Infection Inflammation Malignancy Mechanical/Atelectasis Trauma Metabolic Circulatory- Hemorrhage Immune Infiltrative Idiopathic Iatrogenic Idiopathic
Smooth
Hemorrhage
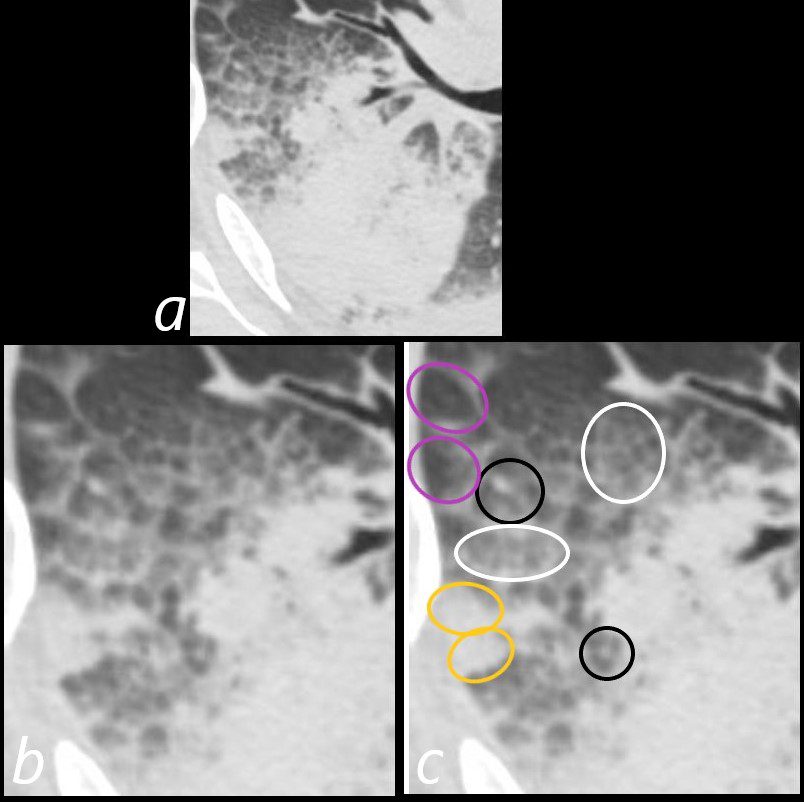
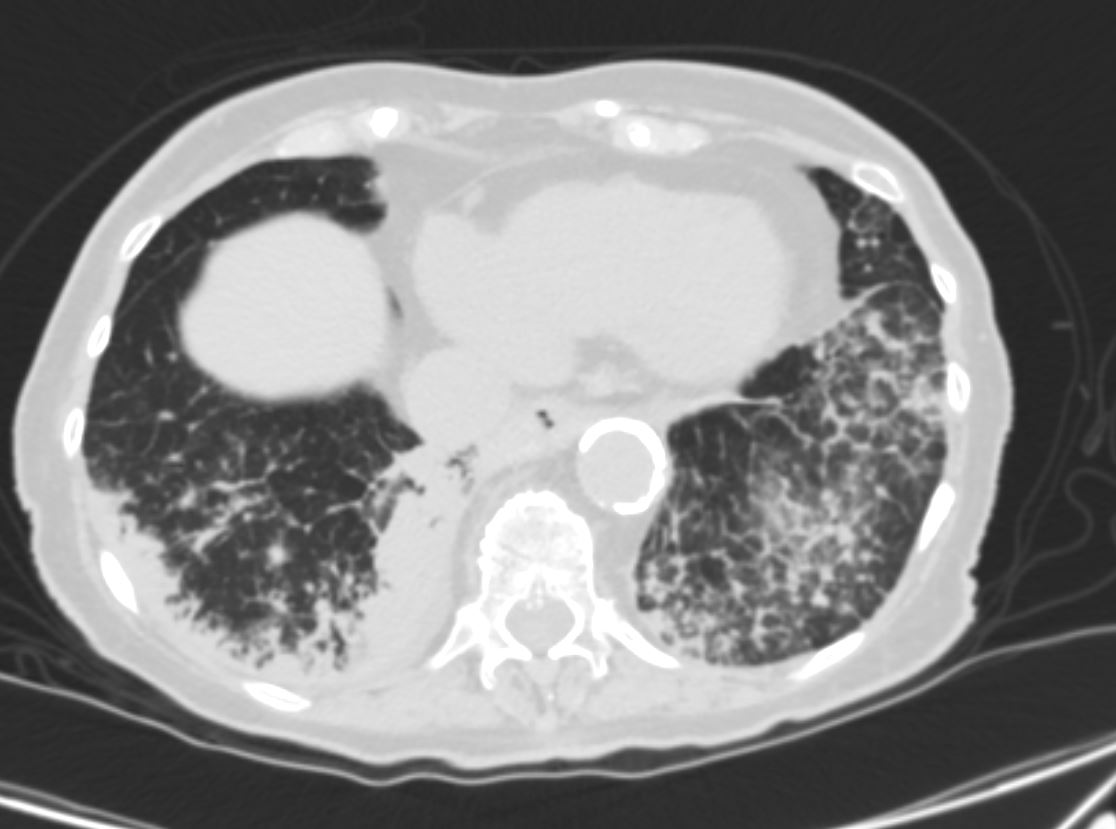
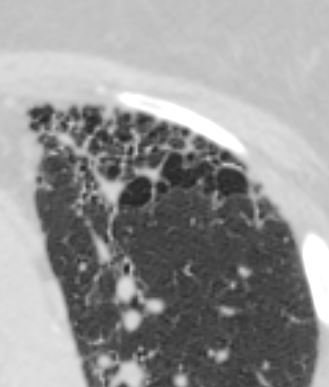
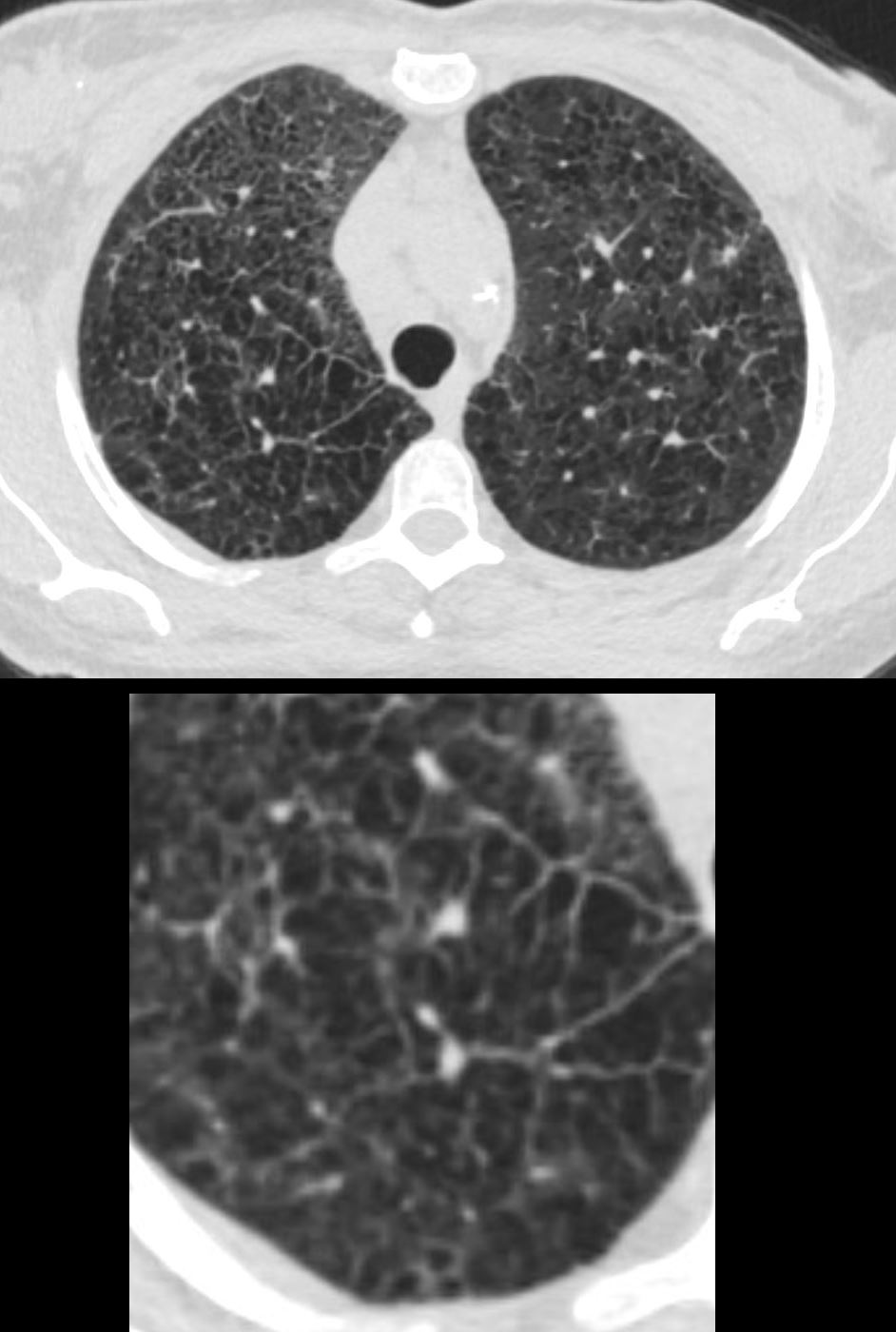
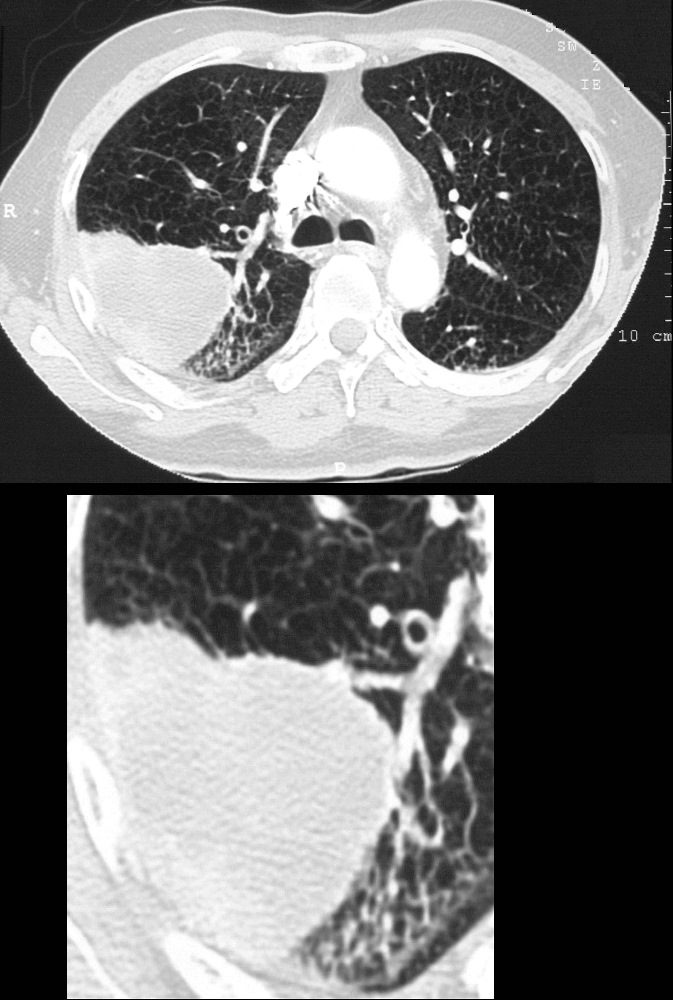
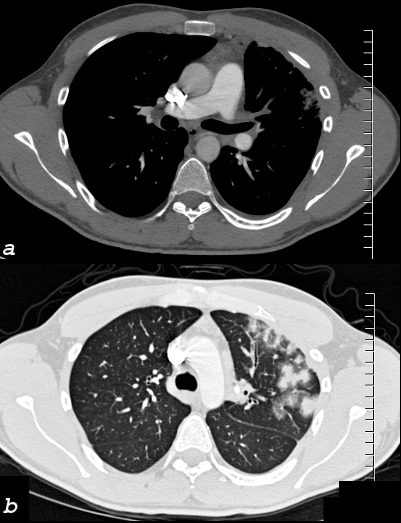
75-year-old man on blood thinners s/p aortic valve replacement, s/p trauma, presents with hemoptysis. He was afebrile and without an elevated white count
Axial CT at the level below the carina shows heterogenous changes of the secondary lobules. The changes in the posterior segment of the right upper lobe (a magnified below in b and c ) and show secondary lobules with ground glass changes (white rings) It is difficult to distinguish those with normal lung parenchyma and those with mosaic attenuation. It is hypothesized that those with prominent centrilobular nodules (black rings c) more than likely represent mosaic attenuation due to small airway disease. The lower density secondary lobules which do not have a prominent centrilobular nodule (c, purple rings), may either reflect normal parenchyma or mosaic attenuation. The orange rings likely reflect consolidation in side-by-side secondary lobules.
Ashley Davidoff MD TheCommonVein.net 165Lu 135854cL01
CHF
CT scan shows Diffuse ground glass pattern with thickening of the interlobular septa and manifesting as crazy paving pattern
Ashley Davidoff MD TheCommonVein.net 131742
Aspiration

Ashley Davidoff MD TheCommonVein.net crazy paving ICU 002
HIV ? Infection
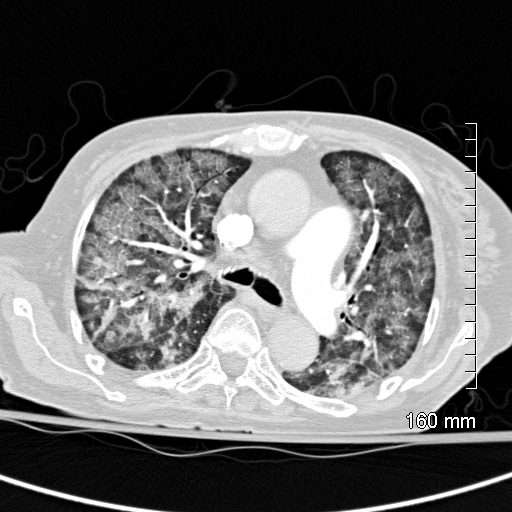
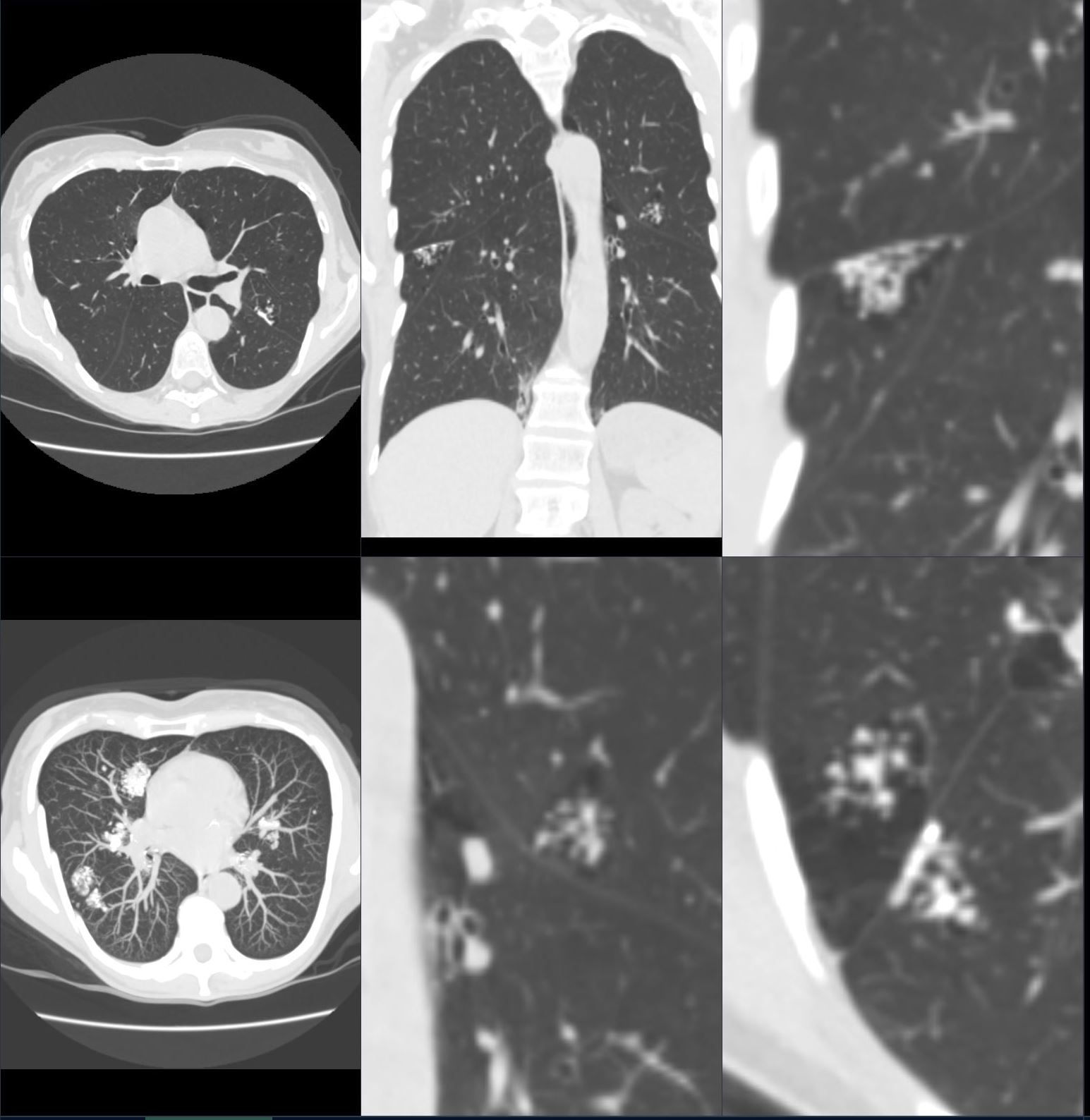
36 year old female with HIV presents with dyspnea. CT scan on presentation (upper images) show extensive disease with crazy paving pattern. Following adjunctive steroid therapy, the patient showed early mild improvement with persistence of crazy paving, peripheral sparing and regions of improved aeration (middle panel). Continued improvement continued subsequently with improved aeration, minimal residual crazy paving and bronchovascular infiltrate ( lower panel).
Ashley Davidoff MD TheCommonVein.net 30755c
Acute Eosinophilic Pneumonia vs COP
60 year old male presents with right sided pleuritic chest pain 15 months ago
CT shows multiple wedge shaped consolidations with some surrounding ground glass (RUL, LUL, LLL), focal nodules and regional segmental regions of ground glass consistent with multifocal pneumonia
Ashley Davidoff MD TheCommonVein.net
NSIP
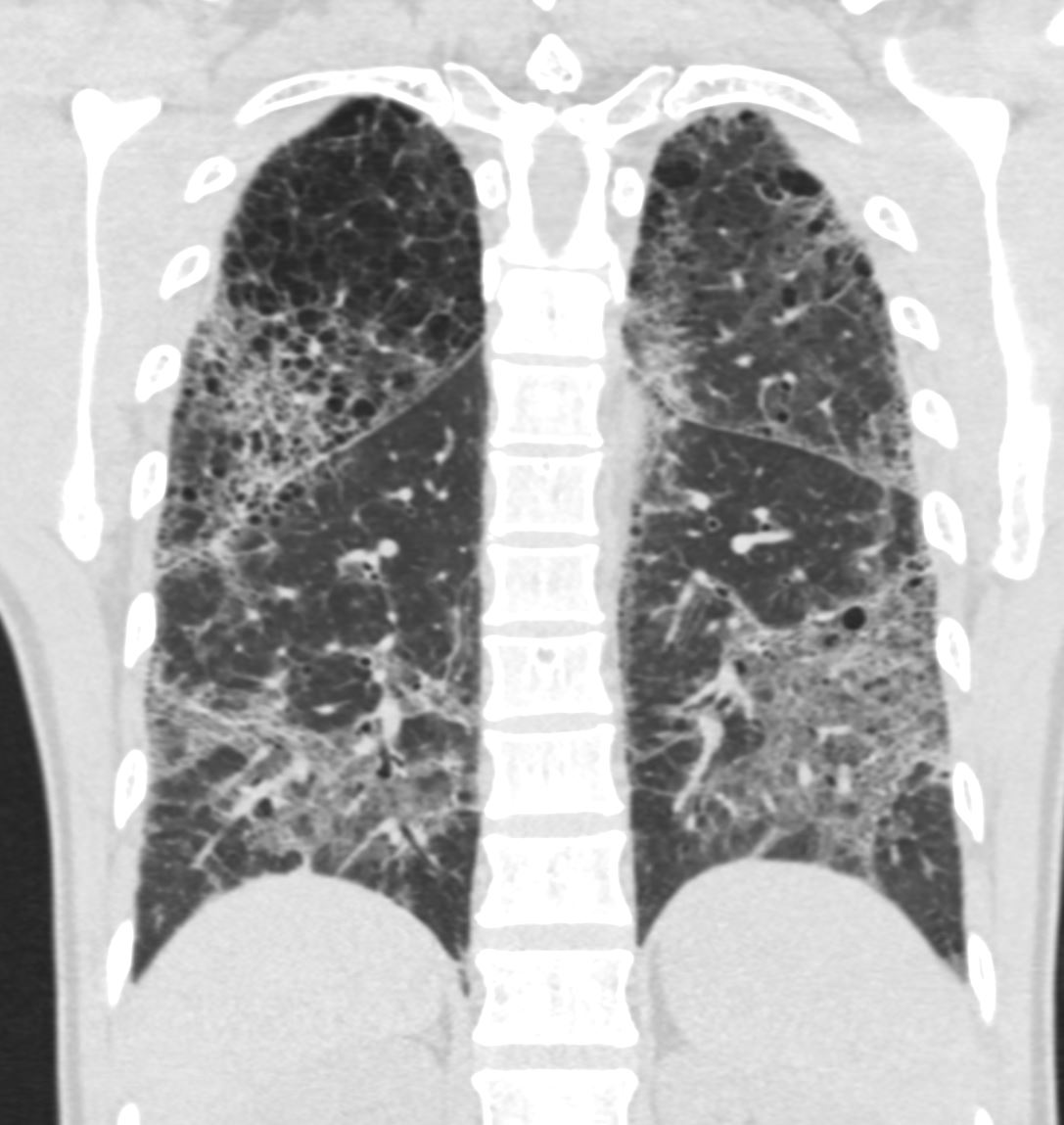
71-year-old female presents with a history of scleroderma, ILD, hypothyroidism and dcSSc
CT of the lower lobes in the coronal plane, shows extensive ground glass changes with irregular thickening of the interlobular septa.
Ashley Davidoff MD TheCommonVein.net 196Lu 136616
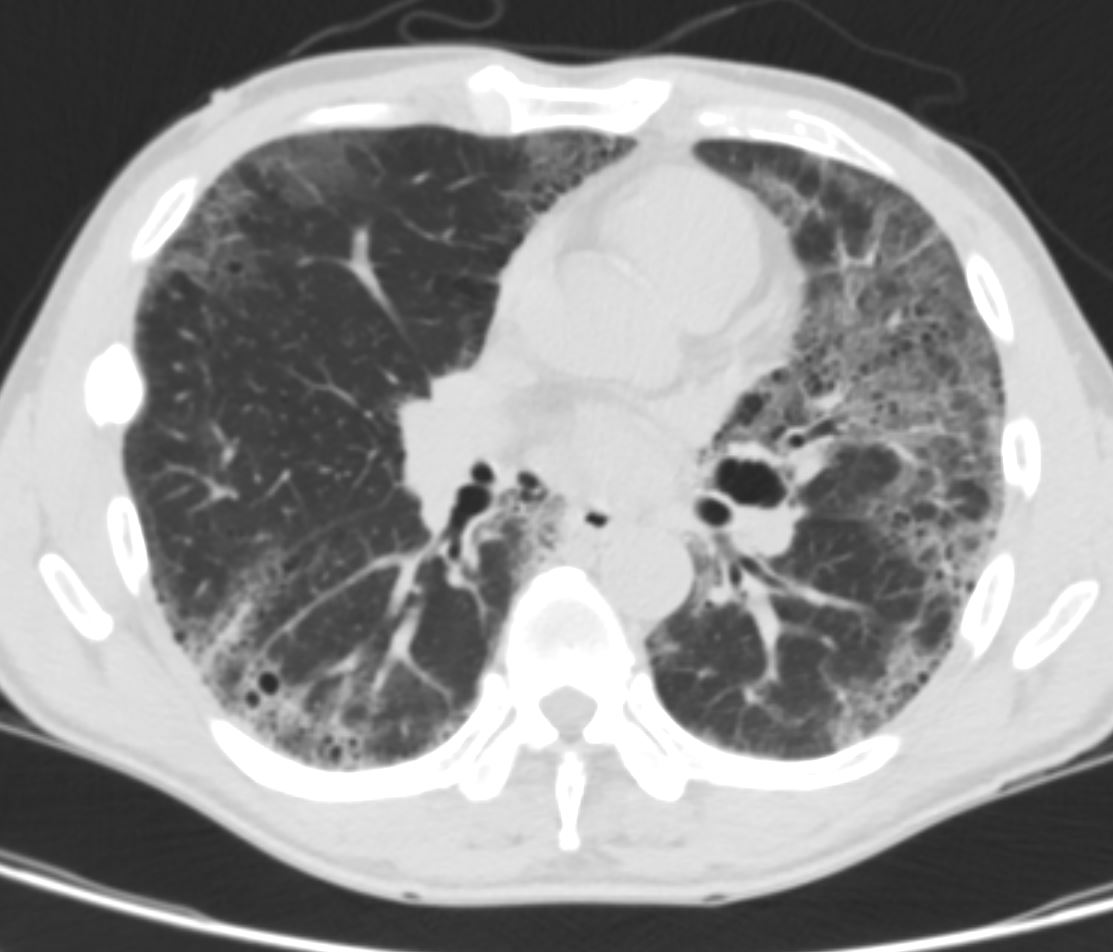
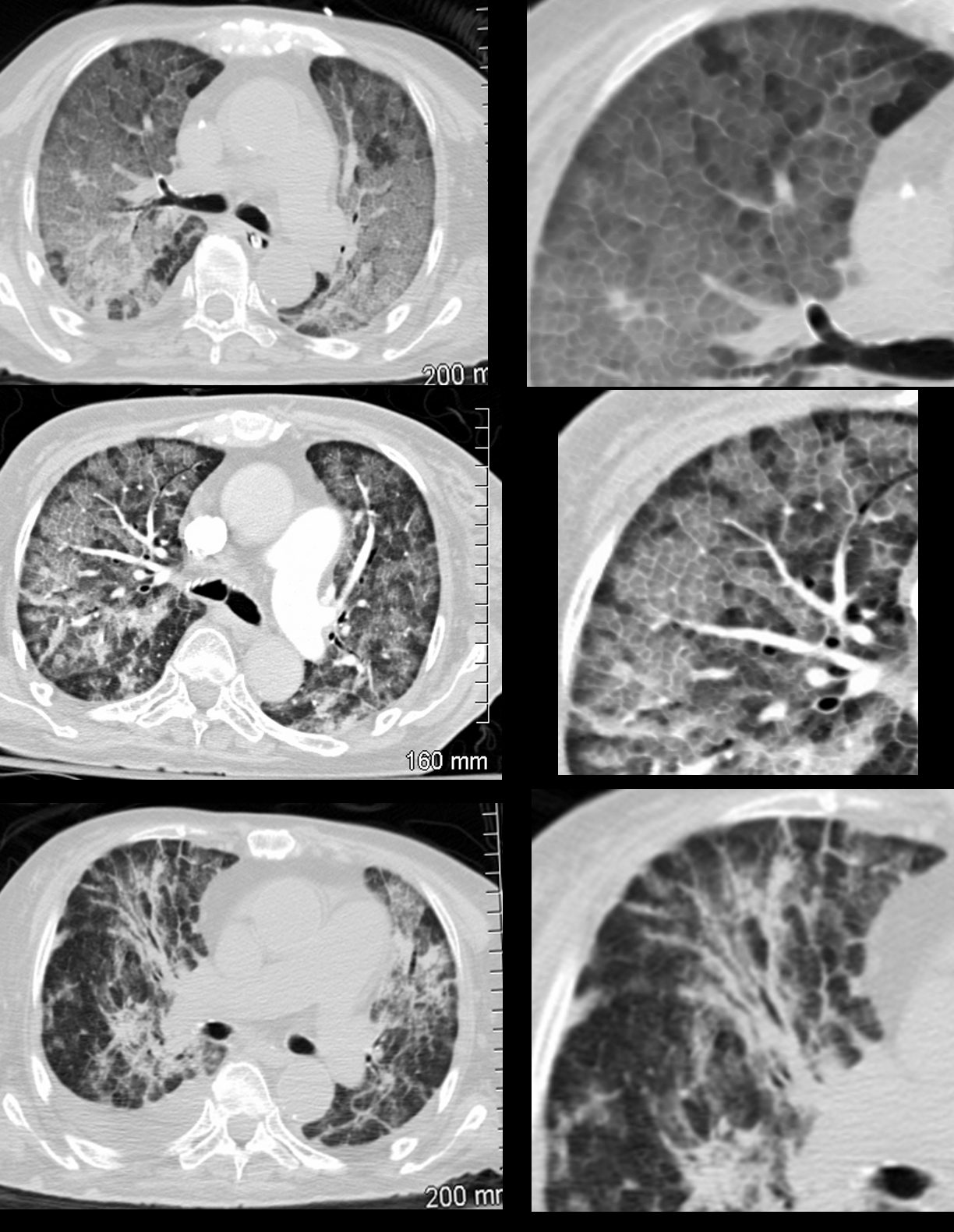
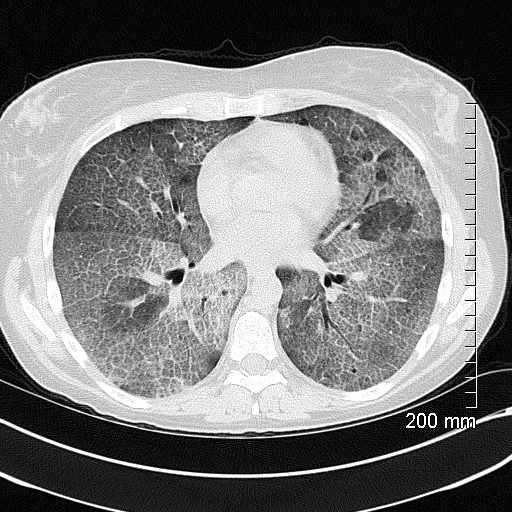
59-year-old male presents with history of scleroderma, Raynaud’s disease, and ILD
Axial CT shows extensive fibrotic change in the apical segments of the lower lobes and the anterior segments of the upper lobe.
There is volume loss architectural distortion, bronchiolectasis and subpleural sparing exemplified in the right lower lobe. peripheral reticular changes, ground glass, bronchiolectasis volume loss and subpleural sparing .
There are bands of fibrosis in the periphery of the right upper lobe with suggestion of intralobular fibrosis.
The spared secondary lobules in the right upper and right lower lobes have also undergone enlargement secondary to the fibrotic process
Ashley Davidoff MD TheCommonVein.net 110Lu 136596
Axial CT shows peripheral reticular changes, ground glass, bronchiolectasis at both lung bases, volume loss with crowding of the bronchovascular bundles posteriorly and subpleural sparing posteriorly. Note air-fluid level in the distended esophagus.
Ashley Davidoff MD TheCommonVein.net 110Lu 136598
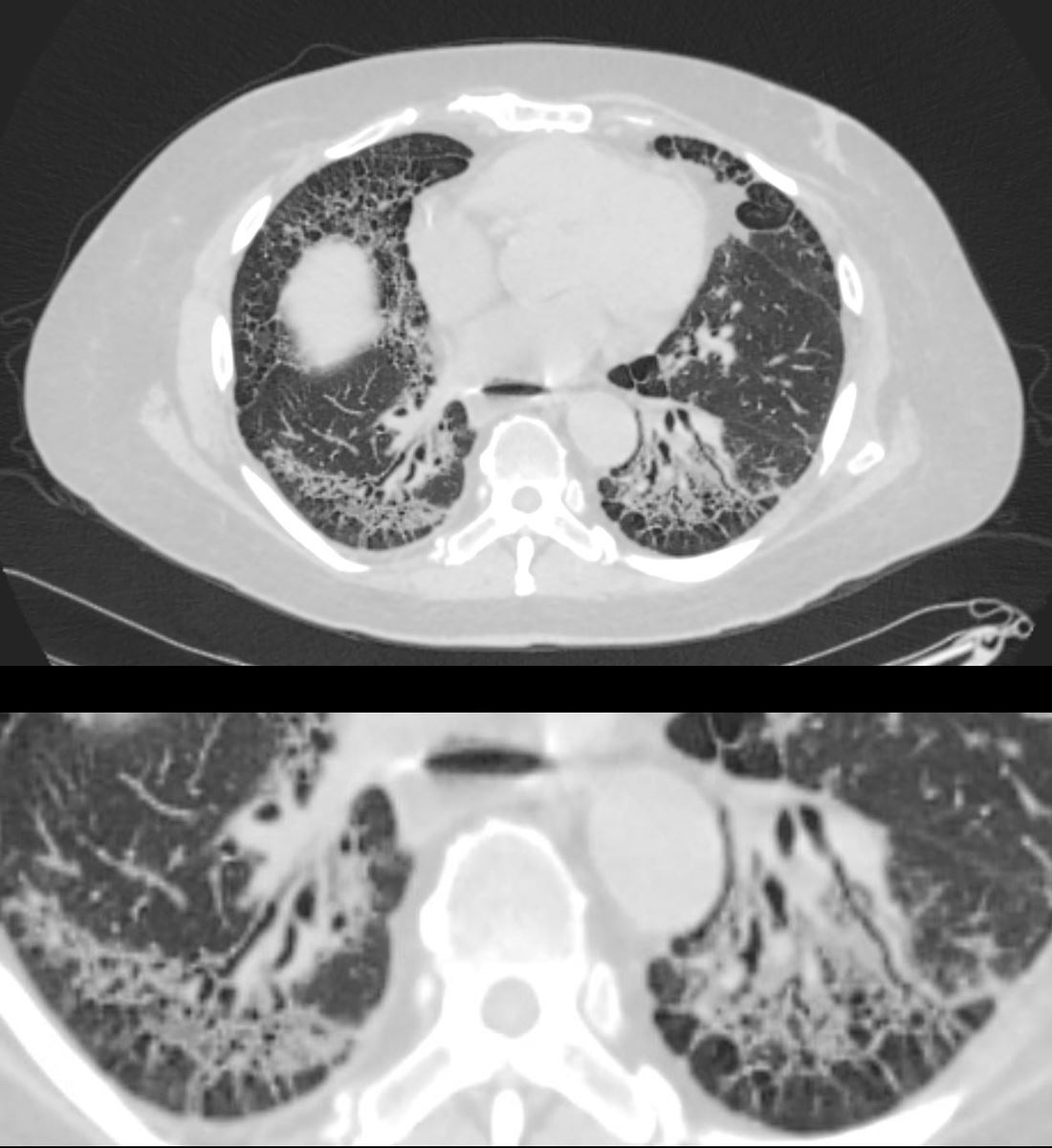
59-year-old male presents with history of scleroderma, Raynaud’s disease, and ILD
Upper Image
Axial CT shows bibasilar ground glass, bronchiectasis, and bronchiolectasis with volume loss and with crowding of the bronchovascular bundles posteriorly. There is subpleural sparing. Note air-fluid level in the distended esophagus.
The lower image focuses on the peripheral sparing. The spared secondary lobules have also undergone enlargement secondary to the fibrotic process
Ashley Davidoff MD TheCommonVein.net 110Lu 136598c01
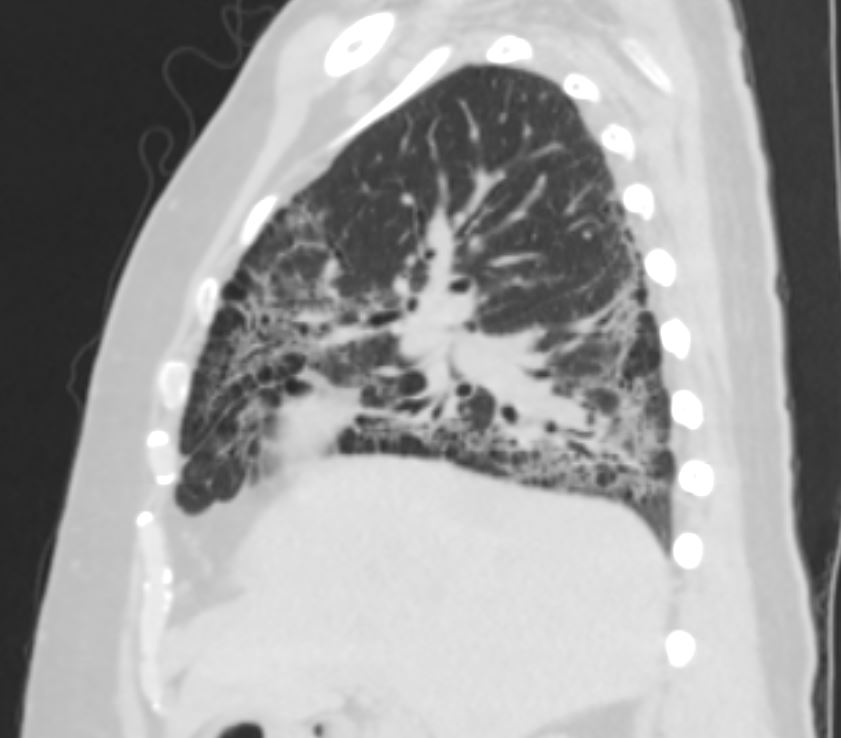
Sagittal CT shows, ground glass changes, bronchiolectasis at the lung base, volume loss with crowding of the bronchovascular bundles posteriorly.
Ashley Davidoff MD TheCommonVein.net 110Lu 136603
Alveolar Septal Amyloidosis
Scattered foci of nodular and calcified changes of secondary lobules involving the centrilobular region and interlobular septa. The affected secondary lobule in the right lower lobe abuts and involves the fissure
Ashley Davidoff TheCommonVein.net b11802
Alveolar Proteinosis
Excellent example of crazy paving
Ashley Davidoff TheCommonVein.net 117625
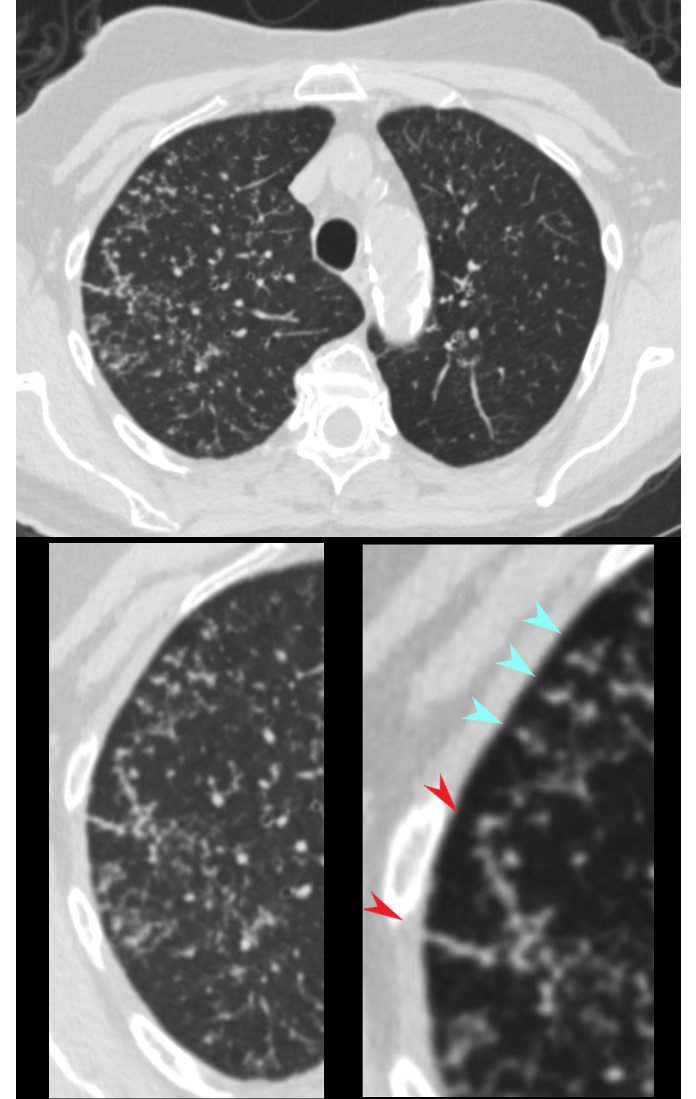
Acute Moderate CHF with Interstitial Edema
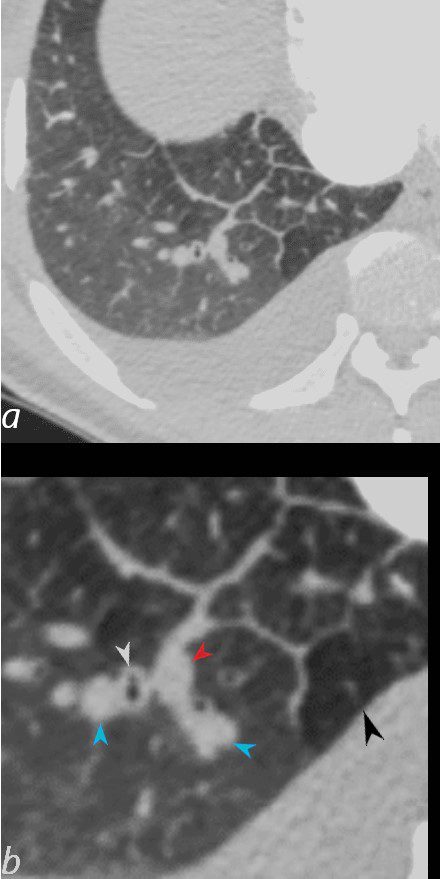
50-year-old female with diabetes, chronic renal failure and congestive heart failure. CT in the axial plane through the right posterior recess, shows thickened interlobular septa at the right base, congested arterioles (light blue arrowheads, b), alongside the bronchioles, peribronchial cuffing (white arrowheads, b), a congested pulmonary venule in the interlobular septum (red arrowhead arrowheads, b), ground glass changes and a secondary lobule demonstrating mosaic attenuation (black arrowhead arrowheads, b). The IVC is dilated and a small complex effusion is present.
Ashley Davidoff MD TheCommonvein.net 135783cL 193Lu
Irregular
51-year-old female smoker with a history of COPD asthma and pulmonary hypertension presents with progressive dyspnea. Axial CT through the upper lung fields shows extensive changes of centrilobular emphysema and an expanded group of secondary lobules noted in the right upper lobe Path confirmed a diagnosis of DIP
Ashley Davidoff MD TheCommonVein.net 252Lu 135963c
Nodular
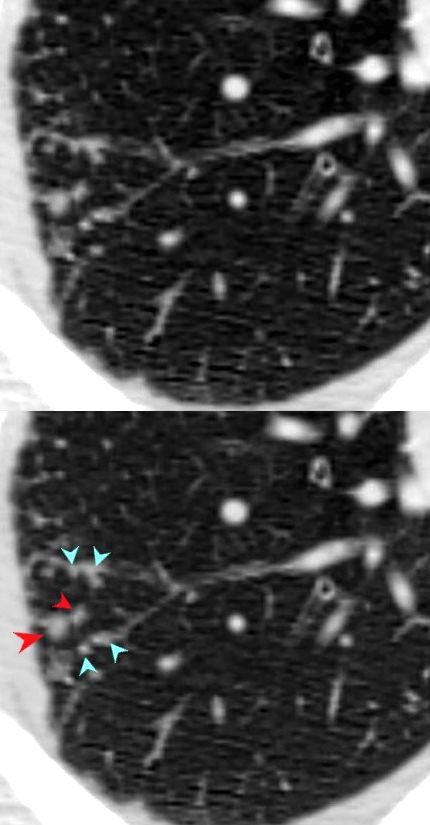
Small Airway Disease and Nodular Thickening of the Interlobular Septum -Right Upper Lobe
Active TB
CT in the axial plane shows extensive small airway disease dominant in the right upper lobe characterized by innumerable, ground glass micronodules, centrilobular nodules (teal blue arrowheads) and nodular thickening of the interlobular septa likely reflecting lymphatic involvement (red arrowheads)
Ashley Davidoff MD TheCommonVein.net 135825cL 192Lu
Sarcoidosis Interlobular and Intralobular Nodules
SARCOIDOSIS, ACTIVE – ALVEOLAR FORM
SARCOIDOSIS, ACTIVE – ALVEOLAR FORM
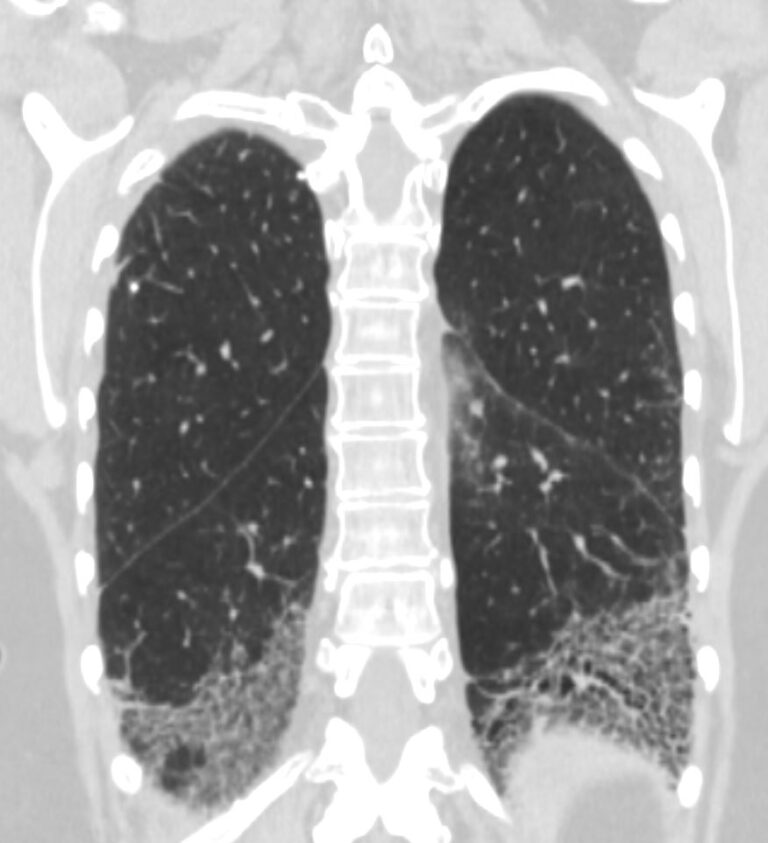
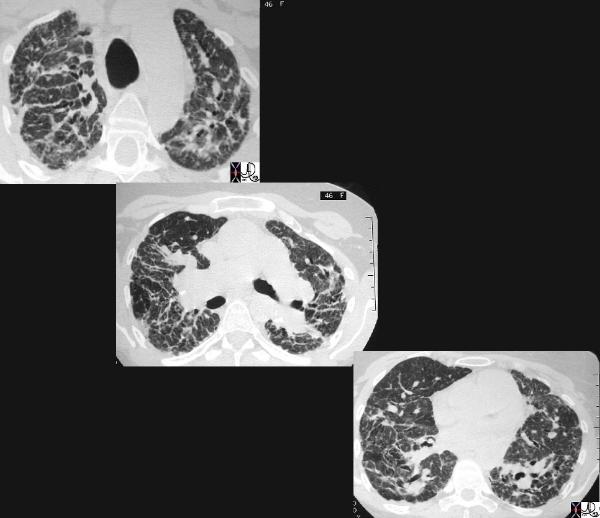
48-year-old previously well presented with dyspnea and initial CXR showed an infiltrate at the right base, and clinically resolved. He presented a year later with right chest pain and low grade ever and the CXR showed patchy opacities in the LUL and in the RLL
A subsequent CT showed LUL nodular opacities and subpleural rim of consolidation in the LUL and more prominently at both lung bases, associated with significant mediastinal adenopathy. Lymphovascular nodularity was noted in the bronchovascular bundles as well as in the interlobular septa, consistent with sarcoidosis
CXR and CT 4 years later showed almost complete resolution of the parenchymal findings and the CT findings except for minimal reticulation and scarring in the subpleural regions
Ashley Davidoff MD
Sarcoidosis End Stage Fibrotic
This cross sectional series of 3 CT images shows end stage sarcoidosis characterised by marked thickening along the lymphovascular bundles. The first image in the upper left shows marked thickening of the interlobular septa caused by granulomatous changes along the lymphatics. Courtesy Priscilla Slanetz MD. 31866c

Ashley Davidoff MD thecommonvein.net 134901-lungs UIP
Calcified Nodular
CALCIFICATION ALONG LYMPHOVASCULAR BUNDLES (red arrows)
INACTIVE SECONDARY TB WITH EXTENSIVE PARENCHYMAL AND LYMPHOVASCULAR INVOLVEMENT
48-year-old male with history of TB presents with back pain
AP view of the spine shows complex lesion in the right apex characterized by fibronodular opacities. There are scattered calcifications throughout the lungs but some are centered around the lymphatics, including the interlobular septa and centrilobular region
Ashley Davidoff MD TheCommonVein.net
Lymphangitis Carcinomatosis
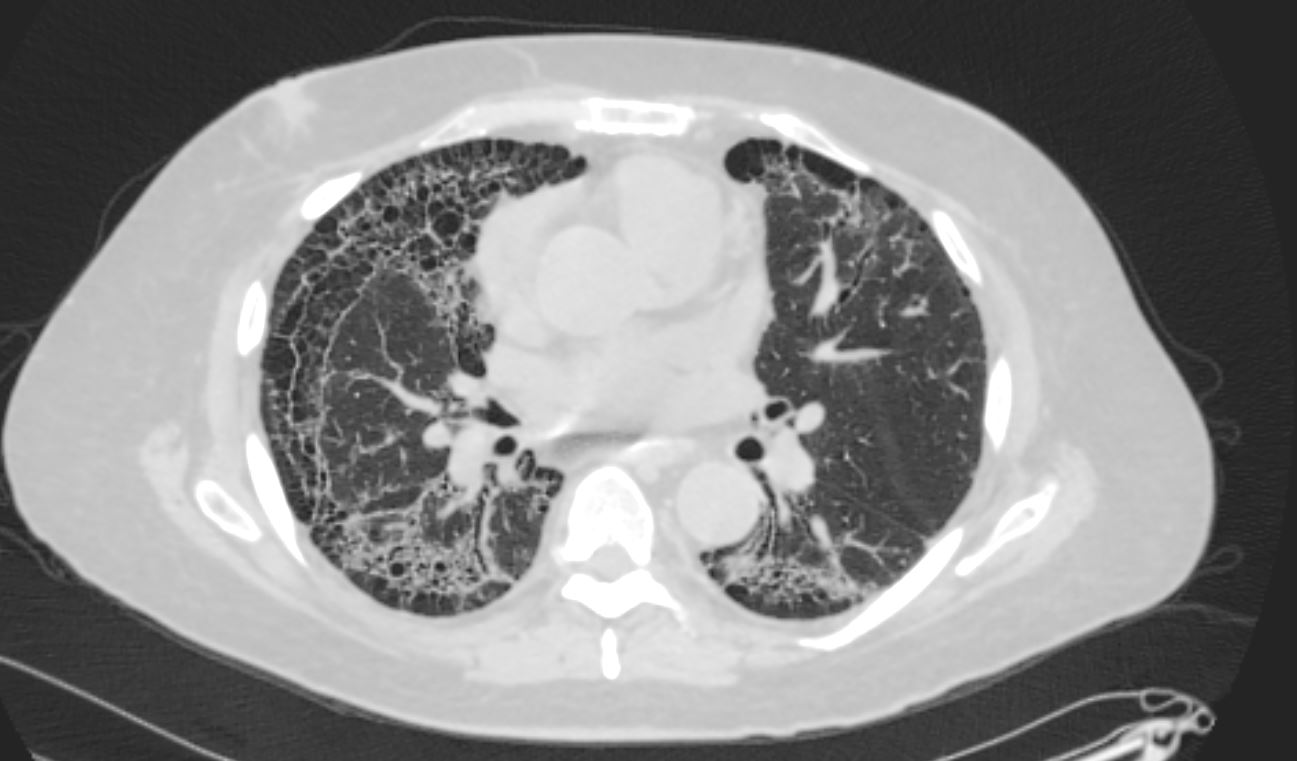
67-year-old man with prior history of bladder cancer. CT scan in the axial plane shows a large right upper lobe lung mass. Posterior to the mass, the interlobular septa are thickened.. These findings suggest lymphangitis carcinomatosis. Peribronchial thickening of the apical segmental airway may be due either to lymphangitis or chronic bronchitis There is background evidence of centrilobular emphysema, dominant in both upper lobes giving an internal comparison of the normal vs abnormal size of the interlobular septa
Ashley Davidoff MD TheCommonVein.net 32285c 243Lu

67-year-old man with prior history of bladder cancer. CT scan in the axial plane inferior to the lung mass shows extensive irregular thickening of the interlobular septa magnified in the right lower panel. These findings reflect lymphangitis carcinomatosis. There is background evidence of centrilobular emphysema, dominant in both upper lobes. A magnified view in the right lower panel offers an internal comparison of the abnormal vs the normal size and shape of the interlobular septa
Ashley Davidoff MD TheCommonVein.net 32287c 243Lu
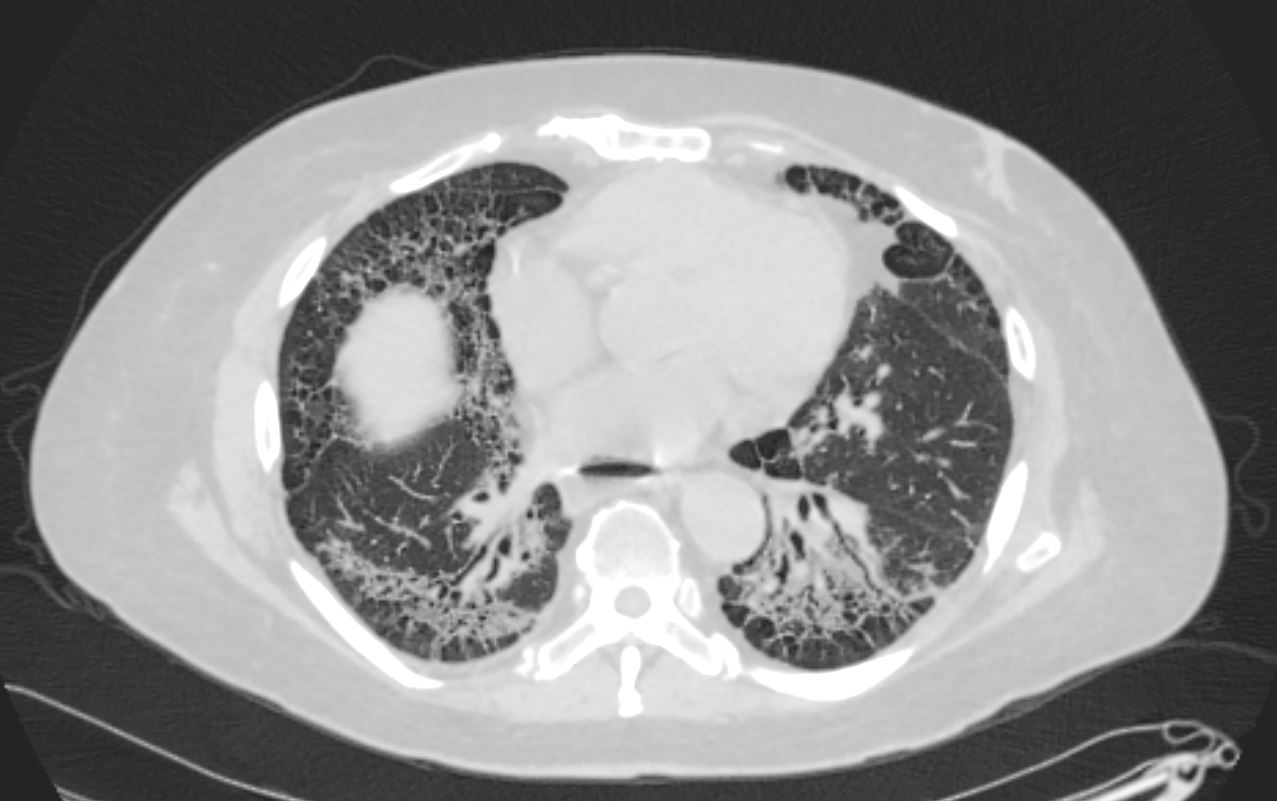
Adenocarcinoma of Left Lung with
Coarsened Septal Thickening LUL
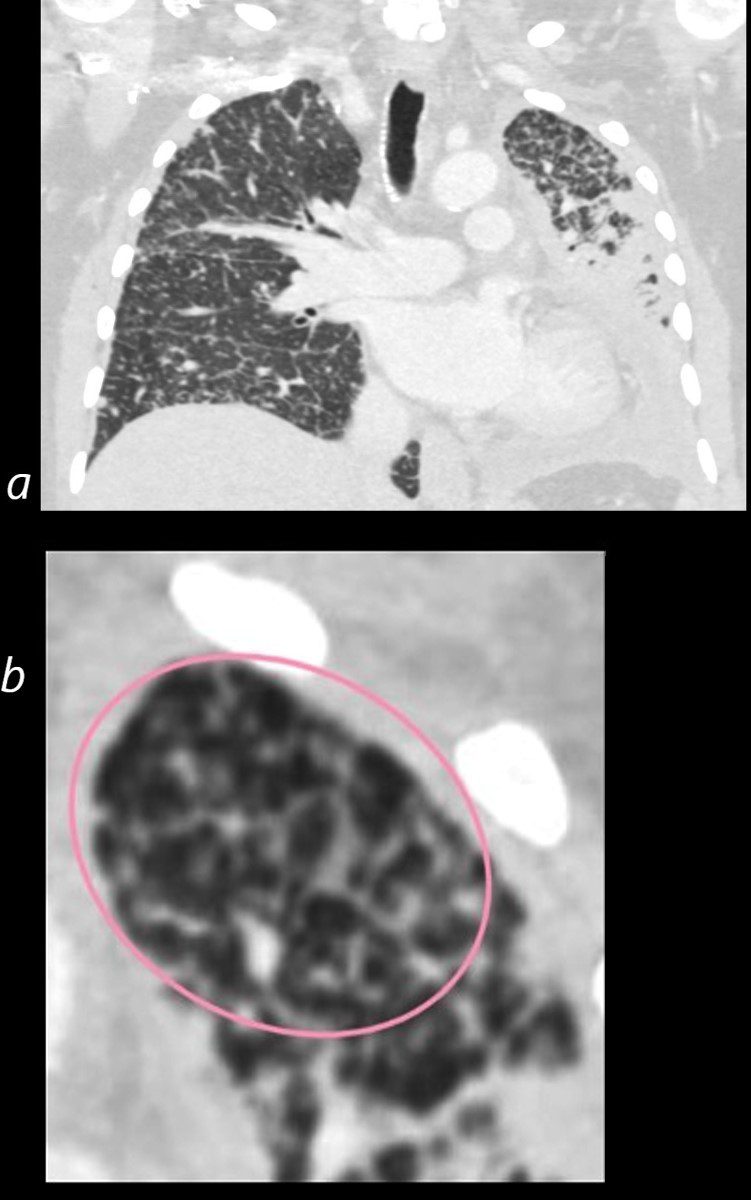
50 year old female with primary adenocarcinoma with the primary lesion presenting as pneumonic consolidation of the left lower lobe, and diffuse reticulonodular changes bilaterally
Image b is a magnified view of the left upper lobe and shows nodular thickening of the interlobular septa representing lymphatic spread along the lymphovascular bundles (pink oval)
The right lung shows interlobular septal thickening centrilobular nodules, and nodular thickening of the minor fissure
These findings are consistent with the diagnosis of lymphangitis carcinomatosa
Ashley Davidoff MD TheCommonVein.net 158Lu 131023c01L
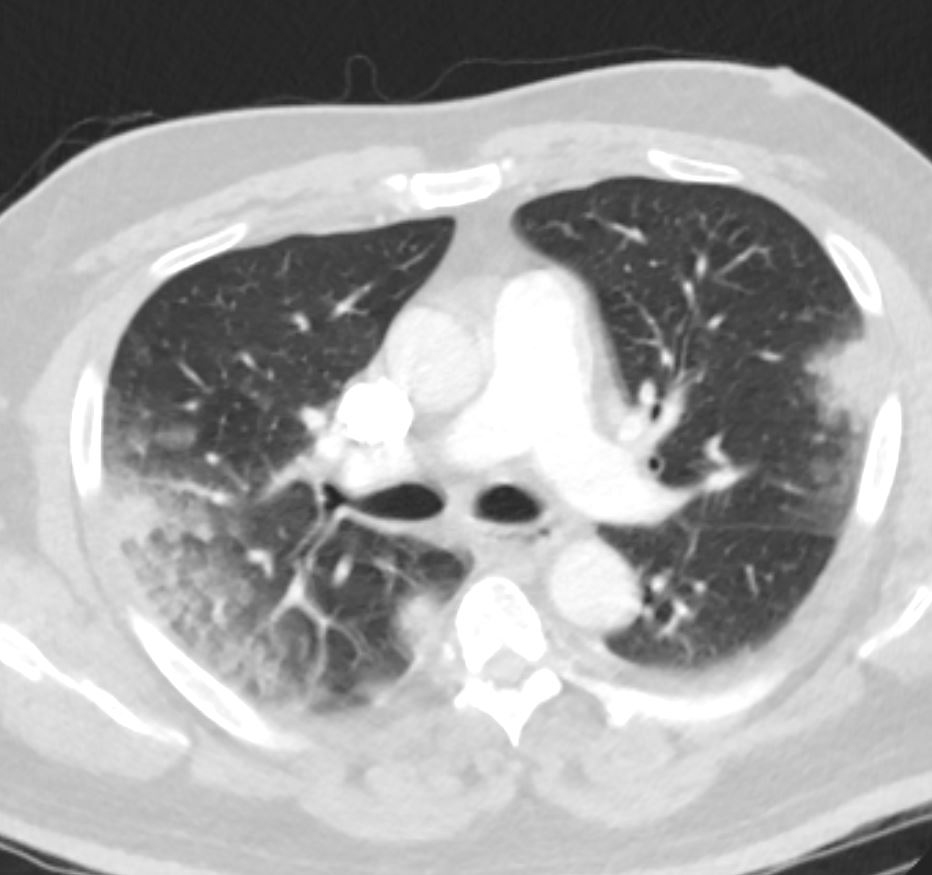
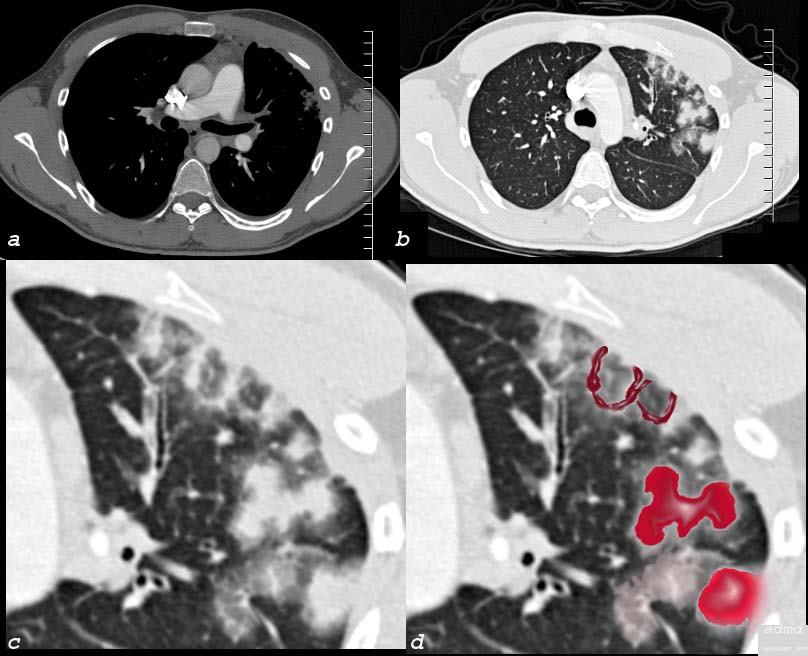
Primary Head and Neck Cancer and Lymphangitis
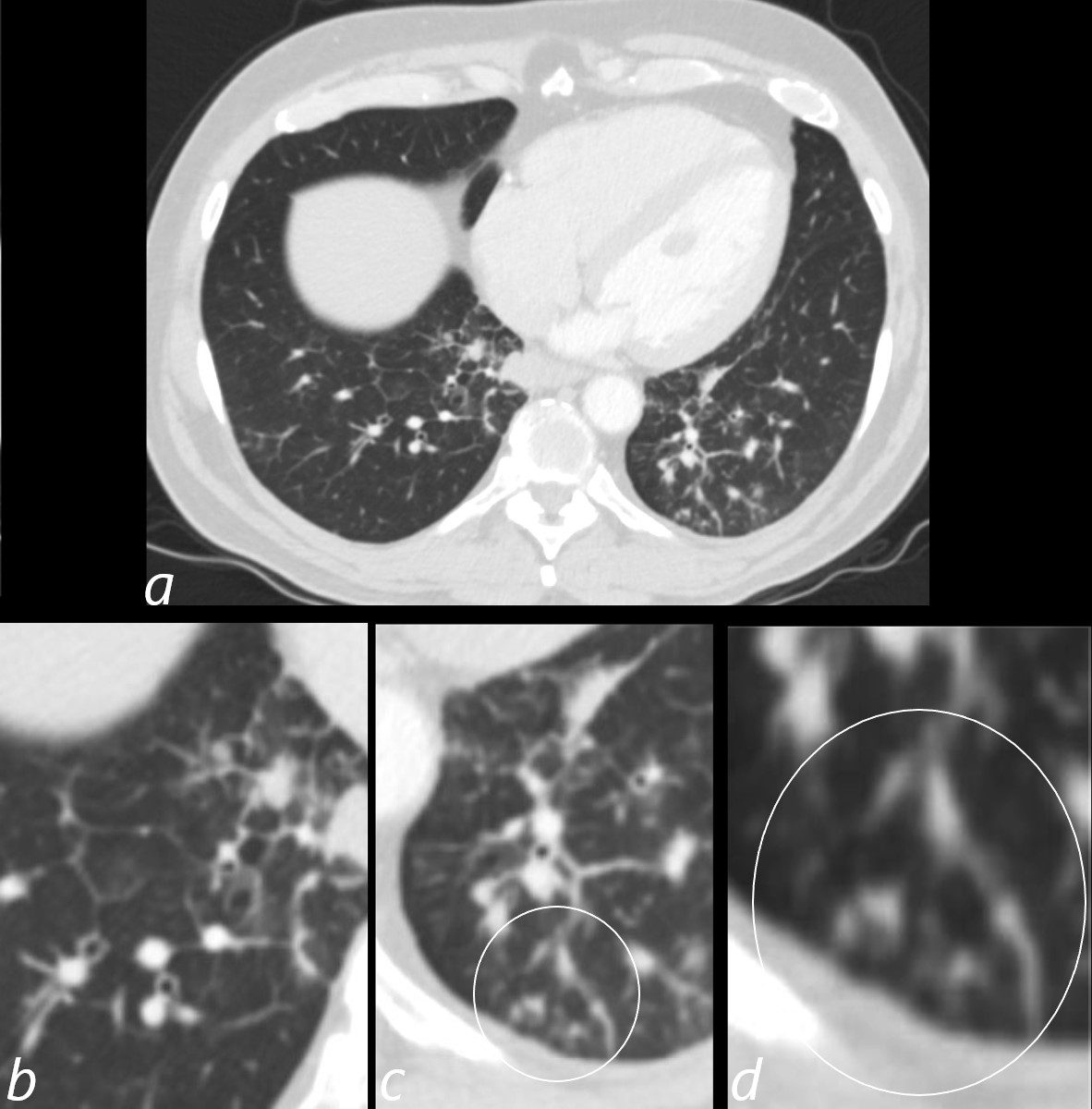
3 months later the patient presented with chest pain and a cough. CT of the chest in the axial plane shows new bilateral lower lobar regions of irregular interlobular septal thickening noted in the right lower lobe a, magnified in b). Ringed in image c and d are 2 side by side secondary lobules with irregular septal thickening centrilobular nodules and other intralobular nodules likely reflecting lymphatic involvement.
Given the changes in the right upper lobe these findings likely reflect lymphangitis carcinomatosa
Ashley Davidoff MD TheCommonVein.net 013Lu 136062cL
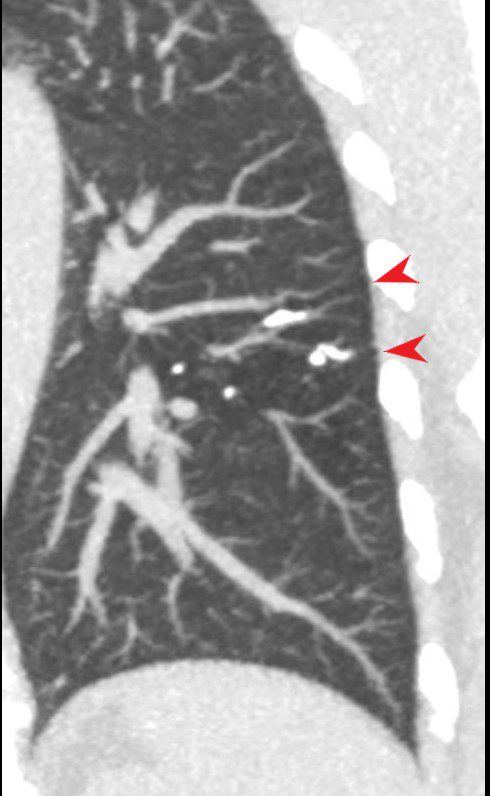
LIP
Post Ablation
26 year old male who presents with shortness of breath a few months following RFA ablation for atrial fibrillation. Image a shows the left upper lobe thrombosed and the left lower vein contrast filled
Image b (the lung windows) shows thickening of the interlobular septa and secondary lobules distended with material, porobably representing blood.
following male SOB s/p RFA ablation for atrial fibrillation lung pulmonary let upper lobe pulmonary vein thrombosed secondary lobule interlobular septa are thickened secondary lobule destroyed dx pulmonary vein thrombosis secondary to radiofrequency ablation therapy iatrogenic CTscan Courtesy Ashley Davidoff MD Scott Tsai MD key words
ground glass changes pulmonary infarction venous infarction
TheCommonVein.net 75413c02
- Smooth
- Interstitial Edema
- hemorrhage
- Verno-Oclusive Disease
- Lympangitic spread
- Lymphangiomatosis
- Amyloidosis
- Pneumonia
- Alveolar Proteinosis
- Nodular
- Lympangitic spread
- Lymphoproliferative Disease
- LIP
- Sarcoidosis
- Silicosis
- Pneumoconiosis
- Irregular
- End Stage Lung Disease
- Sarcoidosis
- UIP
- Asbestosis
- HP
- Peripharal Lobular
- IPF
- UIP
- OP
Links and References
- TCV