Etymology
- Derived from the Greek words bronchion, meaning “small airway,” and -itis, meaning “inflammation.” The term refers to inflammation of the bronchioles.
AKA
- Small airway inflammation
What is it?
- Bronchiolitis is a clinical and radiological condition characterized by inflammation and injury to the bronchioles, the smallest airways in the lungs, leading to airway narrowing, obstruction, and impaired gas exchange.
Caused by:
- Most common causes:
- Viral infections (e.g., respiratory syncytial virus [RSV] in children)
- Post-infectious inflammatory response
- Less common causes:
- Infection:
- Mycoplasma pneumoniae
- Influenza virus
- Inflammation:
- Chronic inhalation of irritants (e.g., smoke, fumes)
- Hypersensitivity pneumonitis
- Immune:
- Rheumatoid arthritis-associated bronchiolitis
- Connective tissue diseases
- Neoplasm:
- Bronchiolar obstruction due to tumors
- Mechanical:
- Aspiration of foreign material
- Inflammation:
- Chronic bronchitis
- Connective tissue diseases (e.g., rheumatoid arthritis)
- Radiation-induced bronchiolitis
- Inherited and Congenital:
- Primary ciliary dyskinesia
- Alpha-1 antitrypsin deficiency
- Other:
- Drug-induced bronchiolitis (e.g., chemotherapy agents, amiodarone)
- Infection:
Resulting in:
- Airway narrowing and obstruction
- Impaired mucociliary clearance
- Reduced gas exchange efficiency
Structural Changes:
- Bronchiolar wall thickening
- Peribronchiolar inflammation
- Mucus plugging and potential fibrosis in chronic cases
Pathophysiology:
- Bronchiolitis develops when the bronchiolar epithelium is injured due to infection, inflammation, or other insults. This injury triggers an inflammatory response, leading to swelling of the bronchiolar walls, mucus production, and sometimes fibrosis. Air trapping and ventilation-perfusion mismatch may result, causing symptoms such as dyspnea and hypoxemia.
Pathology:
- Inflammatory infiltrates in and around bronchioles
- Mucus and cellular debris obstructing the lumen
- Fibrosis in chronic or recurrent cases
Diagnosis
Clinical:
- Symptoms vary based on etiology:
- Acute: Cough, wheezing, dyspnea, and fever
- Chronic: Persistent cough, dyspnea, and exercise intolerance
- Examination findings:
- Wheezing or crackles on auscultation
- Signs of hypoxemia in severe cases
Radiology:
- CXR:
- Hyperinflation, particularly in acute viral bronchiolitis
- Patchy areas of consolidation or atelectasis
- CT of the Chest:
- Tree-in-bud opacities in infectious or inflammatory bronchiolitis
- Mosaic attenuation indicating air trapping
- Bronchiolar wall thickening
Labs:
- Viral testing (e.g., RSV antigen)
- Sputum cultures for bacterial or fungal infections
- Autoimmune panels for connective tissue disease-associated bronchiolitis
Management:
- Acute bronchiolitis:
- Supportive care:
- Oxygen therapy for hypoxemia
- Hydration and fever management
- Antiviral or antibiotic therapy if indicated
- Supportive care:
- Chronic bronchiolitis:
- Address underlying cause (e.g., corticosteroids for autoimmune diseases)
- Bronchodilators for airway obstruction
- Smoking cessation and avoidance of irritants
- Immunizations (e.g., influenza, pneumococcal vaccines) for prevention
Radiology Detail
CXR
Findings:
- Hyperinflation and peribronchial cuffing
- Subtle patchy opacities in severe cases
Associated Findings:
- Atelectasis or small airway collapse
CT of the Chest
- High-resolution CT of the chest with inspiration and expiration can be used when small airway obstruction is suspected or for clarification of mosaic attenuation identified on conventional CT.
Parts:
- Terminal and respiratory bronchioles
Size:
- Bronchiolar walls appear thickened
Shape:
- Tree-in-bud opacities representing impacted bronchioles
Position:
- Distributed in the central or peripheral lung zones depending on etiology
Character:
- Irregular, nodular, or beaded bronchiolar patterns
Time:
- Acute or chronic, depending on the underlying cause
Associated Findings:
- Air trapping and mosaic attenuation in expiratory images
Other relevant Imaging Modalities
MRI/PET CT/NM/US/Angio:
- MRI: Rarely used but may assess associated soft tissue abnormalities
- PET-CT: Useful in identifying active inflammation or malignancy in atypical cases
Pulmonary Function Tests (PFTs):
- Obstructive pattern with decreased FEV1/FVC ratio
- Air trapping and reduced diffusion capacity in severe cases
Recommendations:
- CT of the Chest for detailed evaluation of bronchiolar changes
- Viral or autoimmune testing based on clinical suspicion
- Early intervention to prevent progression to chronic disease
Key Points and Pearls:
- Bronchiolitis refers to inflammation of the bronchioles and can present acutely (e.g., viral infections) or chronically (e.g., connective tissue diseases).
- CT of the Chest is the gold standard for identifying small airway changes, including tree-in-bud opacities and mosaic attenuation.
- Management includes supportive care, targeted therapy for underlying causes, and prevention through immunizations and avoidance of irritants.
- Types
- primary bronchiolar disease
- acute bronchiolitis
- usually viral infections,
- infants and children
-
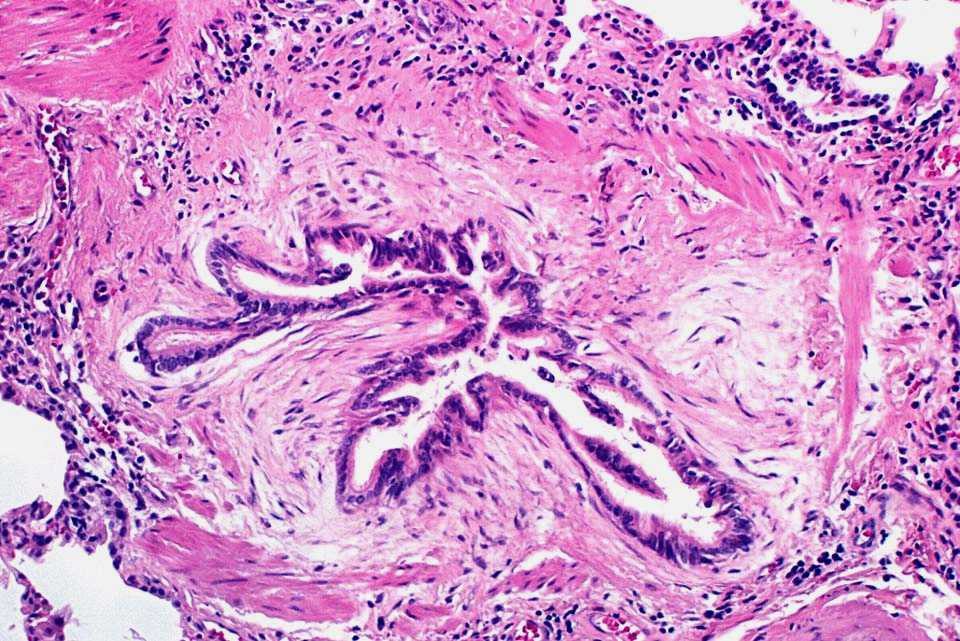
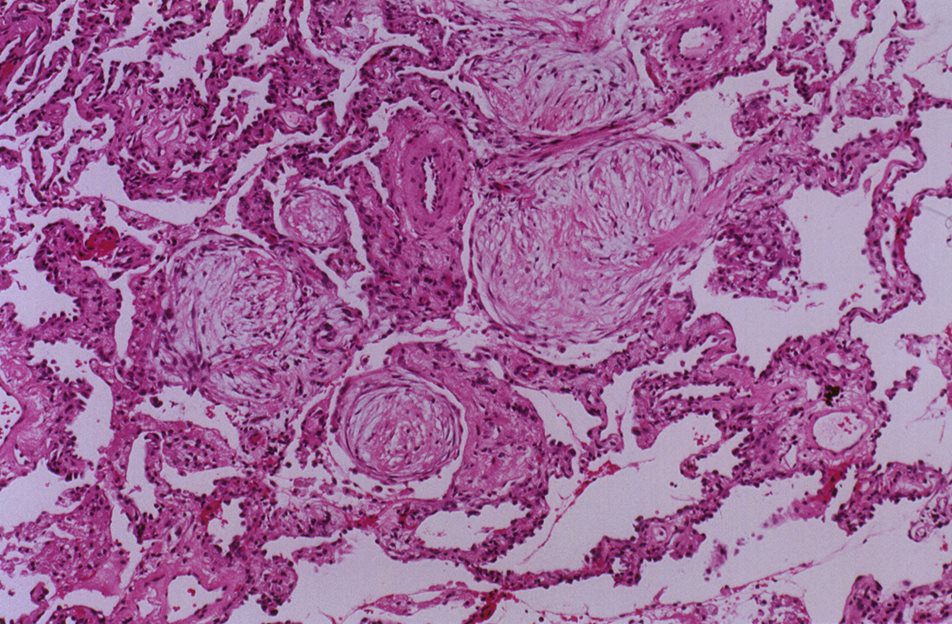
Histopathology of acute bronchiolitis characterized by dense peribronchiolar infiltrate of acute and chronic inflammatory cells associated with an intraluminal exudate rich in neutrophils
Ryu, J Pulmonary Medicine Bronchiolitis Pulmonology Advisor
- usually viral infections,
- respiratory bronchiolitis,
- smoking adults
-
- smoking adults
- acute bronchiolitis
- primary bronchiolar disease
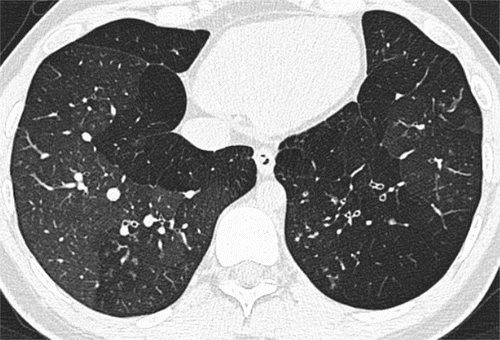
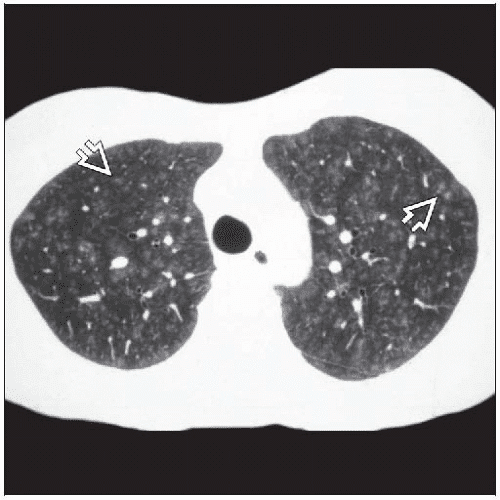
Mosaic attenuation pattern. CT scan through lower lobes shows the indirect sign of constrictive obliterative bronchiolitis, in this case the sequel to a severe viral lower respiratory tract infection.
https://pubs.rsna.org/doi/full/10.1148/radiol.13120908
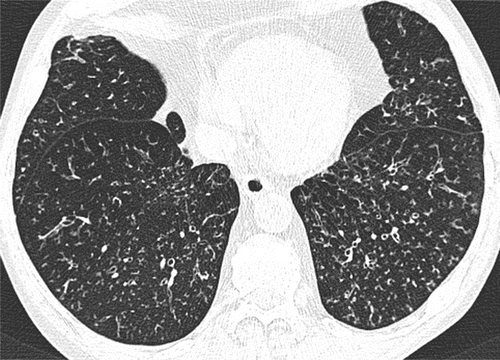
https://pubs.rsna.org/doi/full/10.1148/radiol.13120908
- constrictive or obliterative bronchiolitis
- bronchiolitis obliterans syndrome
- bone marrow transplant
- lung transplant
-

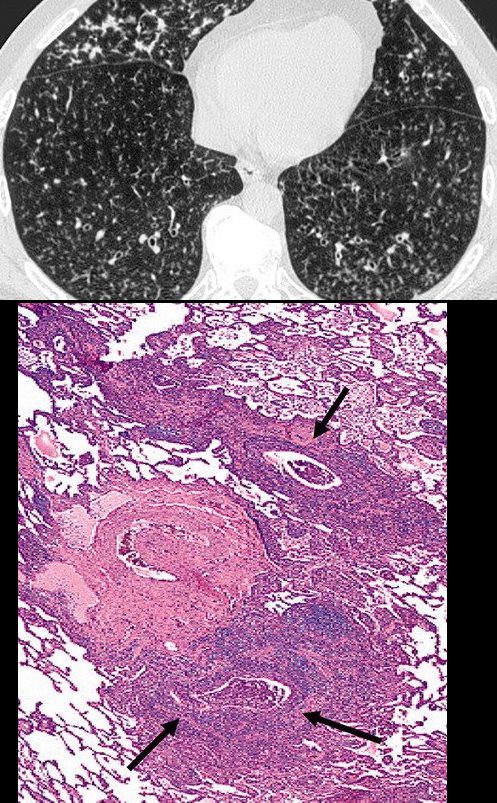
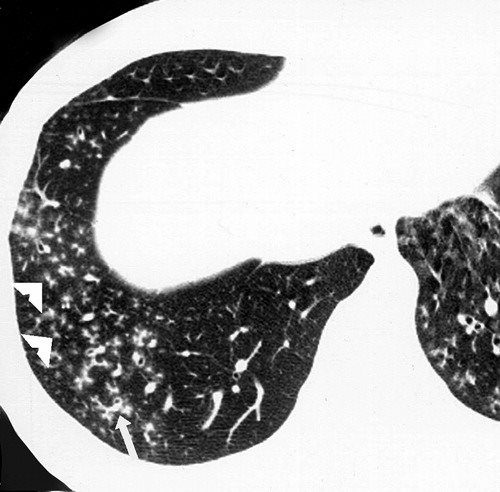
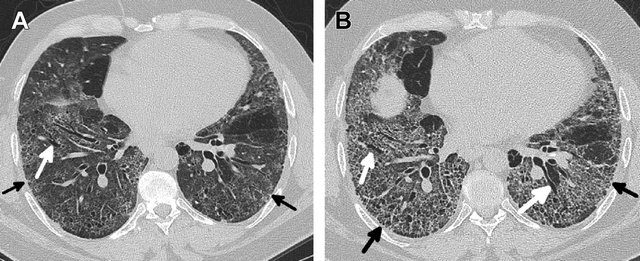
Obliterative bronchiolitis after bone marrow transplantation in a 47-year-old man with myeloma. (a) Expiratory high-resolution CT scan shows diffuse centrilobular nodules connected to branching linear opacities bilaterally. Note the air trapping in the right lower lobe. (b) Photomicrograph (original magnification, ×200; hematoxylin-eosin stain) of a specimen from open lung biopsy shows the bronchiolar walls surrounded by concentric chronic inflammatory infiltrates (arrows).
Rossi, SE et al Tree-in-Bud Pattern at Thin-Section CT of the Lungs: Radiologic-Pathologic Overview RadioGraphics Vol. 25, No. 3 2005 - collagen diseases
-

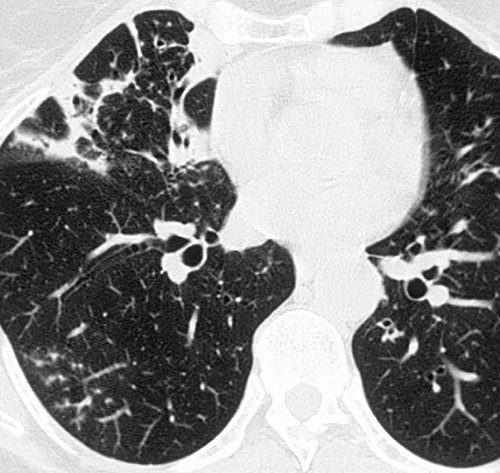
Sjögren syndrome in a 54-year-old woman. Thin-section CT scan shows peripheral tree-in-bud patterns in the right lower lobe. Note the bronchial dilatation, bronchial wall thickening, and consolidation.
Rossi, SE et al Tree-in-Bud Pattern at Thin-Section CT of the Lungs: Radiologic-Pathologic Overview RadioGraphics Vol. 25, No. 3 2005
-
- inhalational diseases
-

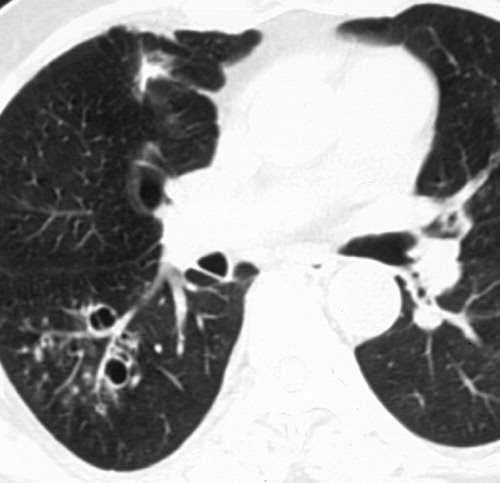
Inhalation bronchiolitis in a 56-year-old man after accidental exposure to sulfur dioxide. High-resolution CT scan shows bronchiectasis in combination with the tree-in-bud pattern in the right lower lobe.
Rossi, SE et al Tree-in-Bud Pattern at Thin-Section CT of the Lungs: Radiologic-Pathologic Overview RadioGraphics Vol. 25, No. 3 2005
-
- CT air trapping mosaic attenuation
-

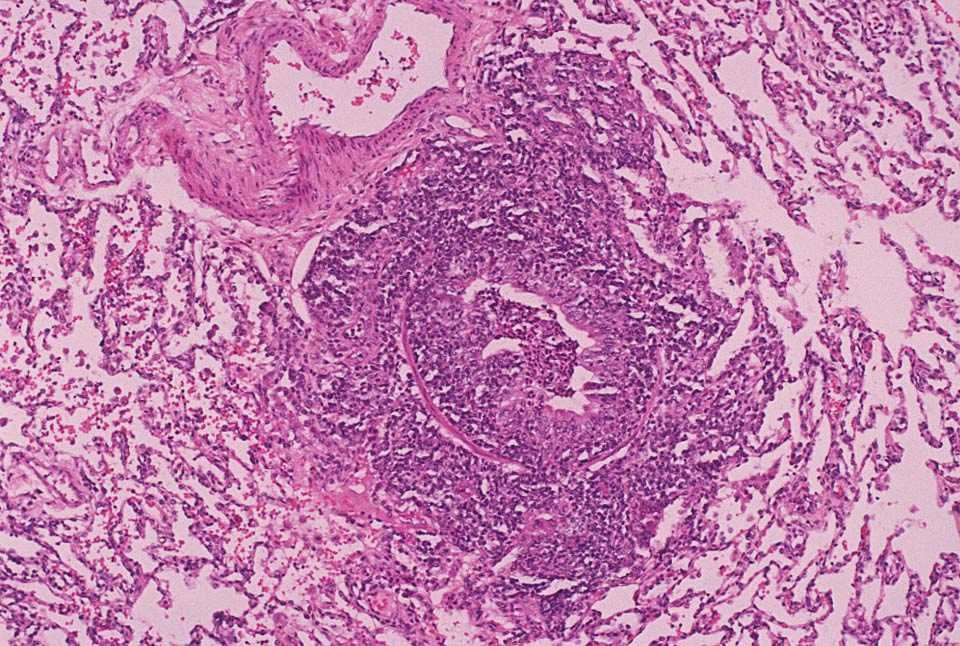
Histopathology of constrictive bronchiolitis characterized by fibroblast proliferation and stromal edema with associated collagen deposition in the submucosa, resulting in airway luminal constriction
Ryu, J Pulmonary Medicine Bronchiolitis Pulmonology Advisor
- bronchiolitis obliterans syndrome
- follicular bronchiolitis,
- connective tissue disease,
- immunodeficiency disorders, or
- chronic infections.
- diffuse panbronchiolitis,
- Asian population (particularly in the Japanese).
-

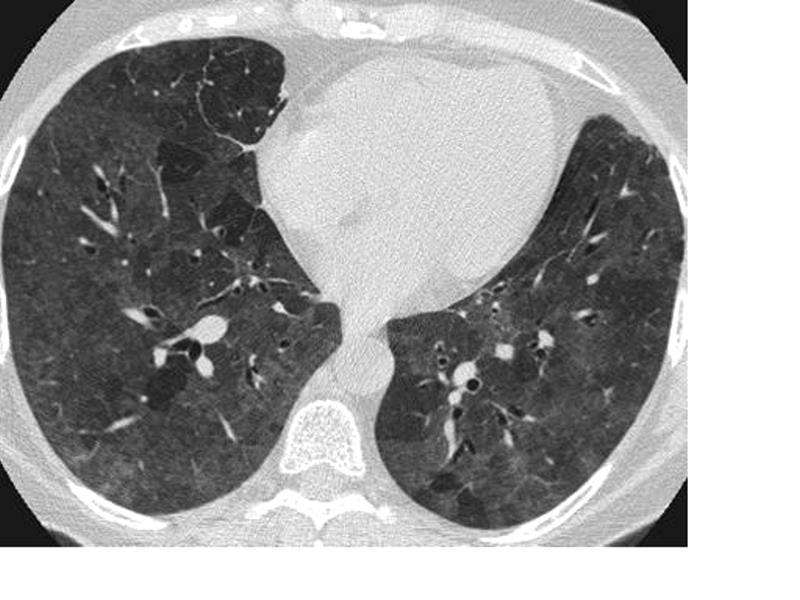
Diffuse panbronchiolitis in a 44-year-old Japanese man. High-resolution CT scan shows diffuse small centrilobular nodules and branching linear opacities (arrow), which resemble the objects used in the game of jacks. Note the bronchiolar dilatation and mucoid impaction (arrowheads).
Rossi, SE et al Tree-in-Bud Pattern at Thin-Section CT of the Lungs: Radiologic-Pathologic Overview RadioGraphics Vol. 25, No. 3 2005
- diffuse aspiration bronchiolitis,
- mineral dust airway disease
- inorganic dusts, – occupation-related
- silica,
- silicates,
- asbestos,
- iron oxide,
- aluminum oxide,
- talc,
- mica, and
- coal. The disorder is primarily
- inorganic dusts, – occupation-related
- related to ILD

Hellemons M etal Eur Respir Rev 2020; 29: 190181. – September 30, 2020
Kligerman S et al Clinical-Radiologic-Pathologic Correlation of Smoking-Related Diffuse Parenchymal Lung Disease 2016
- hypersensitivity pneumonitis (HP)
-

Head cheese or brawn is a cold cut terrine or meat jelly, often made with flesh from the head of a calf or pig (less commonly a sheep or cow), typically set in aspic, that originated in Europe. Usually eaten cold, at room temperature, or in a sandwich, the dish is, despite the name, not a dairy cheese. The parts of the head used in the dish vary, though commonly do not include the brain, eyes or ears of the animal. The tongue, and sometimes the feet and heart of the animal may be included; the dish is also made using trimmings from more commonly eaten cuts of pork and veal, with the addition of gelatin as a binding agent. Head cheese may also be made without using the flesh from the head of an animal.
Courtesy Rainer Zenz source Wiki -

Hypersensitivity Pneumonitis
High-resolution CT: increase in density in areas of ground glass and air trapping in lower lobes in patients with hypersensitivity pneumonitis
Courtesy Mluisamtz11 -
- cryptogenic or secondary organizing pneumonia (OP),
-

Histopathology of organizing pneumonia (or BOOP), characterized by intraluminal plugs of proliferating fibroblasts that fill distal airways and peribonchiolar air spaces
Ryu, J Pulmonary Medicine Bronchiolitis Pulmonology Advisor - sarcoidosis, and
- idiopathic pulmonary fibrosis (IPF).
Links and References
Ryu, J Pulmonary Medicine Bronchiolitis Pulmonology Advisor
Winningham P, J. et al Bronchiolitis: A Practical Approach for the General Radiologist RadioGraphicsVol. 37, No. 3 2017
Links and References
TCV
Small Airway Disease Introduction
Fleischner Society
bronchiolitis
Pathology.—Bronchiolitis is bronchiolar inflammation of various causes (,33).
CT scans.—This direct sign of bronchiolar inflammation (eg, infectious cause) is most often seen as the tree-in-bud pattern, centrilobular nodules, and bronchiolar wall thickening on CT scans. (See also small-airways disease, tree-in-bud pattern.)