- Etymology: Derived from the Latin “paraseptal,” meaning “adjacent to the septum.” Refers to emphysema affecting the distal acinus near interlobular septa and pleura.
- AKA: Distal Acinar Emphysema, Subpleural Emphysema.
- What is it? Paraseptal emphysema is a subtype of emphysema involving the distal acinus, predominantly affecting the subpleural and paraseptal regions, characterized by localized airspace enlargement and potential bulla formation.
- Caused by:
- Smoking (most common): Chronic inflammation damages the distal acinus.
- Inflammation/Immune: Chronic obstructive pulmonary disease (COPD).
- Mechanical trauma: Repeated alveolar stress and overdistension.
- Congenital: Associated with Marfan syndrome or Ehlers-Danlos syndrome.
- Other: Idiopathic in some cases, especially in young adults.
- Why it occurs in the periphery:
- Mechanical forces at the pleural interface create high strain during ventilation cycles.
- Peripheral secondary lobules are less structurally supported, making them vulnerable to damage.
- Pressure gradients and stress concentration at interlobular septa and pleura predispose these areas to emphysematous changes.
- Resulting in:
- Localized alveolar destruction near the pleura.
- Formation of subpleural bullae.
- Compression of adjacent parenchyma.
- Risk of rupture leading to spontaneous pneumothorax.
- Structural Changes:
- Dilated distal acini in the subpleural and paraseptal regions.
- Coalescence of airspaces forming bullae.
- Thinning or destruction of interlobular septa.
- Pathophysiology:
- Chronic inflammation and protease activity lead to the breakdown of alveolar walls.
- Initially, interlobular septa act as barriers, localizing airspace enlargement into small subpleural bullae.
- Over time, septal walls break down, allowing bullae to enlarge further.
- This process reduces lung elasticity, causes ventilation-perfusion mismatch, and may compromise adjacent lung tissue.
- Pathology:
- Gross: Bullae or air-filled spaces near pleura, often upper-lobe predominant.
- Microscopic: Dilated distal acini with loss of alveolar walls; no epithelial lining in bullae.
- Diagnosis:
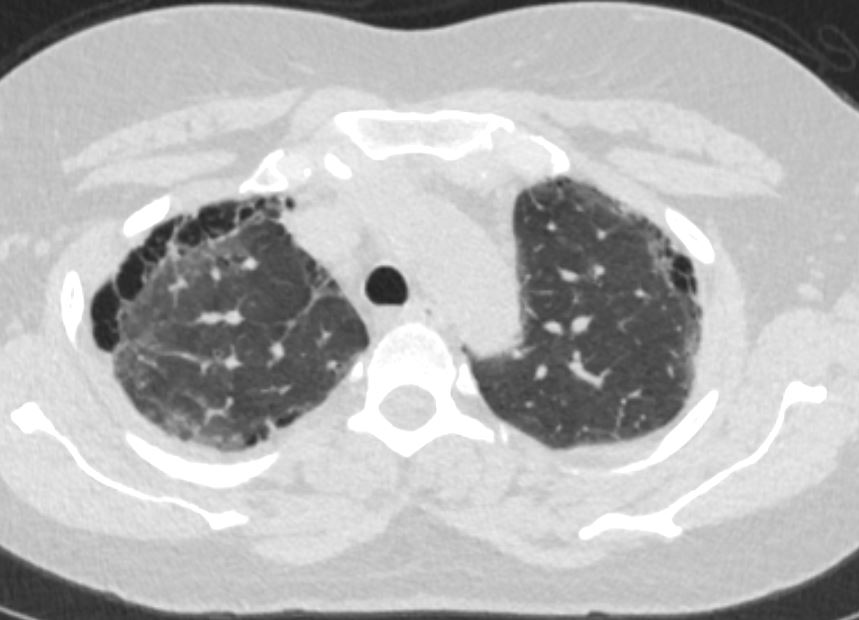
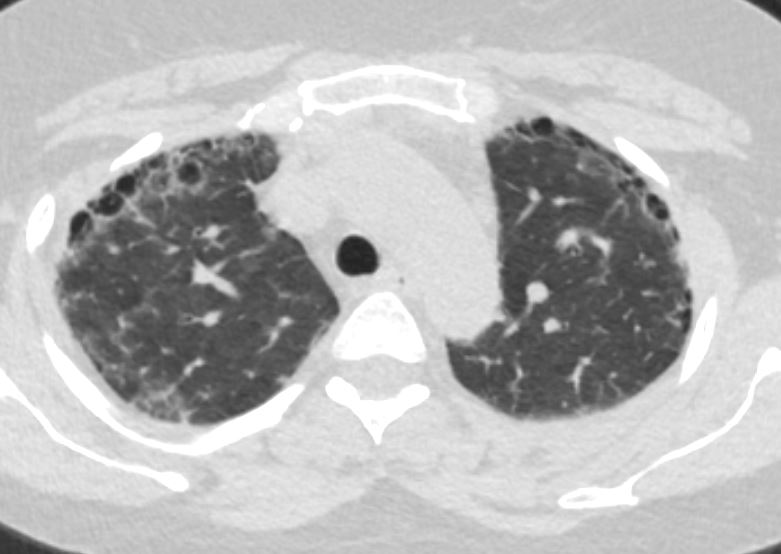
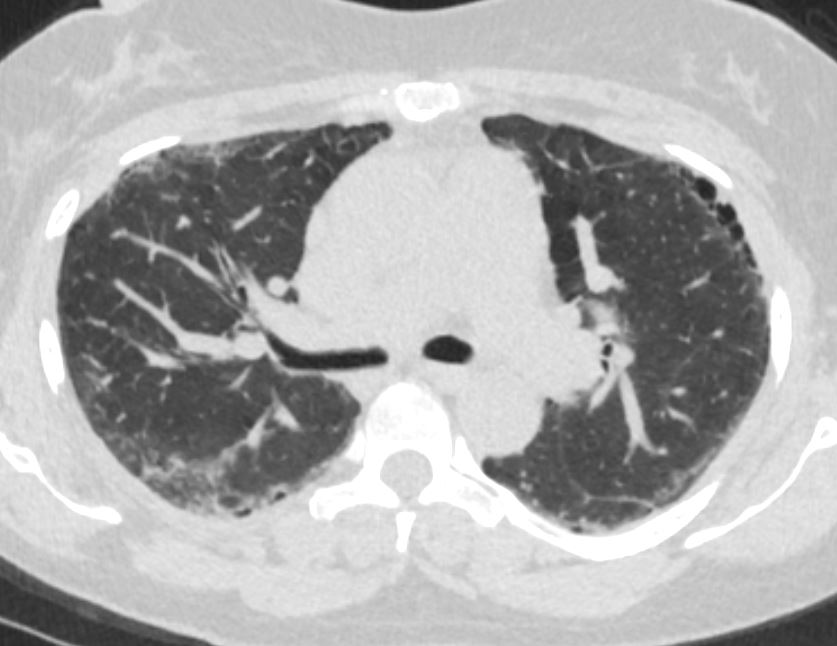
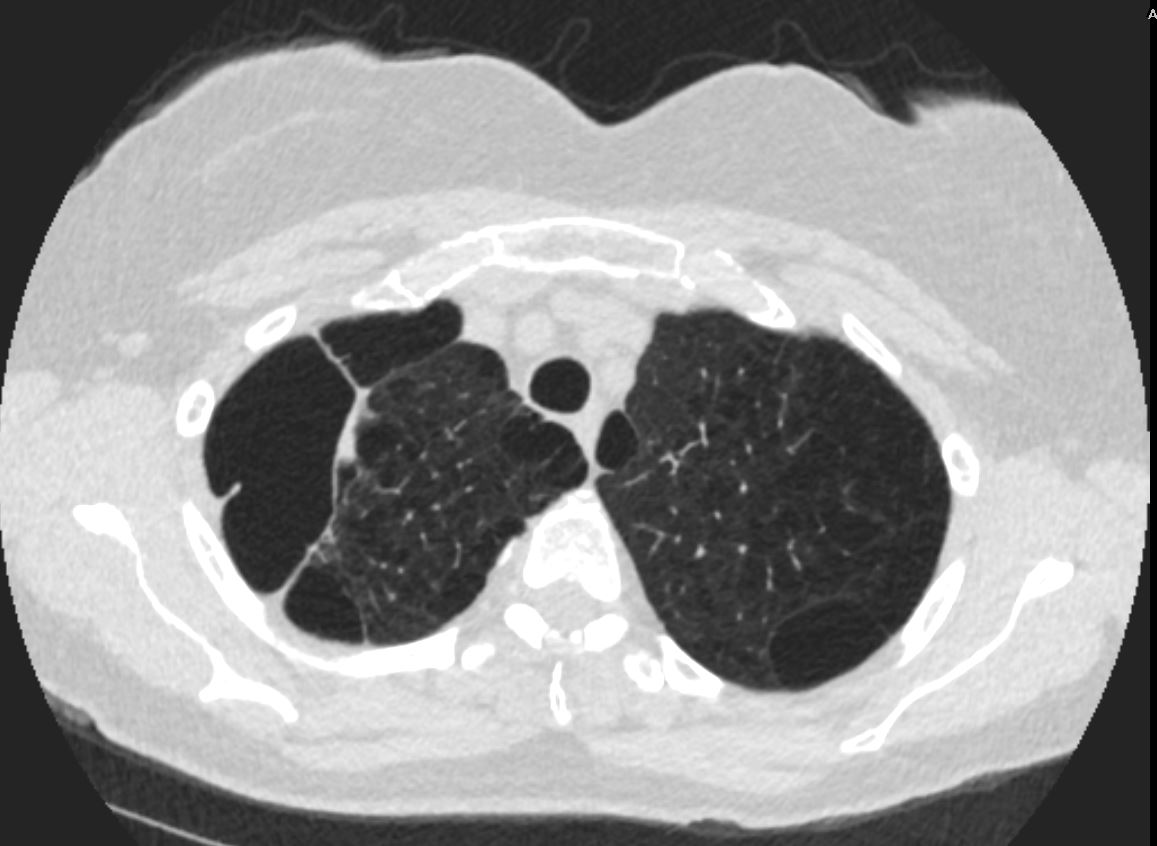
- CXR: Subpleural lucencies or bullae, typically near the upper lobes.
- CT: Definitive for detecting small bullae and distinguishing from other conditions.
- Clinical:
- Symptoms: Often asymptomatic unless complicated by pneumothorax. Mild dyspnea may occur in advanced cases.
- Signs: Spontaneous pneumothorax, especially in young, thin males.
- Radiology:
- CXR: Thin-walled subpleural lucencies; associated findings include pneumothorax.
- CT: Bullae appear as well-defined, hypoattenuated airspaces >1 cm, predominantly subpleural. Changes are often upper-lobe predominant.
- MRI/PET-CT/US: Rarely used; ultrasound may detect pneumothorax but not emphysema.
- Pulmonary Function Tests (PFTs):
- May be normal in isolated paraseptal emphysema.
- Severe cases show an obstructive pattern with increased total lung capacity and residual volume.
- Management:
- Lifestyle modifications: Smoking cessation to slow progression.
- Monitoring: Follow-up imaging to assess bulla size and pneumothorax risk.
- Complication management: Chest tube placement for pneumothorax; bullectomy for recurrent pneumothoraces or large symptomatic bullae.
- Pulmonary rehabilitation: Exercise and breathing strategies.
- Recommendations:
- Avoid smoking to prevent progression.
- Monitor individuals with paraseptal emphysema, particularly young adults and smokers, for pneumothorax.
- Early intervention for recurrent pneumothorax is critical.
- Key Points and Pearls:
- Paraseptal emphysema predominantly affects the upper lobes and is associated with pneumothorax.
- Subpleural bullae are characteristic findings on imaging.
- Pathophysiology involves localized destruction of alveoli with potential enlargement into bullae.
- Proper diagnosis and management can prevent complications such as pneumothorax and impaired lung function.
Ashley Davidoff TheCommonVein.net
Ashley Davidoff TheCommonVein.net
Ashley Davidoff TheCommonVein.net
Ashley Davidoff MD
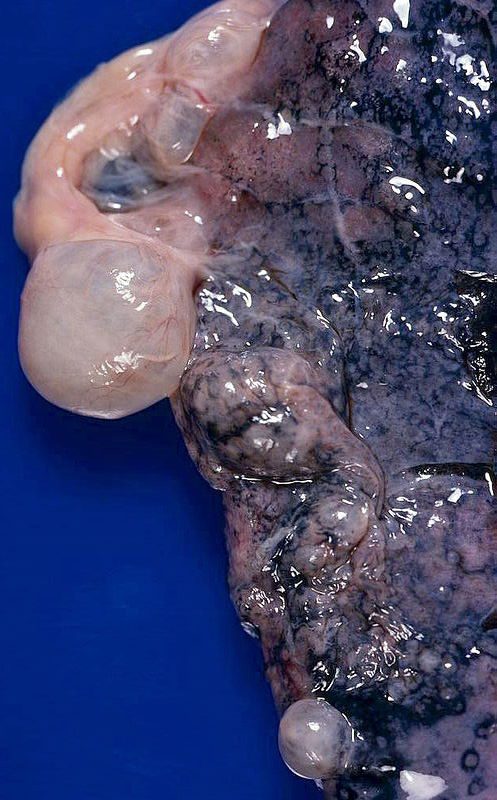
Large, prominent subpleural bullae. Spontaneous pneumothorax often results from rupture of such lesions.
Bullous (paraseptal) emphysema limited to lung periphery. Usually not smoking-related. Rupture is most common cause of spontaneous penumothorax…mostly young adults.
Courtesy Yale Rosen MD
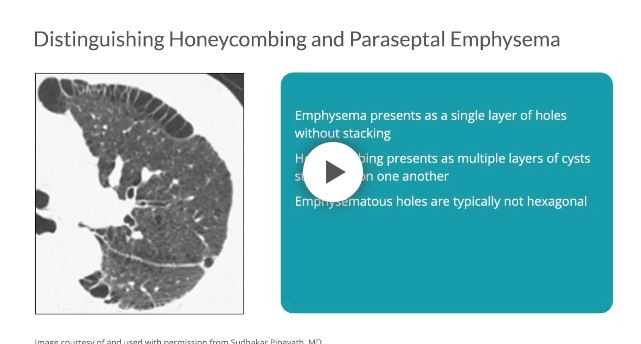
Distinguishing between honeycombing and paraseptal emphysema may be difficult, especially when coexisting on a single scan. As compared with honeycombing, which may present as multiple layers of cysts stacked upon one another, emphysema presents as a single layer of holes without stacking.7 Furthermore, emphysematous holes are typically not hexagonal; therefore, the shape of the cysts and their propensity to stack can help to distinguish one from the other.7
as relatively reduced CT attenuation at subpleural or peribronchovascular areas with or without intact interlobular septa
Paraseptal emphysema is a
- chronic lung condition
- characterized by the destruction and enlargement of the alveoli
- involves the peripheral areas of the lungs,
- Alveolar Destruction:
- the walls of the alveoli in the peripheral areas of the lungs
- become damaged and
- lose their elasticity.
- Air Trapping:
- As the alveoli lose their elasticity, t
- become less efficient at expelling air during exhalation.
- leads to air becoming trapped in these distal alveolar spaces, resulting in localized overinflation.
- Tension of the pleura
- pulling on the periphery of the lung during inspiration
- contributes to greater mechanical stress on the peripheral alveoli.
- Stress Distribution:
- The tension on the pleura is
- transmitted to the adjacent alveoli.
- Stretching and Shearing
- The mechanical forces
- can cause stretching and shearing forces on the alveoli.
- result in damage to the alveolar walls and
- more so if smoking or disease
- have caused decreased elasticity
- Stress Distribution:
-
- Bullae Formation:
- Prolonged air trapping and
- overinflation can cause the
- formation of large, bullae.
- can exert pressure on surrounding lung tissue and interfere with normal lung function.
- Associated Conditions:
- often associated with other forms of emphysema,
- Smoking is a significant risk factor
- as well as other lung conditions.
- Why does paraseptal emphysema affect the periphery of the lungs?
- due to differences in ventilation and anatomical structure within the lung tissue.
- Ventilation Distribution:
- The lungs are not uniformly ventilated throughout their structure.
- Peripheral lung regions, which are further away from the main airways,
- receive less ventilation compared to the central regions.
- Alveolar Structure: The alveoli, in the peripheral or subpleural areas
- have thinner walls
- Pressure Differences:
- alveoli near the periphery have
- relatively higher pressures during exhalation
- due to the increased resistance
- lead to stress and strain on the alveolar walls
- alveoli near the periphery have
- Air Trapping:
- When air becomes trapped in the alveoli due to reduced elasticity of the alveolar walls,
- tends to accumulate more in the peripheral regions
