-
-
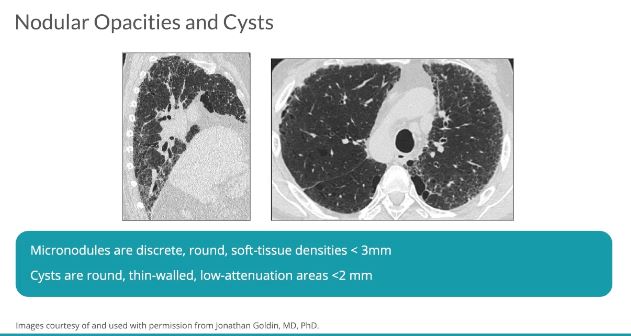
TCV Definition: Lung Cyst
- Etymology
Derived from the Greek word “kystis,” meaning bladder or sac. - AKA
Pulmonary cyst - Definition
- What is it?
A lung cyst is a gas-filled space within the lung parenchyma, characterized by a thin, perceptible wall typically less than 2-4 mm in thickness. These cysts can vary in size and distribution and are associated with a wide range of underlying conditions. - Caused by
- Most common causes
- Smoking-related diseases
- Pulmonary Langerhans cell histiocytosis (PLCH): A frequent cause in smokers, typically with upper lobe predominance and cysts of varying wall thickness.
- Emphysema-related bullae: Large, thin-walled air-filled spaces caused by parenchymal destruction in smokers.
- Congenital disorders
- Congenital pulmonary airway malformation (CPAM): Seen in pediatric populations but may persist into adulthood.
- Bronchogenic cysts: Often incidental findings with well-defined, thin-walled cysts.
- Cystic lung diseases
- Lymphangioleiomyomatosis (LAM): Primarily affects women of childbearing age, characterized by diffuse cystic changes.
- Birt-Hogg-Dubé syndrome: Associated with basal-predominant cysts and genetic mutations in the folliculin gene.
- Smoking-related diseases
- Other causes include
- Infectious causes
- Pneumocystis jirovecii pneumonia (PJP): Common in immunocompromised patients, producing thin-walled cysts.
- Tuberculosis: Can produce thin-walled cavities resembling cysts.
- Post-viral pneumonias: Rarely associated with cyst formation.
- Inflammatory causes
- Pulmonary Langerhans cell histiocytosis (PLCH): Smoking-related, with irregular, thick- and thin-walled cysts predominantly in the upper lobes.
- Lymphoid interstitial pneumonia (LIP): Associated with lower lobe predominance and bronchovascular bundles.
- Sarcoidosis: Late-stage disease may cause cyst formation.
- Neoplastic causes
- Cystic adenocarcinoma of the lung: Malignant transformation presenting with cystic components.
- Metastatic disease: Rarely associated with thin-walled cystic changes.
- Other causes
- Trauma: Pneumatoceles following blunt trauma or infection.
- Drug-induced lung injury: Medications like methotrexate or amiodarone.
- Infectious causes
- Most common causes
- Resulting in
- Single cyst: Typically focal pathology such as neoplasm, trauma, or localized infection.
- Multiple cysts: Indicative of diffuse lung disease (e.g., LAM, PLCH) or systemic involvement.
- Potential complications: Include pneumothorax, secondary infection, and, rarely, malignant transformation.
- What is it?
Lymphangioleiomyomatosis (LAM),
- Etymology
- Langerhans cell histiocytosis (PLCH),
-

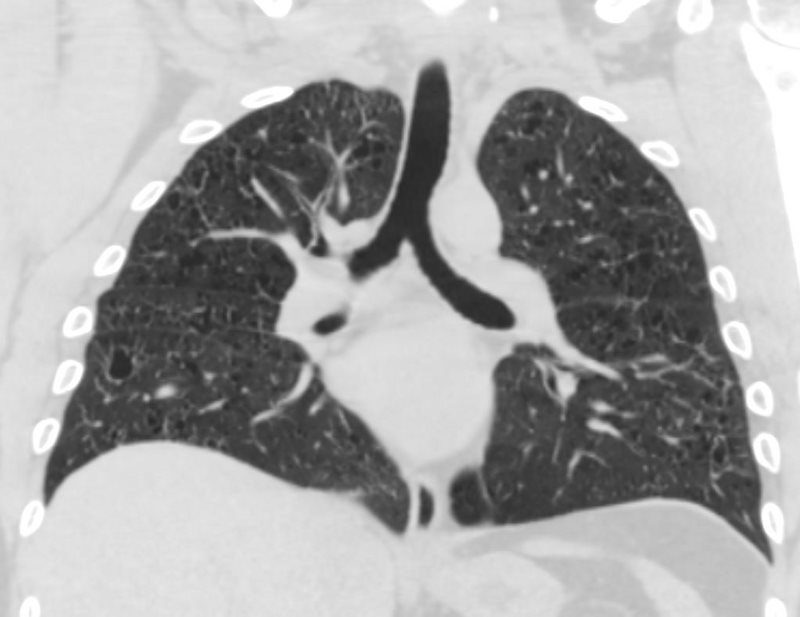
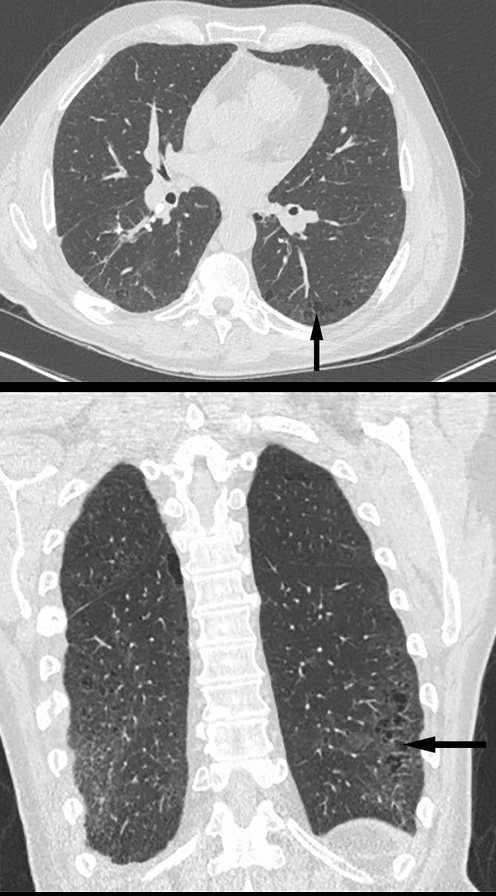
Pulmonary Langerhans Cell Histiocytosis
Thiin Walled Bizarre Shaped Upper Lobe Cysts
Ashley Davidoff MD TheCommonVein.net- Langerhans Cell Histiocytosis
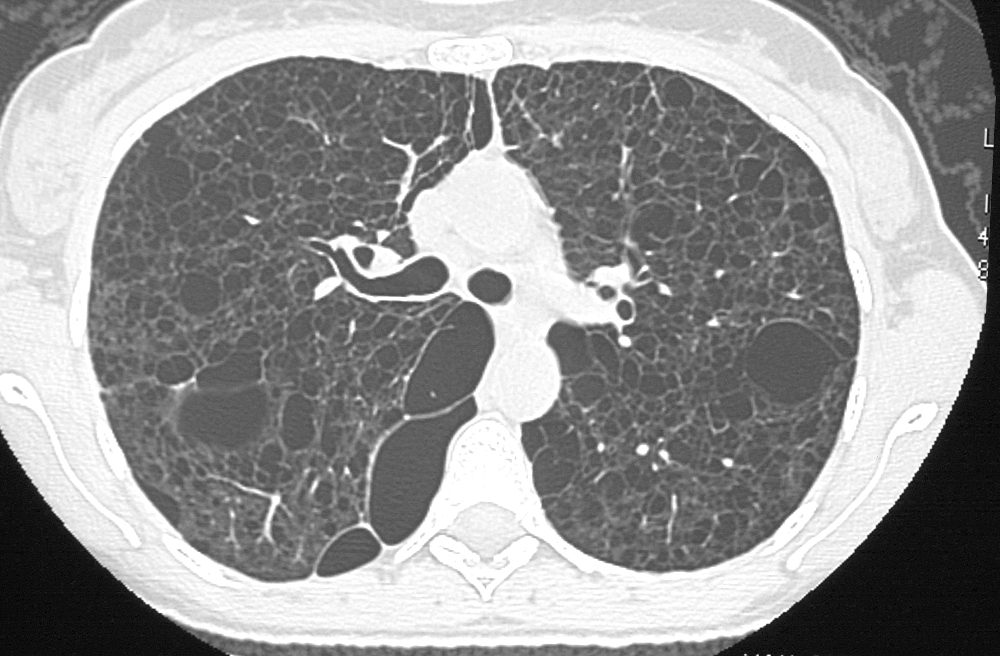
 CT scan shows multiple small cysts sometimes irregular in shape predominantly in the upper lobes. The cysts are round and air filled large and are between 5mm-8mm
CT scan shows multiple small cysts sometimes irregular in shape predominantly in the upper lobes. The cysts are round and air filled large and are between 5mm-8mm
- Langerhans Cell Histiocytosis
- Birt-Hogg-Dubé syndrome (BHD), and
- Lymphoid interstitial pneumonia (LIP), although the differential diagnosis can at times expand to encompass other extremely rare etiologies
- Amyloidosis
- Light Chain Deposition Disease
- Neurofibromatosis
-
- Less Common
- Sjögren syndrome
- light chain deposition disease
- Ehlers Danlos syndrome type IV
- fire-eater’s lung (pneumatoceles)
- lymphomatoid granulomatosis
- neurofibromatosis
- congenital pulmonary airway (cystic adenomatoid) malformation,
- smoking related small airways injury [
- Proteus syndrom
- Look Alikes
- Emphysema
- No wall
- Central soft tissue elements
- Blebs
- Bullae
- >1 cm in diameter, bounded by a
- thin wall (<1 mm)
- background emphysema
- Bronchiectasis
- continuity with airways
- Honeycombing
- enlarged airspaces
- .3 -1.0cms (up to 2.5cms)
- thick fibrous walls
- End stage fibrotic disease
- subpleural
- stacked
- enlarged airspaces
- Pneumatoceles
- thin-walled parenchymal cyst
- Infection
- bacterial pneumonia eg children
- PCP Pneumocystis jirovecii,
- coccidioidomycosis,
- hyperimmunoglobulinemia E syndrome,
- staphylococcal pneumonia
- Chest Trauma
- Emphysema
- Look Alikes
- LAM
-
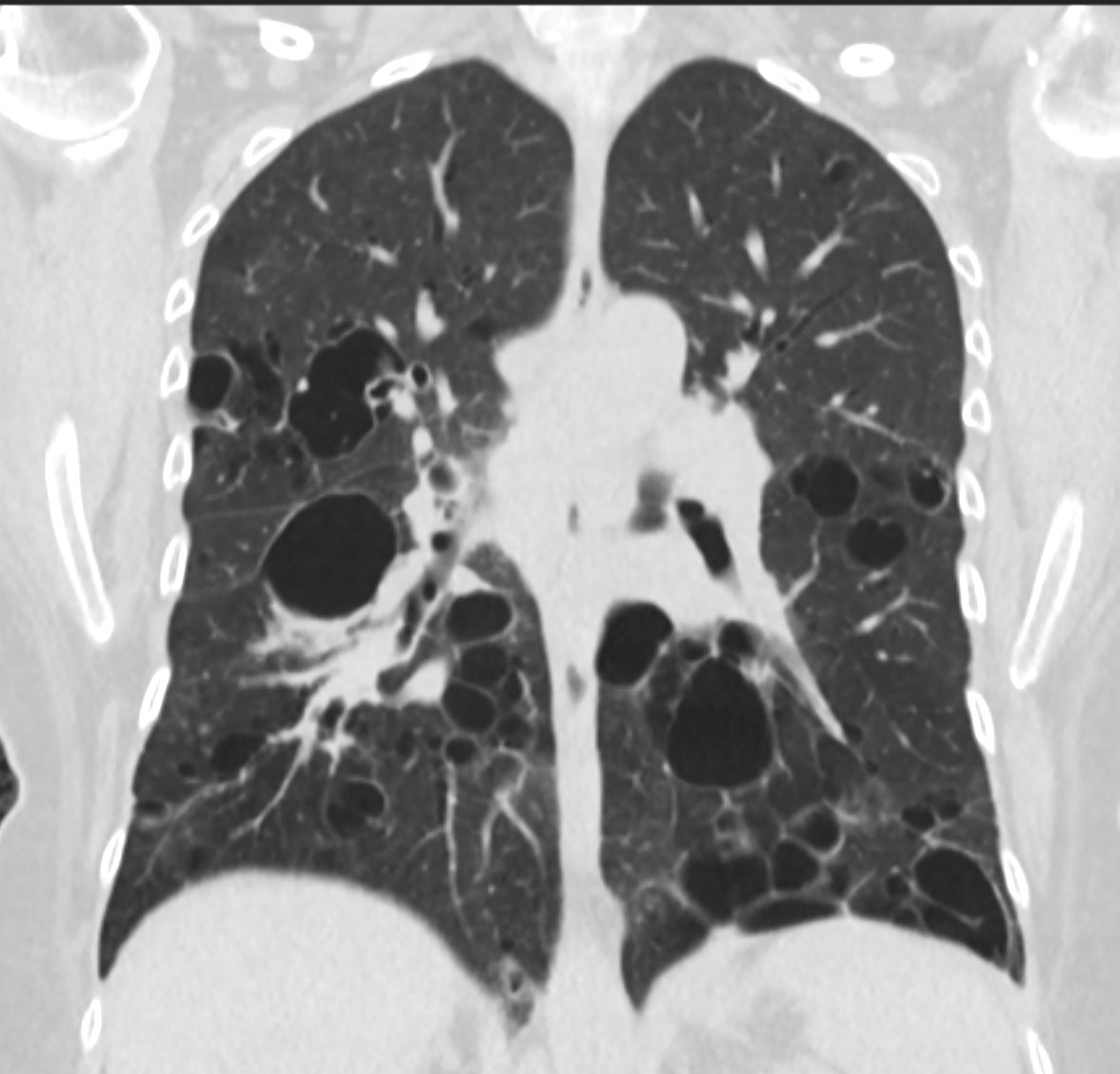
LAM and LYMPHANGIOLEIOMYOMAS in the ABDOMEN
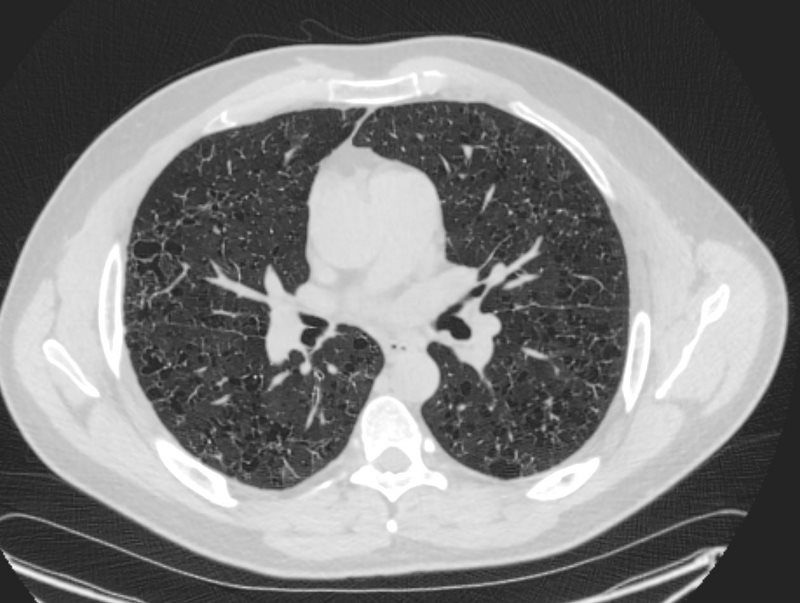
38-year-old patient with progressive dyspnea and cough
CXR (scout for CT) shows hyperinflated lungs with increased lung volumes with bilateral and extensive thin-walled cysts surrounded by very little normal lung parenchyma. The cysts are round and thin-walled except for air filled large irregular pocket in the right apex (image 27628/29) . Some of the cysts do not have walls at all and others have an irregular configuration.
In the abdomen multiple low density lymphangioleiomyomas are present that are due to lymphatic obstruction.
Ashley Davidoff MD TheCommonVein.net
-
Upper
- Infections
- PCP
-

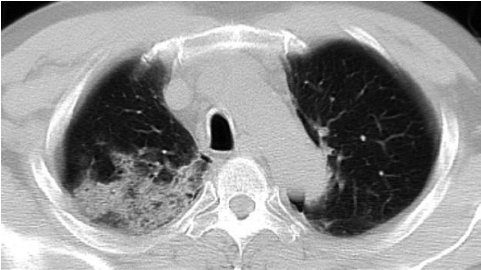
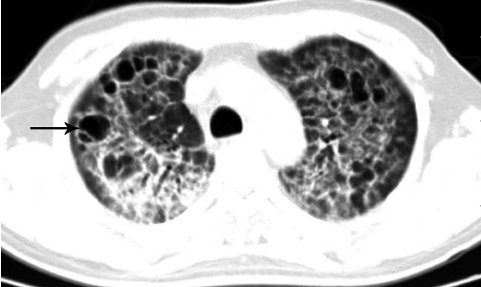
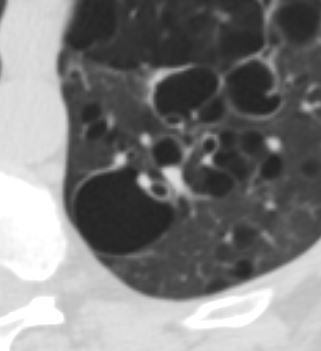
Chest CT of lung cysts dominated PCP in an AIDS patient. Numerous thin walled lung cysts in upper lobe of both lungs. The cysts have various shapes and sizes. In some cysts there are interior separations (arrow). Infiltration lesions are seen around some of the cysts
Lu, Pu-Xuan, et al Correlation between imaging features of Pneumocystis Jiroveci Pneumonitis (PCP), CD4+ T lymphocyte count, and plasma HIV viral load: A study in 50 consecutive AIDS patients Quantitative Imaging in Medicine and Surgery 2(2):124-9, June 2012
Chest CT of a condominated PCP in an AIDS patient. Patchy shadows are shown in the upper lobe of right lung
Lu, Pu-Xuan, et al Correlation between imaging features of Pneumocystis Jiroveci Pneumonitis (PCP), CD4+ T lymphocyte count, and plasma HIV viral load: A study in 50 consecutive AIDS patients Quantitative Imaging in Medicine and Surgery 2(2):124-9, June 2012Complication of PCP Lung Cysts
- PTX,
- incidence 35% in patients with cysts
- frequently bilateral
- often refractory to chest tube Rx,
- frequently need surgery eg pleurodesis
- associated higher mortality rate,
- especially in patients on ventilation.

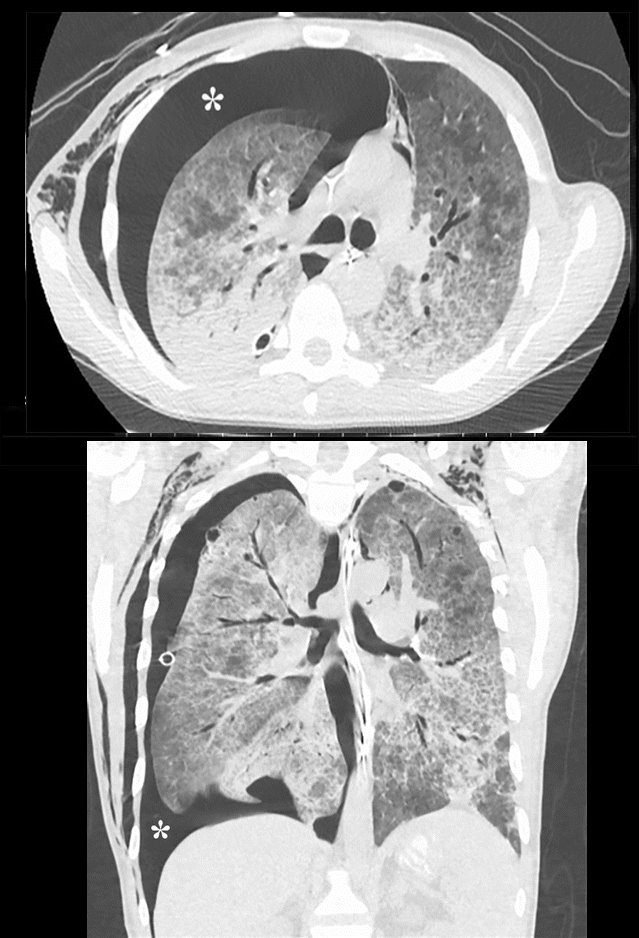
Pneumocystis carinii pneumonia. CT scans in a 32-year-old man with acquired immunodeficiency syndrome and a CD4 count of 7cells per microliter who presented with respiratory arrest. (a) Axial and (b) coronal images in lung windows demonstrate a moderate right pneumothorax (*) and widespread ground-glass and airspace opacities.
Parekh, M et al Review of the Chest CT Differential Diagnosis of Ground-Glass Opacities in the COVID Era Radiology Vol. 297, No. 3 July 2020 - PTX,
- ILD
- DIP
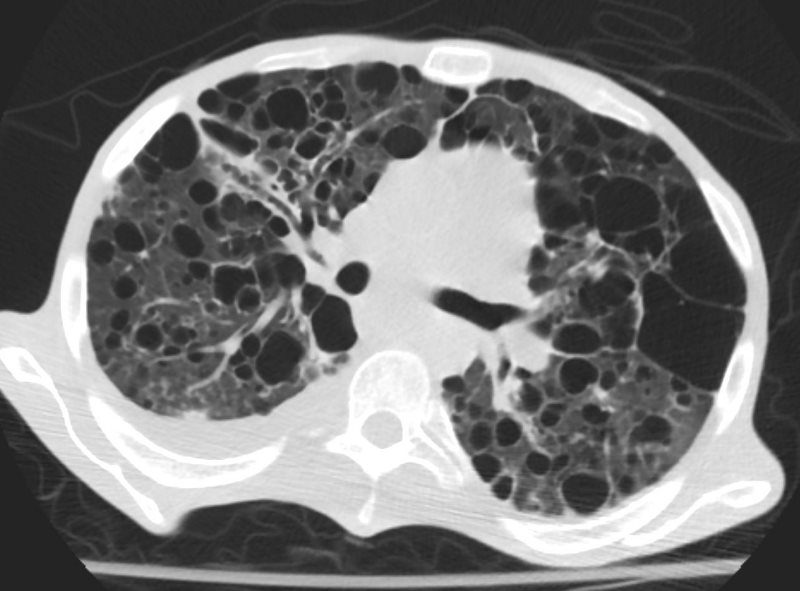
-

Desquamative interstitial pneumonitis. (a) Axial and (b) coronal lung window CT scans in a 64-year-old man with a history of smoking (17 pack-years) and shortness of breath. Images show small cysts in both lower lobes (arrow) with surrounding interstitial prominence.
Parekh, M et al Review of the Chest CT Differential Diagnosis of Ground-Glass Opacities in the COVID Era Radiology Vol. 297, No. 3 July 2020LIP
- Lower Lobe predominance
-

Stable Cystic Changes
47 F SLE Sjogrens LIP vs Birt-Hogg-Dube basilar thin walled cysts lymphadenopathy
Subsegmental right lower lobe infiltrate
Ashley Davidoff TheCommonVein.net
47 F SLE Sjogrens LIP vs Birt-Hogg-Dube basilar thin walled cysts lymphadenopathy
Subsegmental right lower lobe infiltrate
Ashley Davidoff TheCommonVein.net
47 F SLE Sjogrens LIP vs Birt-Hogg-Dube basilar thin walled cysts lymphadenopathy
Ashley Davidoff TheCommonVein.net
Cysts Associated with Blood Vessels in LLL
47 F SLE Sjogrens LIP vs Birt-Hogg-Dube basilar thin walled cysts lymphadenopathy
Subsegmental right lower lobe infiltrate
Ashley Davidoff TheCommonVein.net- LIP Lymphoid Interstitial Pneumonia

-

CT scan of lymphocytic interstitial pneumonia, with pulmonary cysts.
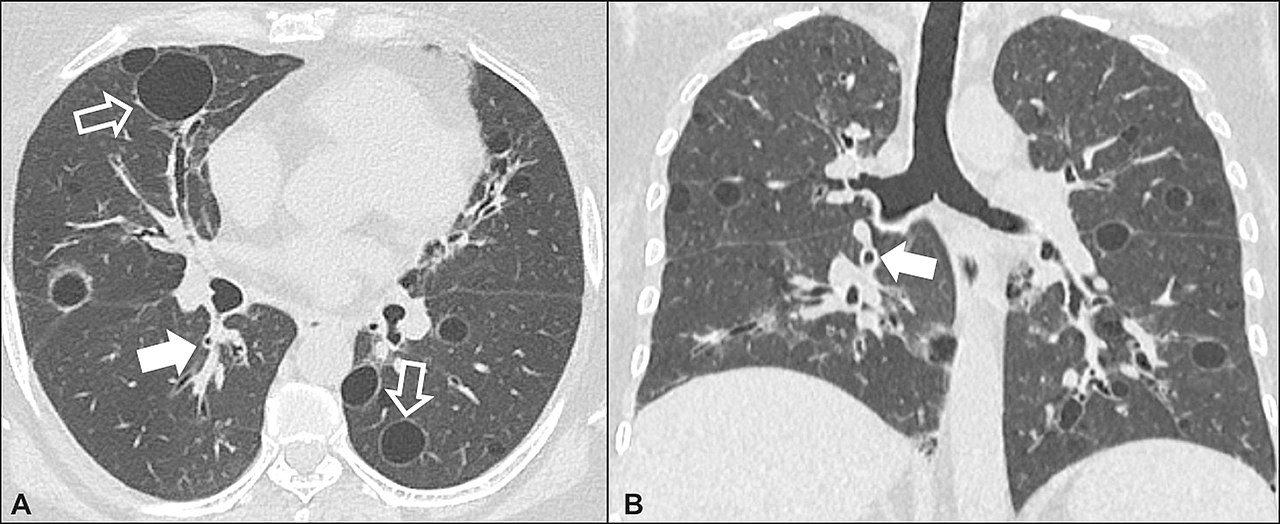
Lymphocytic interstitial pneumonia. A 62-year-old female patient with Sjögren’s syndrome. Axial high-resolution computed tomography scan of the chest (A) and coronal reformatting (B). In A, diffuse thickening of the bronchial walls (closed arrows), some ground-glass opacities and thin-walled cysts of varying sizes, with a diffuse, bilateral distribution (open arrows). In B, distribution predominantly in the lower fields.
Daniel Simões Oliveira et al
Radiologia Brasileira 51 (5): 321–327. - 017Lu 27F LIP HIV AIDS Lymphoma
028Lu LIP Emphysema
-

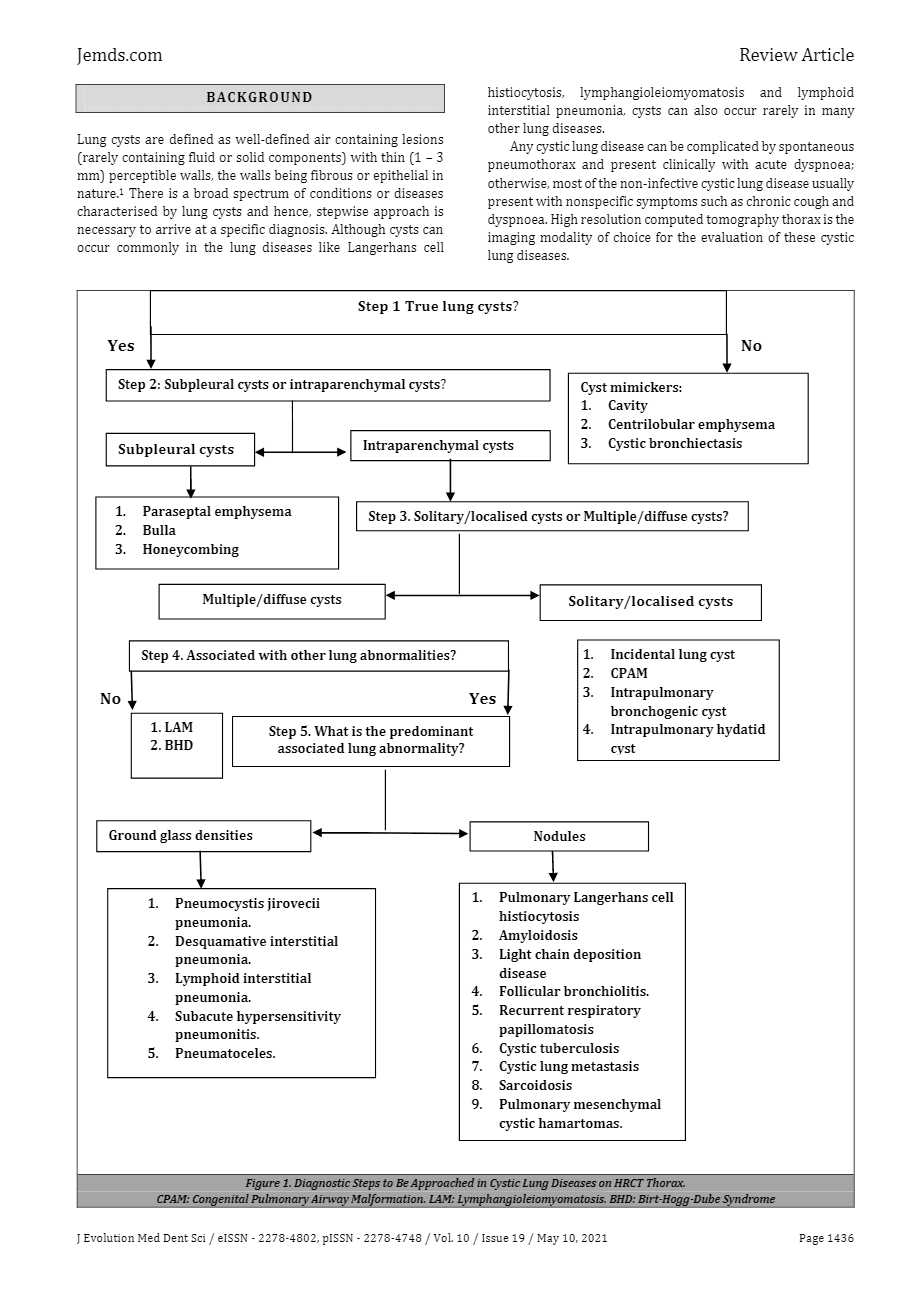
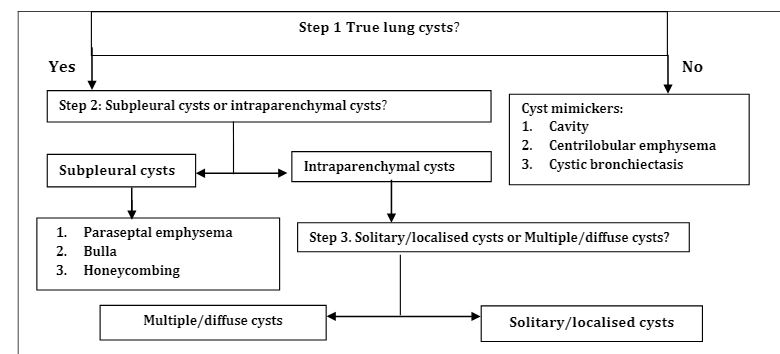
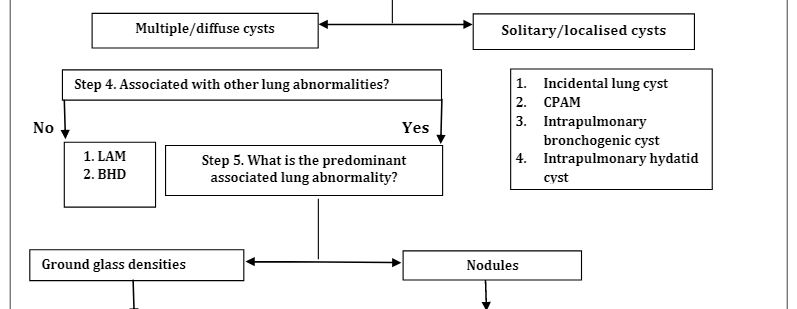
J Evolution Med Dent Sci / eISSN – 2278-4802, pISSN – 2278-4748 / Vol. 10 / Issue 19 / May 10, 2021 
J Evolution Med Dent Sci / eISSN – 2278-4802, pISSN – 2278-4748 / Vol. 10 / Issue 19 / May 10, 2021 
J Evolution Med Dent Sci / eISSN – 2278-4802, pISSN – 2278-4748 / Vol. 10 / Issue 19 / May 10, 2021 - LIP Lymphoid Interstitial Pneumonia
- A Stepwise Diagnostic Approach to Cystic Lung Diseases for Radiologists.
Lee KC, Kang EY, Yong HS, et al. Korean Journal of Radiology. 2019;20(9):1368-1380. doi:10.3348/kjr.2019.0057.
-
Cystic and Cavitary Lung Diseases: Focal and Diffuse.
Ryu JH, Swensen SJ. Mayo Clinic Proceedings. 2003;78(6):744-52.
-
Cystic Lung Diseases: Algorithmic Approach.
Raoof S, Bondalapati P, Vydyula R, et al. Chest. 2016;150(4):945-965. doi:10.1016/j.chest.2016.04.026.
-
Isolated Cystic Lung Disease: An Algorithmic Approach to Distinguishing Birt-Hogg-Dubé Syndrome, Lymphangioleiomyomatosis, and Lymphocytic Interstitial Pneumonia. Escalon JG, Richards JC, Koelsch T, Downey GP, Lynch DA. AJR. American Journal of Roentgenology. 2019;212(6):1260-1264.
-
CT Findings of Pulmonary Cysts.
Arango-Díaz A, Martínez-de-Alegría-Alonso A, Baleato-González S, et al. Clinical Radiology. 2021;76(7):548.e1-548.e12.
-
Cystic Lung Diseases: Radiological Aspects.
Valente T, Guarino S, Lassandro G, et al. Clinical Radiology. 2022;77(5):e337-e345.
-
Park HJ, Chae EJ, Do KH, Lee SM, Song JW.
AJR. American Journal of Roentgenology. 2019;212(4):766-772.
-
Ferreira Francisco FA, Soares Souza A, Zanetti G, Marchiori E. European Respiratory Review : An Official Journal of the European Respiratory Society. 2015;24(138):552-64.
-
Johnson SR, Shaw DE, Avoseh M, et al. Thorax. 2024;79(4):366-377. doi:10.1136/thorax-2022-219738.
-
High-Resolution Computed Tomography of Cystic Lung Disease.
Kusmirek JE, Meyer CA.
Seminars in Respiratory and Critical Care Medicine. 2022;43(6):792-808. .
-
Lymphangioleiomyomatosis and Other Cystic Lung Diseases.
Koslow M, Lynch DA, Cool CD, Groshong SD, Downey GP. Immunology and Allergy Clinics of North America. 2023;43(2):359-377.
-
Elia D, Torre O, Cassandro R, Caminati A, Harari S. European Respiratory Review : An Official Journal of the European Respiratory Society. 2020;29(157):190163.


 CT scan shows multiple small cysts sometimes irregular in shape predominantly in the upper lobes. The cysts are round and air filled large and are between 5mm-8mm
CT scan shows multiple small cysts sometimes irregular in shape predominantly in the upper lobes. The cysts are round and air filled large and are between 5mm-8mm