Histology of the Lung
Copyright 2007
lung histology classification the tissues of the lung derive from endoderm they are grouped together with other
Histology of the lung is the study of the microscopic structure of the lung.
The histological structure is characterised by the functional nature of the structures.
The conduction component is characterised by
air passages composed of ciliated pseudostratified columnar epithelium, (respiratory epithelium) whereas the
respiratory portion progresses from ciliated cuboidal epithelium to squamous epithelium.
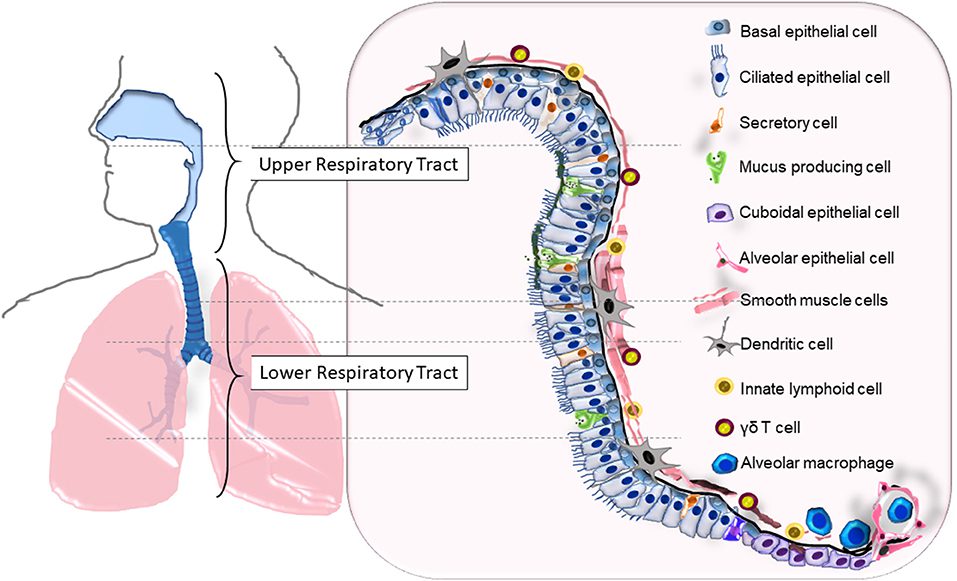
LeMessurier K.S et al Respiratory Barrier as a Safeguard and Regulator of Defense Against Influenza A Virus and Streptococcus pneumoniae Front. Immunol., 04 February 2020
Overview
A. Airway conductive system
B. Respiratory exchange system
A. Airway conductive system
The airway begins with the trachea which divides into two main bronchi which divides into lobar bronchi, which further divide into segmental bronchi. These bronchi keep dividing into smaller and smaller units. The smallest unit is called a bronchiole, which is less than 1mm.
Histologically, though the bronchi keep dividing they essentially retain the same structure.
The bronchi are composed of:
– Respiratory epithelium
– A thin Lamina Propria
– Bronchial smooth muscle (which forms a band around the bronchi)
– Hyaline cartilage (surrounding the bronchi in plates.)
As the bronchi divide from primary to tertiary bronchi:
– the epithelium changes from pseudostratified ciliated columnar epithelium to ciliated columnar epithelium with goblet cells.
– The walls of the bronchi become thinner.
– The hyaline cartilage decreases
– The smooth muscle increases.
The bronchioles are the smallest structures in the conductive passages. They are surrounded only by smooth muscle, as the hyaline cartilage is not present anymore.
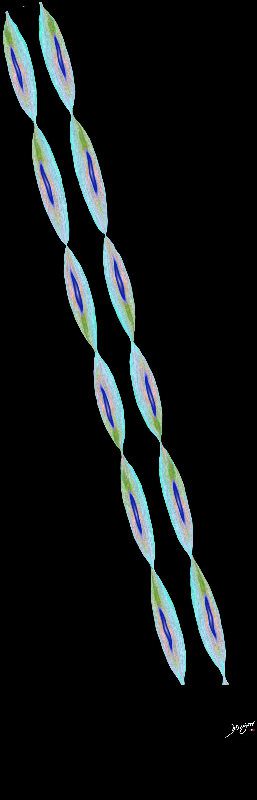
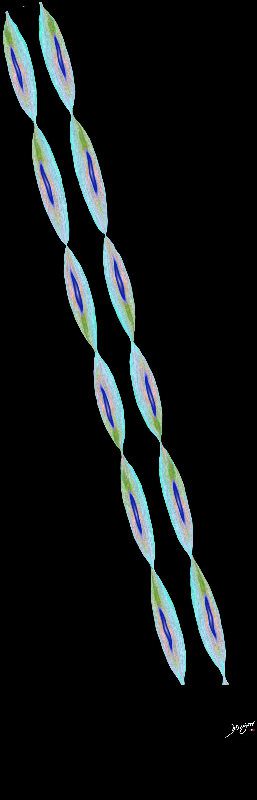
van den Bosch, W. B. et al Structure and function of small airways in asthma patients revisited
European Respiratory Review 2021 30: 2001
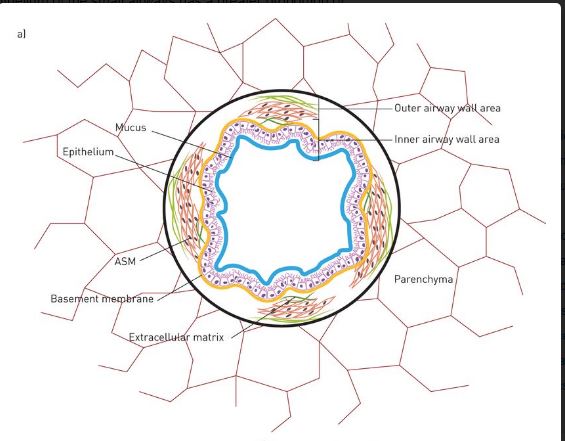
van den Bosch, W. B. et al Structure and function of small airways in asthma patients revisited
European Respiratory Review 2021 30: 2001
The larger bronchioles are lined by ciliated columnar epithelium with goblet cells while the smaller ones also called terminal bronchioles are lined by ciliated cuboidal epithelium with no goblet cells.
B. Respiratory Exchange
This is achieved by the respiratory bronchioles, which are divisions of the terminal bronchioles.

This diagram illustrates the acinus which consists of the respiratory bronchioles (rb 1, 2, 3) the alveolar duct (ad) the alveolar sac (as) and the alveoli. (a)
Courtesy Ashley Davidoff MD 42446b12
TheCommonVein.net
The respiratory bronchioles are transition zones between the conductive passages and the respiratory portion.
They give rise to the alveoli, which coalesce to form alveolar ducts that end into alveolar sacs.
It is between the alveoli and the capillaries that surround it that the gas exchange takes place.
Histologically, the epithelium progresses from cuboidal epithelium without cilia to squamous epithelium as the respiratory bronchioles turn into alveoli and alveolar ducts.
Ashley Davidoff
TheCommonVein.net
Ashley Davidoff
TheCommonVein.net
Ashley Davidoff
TheCommonVein.net
Principles
ng histology principles implies the principles of normal structure at the level of the tissue the tissue can be described by its size shape position character it is made up of characteristic parts which are surrounded by a capsule for its integrity and functionality it depends on support from other tissues and requires life line type connections to allow it to survive and to integrate structurally and functionally with other tissues vascular connections include structures that provide blood supply and drainage the tissues occupy space and share the space with neighbours the tissues change with time and specific physiologic events
Parts
The lung is structurally divided into two parts: the airways and the air filled sacs.
1.The airways
The airways are lined by pseudostratified ciliated columnar epithelium, cartilage and goblet cells. The bronchial mucosa contains neuroendocrine cells which have neurosecretory granules. These on stimulation, secrete serotonin, calcitonin and gastrin releasing peptide ( bombesin). There are submucosal glands scattered through the trachea and bronchi but not the bronchioles. Bronchi are distinguished from bronchioles primarily by the presence of cartilage in their walls and the presence of submucosal glands.




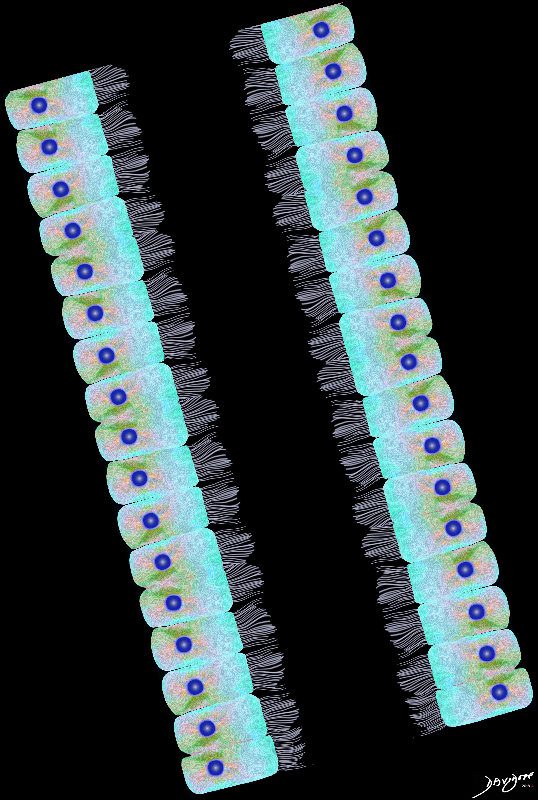
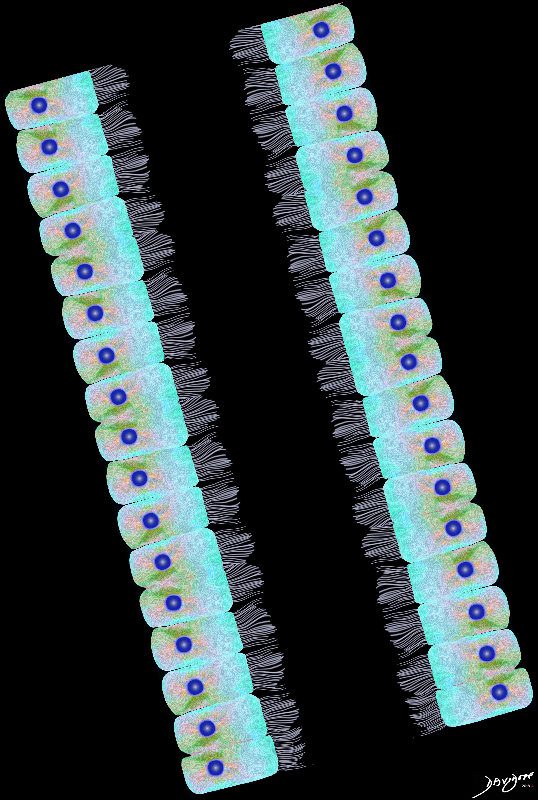
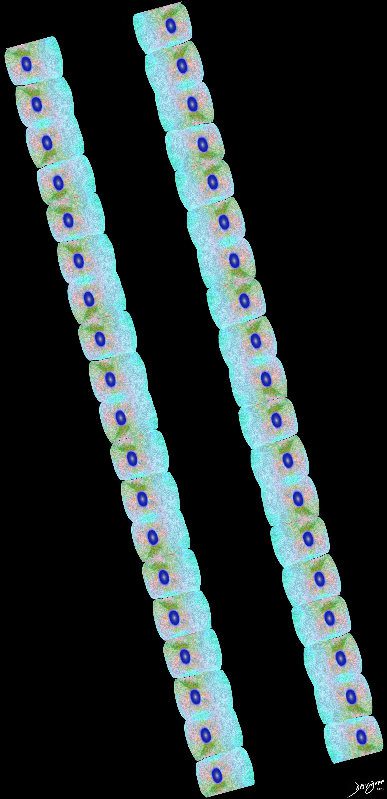
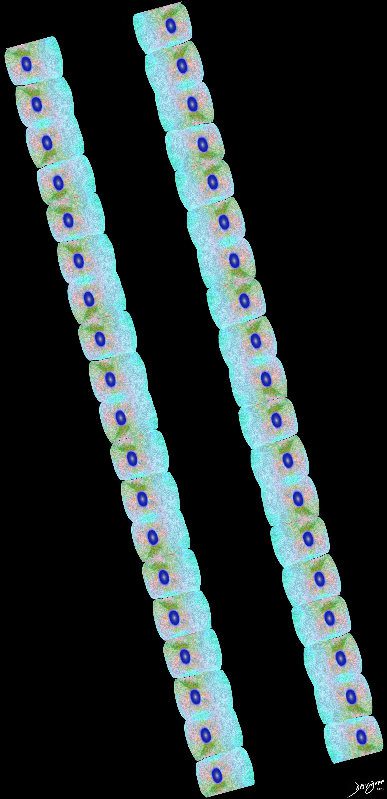
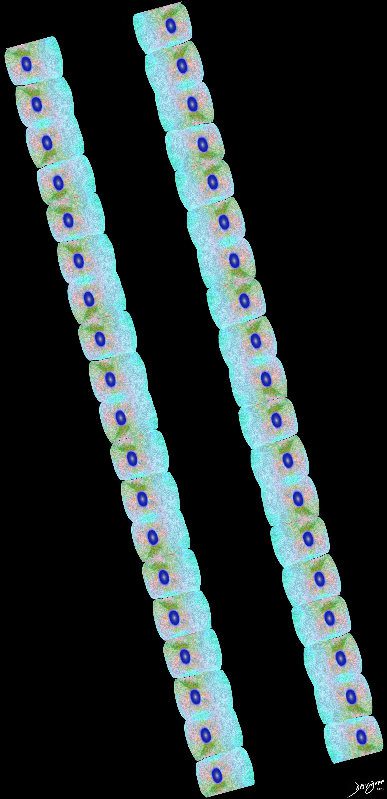
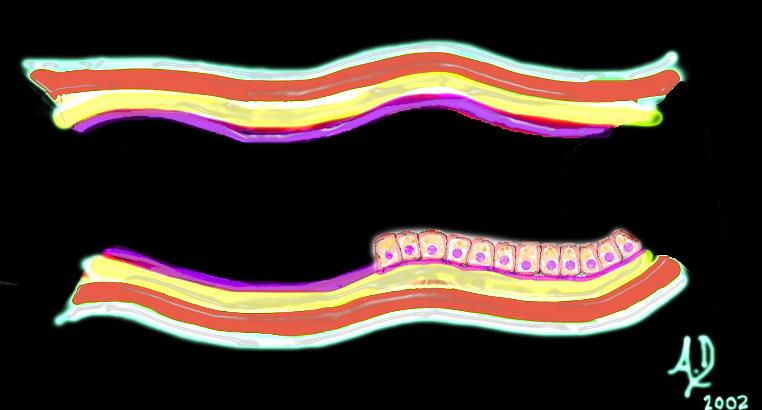
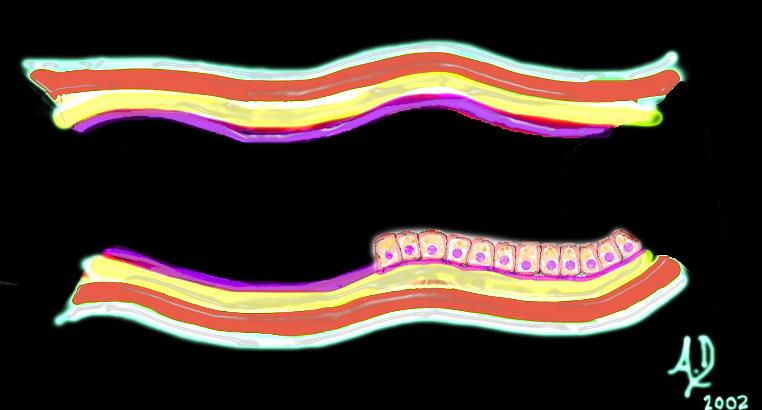
Airways are lined by a pseudostratified ciliated columnar epithelium interspersed with mucus secreting goblet cells
Ashley Davidoff
TheCommonVein.net
2. Alveolar region
The alveolar region is a branching system of alveolar ducts whose walls are made of alveoli. The alveolar ducts end into alveolar sacs which contain alveolar outpouches. The alveoli thus forms the walls of alveolar ducts and sacs. The openings or the mouths of alveoli consist of a dense network of elastic and collagen fibers. Adjacent alveoli are connected by a thin collagen fibers in a spiral or helical fashion which are important in support and compliance of the gas exchange region.



The Buck Ends Here
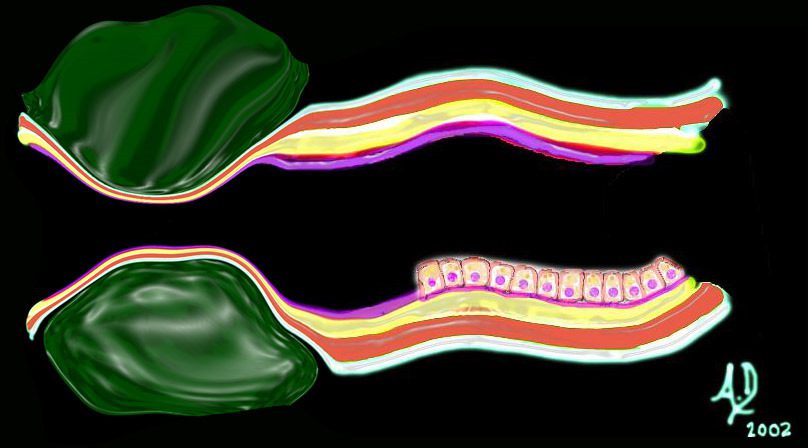
The alveolus is lined by a simple epithelium – one cell layer thick. There are two types of lining cells; Type 1 pneumocytes are squamous cells that cover 90% of the surface of the inner lining of the lung , and type II cuboidal pneumocytes that are in fact much more numerous than Type I. They are involved in the production of surfactant . In the lumen there are resident macrophages which play a crucial role in the immune system. The mucosa is grounded by a basement membrane and a lamina propria, and connected to the lamina propria and basement membrane of the surrounding capillary. The alveolus is lined by a thin layer of surfactant. (teal blue)
Ashley Davidoff TheCommonVein.net
The structure of the alveolar walls (alveolar septa) from blood to air:
1. Capillary endothelium – a dense anastamotic network of capillaries
2. Basement membrane of the capillaries.
3. Alveolar Basement membrane- In the thinner parts of the alveolar walls the basement membrane of the epit helium and endothelium are fused whereas in the thicker parts they are separated by pulmonary interstitial tissue containing collagen and elastic fibers, interstitial cells, smooth muscle cells, mast cells and scattered lymphocytes and monocytes.
4. Alveolar epithelium- This primarily consists of two types of cells:
a. Type 1 pneumocytes [ membranous pneumocytes]- flattened pavement type cells.
b. Type 2 pneumocytes- rounded cells which secrete surfactant contained in osmiophilic lamellar bodies in the cells.These cells are also serve the function of repair of the alveolar epithelium after the destruction of the type 1 pneumocytes
Trachea




Airways are lined by a pseudostratified ciliated columnar epithelium interspersed with mucus secreting goblet cells
Ashley Davidoff
TheCommonVein.net
– Pseudostratified coloumnar epithelium
– Goblet cells
– Clara cells
– Serous and mucous cells
– Lamina propria
– Submucosal glands
– Hyalin cartilage
Bronchi




Airways are lined by a pseudostratified ciliated columnar epithelium interspersed with mucus secreting goblet cells
Ashley Davidoff
TheCommonVein.net
– Pseudostratified, ciliated columnar epithelium
– Goblet cells (few)
– Sero-mucous glands
– Hyaline Cartilage
– Smooth muscle
Bronchioles
– Simple columnar or cuboidal & ciliated epithelium
– No goblet cells
– Smooth muscle (relatively abundant)
– Clara cells
Ashley Davidoff
TheCommonVein.net
Respiratory Bronchiole
– Simple cuboidal, ciliated epithelium (shorter)
– Clara cells
– Alveolar openings
Alveoli



The Buck Ends Here
The alveolus is lined by a simple epithelium – one cell layer thick. There are two types of lining cells; Type 1 pneumocytes are squamous cells that cover 90% of the surface of the inner lining of the lung , and type II cuboidal pneumocytes that are in fact much more numerous than Type I. They are involved in the production of surfactant . In the lumen there are resident macrophages which play a crucial role in the immune system. The mucosa is grounded by a basement membrane and a lamina propria, and connected to the lamina propria and basement membrane of the surrounding capillary. The alveolus is lined by a thin layer of surfactant. (teal blue)
Ashley Davidoff
TheCommonVein.net
– Simple Squamous Epithelium
Cell Type
– In the trachea- serous and mucous cells- secrete fluid, protection of airway.
– In the bronchi – Goblet cells- secrete mucus, protection of the airway.
– In the Bronchioles Terminal and Respiratory – Clara cells – nonciliated, rounded secretory cells –produce a surfactant like compund.
– In the alveolus….?
Type I Pneumocyte
Simple squamous epithelium with pale staining cytoplasm
– flattened for gas exchange, forms a part of the Blood-Gas Barrier
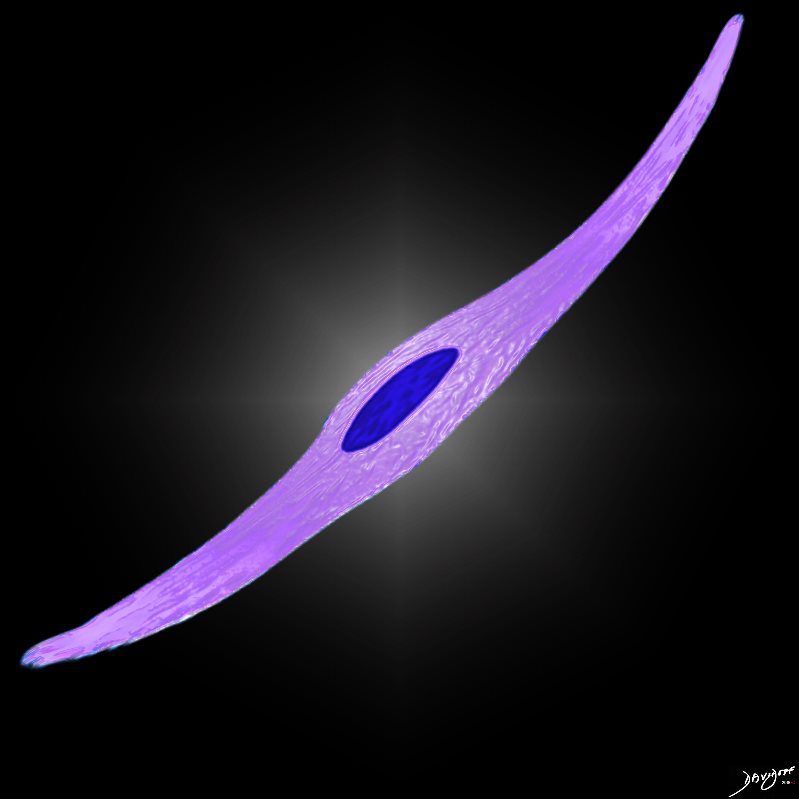
– flattened for gas exchange, forms a part of the Blood-Gas Barrier
Ashley Davidoff
TheCommonVein.net
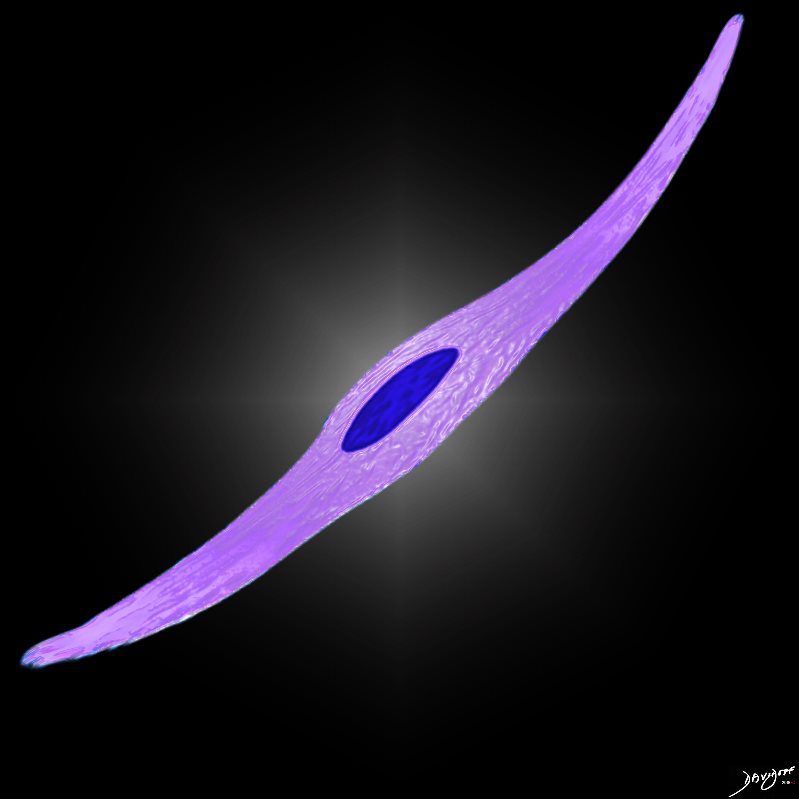
Type II Pneumocyte


It produces the phospholipid – part of the surfactant that reduces surface tension and allows the alveoli to remain open
Ashley Davidoff
TheCommonVein.net
– cuboidal
– reddish foamy and sometimes vacuolated cytoplasm
– produces the phospholipid part of the surfactant that reduces surface tension and allows the alveoli to remain open
Alveolar Macrophages
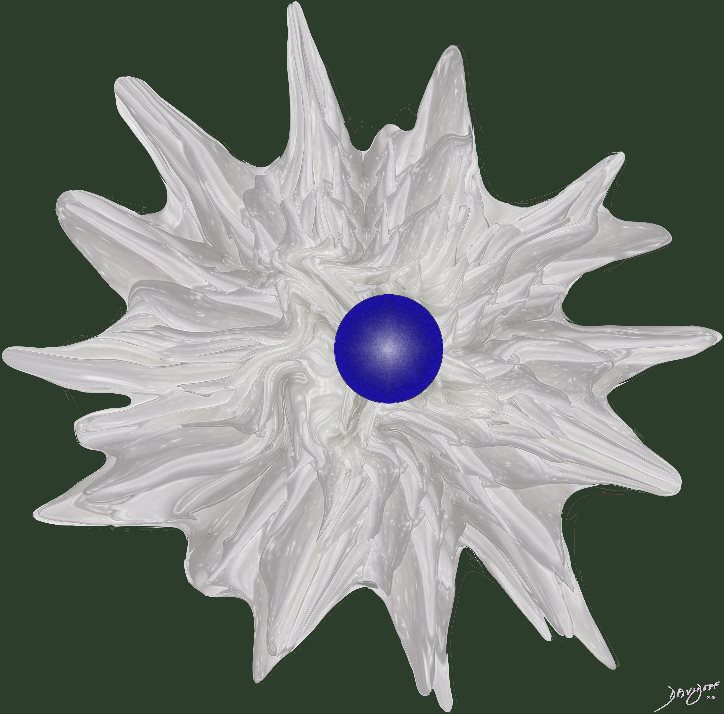
First line of defense against infections of the lung.
Reside in alveolar walls, lymphatic channels and lymph node.
Originate in the bone marrow and are part of the Mononuclear Phagocytic System.
Ashley Davidoff
TheCommonVein.net
– First line of defense against infections of the lung.
– Reside in alveolar walls, lymphatic channels and lymph node.
– Originate in the bone marrow and are part of the Mononuclear Phagocytic System.
Pleura
– Visceral
– Parietal
The visceral and parietal pleura are smooth serous membranes continuous with each other at the lung hila. The pleural space is a cavity between the 2 pleurae into which the lung protrudes. The visceral pleura is the one that covers both the lungs. The parietal and visceral pleurae are separated by a thin layer of fluid. This fluid contains molecules secreted by the mesothelial cells of the pleura which have surfactant like properties.
• Diseases that affect the pleura are:
• Pleural Effusion:
• Inflammatory Pleural Effusions
: Serous, serofibrinous, and fibrinous pleuritis.
• Noninflammatory Pleural Effusions: Noninflammatory collections of serous fluid within the pleural cavities are called hydrothorax.
• The presence of blood into the pleural cavity is known as hemothorax. It is usually a complication of a ruptured aortic aneurysm or vascular trauma. Pure hemothorax is readily identifiable by the large clots that accompany the fluid component of the blood.
• Chylothorax is an accumulation of milky fluid, usually of lymphatic origin, in the pleural cavity. When the fluid is allowed to stand, a creamy, fatty, supernatant layer separates. True chyle can be differentiated from turbid serous fluid due to the fact that serous fluid does not contain fat and does not separate into an overlying layer of high fat content. Chylothorax may be bilateral but is more often confined to the left side.
Pneumothorax:Pneumothorax refers to air or gas in the pleural cavities and may be spontaneous, traumatic, or therapeutic. Pneumothorax can be identified anatomically only by careful opening of the thoracic cavity under water to detect the escape of gas or air bubbles. Pneumothorax can compression, collapse, and atelectasis of the lung and may be responsible for marked respiratory disdistress.
• Tension pneumothorax, can compress the vital mediastinal structures and the contralateral lung.
• Pleural Tumors
• Pleural Fibroma: This is a benign pleural neoplasm, sometimes called benign mesothelioma. Microscopically the tumors show whorls of reticulin and collagen fibers among which are interspersed spindle cells resembling fibroblasts.
• Malignant mesotheliomas
Sarcoidosis
Although sarcoid nodules seek out the lymphatics of the pleura, pleural effusions are distinctly uncommon (1-4%)
Pleura
– Visceral
– Parietal
The visceral and parietal pleura are smooth serous membranes continuous with each other at the lung hila. The pleural space is a cavity between the 2 pleurae into which the lung protrudes. The visceral pleura is the one that covers both the lungs. The parietal and visceral pleurae are separated by a thin layer of fluid. This fluid contains molecules secreted by the mesothelial cells of the pleura which have surfactant like properties.
• Diseases that affect the pleura are:
• Pleural Effusion:
• Inflammatory Pleural Effusions
: Serous, serofibrinous, and fibrinous pleuritis.
• Noninflammatory Pleural Effusions: Noninflammatory collections of serous fluid within the pleural cavities are called hydrothorax.
• The presence of blood into the pleural cavity is known as hemothorax. It is usually a complication of a ruptured aortic aneurysm or vascular trauma. Pure hemothorax is readily identifiable by the large clots that accompany the fluid component of the blood.
• Chylothorax is an accumulation of milky fluid, usually of lymphatic origin, in the pleural cavity. When the fluid is allowed to stand, a creamy, fatty, supernatant layer separates. True chyle can be differentiated from turbid serous fluid due to the fact that serous fluid does not contain fat and does not separate into an overlying layer of high fat content. Chylothorax may be bilateral but is more often confined to the left side.
Pneumothorax:Pneumothorax refers to air or gas in the pleural cavities and may be spontaneous, traumatic, or therapeutic. Pneumothorax can be identified anatomically only by careful opening of the thoracic cavity under water to detect the escape of gas or air bubbles. Pneumothorax can compression, collapse, and atelectasis of the lung and may be responsible for marked respiratory disdistress.
• Tension pneumothorax, can compress the vital mediastinal structures and the contralateral lung.
• Pleural Tumors
• Pleural Fibroma: This is a benign pleural neoplasm, sometimes called benign mesothelioma. Microscopically the tumors show whorls of reticulin and collagen fibers among which are interspersed spindle cells resembling fibroblasts.
• Malignant mesotheliomas
Sarcoidosis
Although sarcoid nodules seek out the lymphatics of the pleura, pleural effusions are distinctly uncommon (1-4%)
Support Structures
The support to the lung is given by the connective tissue surrounding the lung as well as the connective tissue inside the lung.
This can be divided into 2 parts depending on the characteristics of the interstitial tissue.
1. Parenchymal or alveolar wall interstitial tissue – The parenchymal connective tissues are extensions of the loose- binding connective tissue. During inflation of the lung the pressure in the alveoli is transmitted to adjacent alveoli to the alveolar ducts to the bronchioles and then to the loose- binding connective tissue supporting a lung lobule and ultimately to the visceral pleura. This equalizes the pressure through the entire lung and prevents it from collapsing. The interstitial tissue is made up of glycosaminoglycans which forms a gel like matrix which also provides support.
2. Loose binding or extra alveolar connective tissue – peribronchiovascular sheath, interlobular septa and visceral pleura. The connective tissue fibers form a network around the airways and airspaces which allows the lung to expand and prevents excess tissue recoil and so preventing their collapse.
ALVEOLAR DUCT
The connective tissue bundles of the alveolar duct walls are arranged in a spirals They play an important role in defining the overall integrity and compliance of the alveolar ducts and sacs
ALVEOLI
The mouths of the alveoli, are suported by collagen and elastin bundles. Adjacent alveoli are supported by interconnecting collagen fibers that course through the alveolar walls.
The Acinus
The bronchi proceed from the mainstem bronchus via 16 to 23 divisions into the terminal bronchioles. Thereafter sac-like protrusions develop in the system, which allow gas exchange to start taking place. The first branch that is able to perform this gas exchange is called the respiratory bronchiole. After three divisions the respiratory bronchioles become alveolar ducts and after further division become alveolar sacs. Finally, at the terminal end of this pathway, are the alveoli. The system that starts at the respiratory bronchiole and terminates at the alveoli is called an acinus, and it is functionally characterized by having the ability to both conduct air as well as enable gas exchange. The acinus averages about 7mm in diameter. When it is filled with fluid, it can be visualized on a CXR as a 6mm density called an “acinar shadow.” As a structural entity it has little diagnostic utility. We will expand on the pulmonary lobule in the next section which has greater implications for the imaging of the lung. Functionally, however, the acinus can be considered as the unit of gas exchange in the lung.



This diagram illustrates the acinus which consists of the respiratory bronchioles (rb 1, 2, 3) the alveolar duct (ad) the alveolar sac (as) and the alveoli. (a)
Courtesy Ashley Davidoff MD 42446b12
TheCommonVein.net



The acinus with its arborizations is shaped more like a bunch of grapes.
Courtesy of: Ashley Davidoff, M.D 42650
TheCommonVein.net
Size
– The trachea is 10-12 cm in length with a diameter of about 2 cm.
– Bronchi – diameter less than 1mm.
– Terminal bronchioles- diameter less than 0.5 mm
General diamters of the downstream airways include lobular and segmental bronchi (5-8mm), subsegmental bronchi and bronchiole (1.5-3mm), lobular bronchiole (1mm), terminal bronchiole (.7mm) and acinar bronchiole (.5mm). (Webb, Muller, Naidich.)
– Each alveolus is about 200 microns in diameter. There are about 300 million alveoli present in the lung which provides about 140 square meters of surface area for gas exchange.
– The thickness of the blood air barrier varies from 1 to 1.5 microns in thickness.
There are between 3 and 13 alveolar duct branches which terminate in alveolar sacs. The human lung contains about 500 million alveoli which are about 225 mum in diameter and are roughly spherical in shape.
An acinus averages 0.75 mm in diameter.
Shape
The trachea is made up of different layers, each layer is composed of a different tissue.
– Respiratory epithelium
– Basement membrane
– Submucosal glands which contain small blue cells – lymphocytes
– Perichondrium
– Tracheal cartilage
– Trachealis smooth muscle
– Bronchi
The shape and structure of the bronchi is similar to that of the trachea except for:
– The cartilage is replaced by plates of cartilage
– Serous and mucous glands are present but fewer in number.
Bronchioles
– Tubes with circular smooth muscle and lacking cartilage and glands. They contain Clara cells.
Alveolar ducts and alveolar sacs
– These consist of alveoli which are air filled sacs with a dense capillary network around them.
The alveolus is roughly rounded in shape
Position
The lung is divided structurally and functionally into 2 parts
1. The ventilatory part or the ductal system
This consists of the trachea, 2 main bronchi and bronchioles right upto the terminal bronchioles. The other functions of the airways or ducts are moistening and filtering of air before it reaches the blood-air barrier for exchange.
2. The respiratory portion
This consists of the respiratory bronchioles, alveolar ducts and alveolar sacs. The alveoli contain type 2 pneumocytes which secrete surfactant which reduces surface tension and duct cells or alveolar macrophages which are the first line cells in defense.
Principles
ng histology principles implies the principles of normal structure at the level of the tissue the tissue can be described by its size shape position character it is made up of characteristic parts which are surrounded by a capsule for its integrity and functionality it depends on support from other tissues and requires life line type connections to allow it to survive and to integrate structurally and functionally with other tissues vascular connections include structures that provide blood supply and drainage the tissues occupy space and share the space with neighbours the tissues change with time and specific physiologic events
Connections
The connective tissue fibers of the visceral pleura are continuous with bronchovascular sheaths surrounding the conducting airways and the pulmonary arteries and veins. These airways and blood vessels can be considered as lying within tunnels in the lung parenchyma. The pulmonary vein contains some cardiac tissue as it approaches the left atrium.
lung histology connections the tissues of the xx form a continuum within the aa that starts at the xx and ends at the xx mucosal transition from the xx is from a bb epithelium to a cc epithelium the xx has a similar type cc epithelium the tissues are connected to the rest of the body by the vascular system nervous system lymphatic system and endocrine system ligamentous connections of the xx are to the xx and xx
Blood Supply
The blood supply to the lung is from 2 sources:
1. Pulmonary circulation
2. Bronchial circulation
1. Pulmonary Circulation
The pulmonary circulation is set apart from the other systemic circulations by the fact that has a smaller amount of smooth muscle and less surrounding tissue, thus making it more distensible and increasing its capacitance.
The pulmonary circulation can be divided into 2 on the bases of the connective tissue compartments
a. Extralveolar pulmonary circulation- These vessels lie in the loose-binding connective tissue. Eg. Peribronchovascular sheaths, interlobular septa. These vessels have loose connective tissue sheaths and supply the lung right up to the terminal bronchioles. The extra alveolar branches have a large amount of elastic fibers [elastic pulmonary arteries] which decrease in number as the diameter of the vessel decreases. An additional muscular layer also appears in the smaller arteries [muscular pulmonary arteries]. The muscular arteries supply the lung lobules and accompany the bronchioles.
b. Alveolar pulmonary circulation- These blood vessels run in the parenchymal connective tissue around the alveolar walls. These are pulmonary arterioles which arise from the muscular arteries but the muscle fibers gradually get fewer in number until all that the vessel wall is composed of is a single layer of endothelial cells and an elastic lamina.
The pulmonary arteries enter into the respiratory units whereas the veins occupy the surrounding connective tissue. Each artery supplies a specific zone of tissue whereas each vein drains many such zones.
The pulmonary arterioles branch out to form capillaries which runs across several
Venous Drainage
The venous drainage from the lungs is divided into two types:
1. Pulmonary veins
Pulmonary veins are thinner than the arteries because the muscular is not well developed. The pulmonary arterioles branch out to form capillaries which runs across several alveoli before forming venules. These venules run through the connective tissue which surrounds the alveoli. Therefore, each venule drains a number of alveoli. The venules unite to form progressively larger veins which finally form the lobar vein whch drains the pulmonary lobes. These lobar veins ultimately terminate into superior and inferior pulmonary veins.
2. Bronchial Veins
Bronchial veins arise from the bronchial capillaries. Some of these venous units join pulmonary veins to form bronchopulmonary veins. The bronchial veins ultimately drain into the azygous, hemiazygos or the intercostals veins.
Lymphatic Drainage
The lungs have an extensive lymphatic system, which helps to maintain homeostasis and is involved in defense mechanisms. They run alongside the pulmonary blood vessels.
The lymphatic vessels can be divided into 2 parts:
1. Superficial plexus- located in the connective tissue visceral pleura.
2. Deep plexus- located in the peri-bronchovascular connective tissue sheaths.
The superficial and deep plexuses communicate in the interlobular septa.
There are no lymphatic channels present in the alveolar walls.
Lymphoid tissue: is distributed along the tracheobronchial tree. Some tissue is also present along the blood vessels. The lymphoid tissue is involved in both cell mediated as well as antibody mediated immune response.
The alveoli lack lymphatics. The lymphatics first appear in the distal small bronchioles. Lymph nodes are positioned along the 2nd or third order branches of the bronchi.
The radiologist is usually only able to see the lymph nodes of the hilum.
Nerve Supply
The lung has a rich nerve supply.
It can be divided into:
– Sensory nerve supply
– Motor nerve supply
Sensory nerve supply
This supplies the alveoli and bronchioles. They are unmyelinated [ C fibers] and originate in the airway epithelium, submucosa, interalveolar septa and smooth muscle. The afferent fibers are part of the vagus [parasympathetic] nerve and terminate in the vagal nuclei in the medulla oblongata.
Motor nerve supply
Has both a sympathetic and parasympathetic nerve fibers.
– Sympathetic nerve supply [causes dilatation]
Upper 4 or 5 thoracic paravertebral ganglia[preganglionic fibers] airway, endothelial cells, submucosal glands [postganglionic fibers].
-Parasypmathetic nerve supply [ causes constriction] Brainstem motor nuclei of vagus [ preganglionic fibers] –>smooth muscle and cartilage.
Trachea
The trachea has both cholinergic and adrenergic fibers situated in the submucosa, around the trachea glands and stimulate them to release a seromucous secretion.
There are clusters of neuroendocrine cells distributed along the airway epithelium right upto the alveolar ducts, situated at airway bifurcations. These cells are storage sites of serotonin, dopamine, norepinephrine, bombesin, and calcitonin. Neurons supplying the neuroendocrine cells are storage sites of Vasoactive intestinal peptide and Substance P.
Time – Embryology Growth and Aging
The lung has 2 embryonic origins
Primitive foregut endoderm and the lateral mesoderm.
There are 3 stages in the embryological development of the lung:
– Glandular period: 5th to 17th week of gestation. Lung development commences at 26th day of gestation from the foregut.It invades the splanchnic mesoderm at 4.5 weeks and starts to form saccules which lasts till 7 weeks. These saccules are the future lobar bronchi. Branching continues to form subsegmental branches until the 7th week. These form bronchi lined by columnar epithelium.This stage is completed by the 17th week.
– Canalicular stage: 16th to 26th weeks of gestation. The bronchi and bronchioles continue to grow and branch during this period. They form terminal sacs which are primitive alveoli lined by cuboidal and squamous epithelium. This epithelium grows in association to the endothelial cells, which develop into blood vessels by the end of this gestational period. Respiration is possible by the end of the 25th week.
– Saccular or terminal sac stage: 38th to 40th week of gestation. The peripheral airways form saccules which give rise to alveolar ducts and alveolar sacs. The capillary network develops between the terminal sacs.
Postnatal or late alveolar period: After birth to 8 years of age.
– The first mature alveoli appears only after birth from the terminal sacs. Low ridges appear in the walls of saccules and grow into the lumen. This ultimately results in the saccules becoming alveolar sacs. Septation is initiated at sites where elastin fibers are present in the walls of the saccule.
The aging process results in a loss of elasticity and the development of an age related emphysema, uncommonly a cause of symptoms if an isolated disorder of the lungs.
Historical
Early microscopists Malpighi, Marcello (1628-94), Leeuwenhoek, Antoni van (1632-1723), Swammerdam Identified microscopic structures did not recognize cellular composition 1665 Hooke named the cell walled compartments of dead cork tissue 1831 Brown discovered the nucleus. 1838 Schleiden tcell theory’ 1839 Schwann tcell theory’ animals were composed of cells concept of structural and functional units 1863 Virchow body as a ‘cell state,’ with specialized categories of cells 1841 Henle first thorough account of human histology. 1830 compound light microscope 1875 Hertwig O. discovery of fertilization of the egg 1876 astigmation was eliminated from microscopic instrumentation improvement in resolution
Ashley Davidoff MD
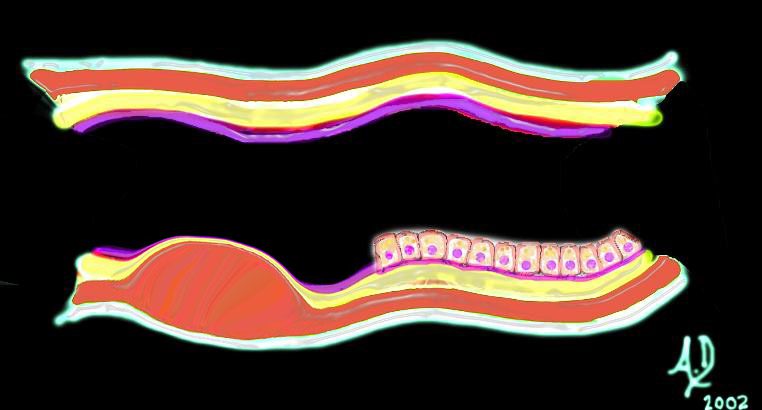
key words art mucosa submucosa muscularis adventitia serosa histology 32347 tube colon small bowel lung bronchus bronchi esophagus stomach large bowel bile duct ureter tube principles
TheCommonVein.net
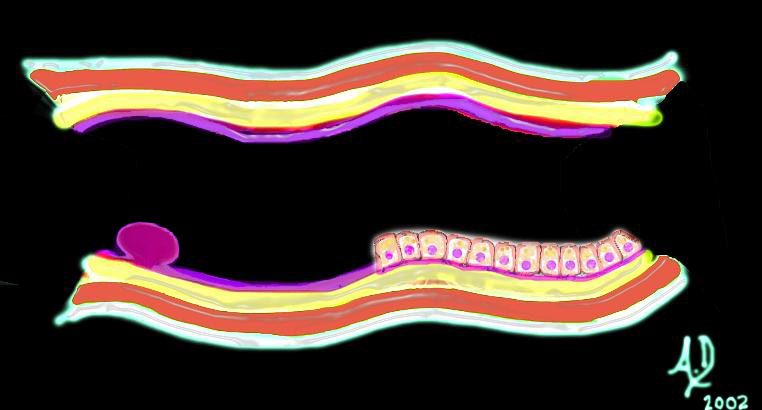
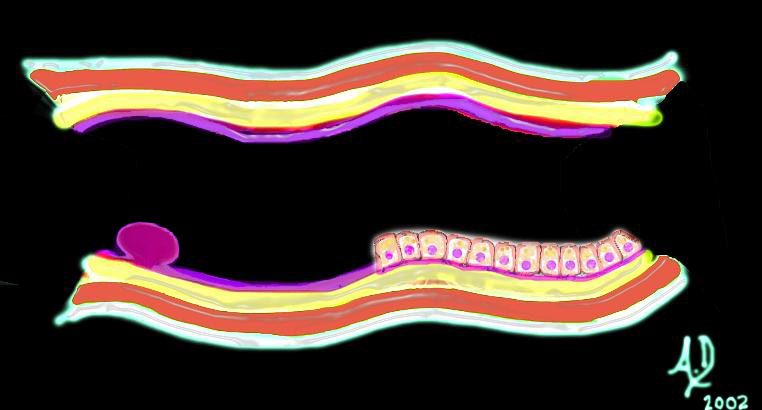
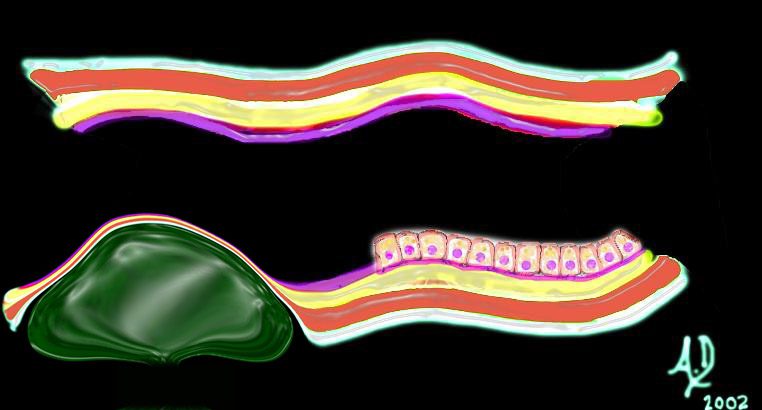
32347d01 key words mucosa submucosa muscularis adventitia serosa mucosal mass polyp neoplasm carcinoma acute angles with the lumen histopathology imaging diagnosis Ashley Davidoff TheCommonVein.net
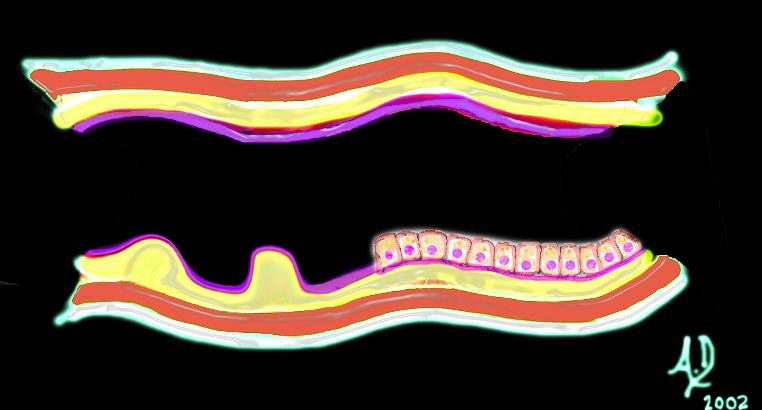
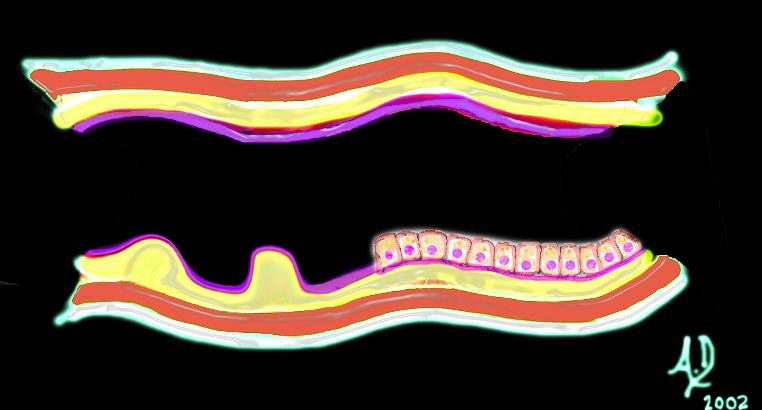
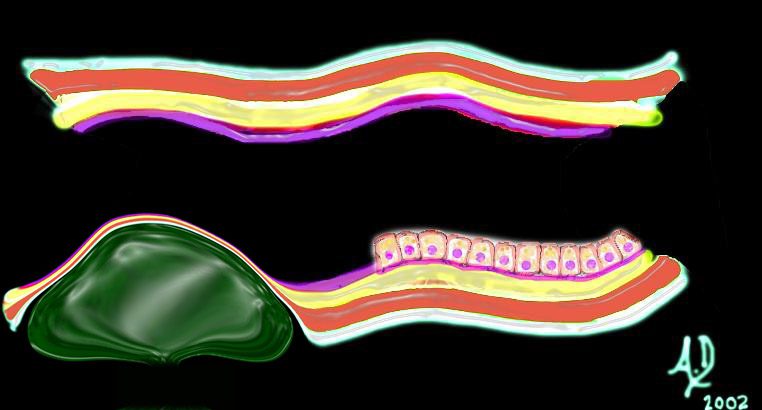
32347d02 key words mucosa submucosa muscularis adventitia serosa submucosal mass edema hemorrhage obtuse angles or right angle 90 degree ninety degree angle with the lumen histopathology imaging diagnosis
Ashley Davidoff TheCommonVein.net
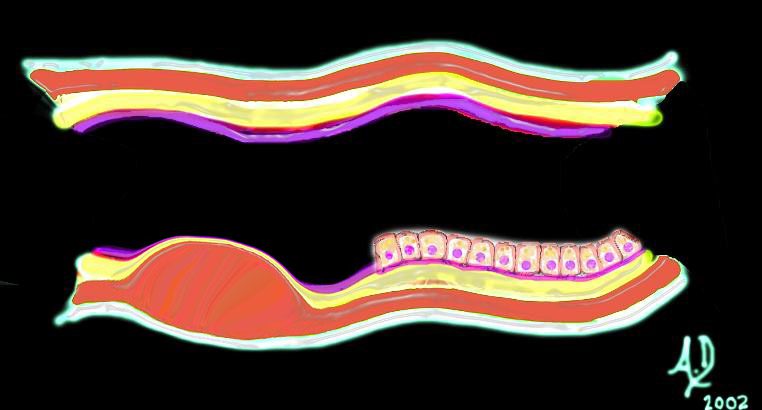
32347d03 key words mucosa submucosa muscularis adventitia serosa submucosal mass edema hemorrhage obtuse angles or right with the lumen histopathology imaging diagnosis Ashley Davidoff TheCommonVein.net
32347d04 key words mucosa submucosa muscularis adventitia serosa submucosal mass edema hemorrhage neoplasm malignancy benign obtuse angles with the lumen histopathology imaging diagnosis
Ashley Davidoff TheCommonVein.net
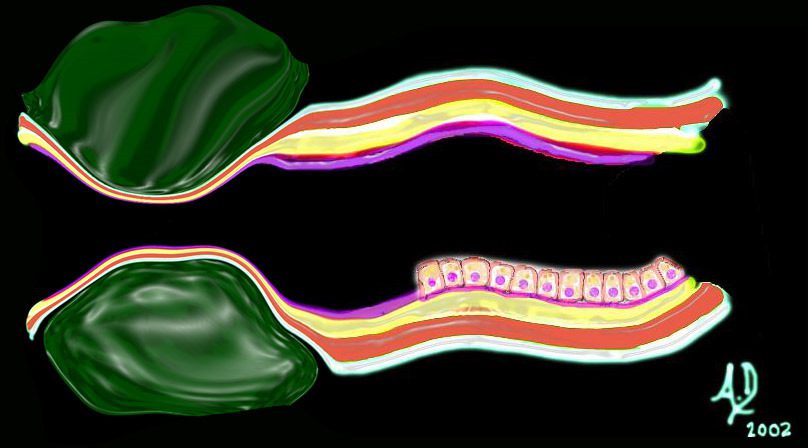
32347d06
key words mucosa submucosa muscularis adventitia serosa submucosal mass edema hemorrhage neoplasm malignancy benign obtuse angles with the lumen circumferential narrowing constriction obstruction histopathology imaging diagnosis Davidoff art Davidoff MD
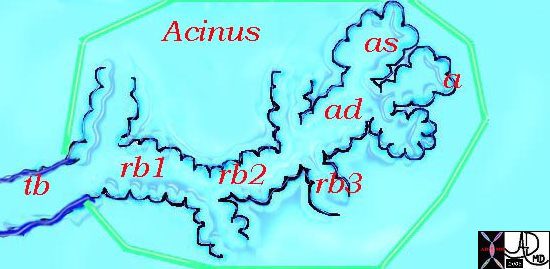
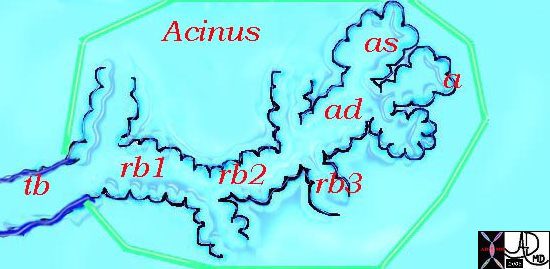
This diagram illustrates the acinus which consists of the respiratory bronchioles (rb 1, 2, 3) the alveolar duct (ad) the alveolar sac (as) and the alveoli. (a)
Courtesy Ashley Davidoff MD 42446b12
Ashley Davidoff
TheCommonVein.net



The acinus with its arborizations is shaped more like a bunch of grapes.
Courtesy of: Ashley Davidoff, M.D 42650
TheCommonVein.net
Links and References
LeMessurier K.S et al Respiratory Barrier as a Safeguard and Regulator of Defense Against Influenza A Virus and Streptococcus pneumoniae Front. Immunol., 04 February 2020
