Introduction
Small Cell Carcinoma
Small cell lung cancers (aka SCLC and oat cell cancer) is a malignant condition of the epithelium usually arising from the central airways and specifically arising from the eneterochromaffin or Kulchitsky cell which embryologically originates from the neural crest. They account for 15-25% of lung cancers, and thus are less common than NSCLC. There is a definite causal relationship with cigarette smoking. The age population is slightly younger than the NSCLC group (27-66yrs SCLC vs 44-61yrs in NSCLC). SCLCs grow more quickly than NSCLCs and are more likely to metastasize early. Often, they have already spread to other parts of the body when the disease is diagnosed.
Structurally the tumor tends to be central , is bulky, fast growing, and usually with early hilar and mediastinal involvement. The malignant cells are characterized by their small size (as their name implies) being <21 microns which is slightly smaller than 2-3 lymphocyte diameters. They also resemble the lymphocyte in shape and character. Most of the population of cells is round to oval in shape but spindle-or polygonal forms occur as well.
The cytoplasm is usually sparse and the nuclii show a high mitotic rate as a result of the rapid growth. The nuclii are granular characterized by a salt and pepper appearance with small or inconspicuous nucleoli. The characteristic feature of malignant cells with a high nuclear to cytoplasmic ratio is also present.
Since they are central tumors, diagnosis is sometimes attained by cytological washings.
Clinically the patient may manifest with the effects of the tumor on the on the larger airways that includes cough, hemoptysis, dyspnea, and wheezing. The central location and tendency to bulky mediastinal involvement sometimes results in SVC syndrome. Paraneoplastic syndromes are characteristic of the disease as well.
The diagnosis is suspected by the CT appearance which shows bulky disease in the hilum and mediastinum. The approach to management is based on whether the disease is “limited” which would allow single port treatment with XRT as opposed to “extensive” disease which implies it has spread beyond the chest or requires more than one XRT port. PET scanning is extremely useful in staging the disease.
Treatment invokes both XRT and chemotherapy. The tumor has a remarkable and characteristic response to chemotherapy being specifically sensitive to mitotic inhibitors. It is this characteristic unique response to chemotherapy that prompted the division and classification of lung cancers into SCLC and NSLC.
Overall median survival for SCLC is 6-10 months. Patients with limited disease have 2 year survival of 10% and for extensive disease it is only 3%. 70 % of patients have extensive disease on presentation.

Courtesy Dr Armando Fraire MD
TheCommonVein.net
32517
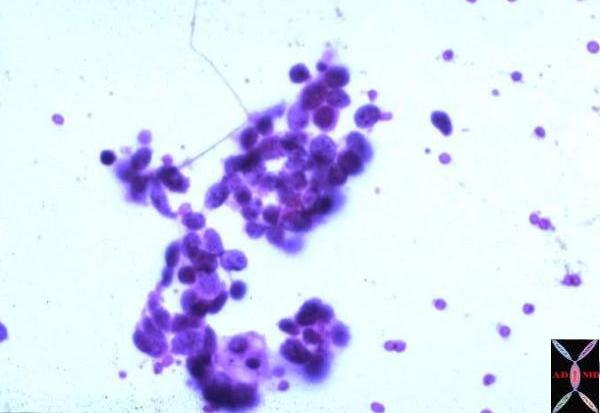
Small Cell Carcinoma of the lung Pleural fluid cytology preparation showing group of dark blue cells with scant cytoplasm consistent with small cell carcinoma.
Courtesy Armando Fraire MD.
TheCommonVein.net
32825
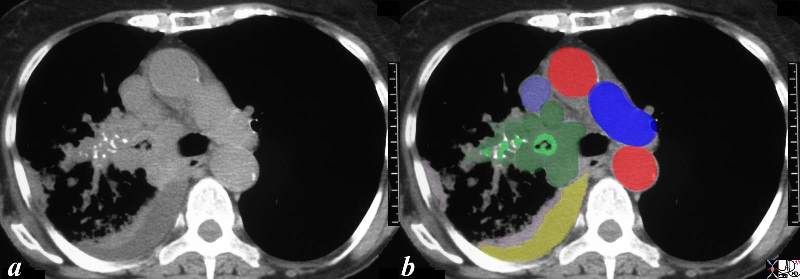
This CT scan is from a middle aged female with poorly differentiated small cell carcinoma, with extensive mediastinal and hilar involvement (dark green in b) extending into and almost occluding the right main stem bronchus light green with black air in the centre) and occluding the smaller airways (light green surrounded by white bronchial cartilage). A complex right effusion (yellow) and atelectasis is seen (light pink). The relationship to the SVC (light blue ) is noted without mass effect at this time, with aorta in red and left pulmonary artery (royal blue). Parenchymal disease is suspected based on the increased soft tissue noted in the mediastinal windows in the right lower lobe.
Courtesy Ashley Davidoff MD
TheCommonVein.net
32429bc03.8s
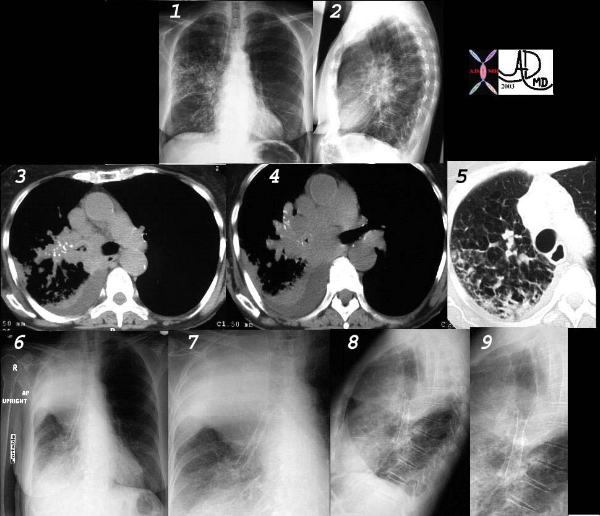
This collage of CT and plain film represents the radiological history of a patient with poorly differentiated small cell carcinoma, with extensive parenchymal involvement of the RUL and RML, and of the airways of RML and RLL. Images 1 and 2 show an interstitial and pneumonic pattern which was persistent over time. The CT shows extensive endobronchial disease involving right main stem (3,4) as well as almost all segments of RLL. This was confirmed by bronchoscopy.
Lymphangitic disease seems to be the dominant finding in the RUL on the lung windows. (5).
Following stent placement through a “pinhole” lesion, the patient occluded the RUL airways with tracheal shift and hyperinflation of the left lung (6,7,8,9). Clinically however, she improved greatly.
Courtesy Ashley Davidoff MD.
TheCommonVein.net
32426cl

Courtesy Ashley Davidoff MD.
TheCommonVein.net
32426_02cl
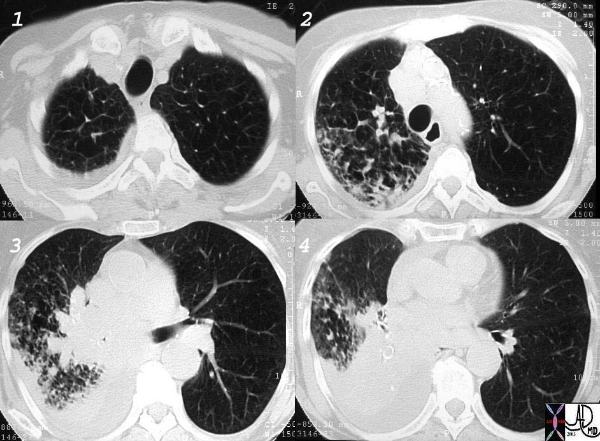
Courtesy Ashley Davidoff MD.
TheCommonVein.net
32426_03cl keywords
lung bronchus lymphatic infiltrate mass obstruction atelectasis thickening interlobular septa neoplasm malignant primary malignancy small cell carcinoma imaging radiology CTscan
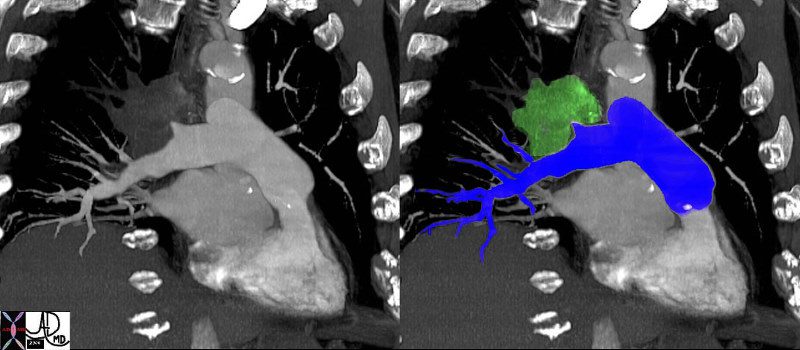
The coronal image shows a centrally placed small cell carcinoma (green mass in right image) occluding the right upper lobe pulmonary artery. (red ring)
Courtesy Ashley Davidoff MD.
TheCommonVein.net
46645c04.
