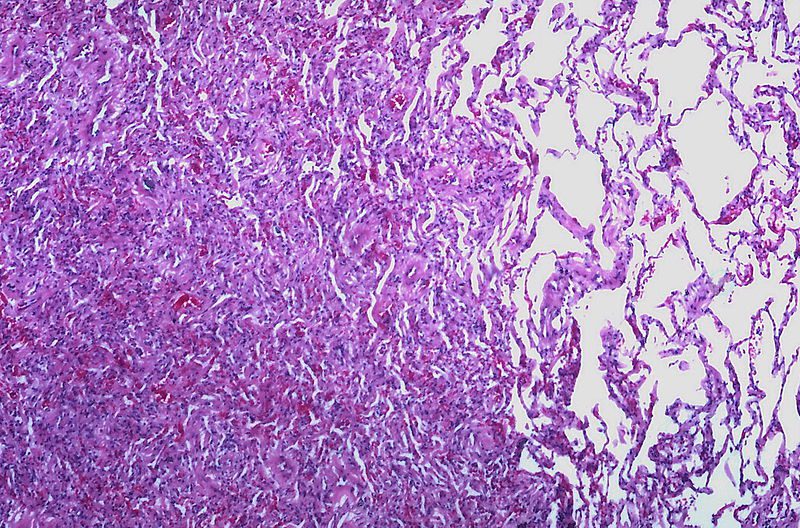
Compressive Atelectasis Secondary Effusion
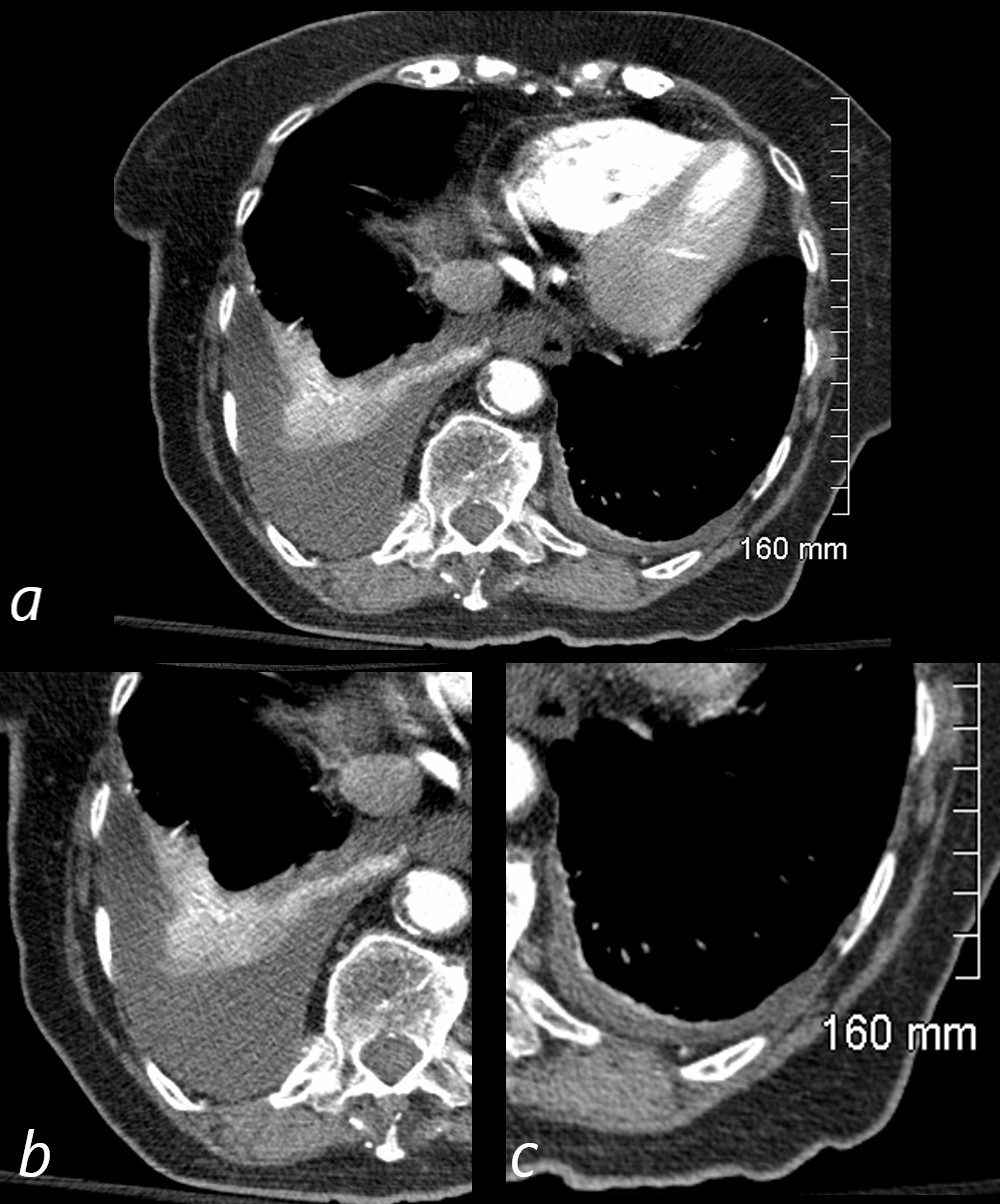
CT with Moderate Right Pleural Effusion, Small Left Effusion and Compressive Atelectasis
92-year-old female presents with dyspnea.
CT scan shows a moderate sized right pleural effusion with compressive atelectasis (magnified in b). There is relative hyperenhancement of the compressed and atelectatic lung due to increased tissue density. At the left lung base, there is a small effusion with a minor degree of atelectasis. (magnified in c)
Ashley Davidoff MD TheCommonVein.net 118437c01
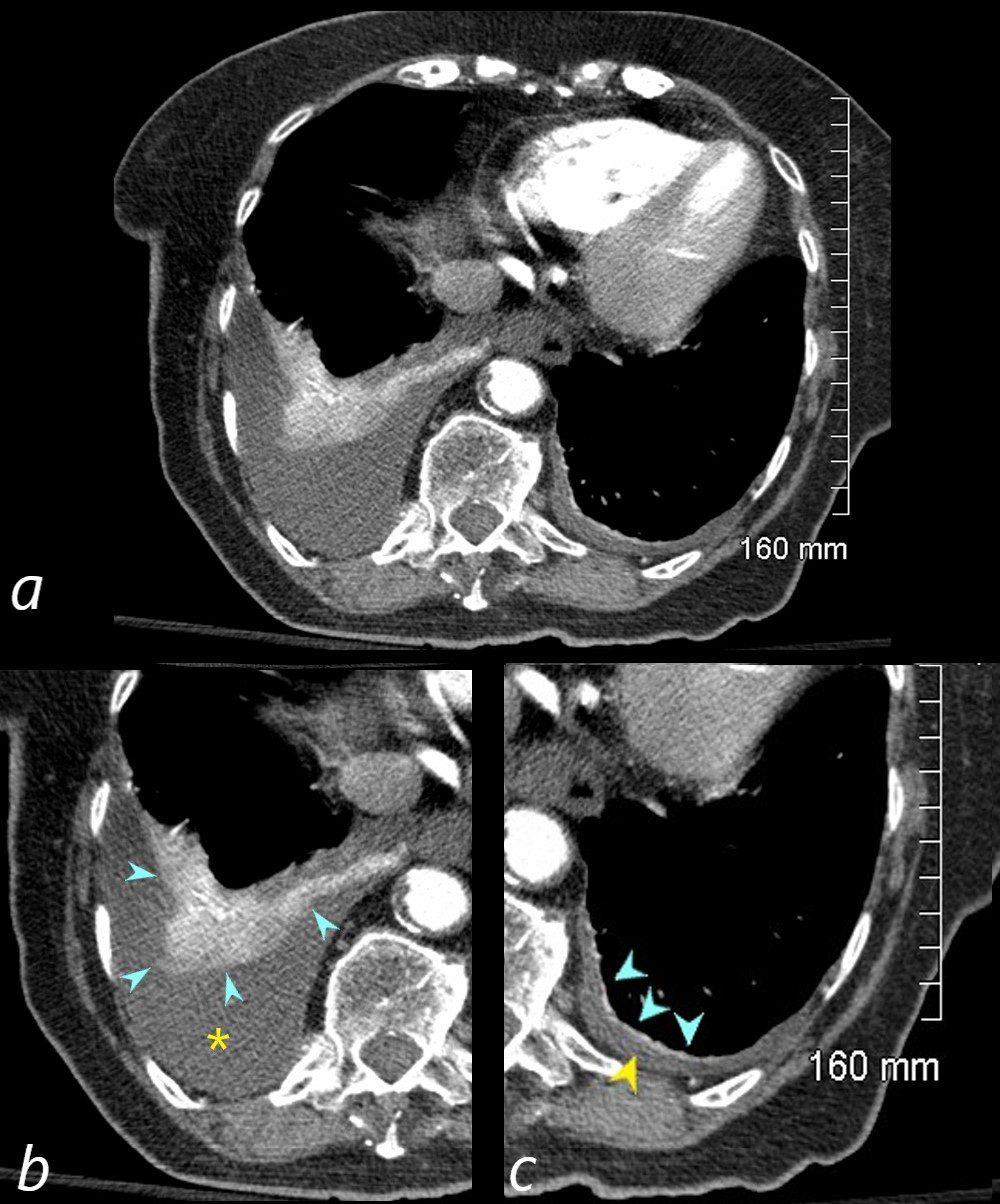
Compressive Atelectasis Secondary Effusion
CT with Moderate Right and Small Left Pleural Effusions with Compressive Atelectasis
92-year-old female presents with a dyspnea.
CT scan shows a moderate sized right pleural effusion , magnified in b (yellow asterisk ) with compressive atelectasis (teal arrowheads) . There is relative hyperenhancement of the compressed and atelectatic lung due to increased tissue density. In the left lower lung field , there is a small effusion (yellow arrowhead ,c) with a minor degree of compressive atelectasis (teal arrowheads, c )
Ashley Davidoff MD TheCommonVein.net 118437c01L
-
-

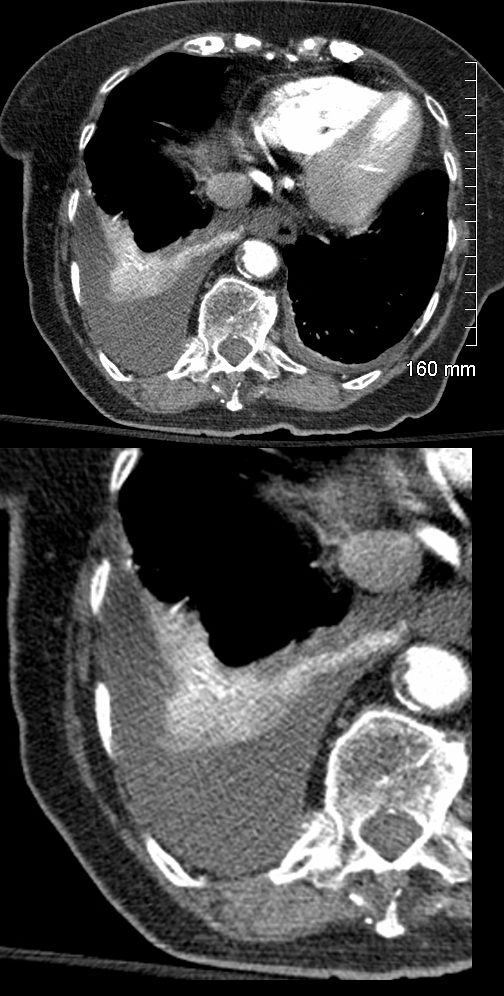
Compressive Atelectasis Secondary Effusion
CT with Moderate Right Pleural Effusion and Compressive Atelectasis
92-year-old female presents with a dyspnea.
CT scan shows a moderate sized right pleural effusion with compressive atelectasis and on the left, there is a small effusion with a minor degree of atelectasis. There is relative hyperenhancement of the compressed and atelectatic due to increased tissue density.
Ashley Davidoff MD TheCommonVein.net 118437c
- air
- Caused by
- Linear Discoid or Plate-Like Atelectasis
- Adhesive Atelectasis
- Caused by
- surfactant deficiency
- diffuse or
- localized
- surfactant deficiency
- Caused by
- (e.g., ARDS, neonatal respiratory distress syndrome).
- Radiology: Diffuse or patchy opacities without significant structural shifts.
- Caused by
- Cicatricial (Fibrotic) Atelectasis: aka Cicatrisation (Traction) Atelectasis
-
-
- Caused by
- graulomatous disease,
- necrotizing pneumonia and
- radiation fibrosis
- bronchietasis
- Result
- air
- lung cannot expand
- pleura
-
- cannot separate
- vacuum and
-
- traction on surrounding structures
Lung collapse due to scarring or fibrosis (e.g., post-tuberculosis, chronic inflammation).
- air
- Caused by
- Radiology: Dense, irregular opacities with volume loss and architectural distortion.
-
-
Gravity Dependent Atelectasis (Dependent Atelectasis)
-
-
- Caused by
- weight of the lungs
- Result
- Crescentic shaped
- ground glass changes
- Caused by
-
-
- Specific subtype associated with pleural diseases (e.g., asbestos exposure).
- Radiology: Curved opacity with a “comet-tail” sign (curved bronchovascular structures leading to the atelectatic area).
Common Locations and Patterns
- Lobar Atelectasis:
- Right middle lobe: Collapses medially, causing a triangular opacity on lateral CXR.
- Right lower lobe: Posterior triangular opacity with diaphragm elevation.
- Left upper lobe: Band-like opacity with leftward mediastinal shift.
- Segmental Atelectasis:
- Localized collapse of individual segments, often subtle on imaging.
Differential Diagnosis
Radiological findings of atelectasis can mimic other conditions:
- Pneumonia:
- Typically shows no volume loss or mediastinal shift.
- Pleural Effusion:
- Causes opacity but usually shifts structures away from the effusion.
- Mass or Tumor:
- May cause atelectasis but with focal mass effect or irregular borders.
Clinical Context and Imaging Role
- Atelectasis can be:
- Acute: Post-surgical, mucus plugging.
- Chronic: Fibrotic processes or prolonged obstruction.
- Radiology provides critical clues to identify the cause, extent, and impact of atelectasis and helps guide further interventions like bronchoscopy or drainage.
- Atelectasis implies collapse of part of the lung.
-
- Caused by
- resulting in absence of air in the affected
- sub-segment
- segment,
- lobe
- lung
- When air does not fill the alveoli, the alveoli collapse.
- Diagnosed by
- stethoscope, percussion, x-ray, CT and bronchoscopy.
File source: commons.wikimedia.org/
Types
-
-
-
-
- Result
-
- Osteophyte-Induced
- Caused by
- Result
- focal atelectasis
- fibrosis
- bronchiolectasis
Links and References
- TCV
- Discoid Atelectasis on CT

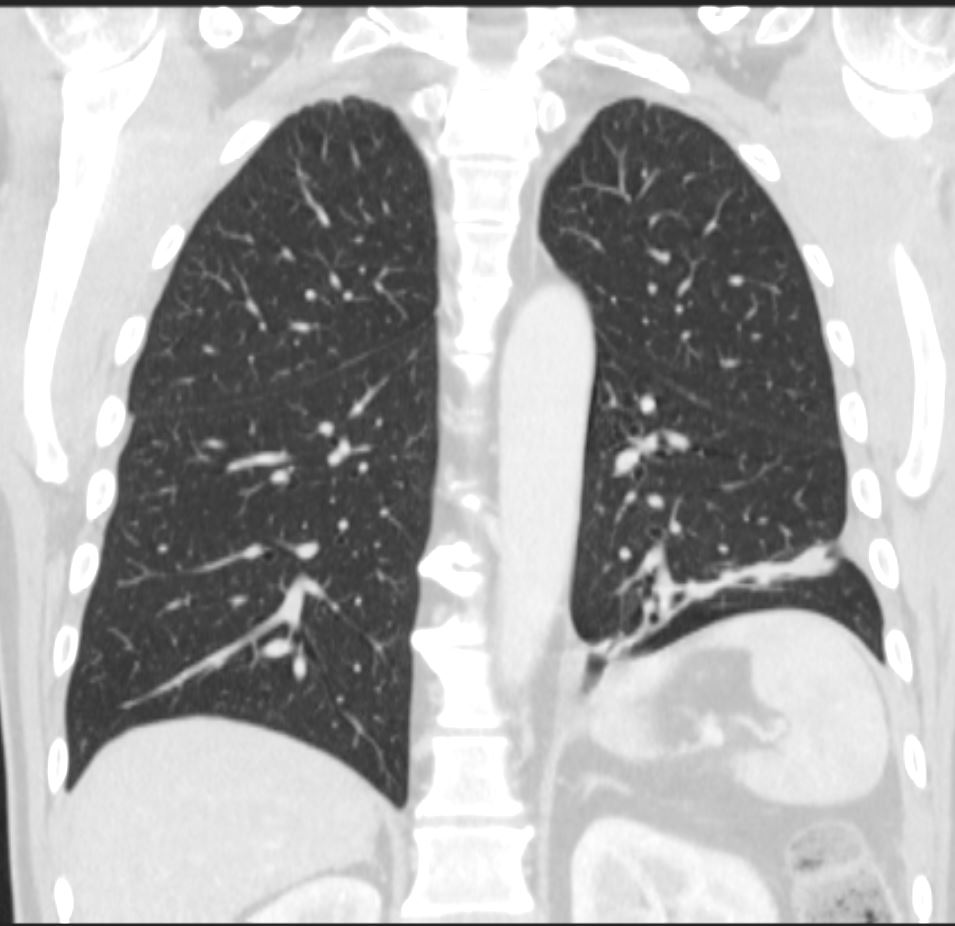
CT Linear Atelectasis 3 Months Later
CT scan in the coronal plane 3 months later shows significant improvement of the atelectasis involving a basal segment of the left lower lobe associated with persistent elevation of the left hemidiaphragm indicating volume loss. The atelectasis now has a discoid, linear, or plate-like appearance
Ashley Davidoff MD TheCommonVein.net 276Lu 136238
aka discoid atelectasis aka plate-like atelectasis
Links and References
TCV