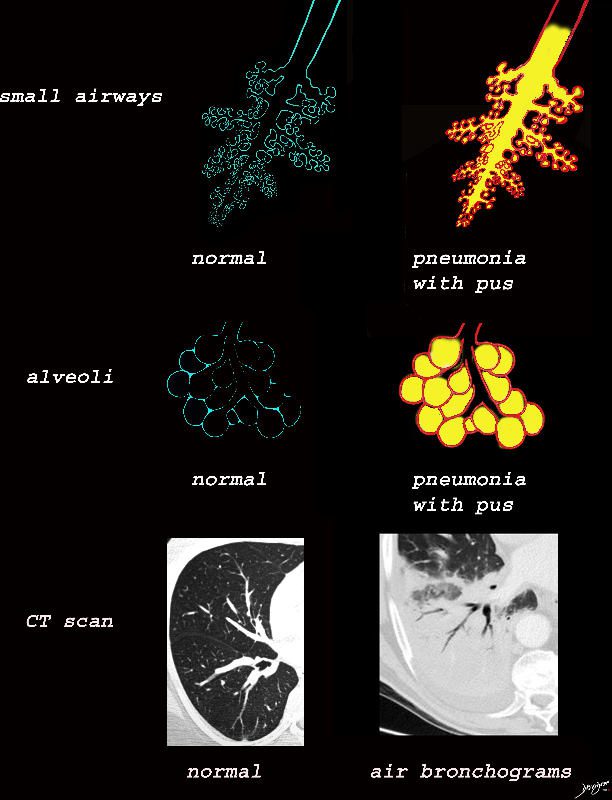
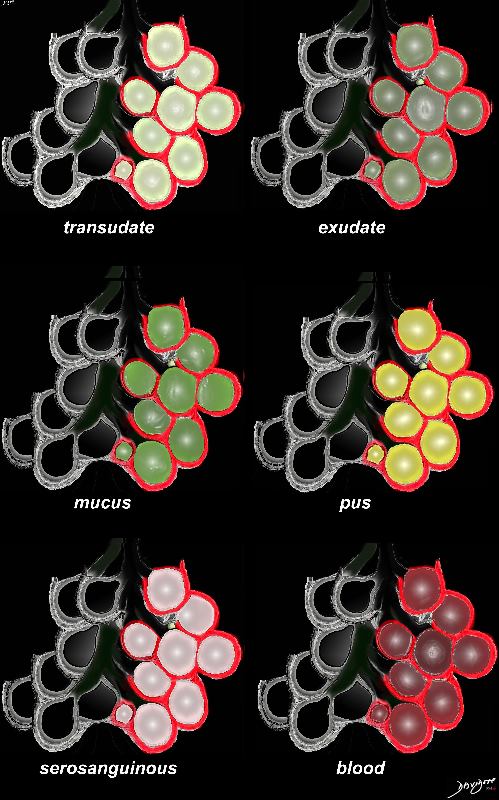
The collage provides a persepective of purulent accumulation in the small airways and the alveoli that results in consolidation. A process that increases the densityof the lungs to a net “white”regional density will result in a consolidation and in this case when the fluid is infected it is labelled “pneumonia” The net result on CT is aair bronchograms within the non aerated dense lung tissue.
Ashley Davidoff MD TheCommonVein.net lungs-0734
Alveoli Replaced by Fluid
Ashley Davidoff MD TheCommonVein.net
lungs-0704d
Alveoli Replaced by Cells
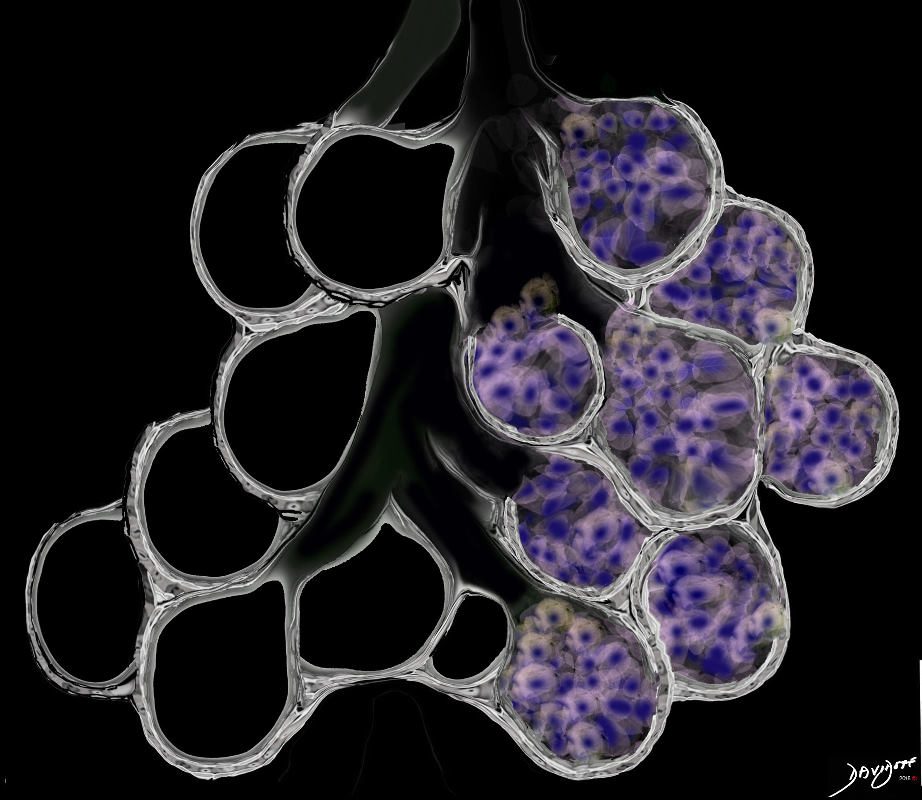
The alveoli may be filled by a cellular infiltration including inflammatory, benign or malignant cells without or with fluid. Type of cells include macrophages, Langerhans cells and malignant cells
Ashley Davidoff MD TheCommonVein.net lungs-0707d- lo res
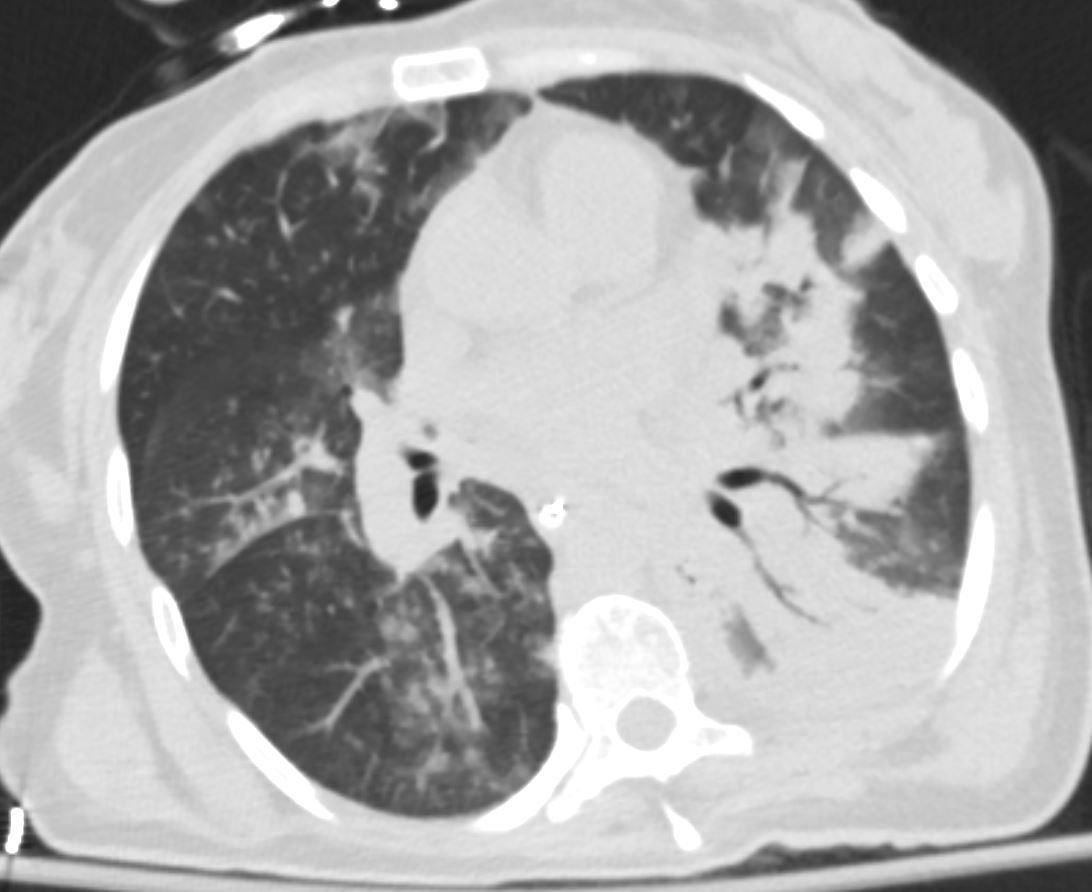
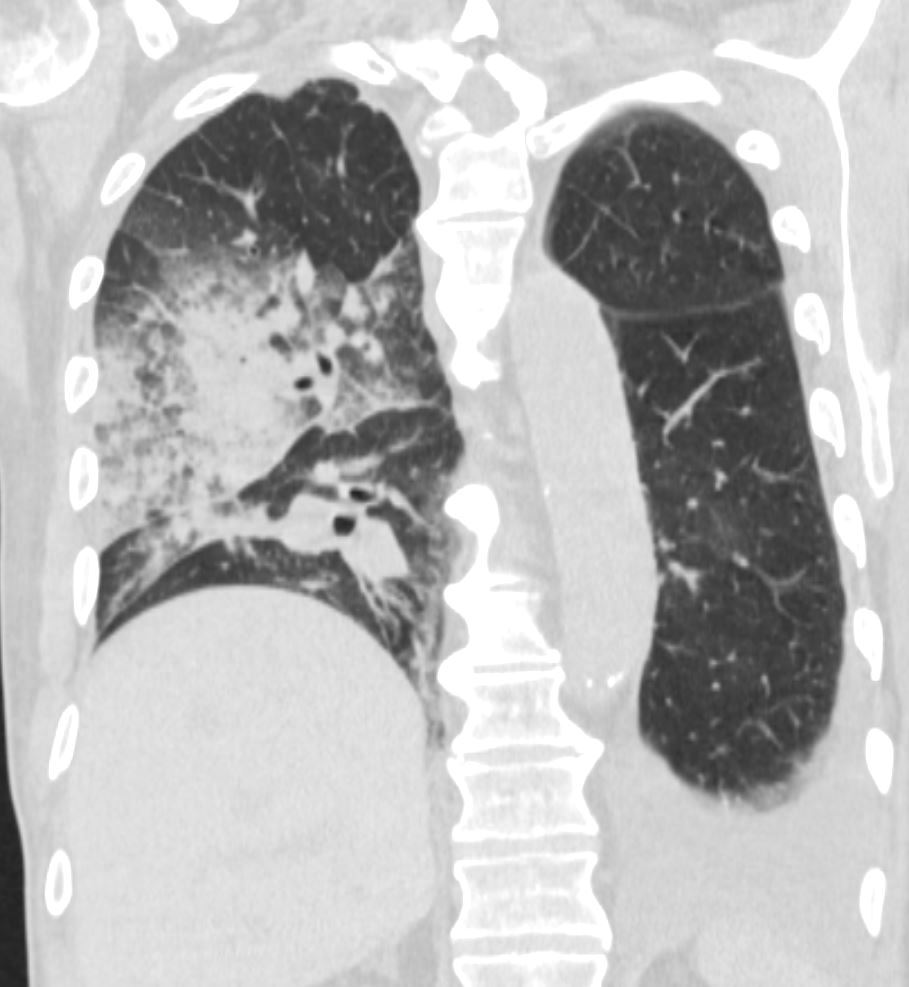
Acute Eosinophillic Pneumonia
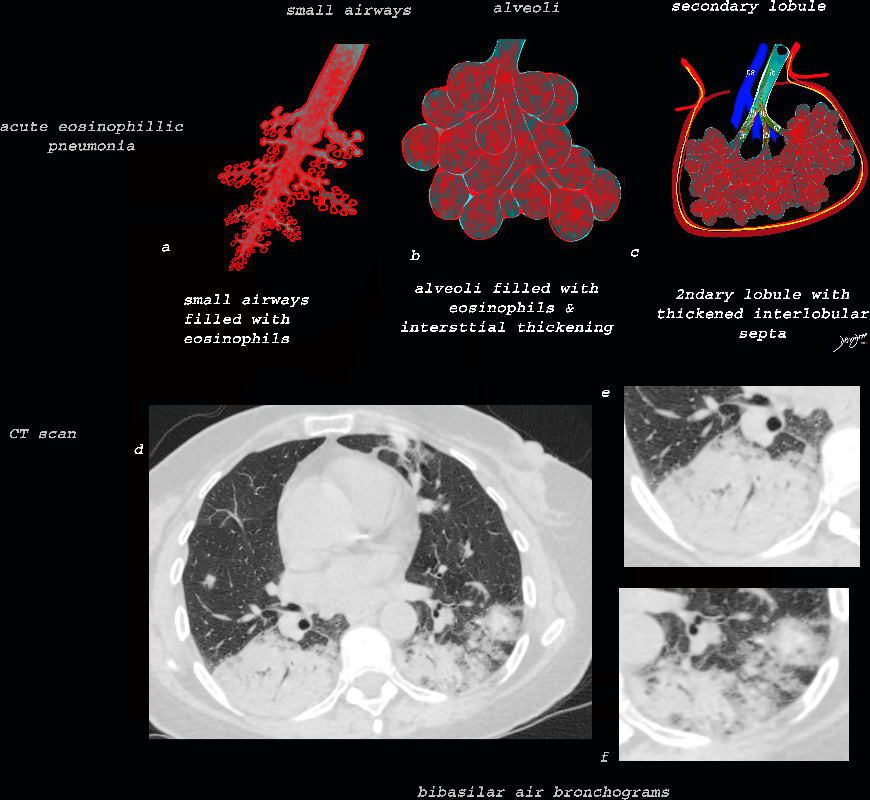
As the disease advances the small airways, and alveoli, get progressively filled with eosinophils, inflammatory cells and fluids resulting in consolidation. This image reveals progressive filling of the small airways, (a) alveoli, (b) and secondary lobules (c) with eosinophils and products of inflammation resulting in multi-segmental consolidations (d), in the lung bases, with air bronchograms at the right base (e), and less dense consolidation at the left base (f)
Ashley Davidoff MD The CommonVein.net lungs-0763
Whether the alveoli are filled with fluid or cells the result of consolidation is the same on Chest X-ray and CTscan
The Result on Imaging of Alveoli Filled with Fluid or Cells
Consolidation with Air Bronchograms
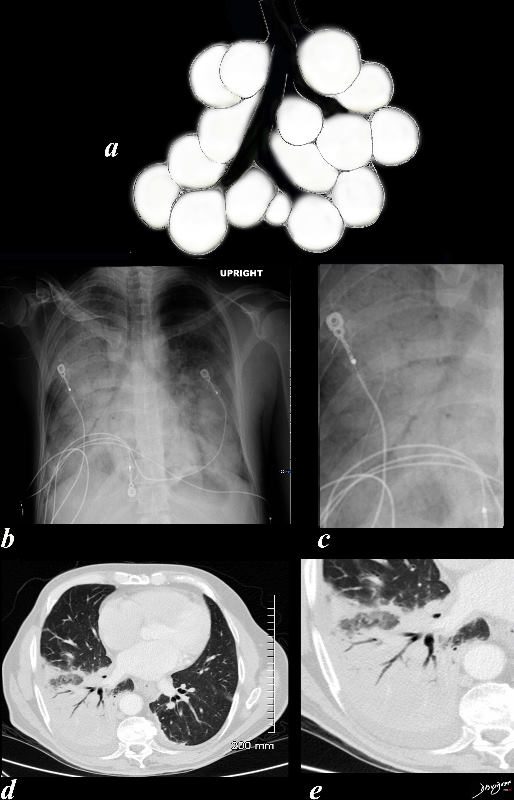
Black White and Gray Densities
The filling of alveoli with fluids or cells results in a density that is “white” on X-ray and CT scan and is in distinct contrast to the black of the air filled airways. This contrast results in an air bronchogram. The smaller airways in a normal patient are not usually visualized because the “black” of the of the airways and the black of the air filled alveoli does not create a contrast.
Ashley Davidoff MD TheCommonvein.net
lungs-0708d
CXR
Lobar Consolidation
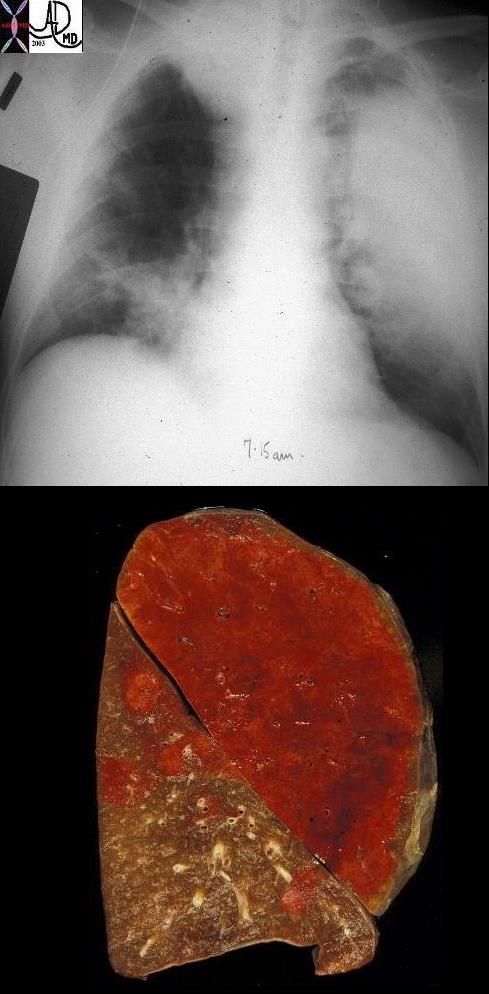
57 old male with LUL lobar pneumonia
A gross pathology specimen showing a hemorrhagic lobar pneumonia (red hepatization)
Ashley Davidoff MD TheCommonVein.net 32321cv
Ashley Davidoff MD TheCommonVein.net 134872.lungs c
Right Upper Lobar Consolidation
Courtesy Ashley Davidoff TheCommonVein.net

Segmental Consolidation
Superior segment
Ashley Davidoff MD TheCommonVein.net 130903c.8

Ashley Davidoff MD TheCommonVein.net

Ashley Davidoff MD TheCommonVein.net

Ashley Davidoff MD TheCommonVein.net
Ashley Davidoff MD TheCommonVein.net
Ashley Davidoff MD TheCommonVein.net
Ashley Davidoff MD TheCommonVein.net
Segmental Consolidation Pulmonary Hemorrhage
GPA (Wegener’s Granulomatosis)
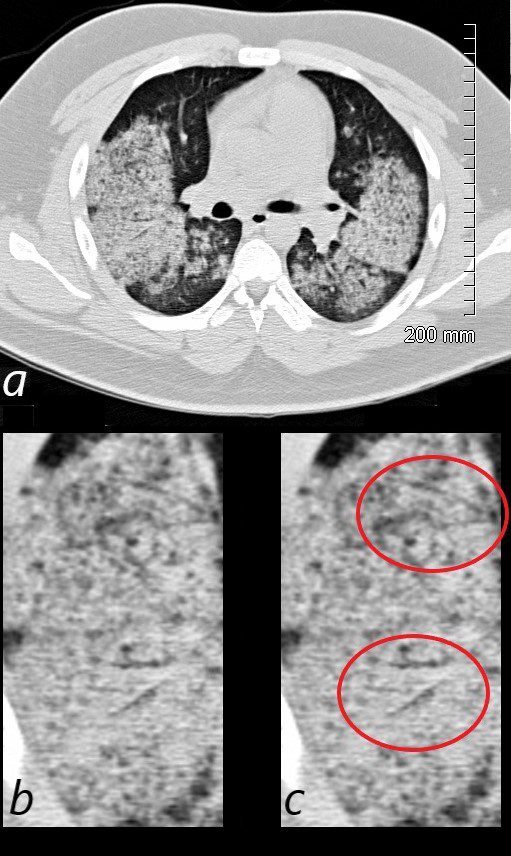
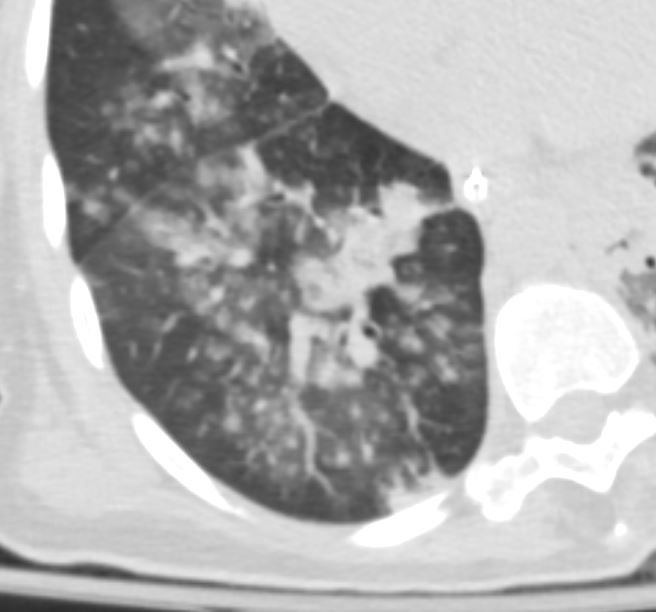
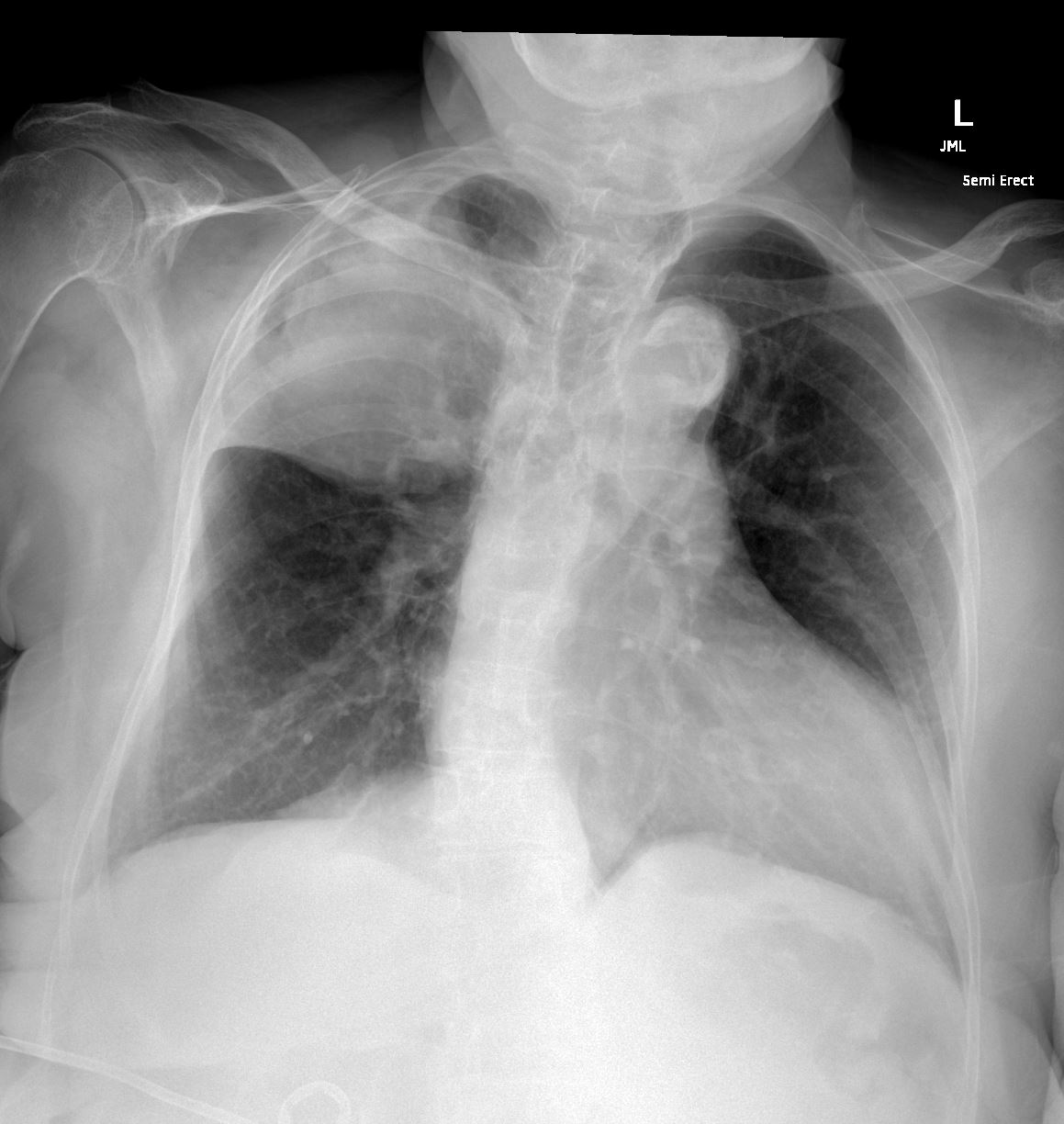
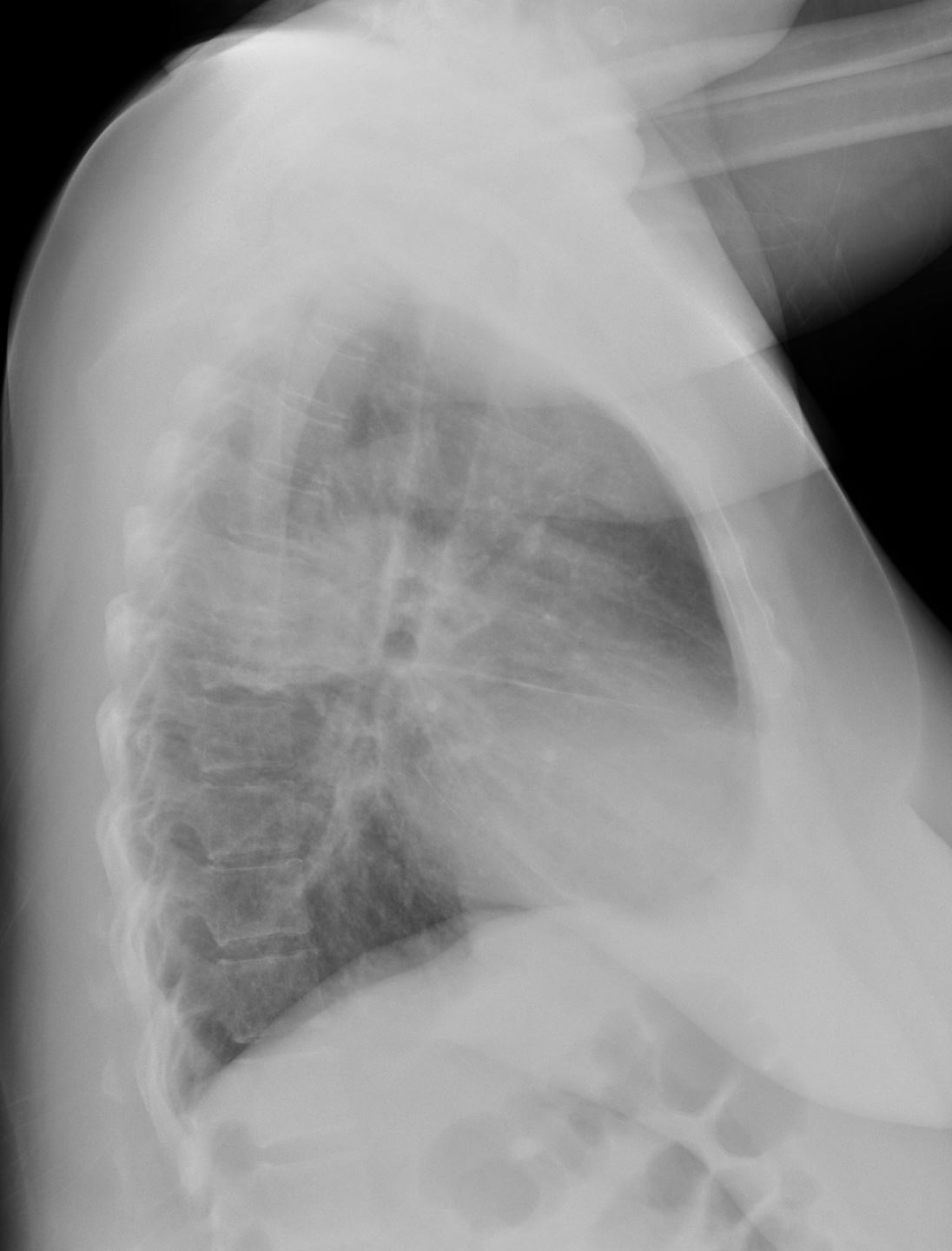
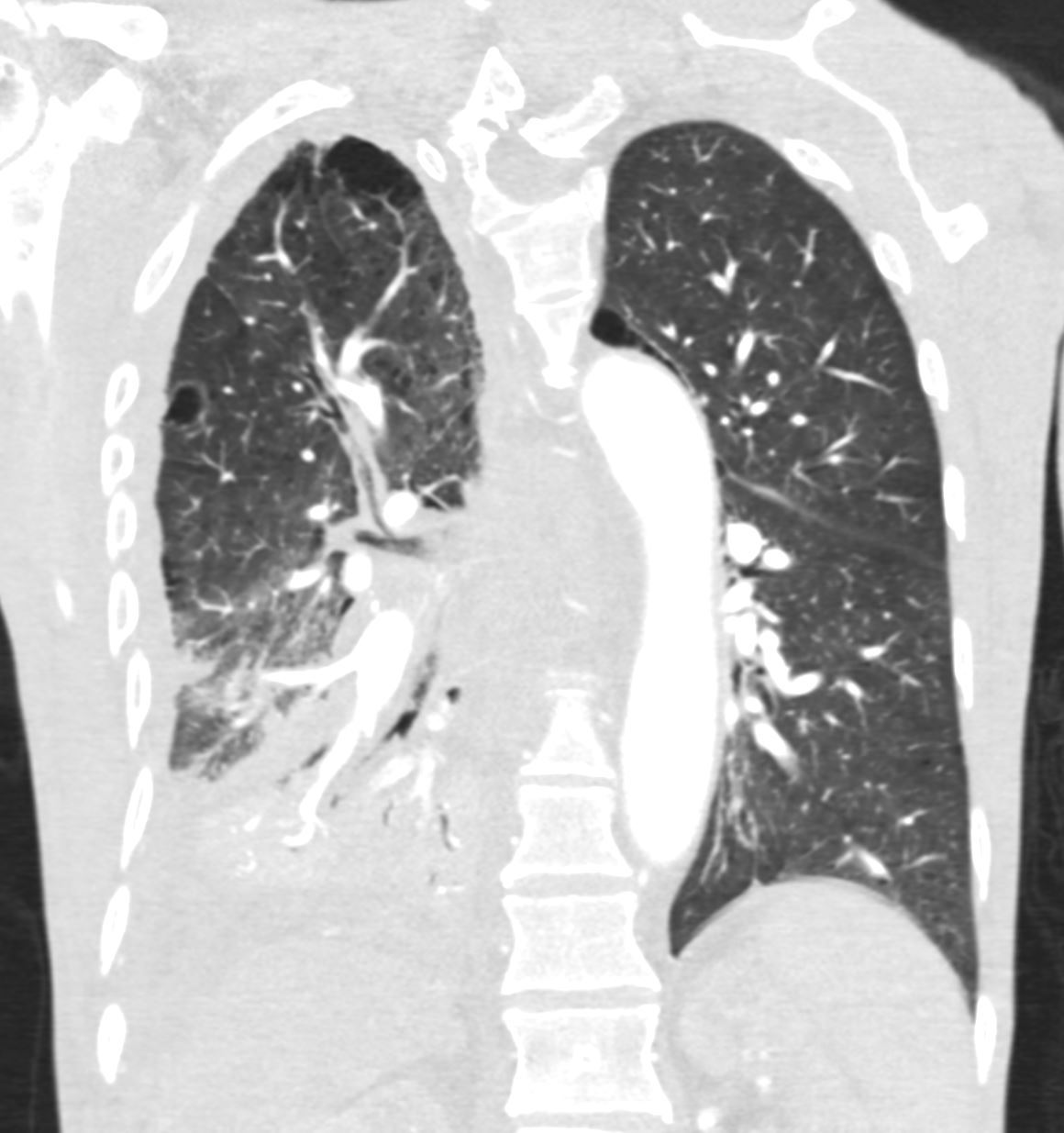
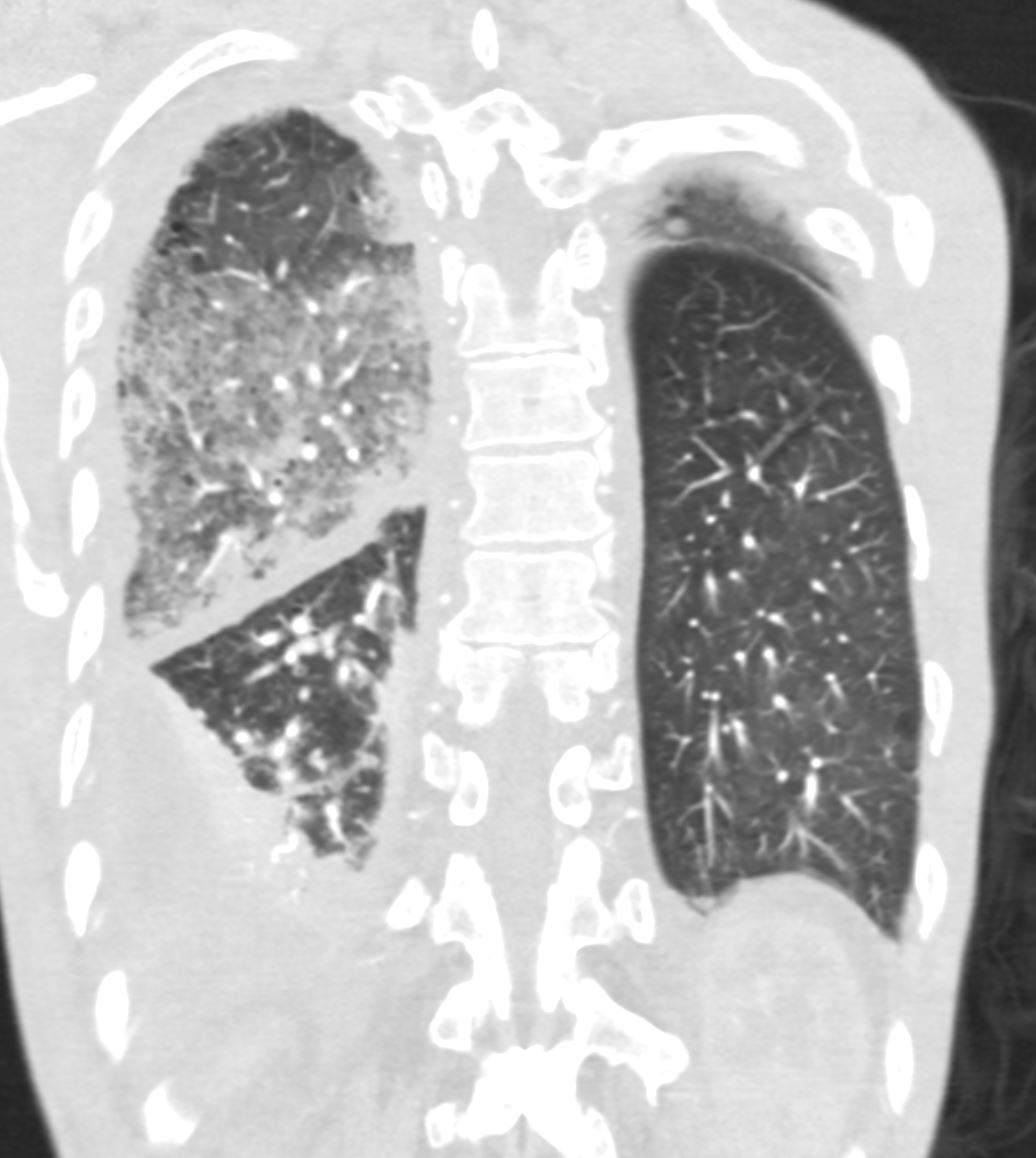
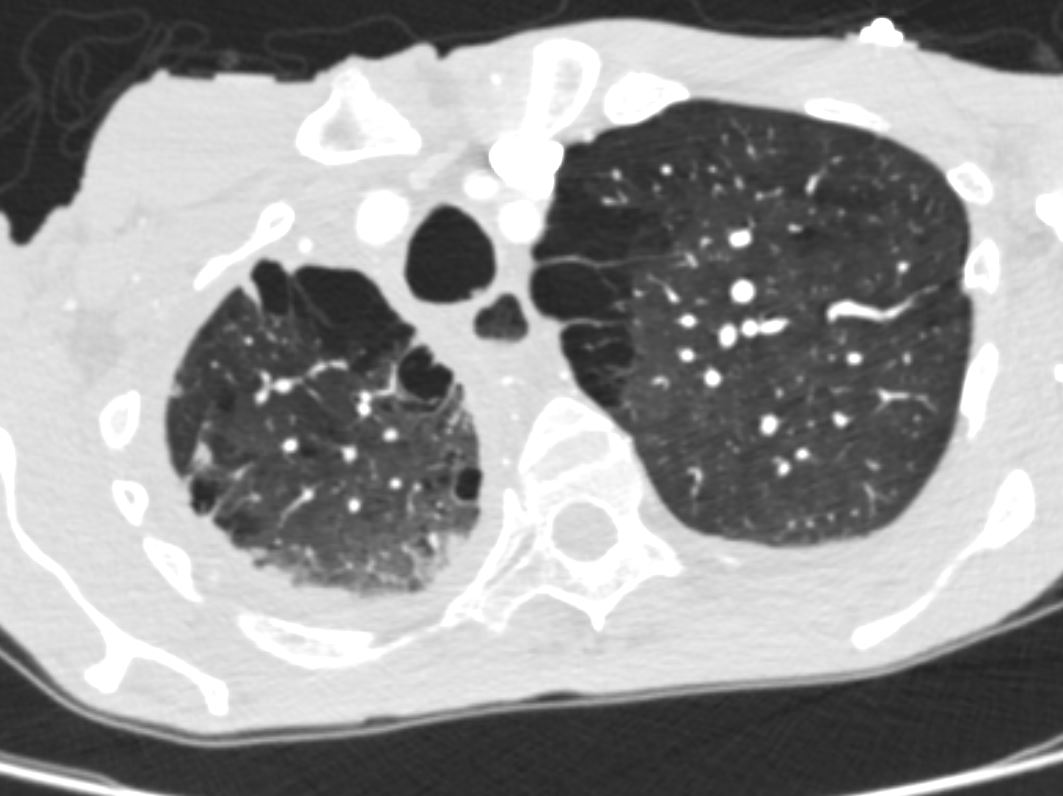
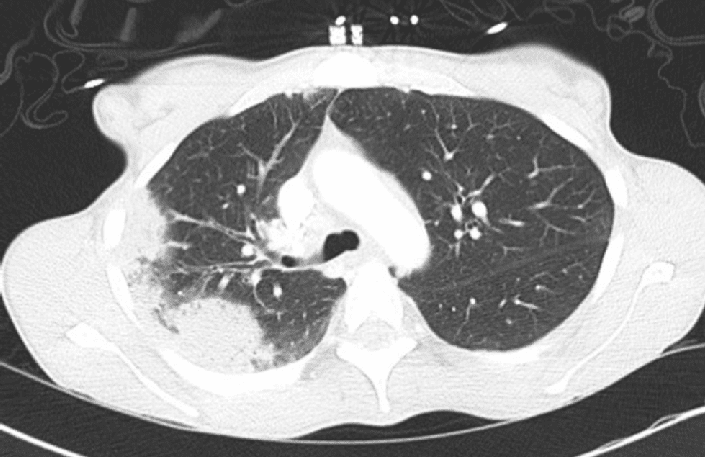
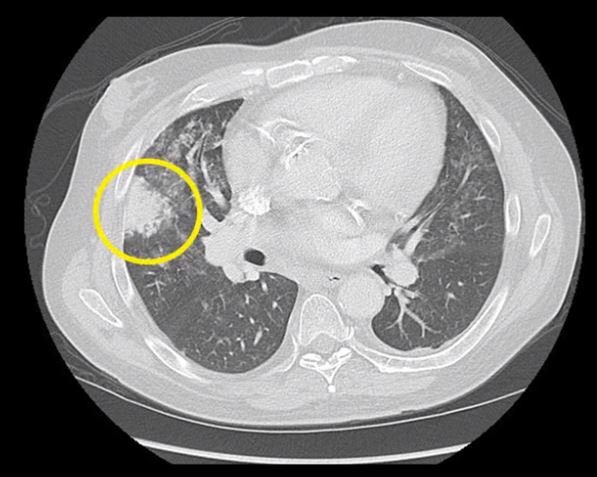
19 year old male previously well with history of hemoptysis, sweating, fevers, myalgias, arthritis over 3 weeks.
CT scan in the axial projection shows diffuse bilateral nodular consolidations with subpleural sparing consistent with pulmonary hemorrhage. Air bronchograms are noted in the posterior segment of the right upper lobe (b ringed in c) and the superior segment of the right lower lobe (b ringed in c)
Labs showed ANCA positivity, acute renal failure (creatinine 6) and renal biopsy showed crescentic glomerulonephritis. These finding are consistent with a diagnosis of GPA. He was treated with cyclophosphamide
Ashley Davidoff MD TheCommonVein.net 139185cL
Subsegmental and Patchy Consolidation

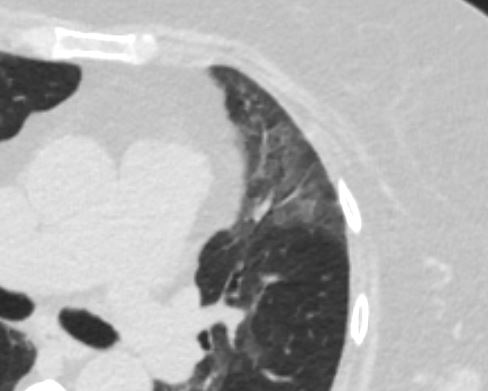
Note a subsegmental consolidation in the anterior segment of the left upper lobe in a 43 year old man with known aspergillus infection. Note the thickening of the walls of the segmental subsegmental and small airways with bronchiectasis and bronchiolectasis. There are centrilobular nodules indicating the small airway disease
Ashley Davidoff MD TheCommonVein.net 117811c

Patchy Consolidation
CT Patchy Consolidation
TB
Ashley Davidoff MD TheCommonVein.net
Ashley Davidoff MD TheCommonVein.net
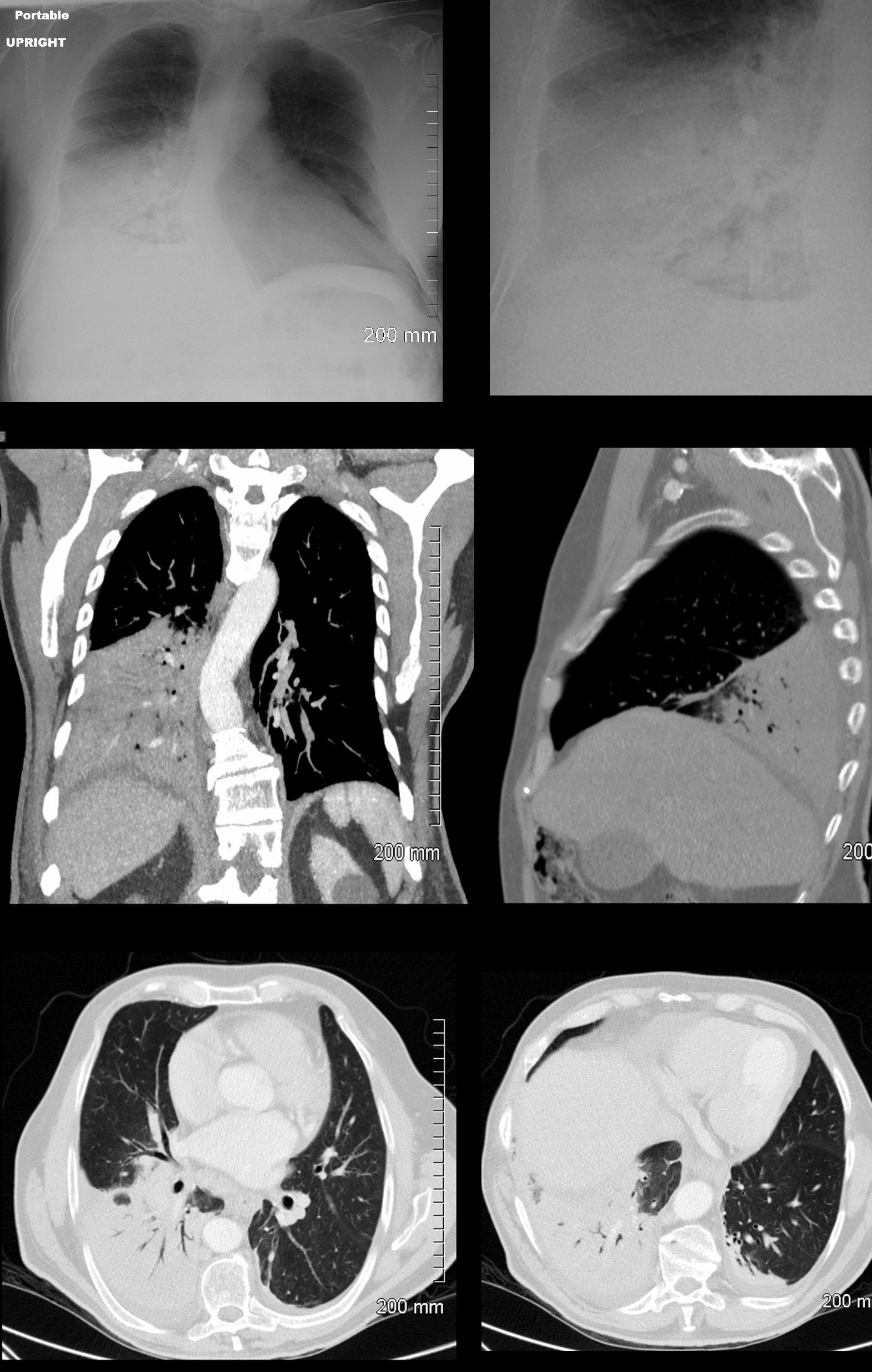
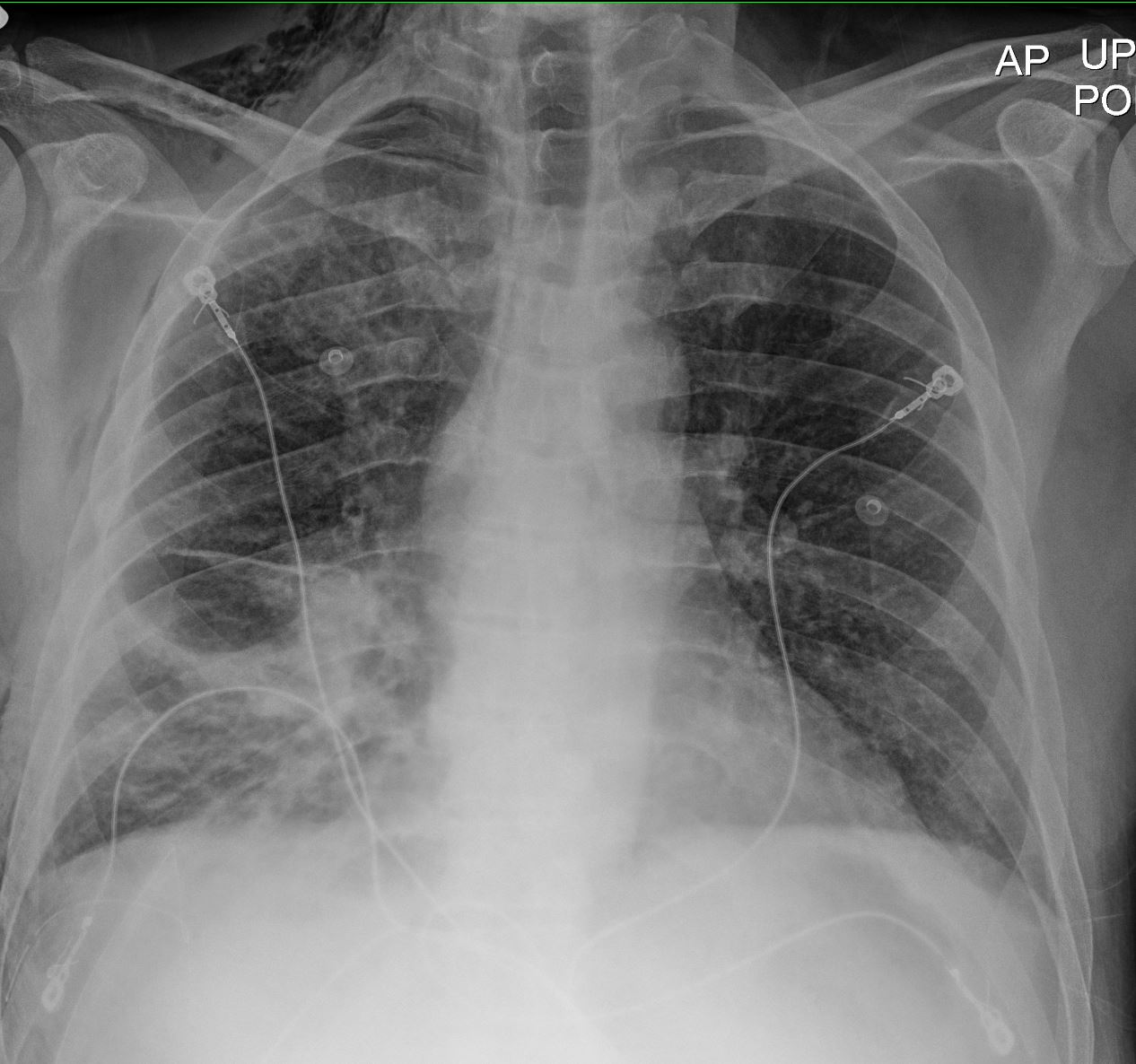
Lobar Consolidation
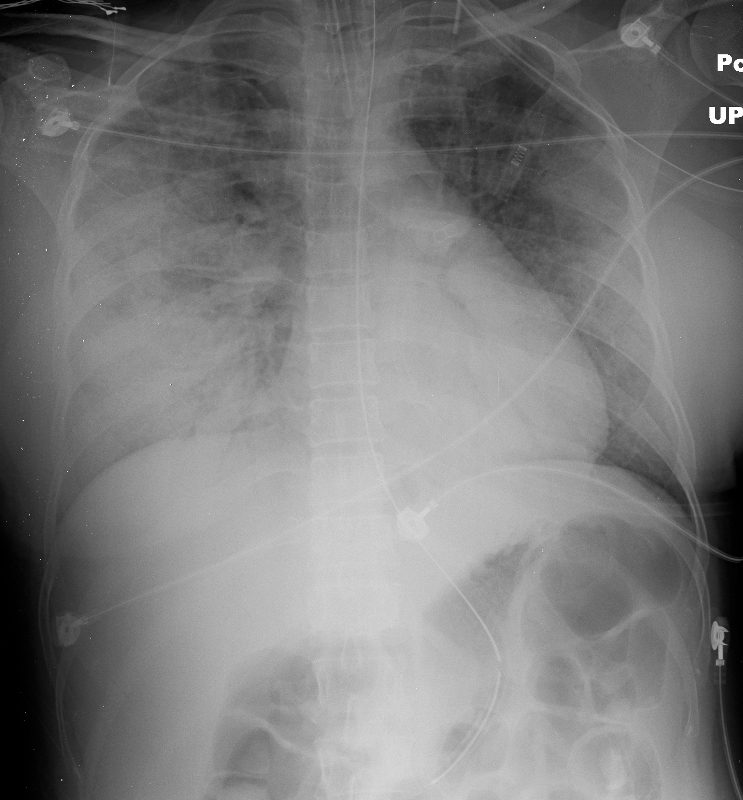
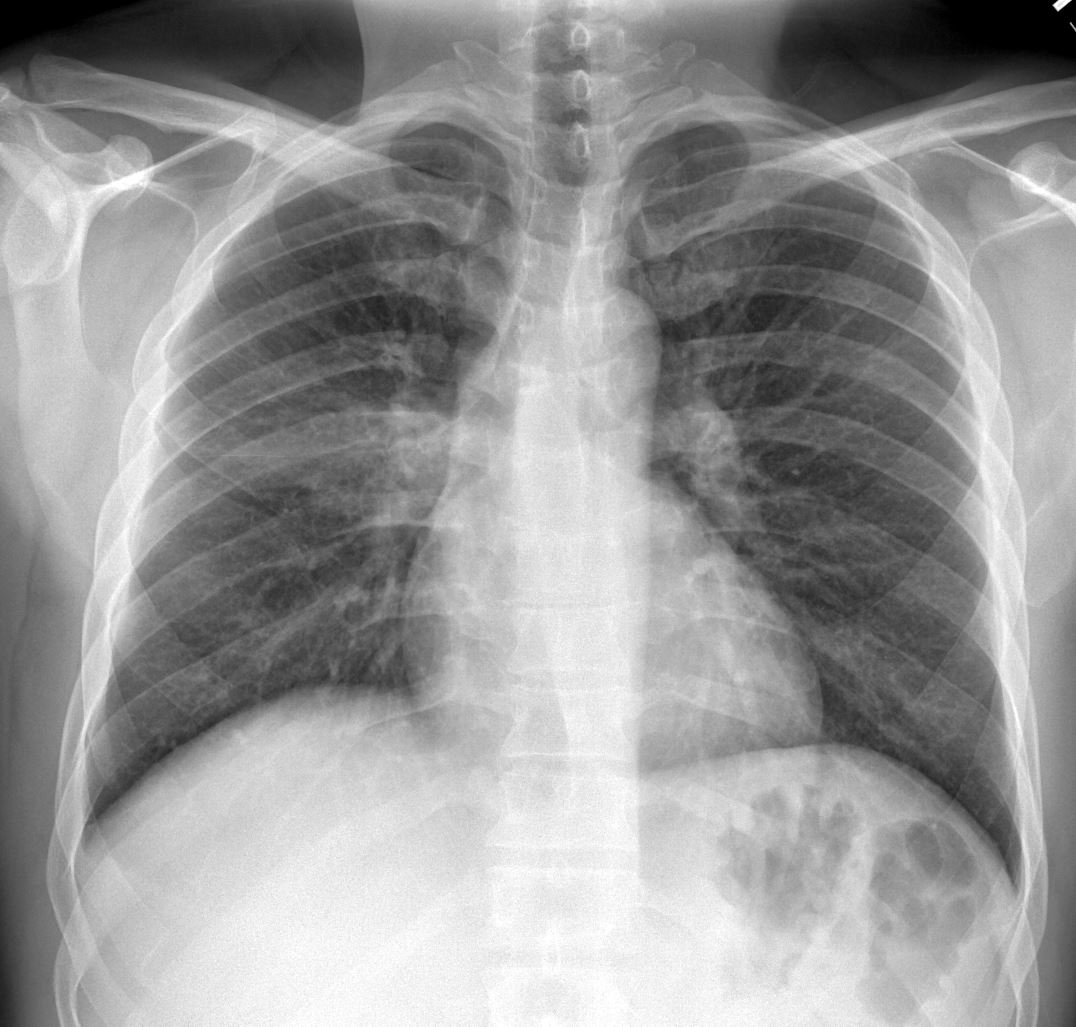
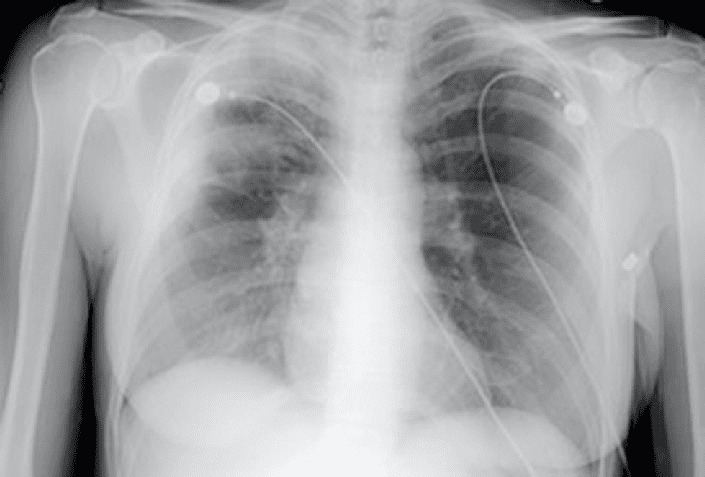
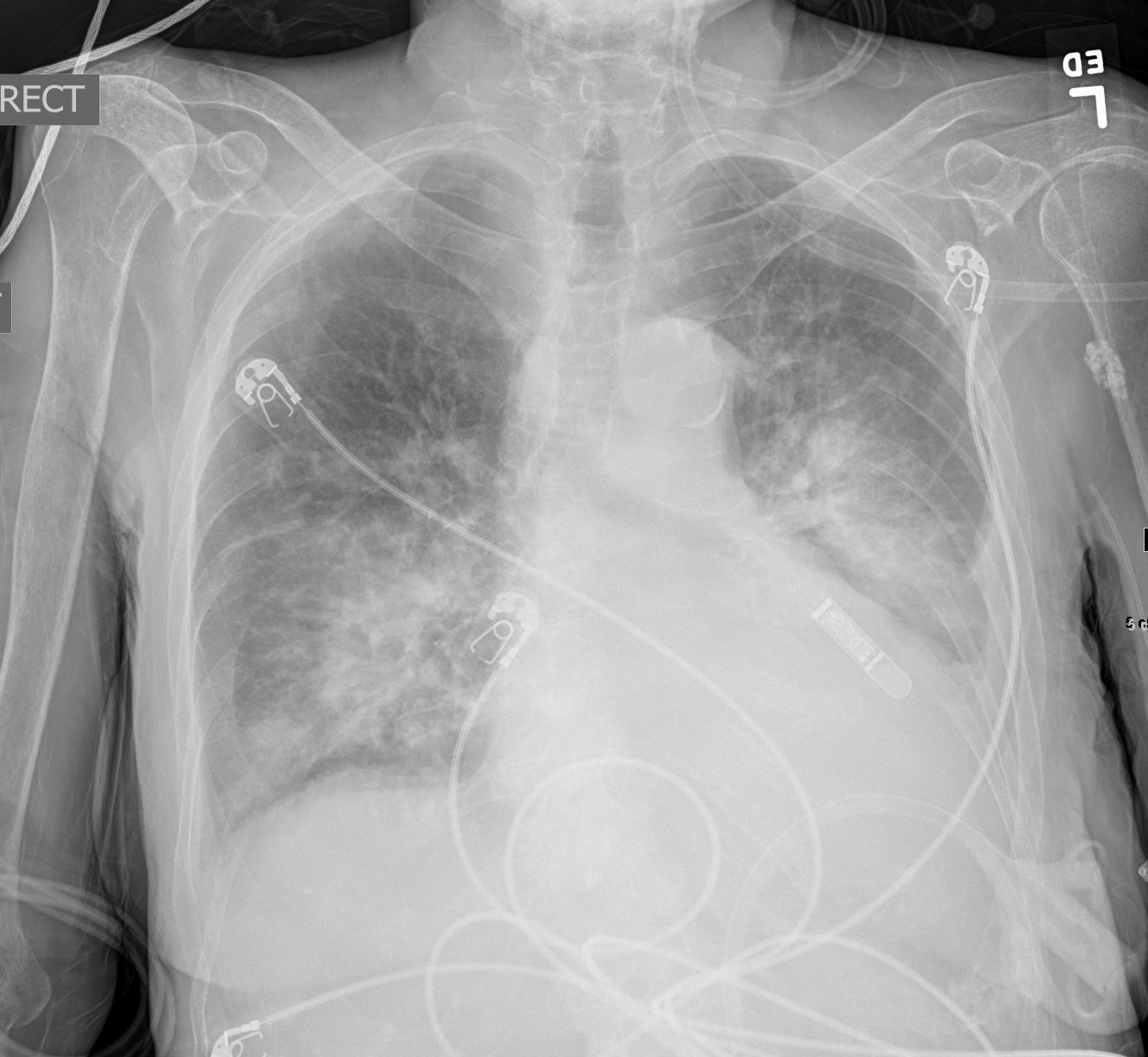
50 year old female with HIV presents with dyspnea. CXR shows extensive multifocal pneumonia with air bronchograms in the right upper and lower lobes as well as the left lower lobe. The patient required intubation
Ashley Davidoff MD TheCommonVein.net 134685
Involving Multiple Lobes and Segments
Ashley Davidoff TheCommonVein.net Ashley Davidoff TheCommonVein.net RML RLL 002
Ashley Davidoff TheCommonVein.net Ashley Davidoff TheCommonVein.net RML RLL 003
Ashley Davidoff TheCommonVein.net Ashley Davidoff TheCommonVein.net RML RLL 004
Ashley Davidoff TheCommonVein.net Ashley Davidoff TheCommonVein.net RML RLL 004
Ashley Davidoff TheCommonVein.net RML RLL 005
Ashley Davidoff TheCommonVein.net RML RLL 006
Peripheral Consolidation
Chronic Eosinophilic Pneumonia
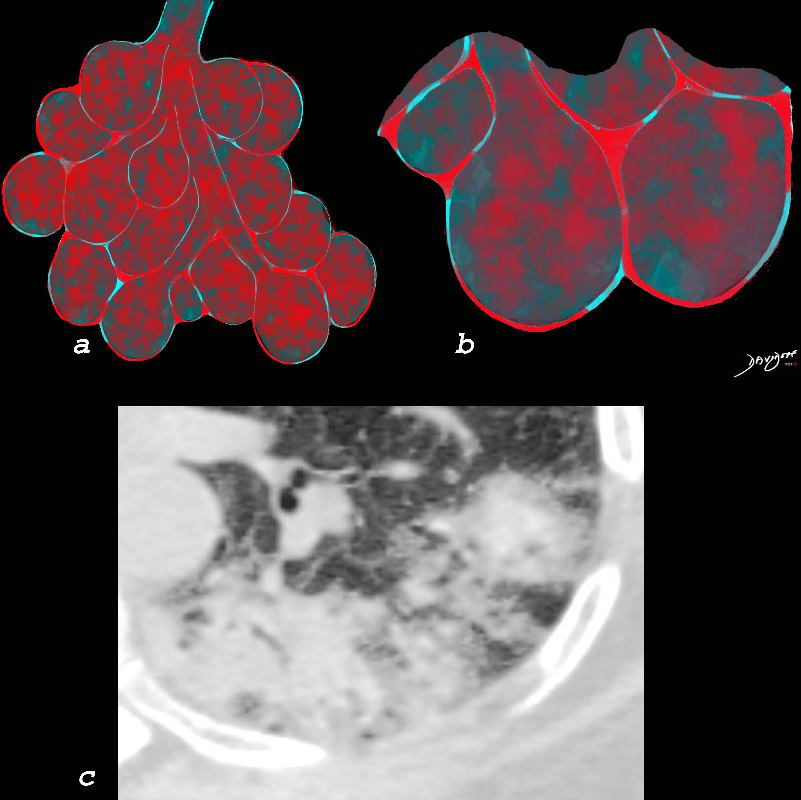
Chronic eosinophilia is characterised by alveolar filling with eosinophils and inflammatory exudates(a) and interalveolar interstitial thickening, (overlaid in red in b). The infiltrates are classically peripherally positioned, usually upper lobes, more commonly bilateral but can be unilateral, and manifest as consolidation and or ground glass opacities. The CT shows a peripheral consolidation in the left upper lobe
Ashley Davidoff MD The CommonVein.net lungs-0764
Crowe M et al Therapeutics and Clinical Risk Management Volume 15:397-403 March 2019 Research Gate
Crowe M et al Therapeutics and Clinical Risk Management Volume 15:397-403 March 2019 Research Gate
Crowe M et al Therapeutics and Clinical Risk Management Volume 15:397-403 March 2019 Research Gate
Aspiration
Lobar Consolidation
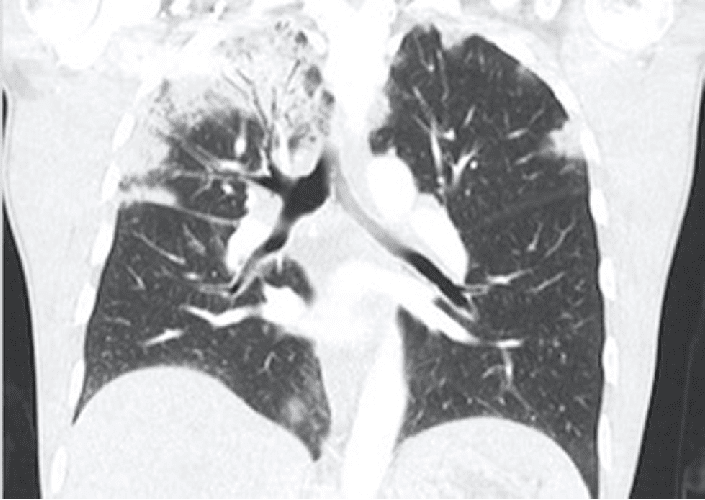
74 year old male alcoholic with bilateral basilar lobar atelectasis caused by bilateral aspiration
CT scan shows airless lower lobes with small bilateral effusions. 3D reconstruction shows total obstruction of the right mainstem bronchus, and patent proximal mainstem bronchus
Ashley Davidoff MD TheCommonVein.net
Segmental Consolidation
Subsegmental or Focal Consolidation
Focal consolidations or infiltrates are another feature of interstitial lung disease (yellow ring with obscuration of the airways and vessels

40 year old male with SLE presented with chest pain and dyspnea and initial CXR showed a vague retrocardiac density
A CT scan that followed showed occlusive pulmonary emboli to the left lower lobe (circled in white) associated with a wedge shaped infarct or focal consolidation (red arrowhead)
Ashley Davidoff MD
Circulatory Causes – Fluid Filled Alveoli
70 year old female s/p cardiac arrest and ROSC. CXR shows centralised alveolar edema as a result of intra- alveolar accumulation of transudate. The centralized distribution of the infiltrates is characteristic of severe heart failure – batwing distribution
Ashley Davidoff MD TheCommonVein.net
Ground Glass Consolidation from COP
Pathology proven diagnosis
Ashley Davidoff MD TheCommonVein.net
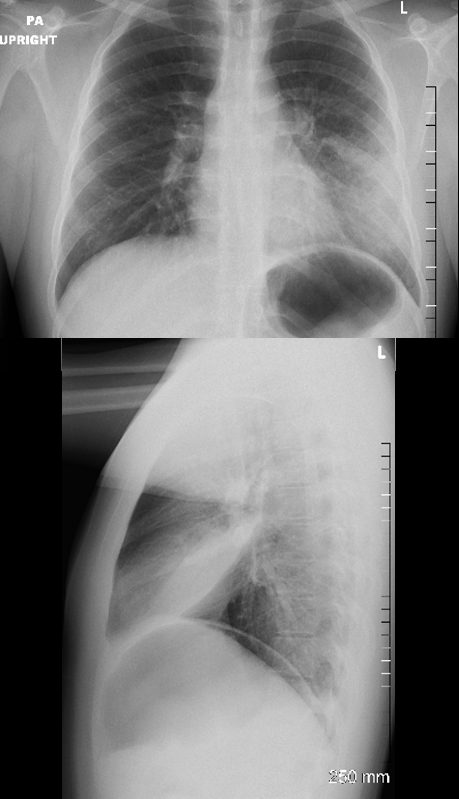
Hemorrhage Trauma
Extensive Ground Glass Changes and Consolidation following Trauma Presents with Hemoptysis On Anticoagulation for AVR No Fever No White Count Ashley Davidoff MD TheCommonVein.net
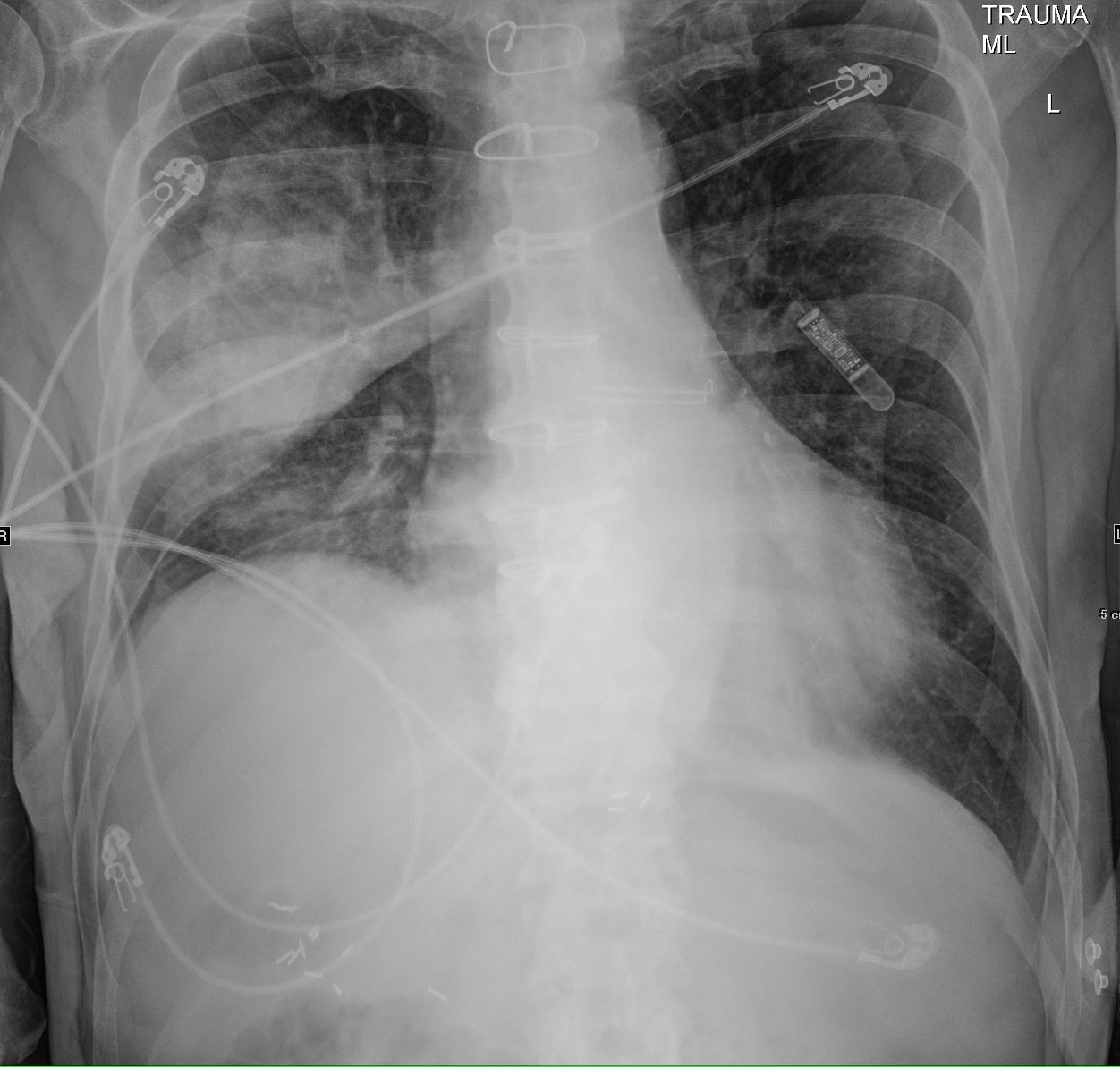
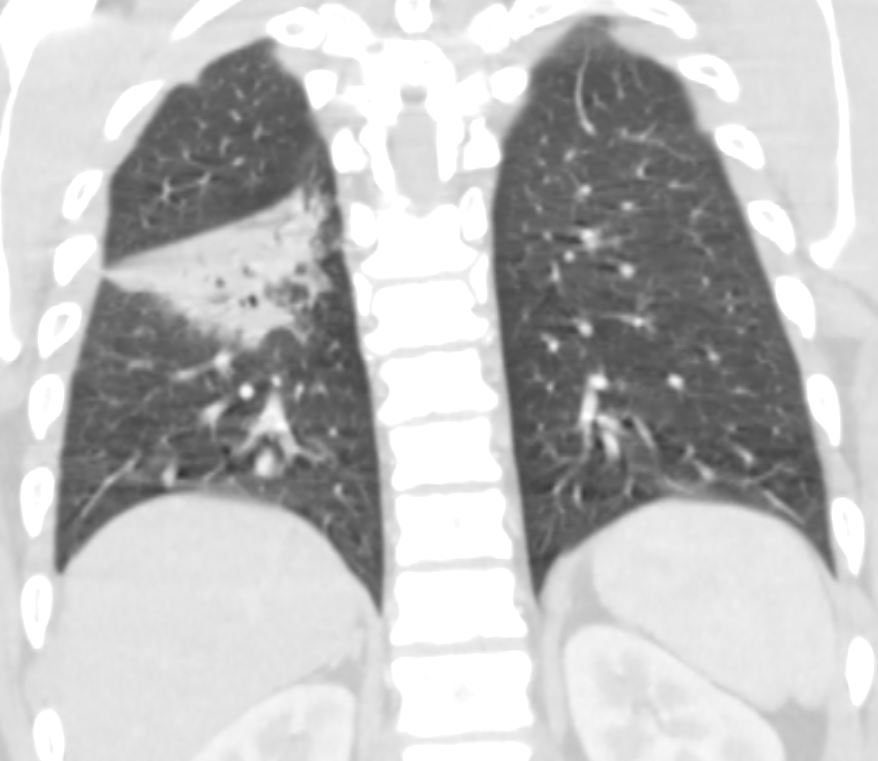
CXR shows an elevated right hemidiaphragm and inferior displacement of the major fissure with a dense right upper lobe consolidation. The mass effect on the major fissure likely results from a hematoma, and the hemorrhage results in air bronchograms and groundglass changes.
Skin folds manifest as bilateral pseudo-pneumothoraces. A loop recorder is noted overlying the left upper chest.
Ashley Davidoff MD TheCommonVein.net 165Lu 135849
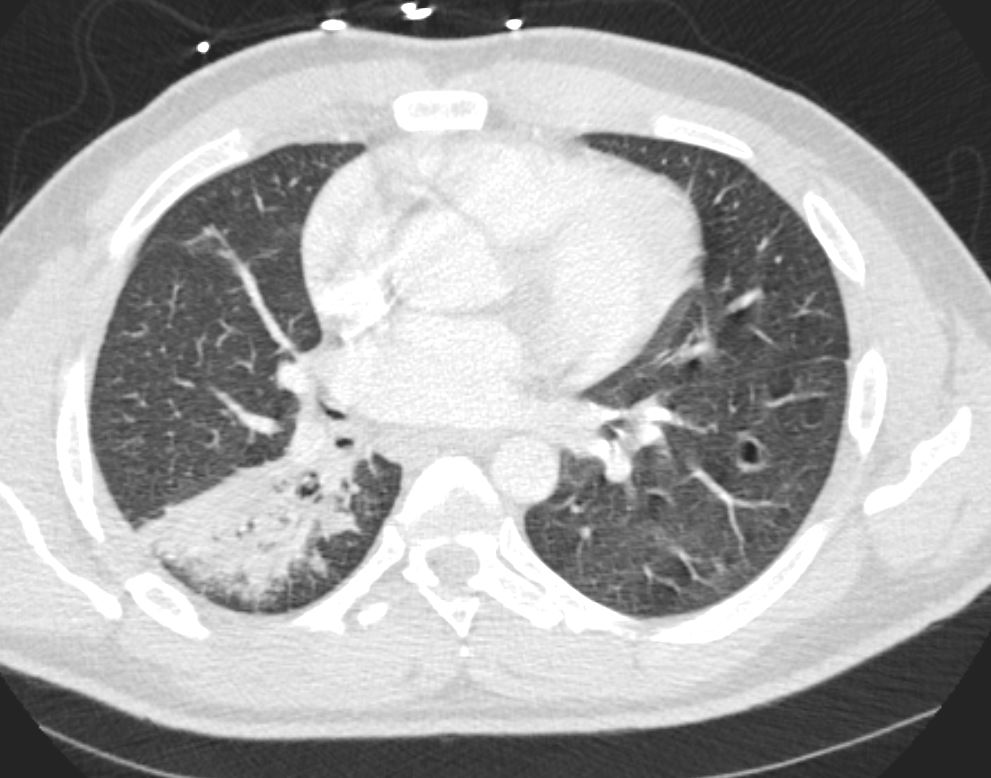
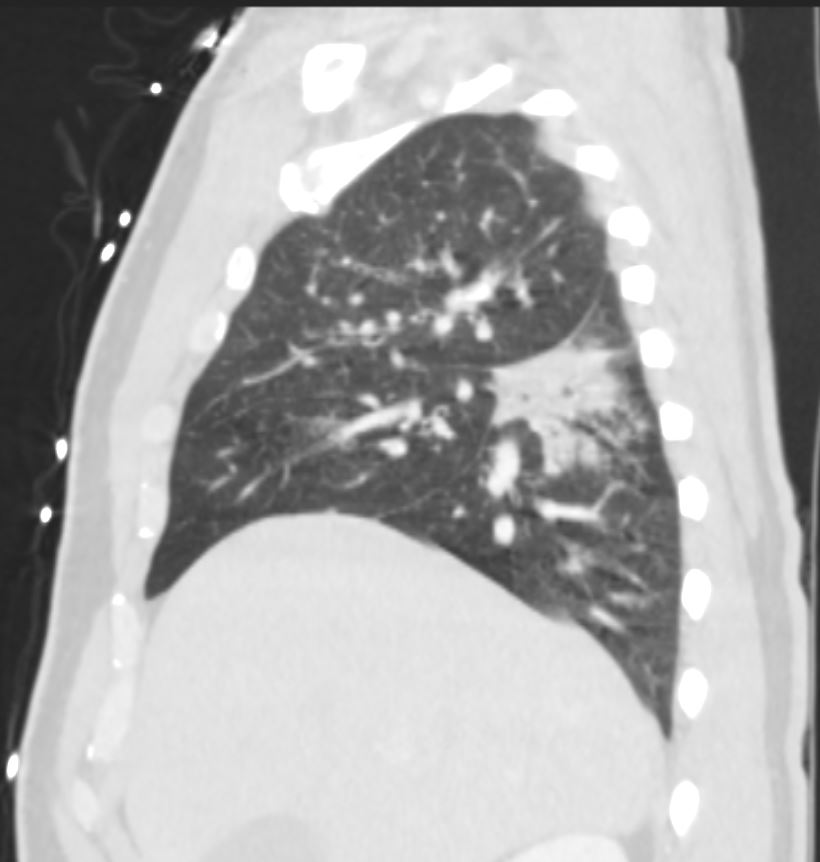
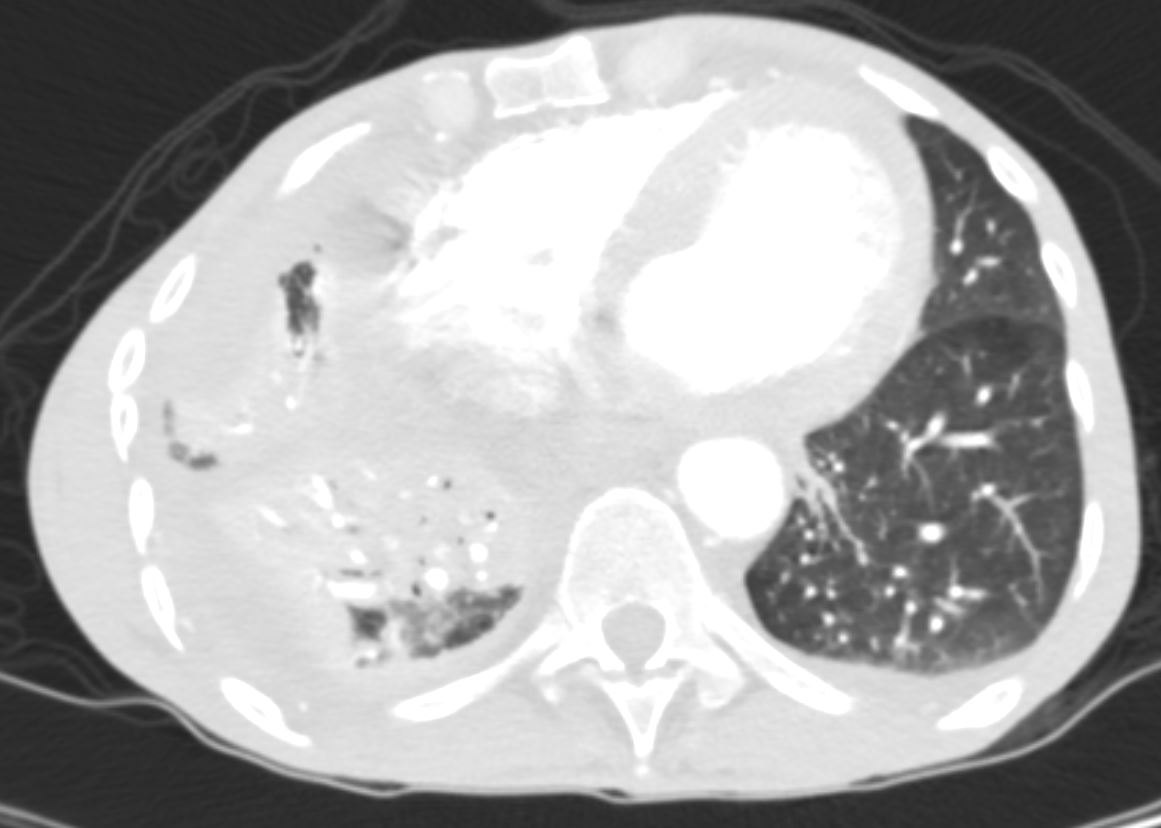
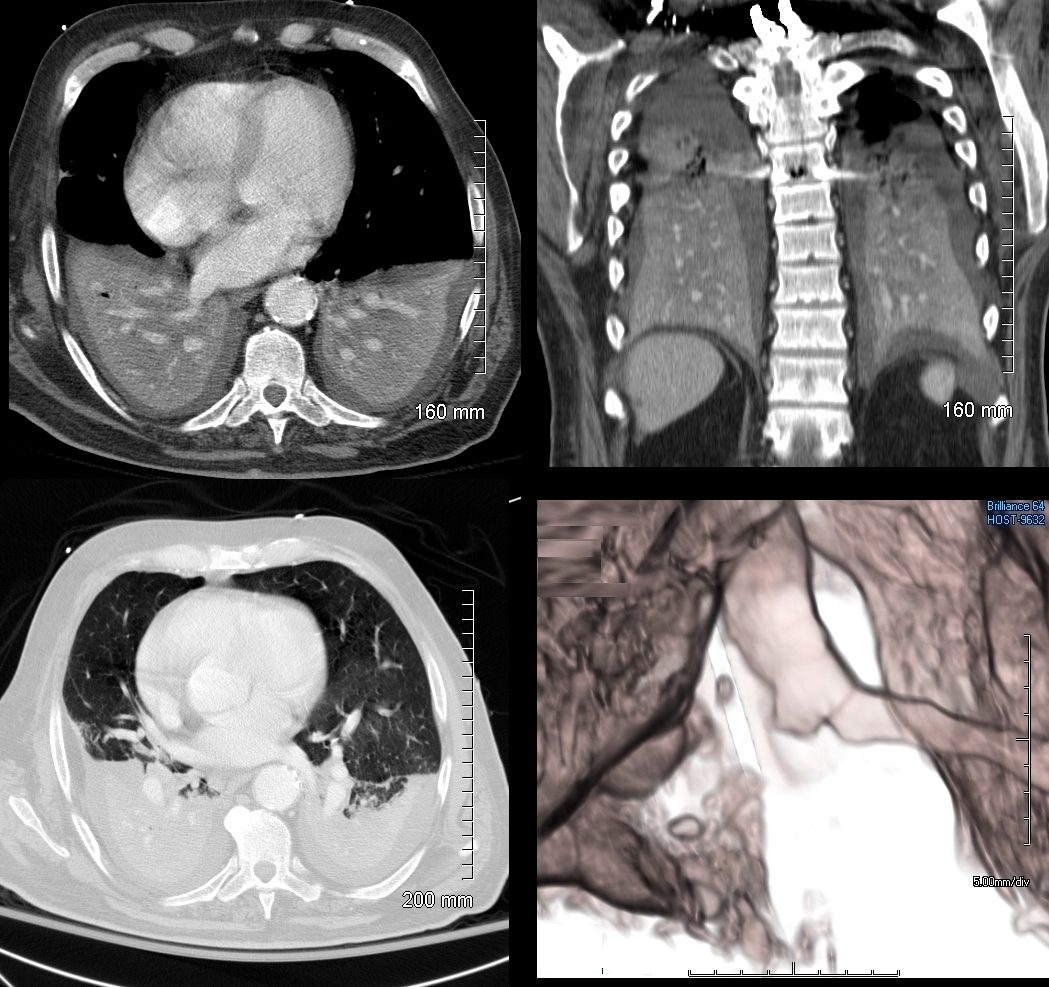
75-year-old man on blood thinners s/p aortic valve replacement, s/p trauma, presents with hemoptysis. He was afebrile and without an elevated white count
Coronal CT of the posterior lung fields shows inferior displacement of the major fissure by a dense right upper lobe consolidation. The mass effect on the major fissure likely results from a hematoma. Lateral to the consolidation there is a combination of ground glass opacity. There is elevation of the right hemidiaphragm. Left sided pleural effusion is present
Ashley Davidoff MD TheCommonVein.net 165Lu 135860
Pulmonary Hemorrhage – Heterogeneity of the Secondary Lobule
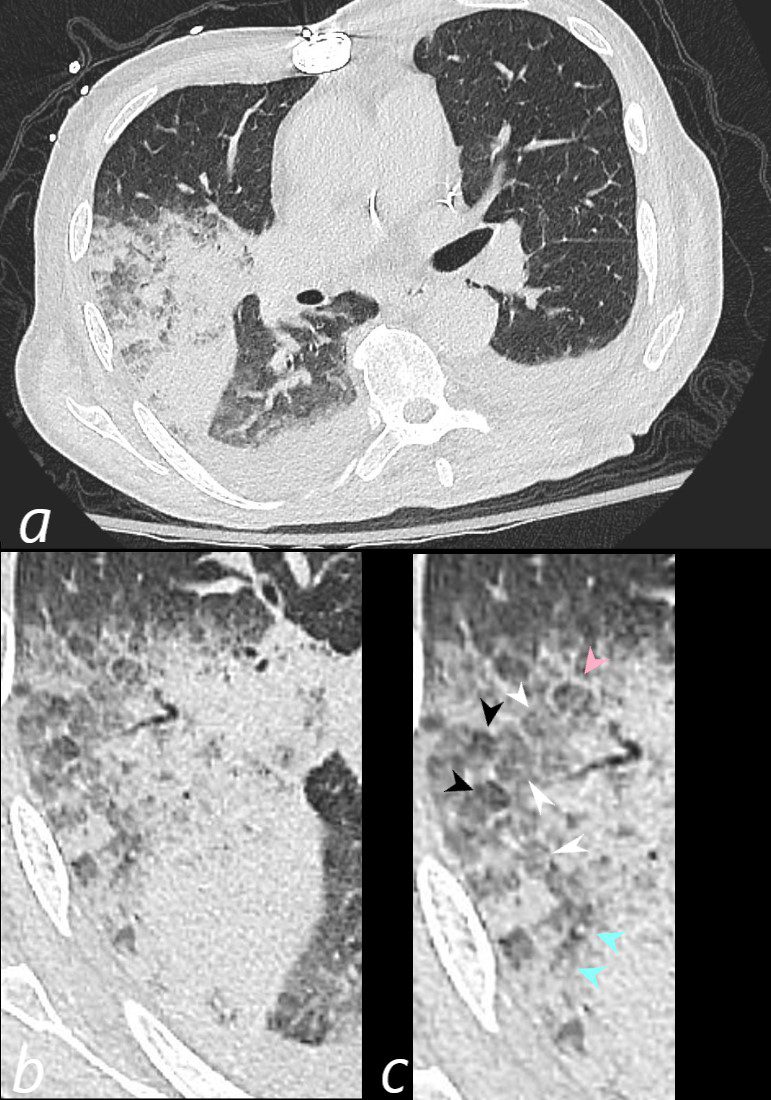
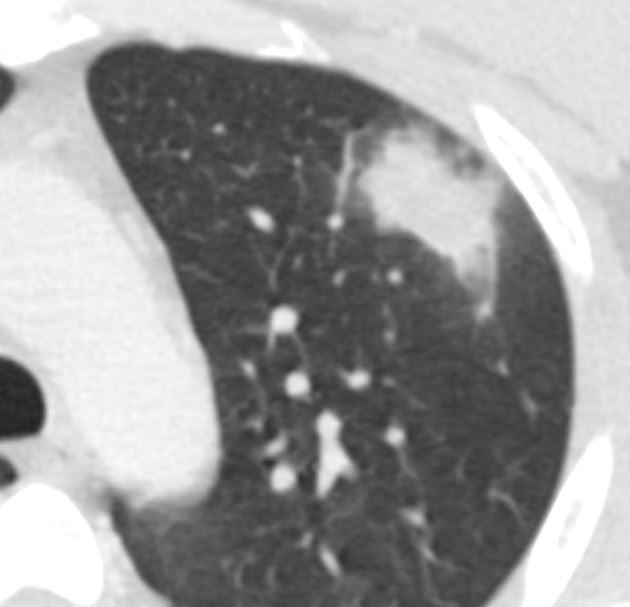
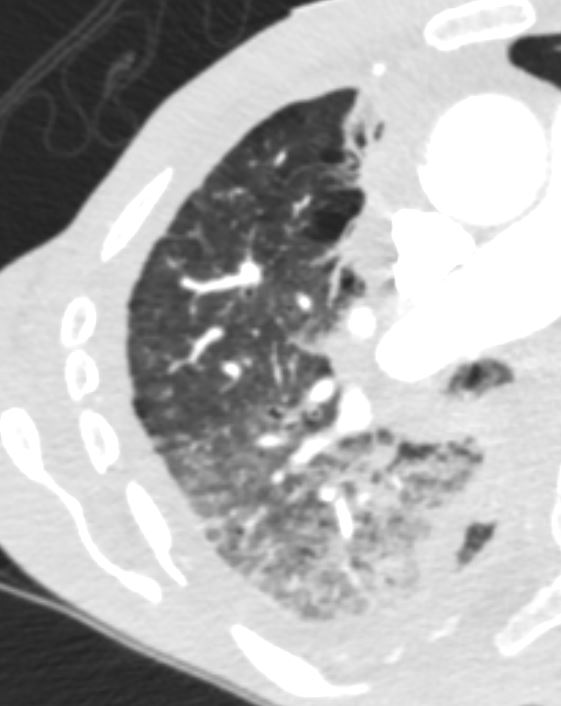
75-year-old man on blood thinners s/p aortic valve replacement presents with hemoptysis s/p trauma. He was afebrile and without an elevated white count
Axial CT at the level below the carina shows medial displacement of the major fissure by a dense right upper lobe consolidation. The mass effect on the major fissure likely results from a hematoma. Anterior to the consolidation there is a combination of ground glass opacity with thickened interlobular septa, and minor region of subsegmental consolidation with air bronchograms, likely resulting from hemorrhage.
The lower panels magnify the regions of the heterogeneity of the secondary lobule with most showing ground glass changes, some normal or with mosaic attenuation (black arrowheads, c), some showing thickened smooth interlobular septa (pink arrowhead, c) and others revealing centrilobular nodules (teal arrowheads, c).
There are bilateral effusions
Ashley Davidoff MD TheCommonVein.net 165Lu 135851cL
Pulmonary Hemorrhage – Heterogeneity of the Secondary Lobule
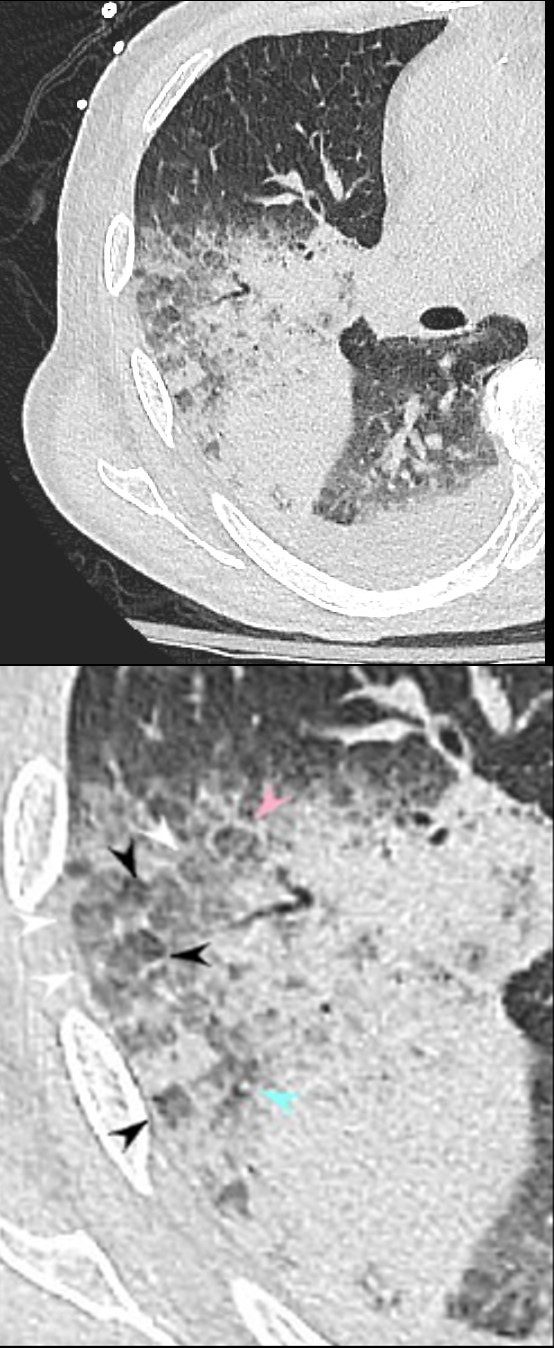
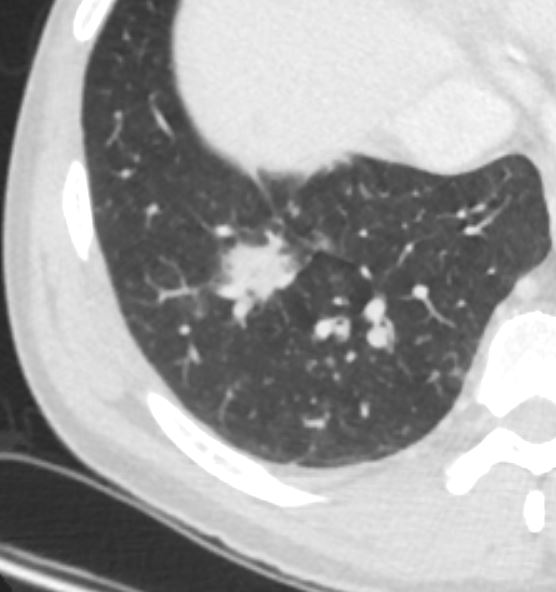
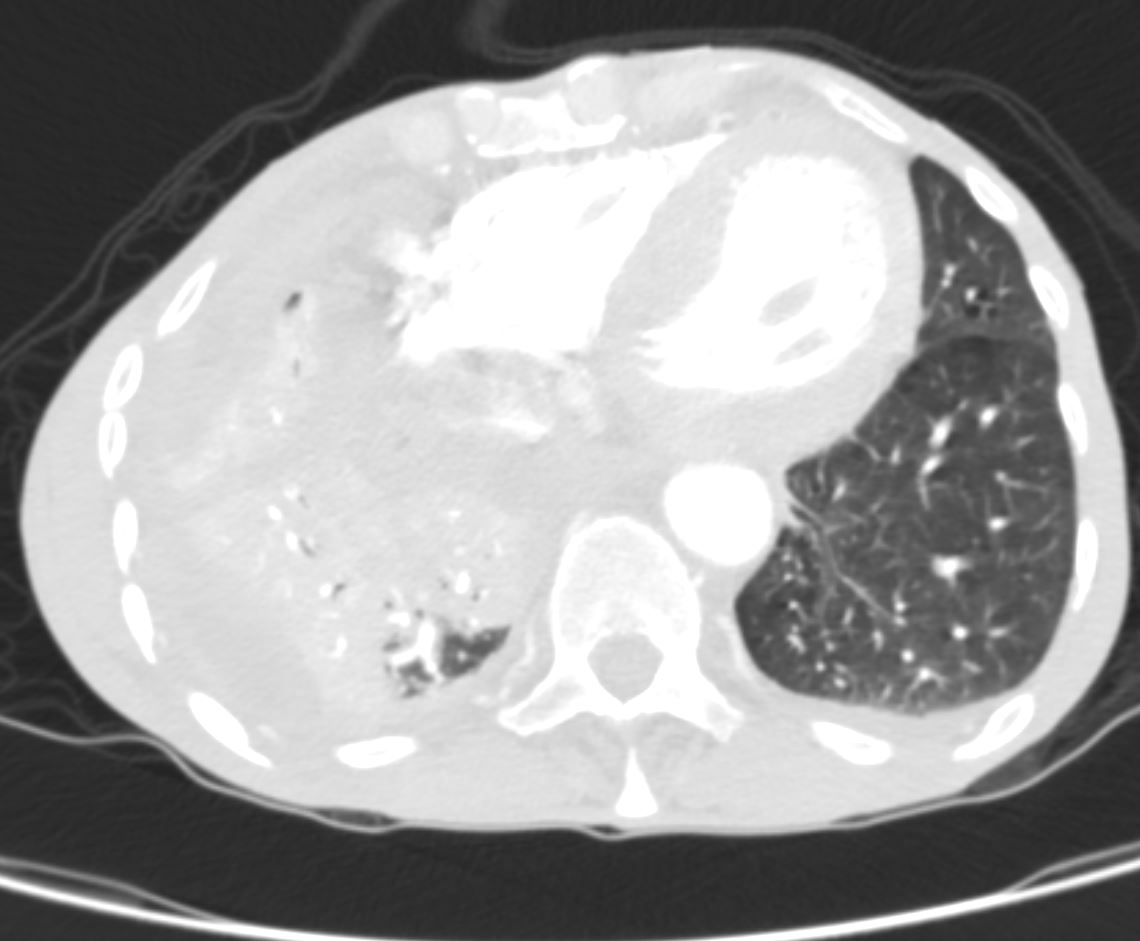
75-year-old man on blood thinners s/p aortic valve replacement, s/p trauma, presents with hemoptysis. He was afebrile and without an elevated white count
Axial CT at the level below the carina shows medial displacement of the major fissure by a dense right upper lobe consolidation. The mass effect on the major fissure likely results from a hematoma. Anterior to the consolidation there is a combination of ground glass opacity with thickened interlobular septa, and minor region of subsegmental consolidation with air bronchograms, likely resulting from hemorrhage.
The lower panel magnifies the regions of the heterogeneity of the secondary lobule with most showing ground glass changes (white arrowheads), some normal or with mosaic attenuation (black arrowheads), some showing thickened smooth interlobular septa (pink arrowhead), and others revealing centrilobular nodules (teal arrowhead).
There are bilateral effusions
Ashley Davidoff MD TheCommonVein.net 165Lu 135852cL
Pulmonary Hemorrhage – Heterogeneity of the Secondary Lobule
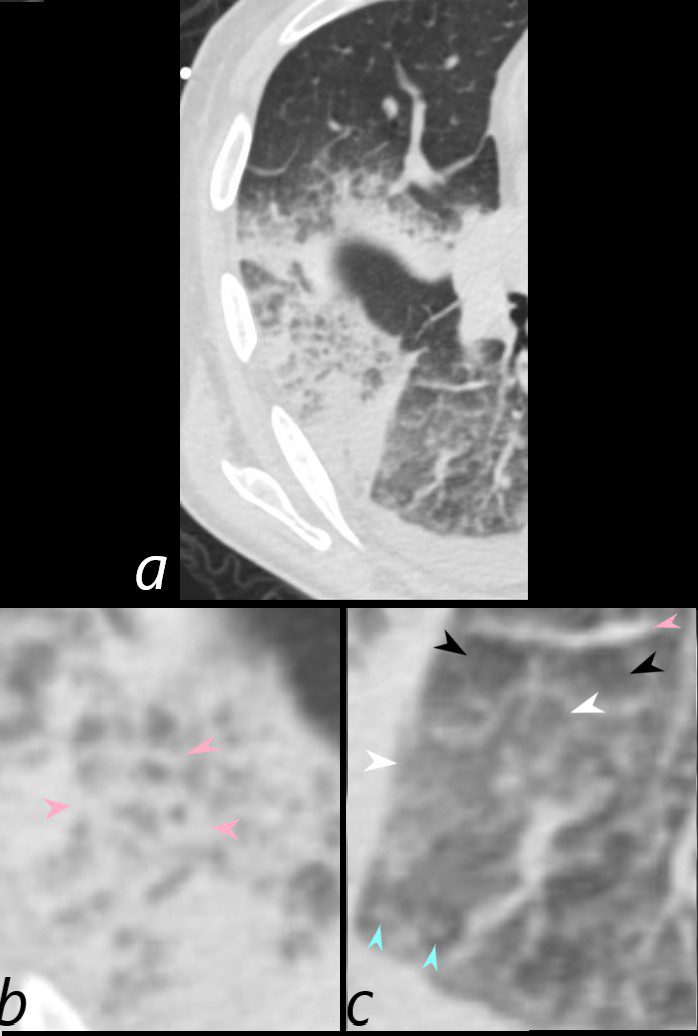
75-year-old man on blood thinners s/p aortic valve replacement, s/p trauma, presents with hemoptysis. He was afebrile and without an elevated white count
Axial CT at the level below the carina at the inferior aspect of the hematoma shows heterogenous changes of the secondary lobules. The changes in the post segment of the right upper lobe (b) show significantly thickened interlobular septa (pink arrowheads) and relatively small secondary lobules caused by the compression of the hematoma. The changes in the apical segment of the lower lobe (c) show a combination of secondary lobules with ground glass changes (white arrowheads) some normal or with mosaic attenuation (black arrowheads), some showing mildly thickened smooth interlobular septa (pink arrowheads), and others revealing centrilobular nodules (teal arrowheads).
There is a right sided effusion
Ashley Davidoff MD TheCommonVein.net 165Lu 135853cL
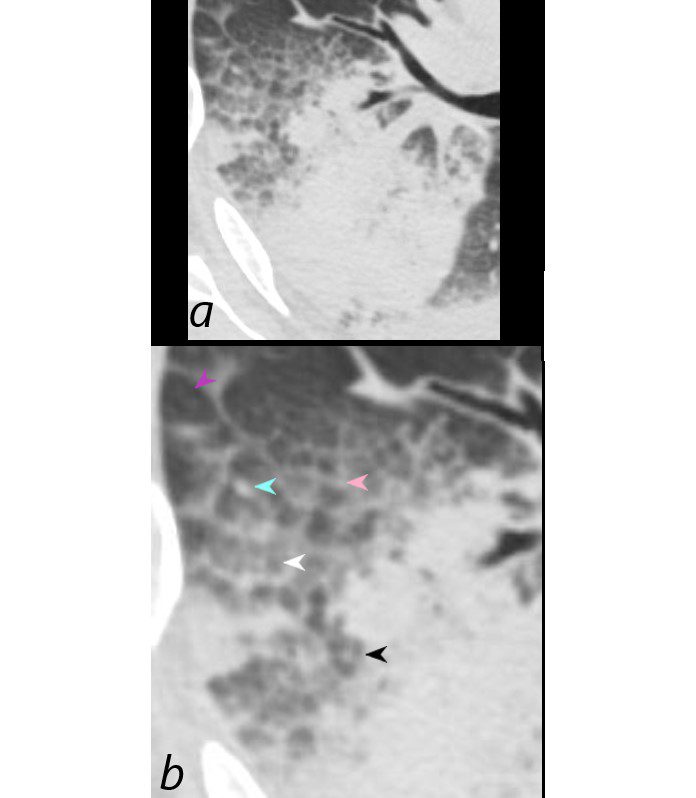
Axial CT at the level below the carina shows heterogenous changes of the secondary lobules. The changes in the post segment of the right upper lobe (a, and magnified in b) show thickened interlobular septa (pink arrowhead) and mostly relatively small secondary lobules caused by the compression of the hematoma, but also by virtue of their more centrally located position. Compare their size to the larger more peripherally located secondary lobule (purple arrowhead). There is also a combination of secondary lobules with ground glass changes (white arrowhead) some normal or with mosaic attenuation (black arrowheads), some showing mildly thickened smooth interlobular septa (pink arrowhead), and others revealing centrilobular nodules (teal arrowhead).
Ashley Davidoff MD TheCommonVein.net 165Lu 135854cL
Cavitation
Staph Aureus
Ashley Davidoff MD TheCommonVein.net cavitating pneumonia 59M 02

Ashley Davidoff MD TheCommonVein.net cavitating pneumonia 59M
Causes
-
-
Infection
-
Neoplasm
- adenocarcinoma with lepidic growth
- primary pulmonary lymphoma
-
Aspiration
-
CHF
-
In ILD
- organizing pneumonia TCV
- sarcoidosis TCV
- Wegener’s granulomatosis
-
Eosinophillic Pneumonia
-
Lipoid Pneumonia
-
Links and References
Haroon A et al Differential Diagnosis of Non-Segmental Consolidations J Pulmon Resp Med 2013