Ashley Davidoff
Definition
Carcinoma of the lung is a malignant disease originating in the epithelium of the airways or respiratory alveoli, with the exact cause not known but with multiple well known high risk factors including cigarette smoking as the major contributor.
The result is a space occupying abnormality in the lung or bronchus with both mechanical and functional effects.
The patient is usually asymptomatic in the early stages, but as the disease progresses symptoms may include coughing, shortness of breath, hemoptysis, chest pain, weight loss, loss of appetite, wheezing, fever, hoarseness.
The diagnosis is initially suspected based on the patients clinical background and a suspicious CXR, and then may be confirmed by sputum cytology, computerized CT scan, bronchoscopy, positron tomography (PET) scan, lung biopsy, or mediastinoscopy.
Treatment options include surgery, radiotherapy, and chemotherapy. Stenting of occluded bronchi with metallic stents helps open obstructed bronchi. Newer techniques in therapy include endobronchial laser therapy and photodynamic therapy (PDT).
Lung cancer is treated according to the histological type and the stage of the disease. Small cell carcinoma is managed primarily by chemotherapy and sometimes radiotherapy while non small cell carcinoma has a wider variety of options including surgery, radiotherapy, and chemotherapy.
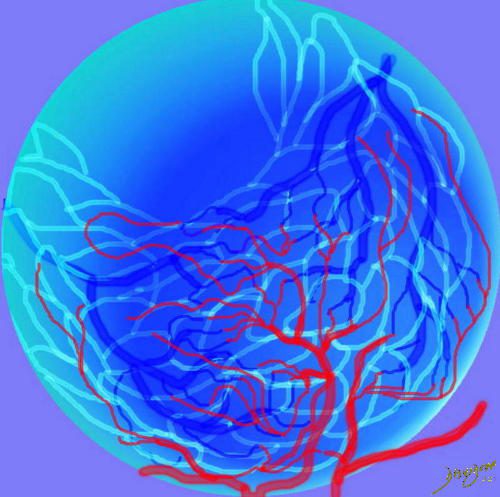
Cancer named as such by Hippocrates as “karkinos,” meaning crab, because the blood vessels surrounding malignant tumors resembled crabs. (32222)

What is the Approach to this Patient?
The CTscan is from a middle aged male with lung carcinoma in the left upper lobe (b in green) characterized by spiculated border (c) extending to the pleura, and an ipsilateral A-P window node (overlaid in green in d) and associated with profound emaciation. code lung cancer malignant mass spiculated A-P window node aortopulmonary node emaciation CTscan 3D volume rendering
Ashley Davidoff
TheCommonVein.net
78088c038.8s

This is the story of lung cancer, (left top) from the tobacco leaves of Virginia, to the cigarette, a nicotine filled alveolus, repeated contact with epithelium, and malignant proliferation with compromise of the lumen. People of all types affected by the curse of smoke. The histology may be of the non small cell or the small cell type, but in either case malignant and space occupying. A cough is common with the clinical presentation and a mass frequent on CT. Biopsy follows with staging by PET scan, multidisciplinary conference, and therapeutic choices – surgery, radiation and or chemotherapy. Mortality is usually inevitable with this devastating disease, but there is always hope for a cure in early stages.
Ashley Davidoff
TheCommonVein.net
10296c
keywords lung pulmonary disease introduction collage people gross pathology smoking
Principles
In this section we discuss the principles of structure and then the principles of malignant growth and the structural changes that occur.
Structural Principles
From the outset is important to understand the classification of lung cancer since the biology and approach to therapy depends significantly on this understanding.
There are two broad categories of lung cancer
Small Cell Lung Cancer (SCLC)
Non Small Cell Lung Cancer (NSCLC)
The reason for dividing them in this way is that SCLC is an aggressive non surgical disease with no curative possibility at this time, while treatment of NSCLC depends dominantly on staging where earlier stages have surgical and curative possibilities.
- Non small lung cancers also are divided into
- Squamous cell carcinoma
- Adenocarcinoma
- Bronchioloalveolar carcinoma
- Large Cell Carcinoma
The lung cancers are structurally divided into those that have a predilection for the larger airways and are called central cancers (more commonly small cell cancer, and squamous cell cancer) and the peripheral cancers that occur in the smallest airways and alveoli (more commonly adenocarcinoma and its subtypes bronchioloalveolar carcinoma and large cell carcinoma)
There are many implications in this structural division of tumors but of great significance is the fact that the major vessels including arteries, veins, airways, and lymphatics take origin or converge at the hilum centrally so that space occupation in this region has far reaching effects on the tree like structures more peripherally. The peripheral tumors on the other hand are close to the end of the line of the branching structure and so the structural implications are not as great.
Central Cancer
The central system in this context incorporates the main bronchi, through 16-23 divisions to, but not including the terminal bronchioles. The first division after the trachea results in the right and left main stem bronchi, and then branching follows to lobar bronchi (right upper, middle and lower, left upper, and lower) , segmental, subsegmental bronchi and then lobular bronchioles. At this point the central airways transitions into the peripheral system at the level of the terminal bronchioles.
About 75% of lung cancers originate from the first order, second order and third order bronchi. Within this group of central airways, the dominant tumors include small cell carcinomas (75-80% of SCLC occur in this region), and squamous cell carcinomas (65% of squamous cases occur in this region). The flexible bronchoscope has an external diameter that ranges between 4.9-6.2mm which will allow access to the fifth and even 6th generation bronchus. (Naidich) Ultrathin bronchoscopes that enable access to the 10th generation (outer diameter 2.7mm -3.8mm)
This diagram shows the basic division of the tracheobronchial tree into lobes. The right lung is divided into right upper (RUL) (teal) right middle, (RML pink) and right lower lobe (RLL green). The left lung is divided into left upper (LUL teal), which includes the lingula(dark blue), and left lower lobe (LLL= green). Note that the two mainstem bronchi are of unequal length and size. The right mainstem is short and fat while the left is long and thin. This irregular dichotomous branching pattern is characteristic of the branching pattern of all the conducting systems within the lungs.
Ashley Davidoff
TheCommonVein.net
32686b05
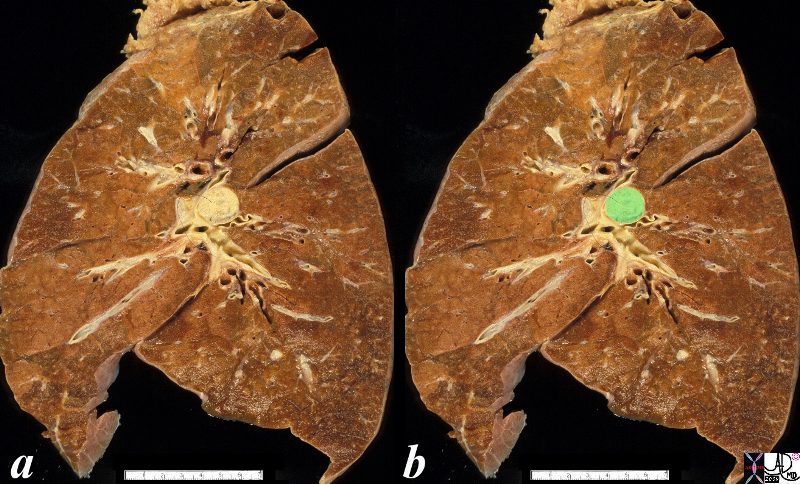
The anatomical specimen shows a 2cms central lesion near the hilum of the left lung causing extrinsic impression on the central bronchovascular bundle. The relatively small size and central location suggests a squamous cell carcinoma though a non small cell carcinoma is also possible
Ashley Davidoff
TheCommonVein.net
32323c02.8s

An axial and a sagittal view of a centrally placed carcinoma that lies on the major fissure of the right lung code lung mass fissure likely carcinoma central probability of it being a squamous cell carcinoma or a small carcinoma is high because of its central location.
keywords lung mass nodule major fissure cancer carcinoma central CTscan
Ashley Davidoff
TheCommonVein.net
75675c01.8s

The CT scan of the centrally positioned small cell carcinoma has structural implication as a result of its central location close to large arteries, veins, airways and lymphatics. In this case the centrally placed tumor (dark green in image b) is pushing on the right mainstem bronchus (shown with white arrow) and the lymphatics with peribronchial thickening (image d light green) and extension into the interlobular septa (bright green in d) Subcarinal nodal involvement and left hilar involvement (light green in b)together with small right effusion (a,b) are also noted suggesting advanced disease.
Ashley Davidoff
TheCommonVein.net
87711c01.8s
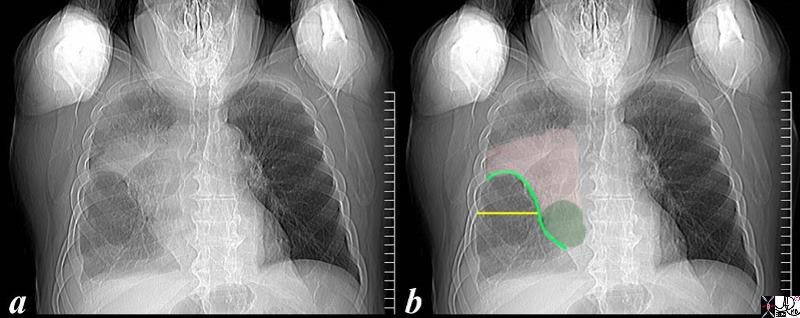
The scout film performed prior to a CT scan from a 76 year old man with chest pain and shortness of breath. The appearance suggests atelectasis of the right upper lobe with the normal position of the minor fissure (yellow) altered so that the upper portion (light green above the yellow line) is shifted upward caused by volume loss of atelectatic right upper lobe. (pink). The lower portion of the fissure (light green below the yellow line) is bulging rightward and outward caused by an implied mass (dark green). The “reversed S sign of Golden” is demonstrated in this case and infers a central mass causing obstruction and resulting in the shape described by the light green line of the minor fissure.
Ashley Davidoff
TheCommonVein.net
87740c02.8s
Peripheral Cancer
The peripheral system starts at the terminal bronchiole which after it divides becomes the respiratory (acinar) bronchiole, alveolar duct, and finally the termination of the system – the alveoli. It is in this region that the peripheral carcinomas commonly arise including adenocarcinoma, its variant bronchioloalveolar carcinoma (BAC) and large cell carcinomas.

This artistic rendition of the small parts of the lung shows the beginning of the peripheral system just before it enters the acinus. This duct is called the terminal duct and it is the last part of the ductal system that has no ability for gas exchange. After its first division, the bronchioles become the respiratory bronchioles, and they are the first in the system to have an ability to both transport the gases as well as enable gas exchange.
Ashley Davidoff
TheCommonVein.net
32645b04b05.8s
The Terminal Bronchiole
The terminal bronchiole is the last airway of the tracheobronchial tree whose sole function is to transport air but without the ability to enable gas exchange. It measures about .7mm.
It terminates by dividing into sac-like protrusions, which allow gas exchange to start taking place. The first branch that is able to perform this gas exchange is called the respiratory bronchiole (acinar bronchiole) which measures about .5mm. After three divisions the respiratory bronchioles become alveolar ducts and after further division become alveolar sacs. Finally, at the terminal end of this pathway, the alveoli emerge.
The Acinus
The acinus is defined as the portion of lung that is distal to the terminal bronchiole (Webb) and is supplied by the respiratory bronchiole and usually measures about 6-10mms in diameter. (Osborne)
The acinus is functionally characterized by having the ability to both conduct air as well as enable gas exchange. When it is filled with fluid, it can be visualized on a CXR as a 6-7mm density called an “acinar shadow.” As a structural entity it has little diagnostic utility. We will expand on the pulmonary lobule in the next section which has greater implications for the imaging of the lung. Functionally, however, the acinus can be considered as the unit of gas exchange in the lung.

This is a drawing of a terminal bronchiole and an acinus which resembles a bunch of grapes. The most upstream component is the terminal bronchiole(the main stalk of the bunch of grapes) which is the first order branch in the peripheral system. It does not have alveoli associated with it and for this reason is not part of the acinus. Its function is to transport the air to respiratory bronchiole, alveolar sac and alveoli, all of which have the ability to exchange gas .
Ashley Davidoff
TheCommonVein.net 42650
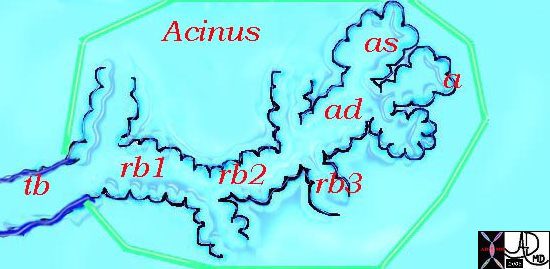
This diagram illustrates the acinus which consists of the respiratory bronchioles (rb 1, 2, 3) the alveolar duct (ad) the alveolar sac (as) and the alveoli. (a)
Courtesy Ashley Davidoff MD 42446b12
Ashley Davidoff
TheCommonVein.net
The Secondary Lobule
The secondary lobule (Webb) is the fundamental functional and structural unit that is enclosed in a membrane, measuring between 1-2.5cms in diameter, and is subtended by a small bronchiole and arteriole. There are usually between 8-12 acini per lobule, but this number varies between 3-24 . (Itoh)
Respiratory Bronchioles, Alveolar sacs, and Alveoli within a Membrane
This drawing shows about 3-6 respiratory bronchioles that serve to make a secondary lobule. Alveolar sacs and individual alveoli are also seen. The yellow border represents the interlobular connective tissue.
Ashley Davidoff
TheCommonVein.net
32153
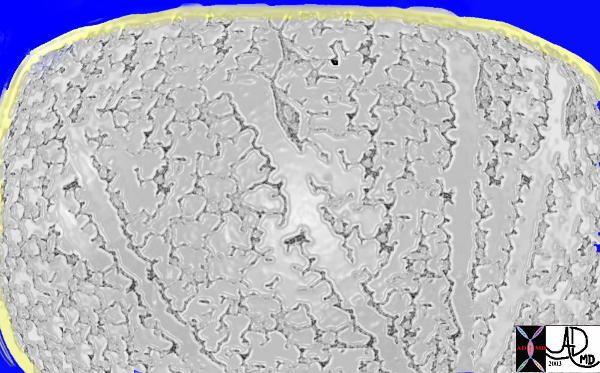
Normal lung histology
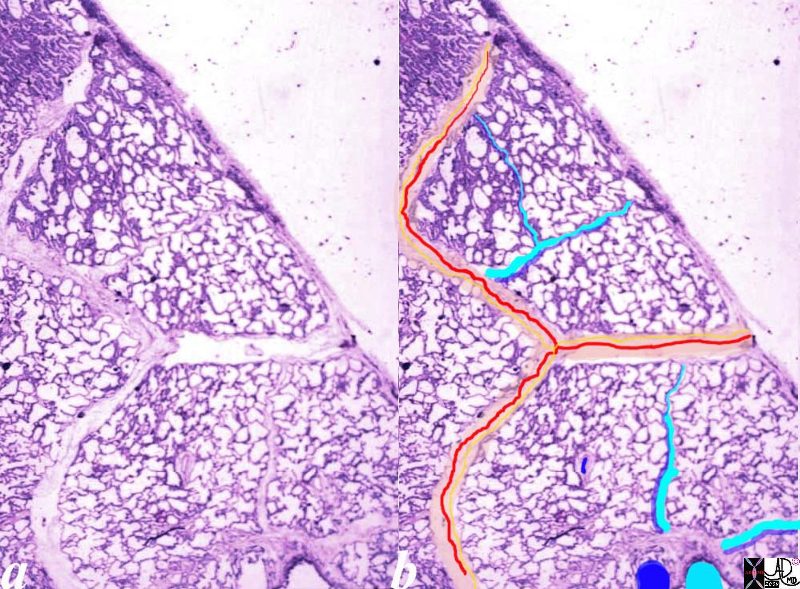
This image is a panoramic view of the lung showing secondary lobules and interlobular septa. Within the interalveolar septae, one sees small venules and lymphatics .
The side by side images show the interlobular septa within which reside the pumonary venules (red) and lymphatics and within the center of the lobule run the respiratory bronchioles (teal) and pulmonary arterioles (blue)
Courtesy Armando Fraire MD. 32649b
key words
lung pulmonary alveoli alveolus secondary lobule interlobular septa vein lymphatic histology
interstitium interstitial
32649c06.8s
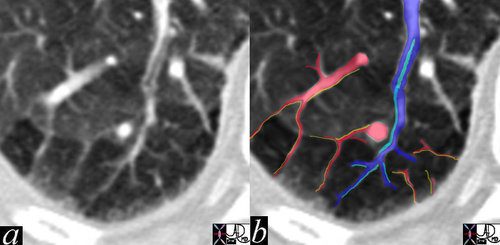
The high resolution CT shows multiple secondary lobules in the periphery of the right lung. A lobular bronchiole is overlaid in teal, while the accompanying lobular arteriole is seen in royal blue entering the lobule and then branching. The peripheral venules are identified in the interlobular septa (red) and joining to form the lobular vein.
In this remarkable CT we were able to identify a few secondary lobules at the periphery of the lung that have a rectangular shape in this instance. The branching structure that enters the lobule (blue in b), is characterised as an arteriole for two reasons. Firstly it is paired with a tubular airway seen in (a) in its most proximal portion as a lucent tubule, and subsequently interpolated in light blue in b. Secondly it branches in the centre of the lobule. It is distinct from the border forming interlobular septum which surrounds it. A second relatively large vessel colored in red receives a branch from the interlobular septum and by virtue of its size and position it has to be a pulmonary venule. We know that the lymphatic vessel accompanies the venule, and so the yellow lymphatic has been implied but not visualised. We also know that connective tissue surrounds these two structures. In this instance the matrix of the lobule that consists of the alveoli is less dense than it should be and is surrounded by normal alveoli. Lucency implies air trapping and air trapping implies small airway disease. Thus this image tells us that the criminal in this case of disorder is the small airway, We now can focus on the small airways with a pathological differential diagnosis, and from there plan the treatment.
key words
lung pulmonary lobule secondary lobule arteriole venule interlobular septa bronchovascular bundle mosaic pattern air trapping fx ground glass
CTscan
Ashley Davidoff MD
47152c01
This drawing demonstrates the open mouth view of the alveolus, which is surrounded by its capillary network. The lining single layer of squamous cells (pneumocytes) can be seen peaking through the vessels.
Ashley Davidoff MD.
TheCommonVein.net
32166
The peripheral cancers either originate from the terminal bronchiole or from the airways of the acinus or from the alveolar cells as in the case of the bronchioloalveolar carcinoma.

The 3.5cms carcinoma is peripherally situated and is sub-pleural in location. It reveals fibroblastic (aka desmoplastic) effect as witnessed by the puckering of the pleura (arrow). It is remote from central bronchovascular structures and therefore remains relatively asymptomatic for an extended duration unless it causes pleuritic pain. The location and desmoplastic puckering of the pleura are characteristic of an adenocarcinoma.
Ashley Davidoff
TheCommonVein.net
32201b.81s
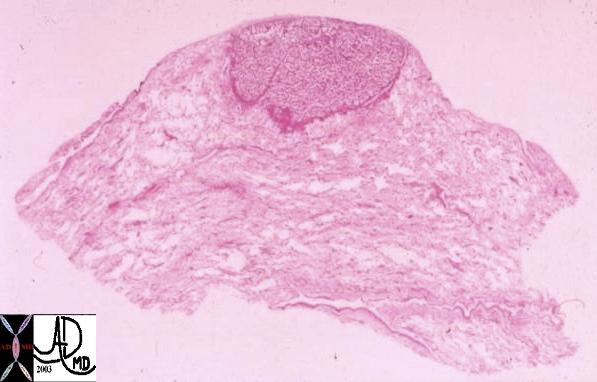
This whole mount of a part of the periphery of the lung reveals a peripherally located nodule without evidence puckering of overlying pleura. Microscopically this proved to be a papillary carcinoma.
Courtesy Armando Fraire MD. 32812
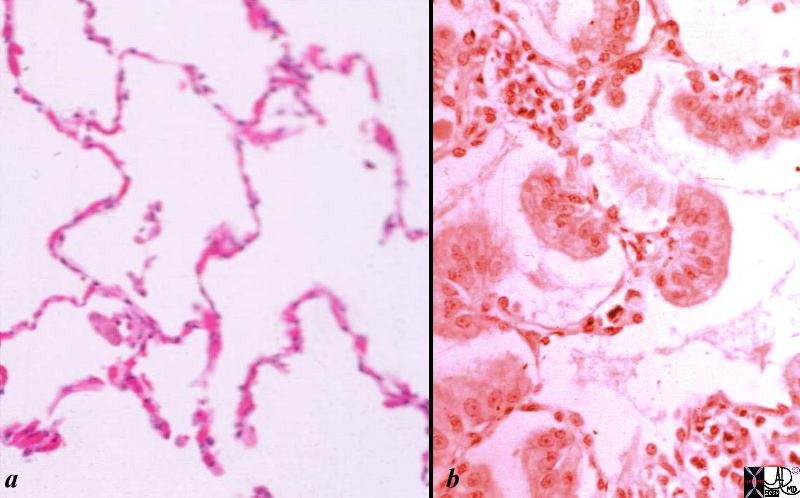
Histological sections of a group of a normal alveoli (a) and alveoli filled with nests of malignant cells.
Normal lung- is shown in low magnification. Note the cup-shaped alveolar spaces outlined by delicate thin alveolar capillary membrane with the lumen of the alveoli being mostly empty .
In image b the malignant cellular material originates from and spreads along the alveolar epithelium without destroying the alveolar walls. The malignant clusters of cells seem to be hanging from the alveolar epithelium like washing from a washing line. Note groups of tall, columnar, mucin producing cells spreading along preexisting alveolar walls, which is typical of bronchioloalveolar carcinoma.
Courtesy Dr Armando Fraire MD
TheCommonVein.net
32828c02.8s
The peripheral lesions from the terminal bronchiolar and alveolar epithelium are mostly but not universally adenocarcinomas and are distinguished by a glandular epithelium with fibrous and stromal response around tumor cell nests. Adenocarcinoma destroys the tissues and connective tissue infrastructure, incites desmoplasia and invades the lymphatics. It sometimes produces mucus
BAC arises from and grows along alveolar surfaces, spreading along the infrastructure, and uses the framework to spread without tissue destruction with resulting pneumonia like appearance on the CT scan.
Cancers arising in the periphery are mostly asymptomatic in the early stages – and therefore at the time of presentation are usually more advanced. Sputum cytology is usually negative presumably because they are so remote.
Draining Lymph Nodes
There are 4 basic group of nodes
Superior Mediastinal Nodes
1 Highest Mediastinal Nodes
2 Upper Tracheal Nodes
3 Prevascular and Retrotracheal Nodes
4 Lower Paratracheal Nodes
Aortic Nodes
5 Subaortic Nodes (A-P window)
6 Paraaortic Nodes (Ascending Aorta or Phrenic)
Inferior Mediastinal Nodes
7= subcarinal nodes
8=Paraesophageal Nodes
9 = Pulmonary Ligament Nodes
Other
10 Hilar Nodes
11 Interlobar Nodes
12 Lobar Nodes
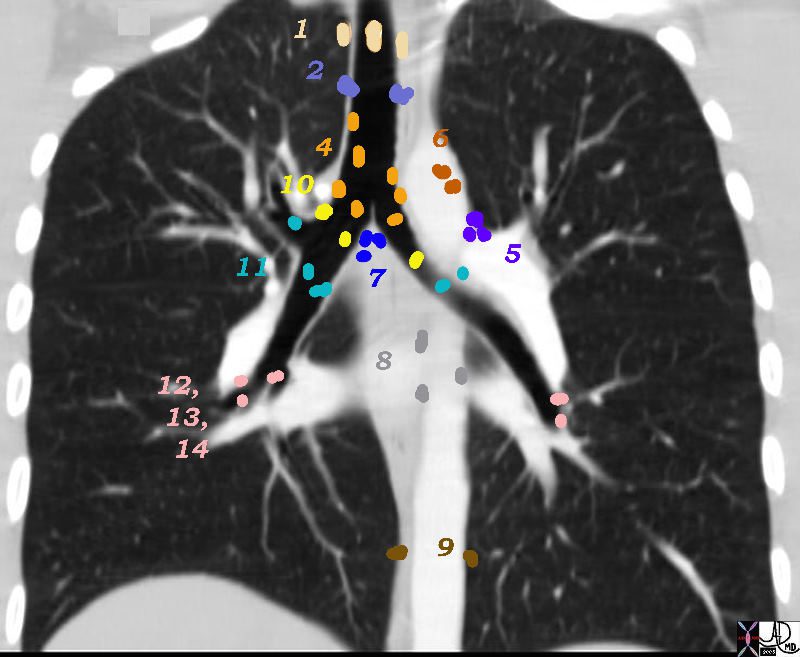
There are Aortic Nodes 5 Subaortic Nodes (A-P window) 6 Paraaortic Nodes (Ascending Aorta or Phrenic) Inferior Mediastinal Nodes 7= subcarinal nodes 8=Paraesophageal Nodes 9 = Pulmonary Ligament Nodes 10 Hilar Nodes 11 Interlobar Nodes 12 Lobar Nodes
Ashley Davidoff
TheCommonVein.net
32682n04.801
Principles of Malignant Disease
Malignant cells occupy the space of normal tissue but they do not contribute to the structural nor functional welfare of the body at large. They arise in the lung more commonly in the proximal airways and either occupy the lumen or extend beyond the lumen and occupy parenchymal space, which may cause mass effect on other neighboring structures including blood vessels, lymphatics, pericardium, pleura, heart, and esophagus.
Partial or total blockage of the bronchi results in obstruction and atelectasis, which can be complicated by secondary infection, and bleeding.
Normal cells reproduce about 50 times before dying. Malignant cells, however, grow uncontrollably.
Malignant cells lack contact inhibition, meaning that they do not stop growing when they make contact with another object. The tumor may invade a neighboring tissue or organ and impede its function.
A malignant tumor may release an angiogenetic growth factor, enabling the formation of feeding blood vessels.
Invasion of the lymphatics and venous structures is inevitable though invasion of arterioles does not usually occur. Once in the mainstream of the venous or lymphatic system they can metastasize and reestablish a new colony with similarly aggressive and parasitic features. The usual “next stop” for hematogenously spread lung primaries is the brain. In the end malignant disease dominates the body and the healthy structures succumb to the unbearable burden.
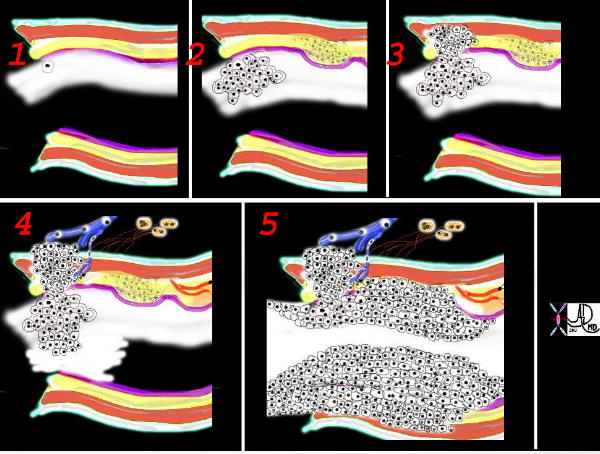
This is a collage showing the evolution of a malignant cell (1) into a nodule restricted to the epithelium (2) which with time penetrates the basement membrane and progressively extends into the submucosa and muscularis (3). Subsequent extension into local lymph nodes and blood vessels occurs (4) as well as growth into the lumen. As it grows circumferentially, narrowing and eventually obstruction of the lumen complicates the process (5) Space in tubular systems is limited and malignant growth has no respect for this space nor for boundaries. By definition malignant disease is space occupying.
Ashley Davidoff
TheCommonVein.net
32336c
