-
Usual Interstitial Pneumonia (UIP)
- What is it?
- UIP is a chronic fibrosing interstitial lung disease.
- Classified as:
- A subtype of idiopathic interstitial pneumonia (IIP).
- Caused by:
- Idiopathic in most cases (as in Idiopathic Pulmonary Fibrosis, IPF).
- Secondary causes include connective tissue diseases (e.g., rheumatoid arthritis), chronic hypersensitivity pneumonitis, asbestosis, and drug-induced lung injury.
- Resulting in:
- Progressive fibrosis leading to impaired gas exchange and restrictive lung disease.
- Characterized by:
- Temporal and spatial heterogeneity of fibrosis on histology, a characteristic feature of UIP that contrasts with the generally homogeneous fibrosis seen in NSIP.
- Honeycombing and traction bronchiectasis on imaging.
- Predominantly subpleural and basal distribution of fibrosis.
- Anatomically affecting:
- Alveolar ducts, alveoli, interlobular septa, and adjacent pleura.
- Pathophysiology:
- Chronic injury to the alveolar epithelium triggers an aberrant repair process.
- Fibroblast proliferation and extracellular matrix deposition lead to irreversible fibrosis.
- Diagnosis:
- Clinical:
- Progressive dyspnea and chronic dry cough.
- Digital clubbing in advanced stages.
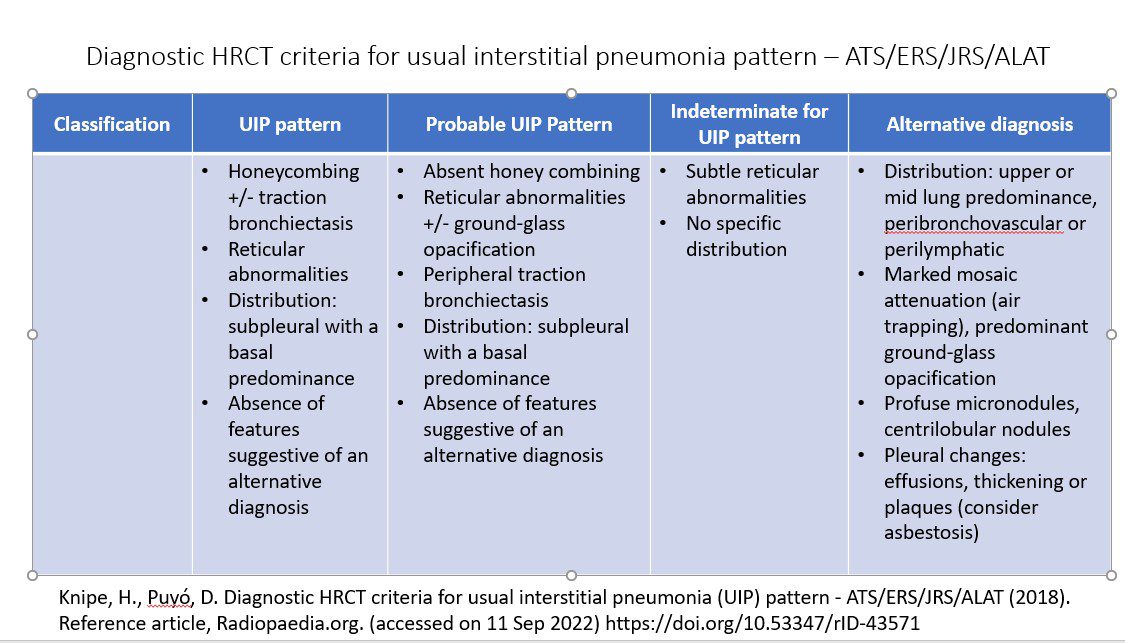
- Imaging:
- Radiologic Principles:
- Presence of fibrosis with temporal and spatial heterogeneity.
- Applied Anatomy:
- Parts: Alveolar ducts, alveoli, interlobular septa, pleura.
- Size: Fibrotic areas vary; typically affect multiple secondary pulmonary lobules.
- Shape: Reticular, honeycombing, or traction bronchiectasis patterns.
- Position: Predominantly basal and subpleural distribution.
- Character: Fibrosis with honeycombing and traction bronchiectasis; absence of ground-glass opacities unless complicating.
- Time: Chronic progression over months to years.
- CXR:
- Reticular opacities with basal and peripheral predominance.
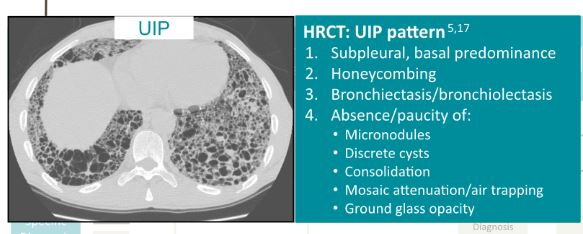
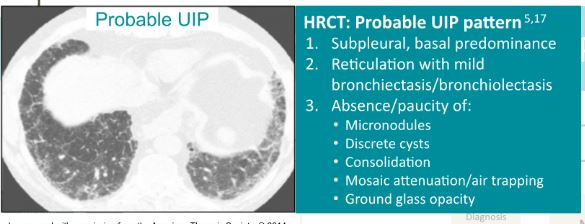
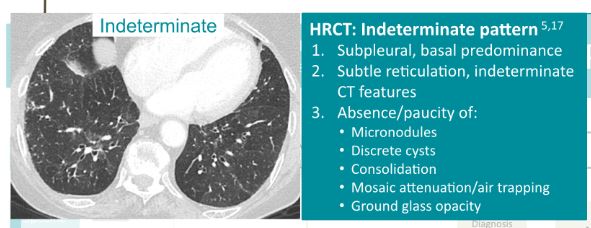
- CT:
- Key Findings:
- Honeycombing (clustered cystic airspaces).
- Reticular opacities and traction bronchiectasis.
- Predominantly subpleural and basal distribution.
- Temporal heterogeneity without significant ground-glass opacity.
- Key Findings:
- PET-CT:
- Limited utility but may show mild metabolic activity in fibrotic regions.
- Other relevant modalities:
- MRI rarely used but may demonstrate fibrosis on T2-weighted images.
- Radiologic Principles:
- Laboratory findings:
- PFTs: Restrictive pattern with reduced total lung capacity (TLC) and diffusion capacity (DLCO).
- Bloods: ANA, RF, or other markers if secondary causes are suspected.
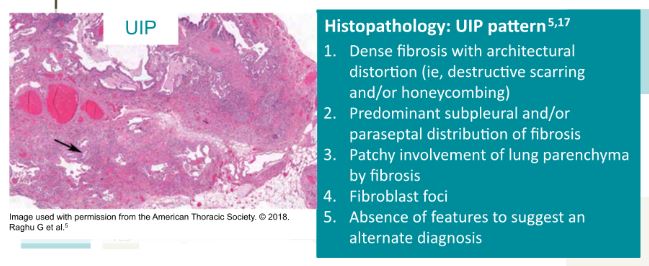
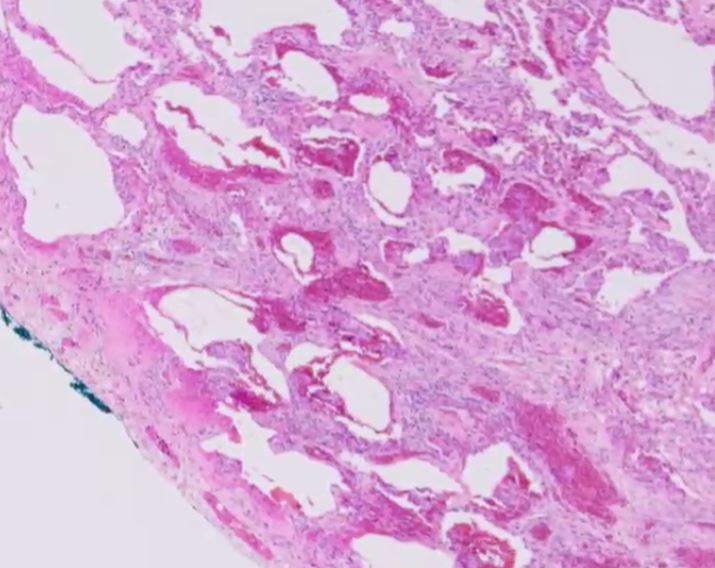
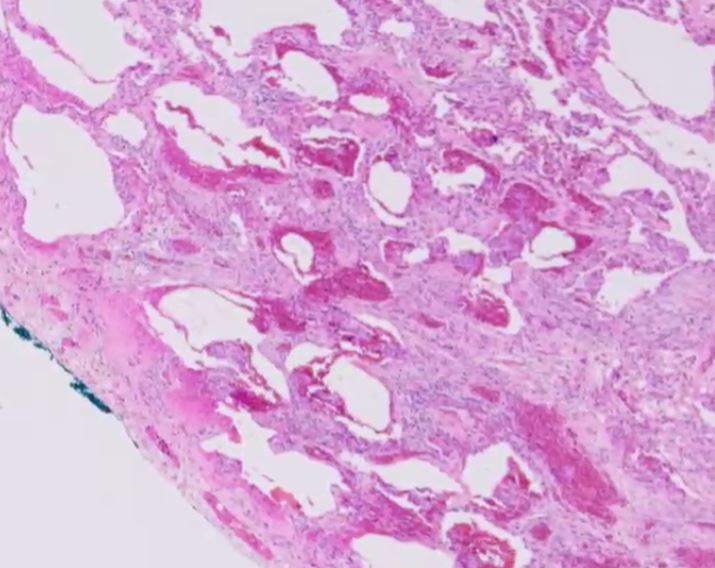
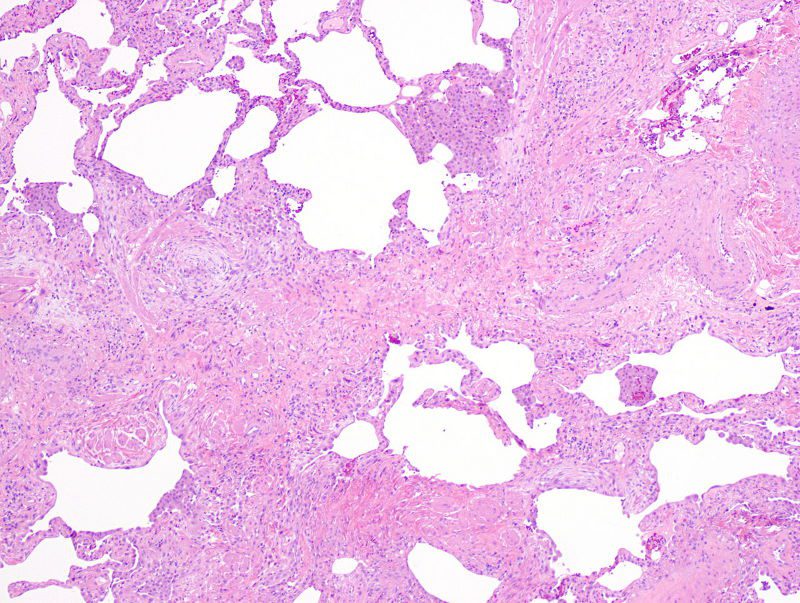
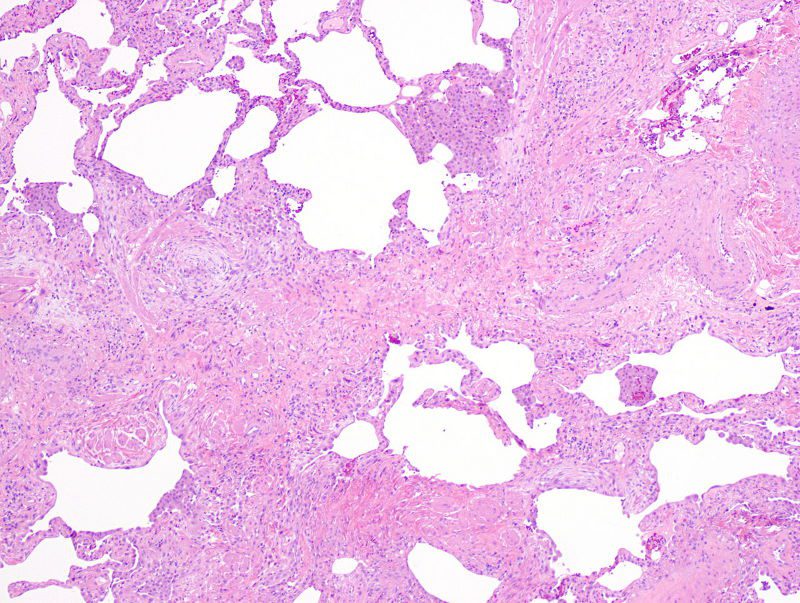
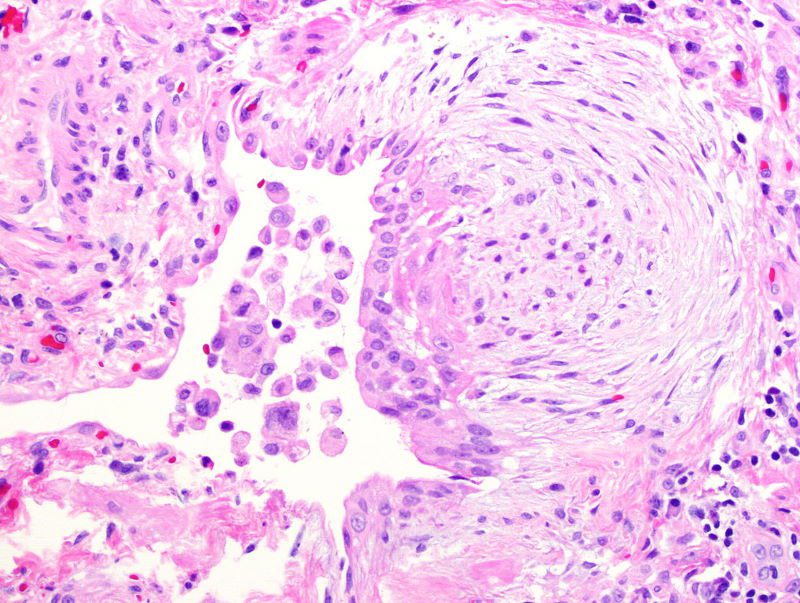
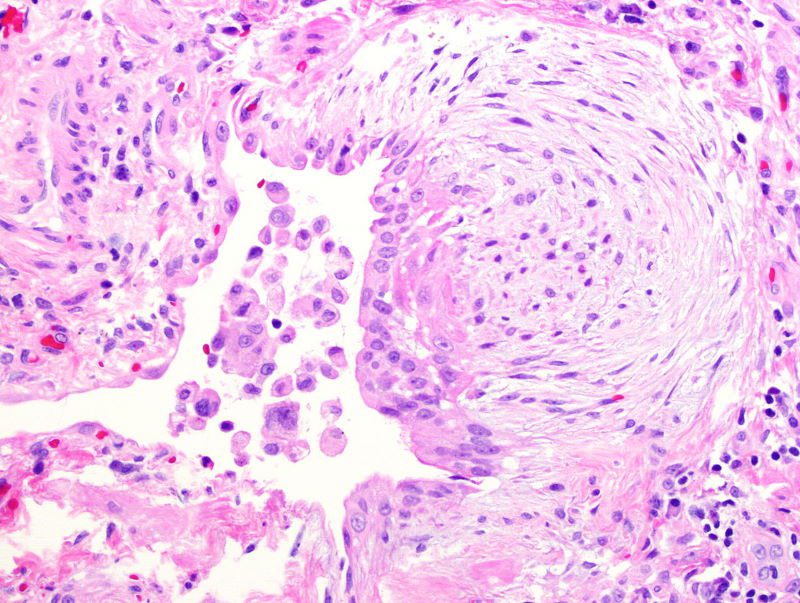
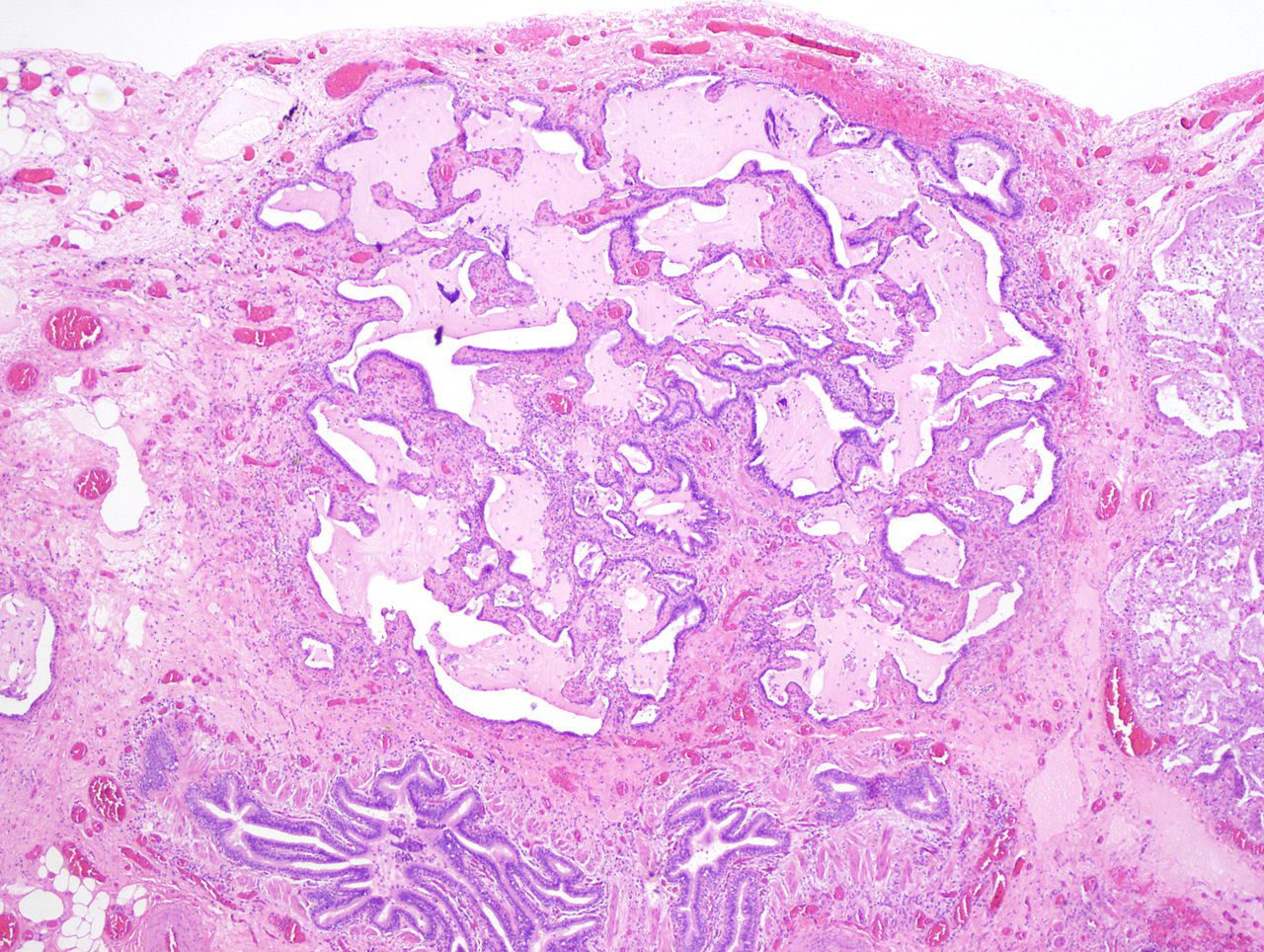
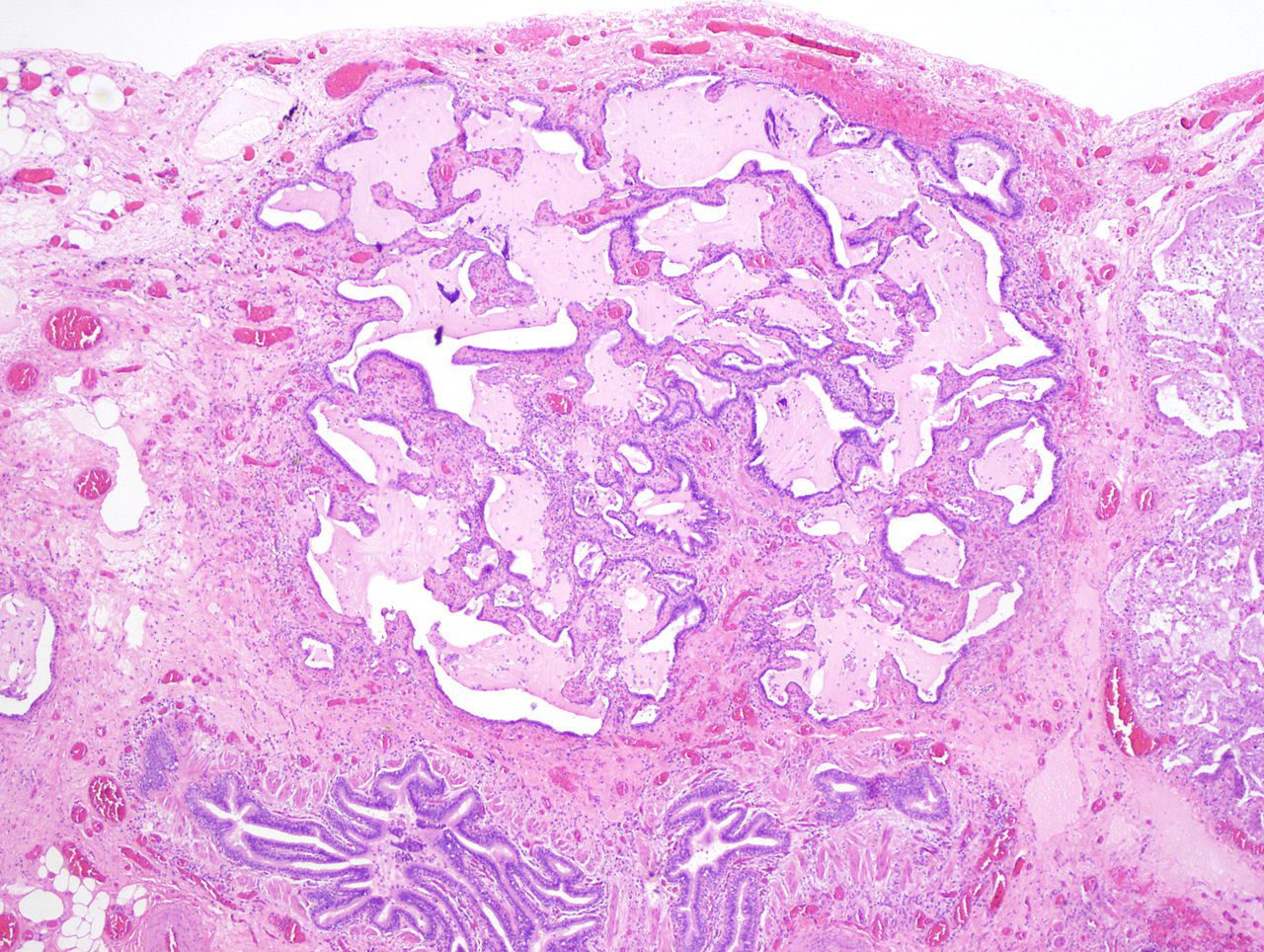
- Pathology: Temporal and spatial heterogeneity with fibroblastic foci, honeycombing (defined as large cystic airspaces surrounded by dense fibrosis, lined by hyperplastic or bronchiolar-type epithelium, often with mucus debris within the spaces), and areas of dense fibrosis.
- Clinical:
- Treatment:
- Antifibrotic agents (e.g., pirfenidone, nintedanib) for IPF.
- Supplemental oxygen and pulmonary rehabilitation.
- Lung transplantation in selected cases.
- Prognosis:
- Poor prognosis with a median survival of 3-5 years for IPF.
- Disease progression may be slowed with antifibrotic treatment.
- Radiological Implications:
- High-resolution CT (HRCT) is critical for diagnosis and monitoring progression.
- Differentiation from other ILDs is key based on imaging patterns.
- Key Points and Pearls:
- Idiopathic Pulmonary Fibrosis (IPF) is a specific clinical diagnosis characterized by progressive pulmonary fibrosis of unknown cause. Usual Interstitial Pneumonia (UIP) is the histological and radiological pattern that defines IPF when no underlying cause is identified. However, UIP can also occur secondary to other conditions, such as connective tissue diseases or chronic hypersensitivity pneumonitis, making it essential to differentiate idiopathic from secondary causes during diagnosis.
- Diagnosis often requires a multidisciplinary approach (radiology, pathology, and pulmonology).
- Honeycombing is a definitive imaging finding but must be distinguished from other cystic lung diseases.
- Absence of ground-glass opacities helps differentiate UIP from NSIP or other ILDs. Additionally, spatial heterogeneity in UIP, while homogeneity is characteristic of NSIP, serves as a distinguishing feature between the two entities.
- What is it?
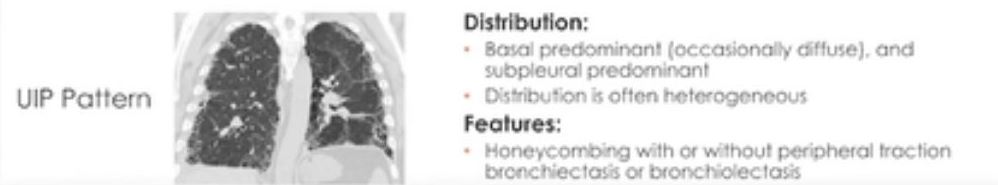
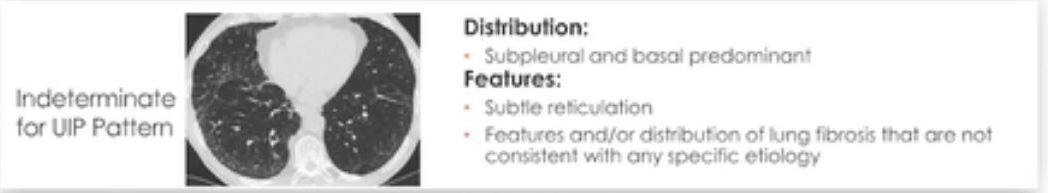
- UIP pattern:

Basilar and peripheral distribution
Ashley Davidoff MD TheCommonvein.net lungs-0769b
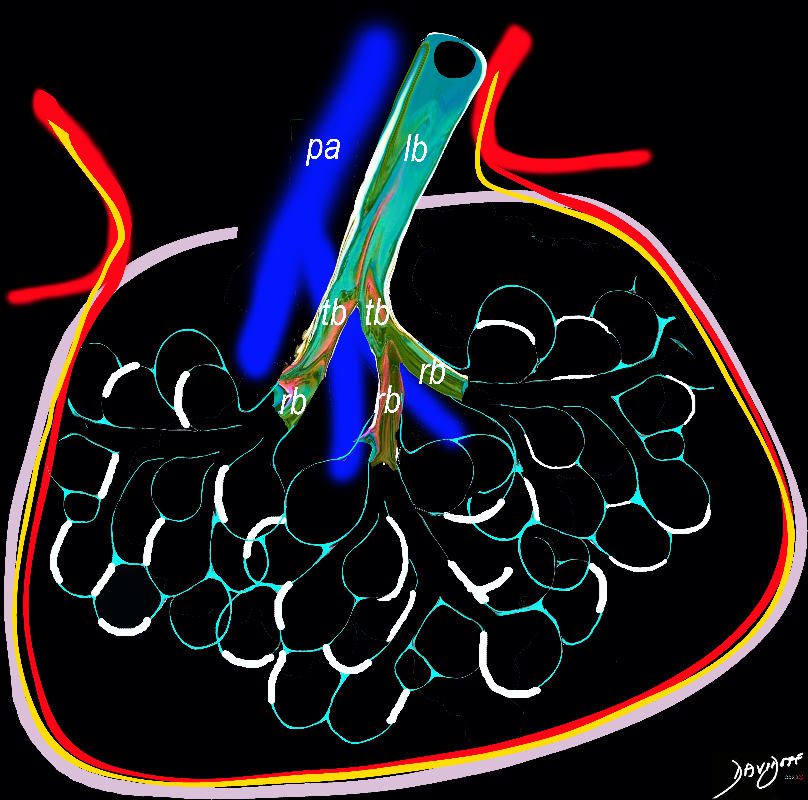
Ashley Davidoff TheCommonVein.net
lungs-0738b
- Starts peripheral
-
- subpleural
- basal
- reticular
- traction bronchiectasis
- honeycombing 70-80%
- +/- bronchiectasis/bronchiolectasis
- Structures Involved
-
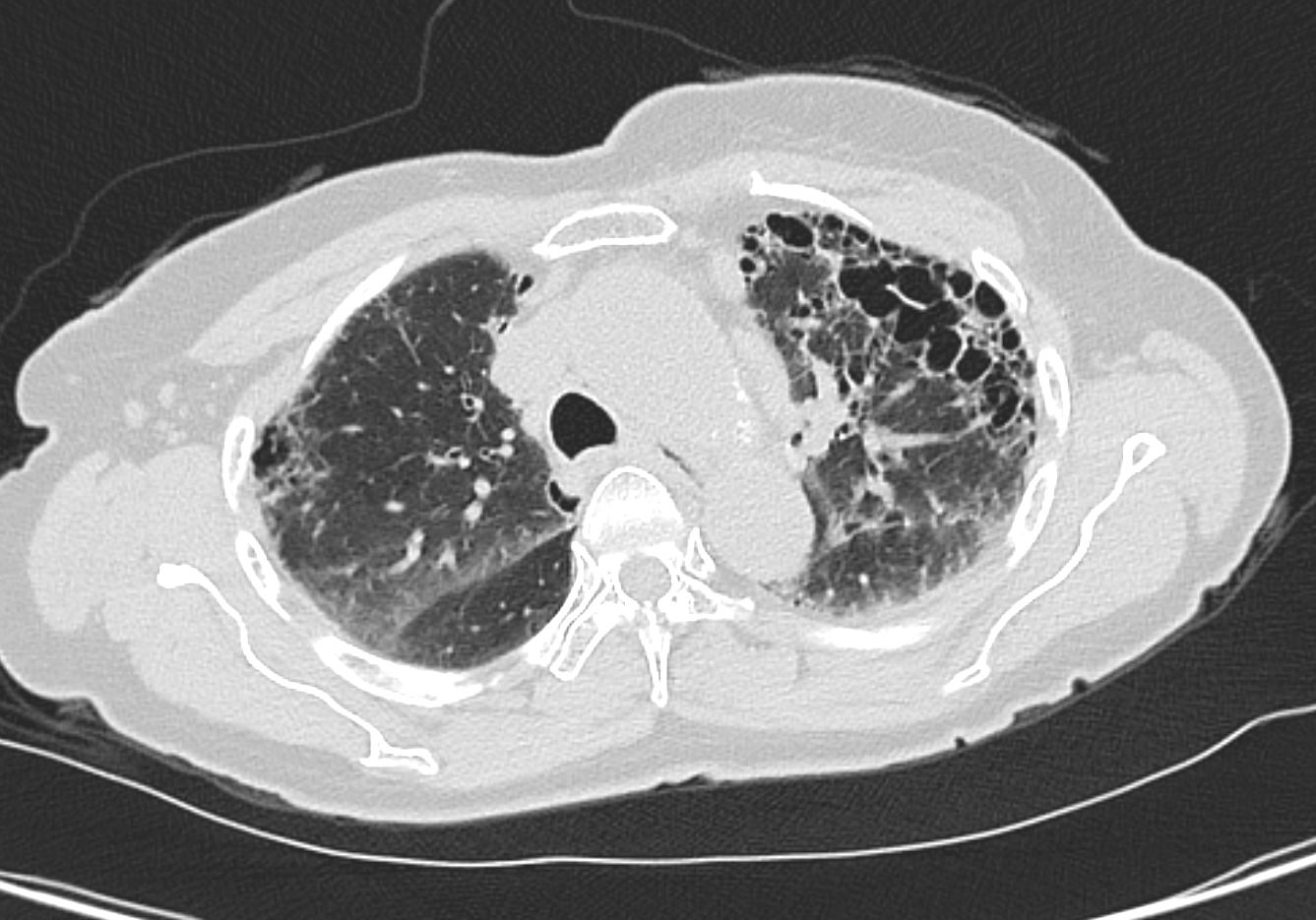
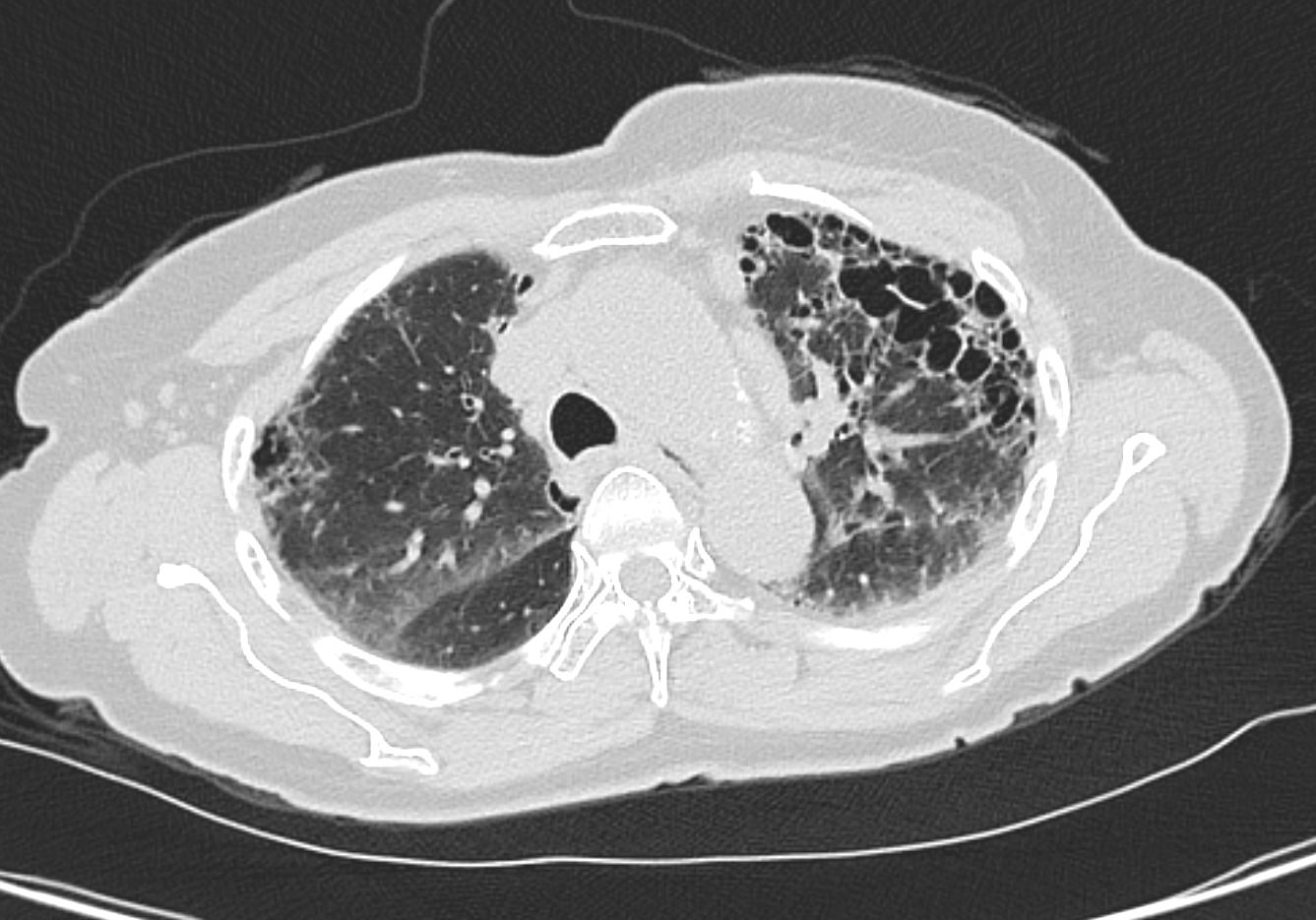
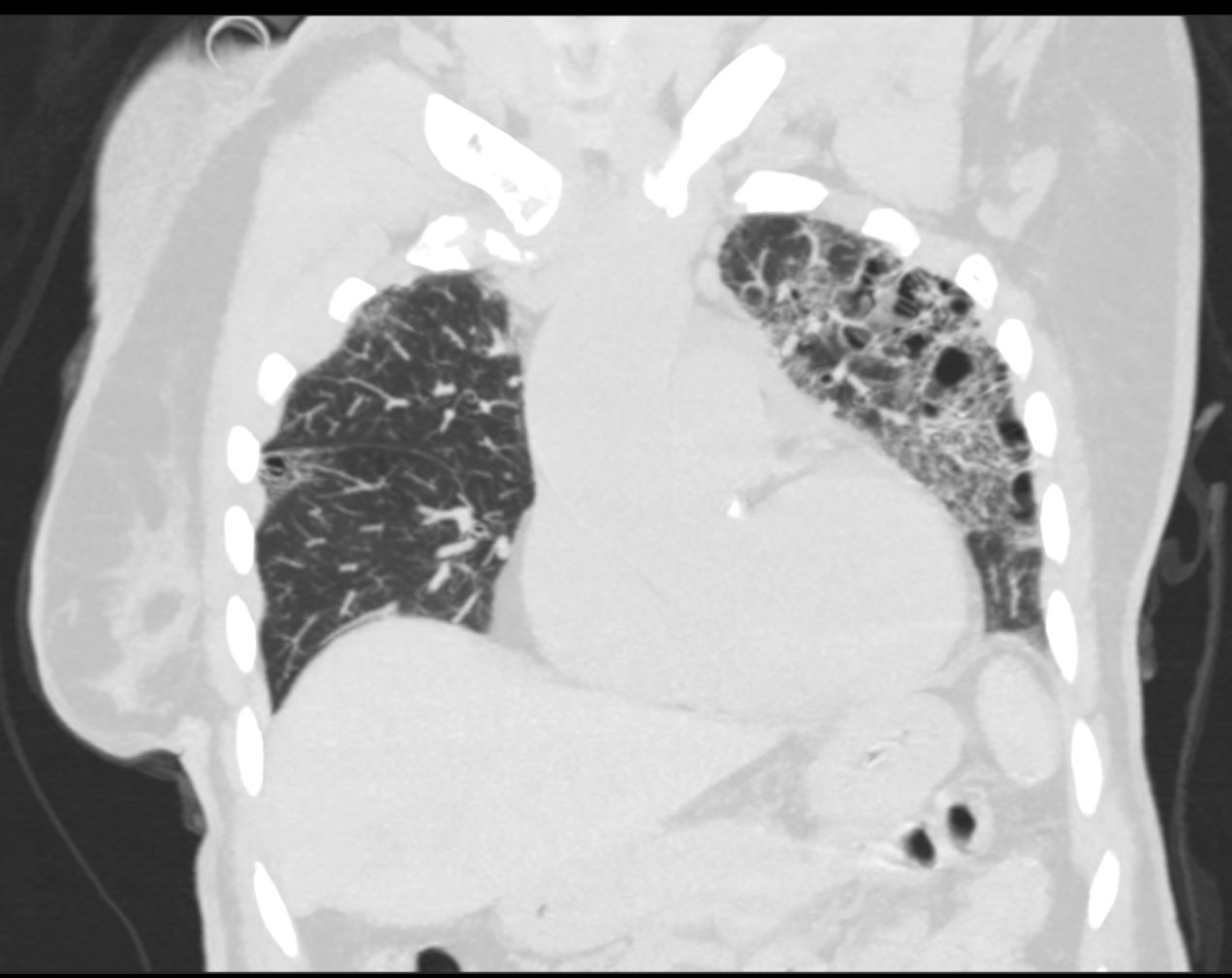
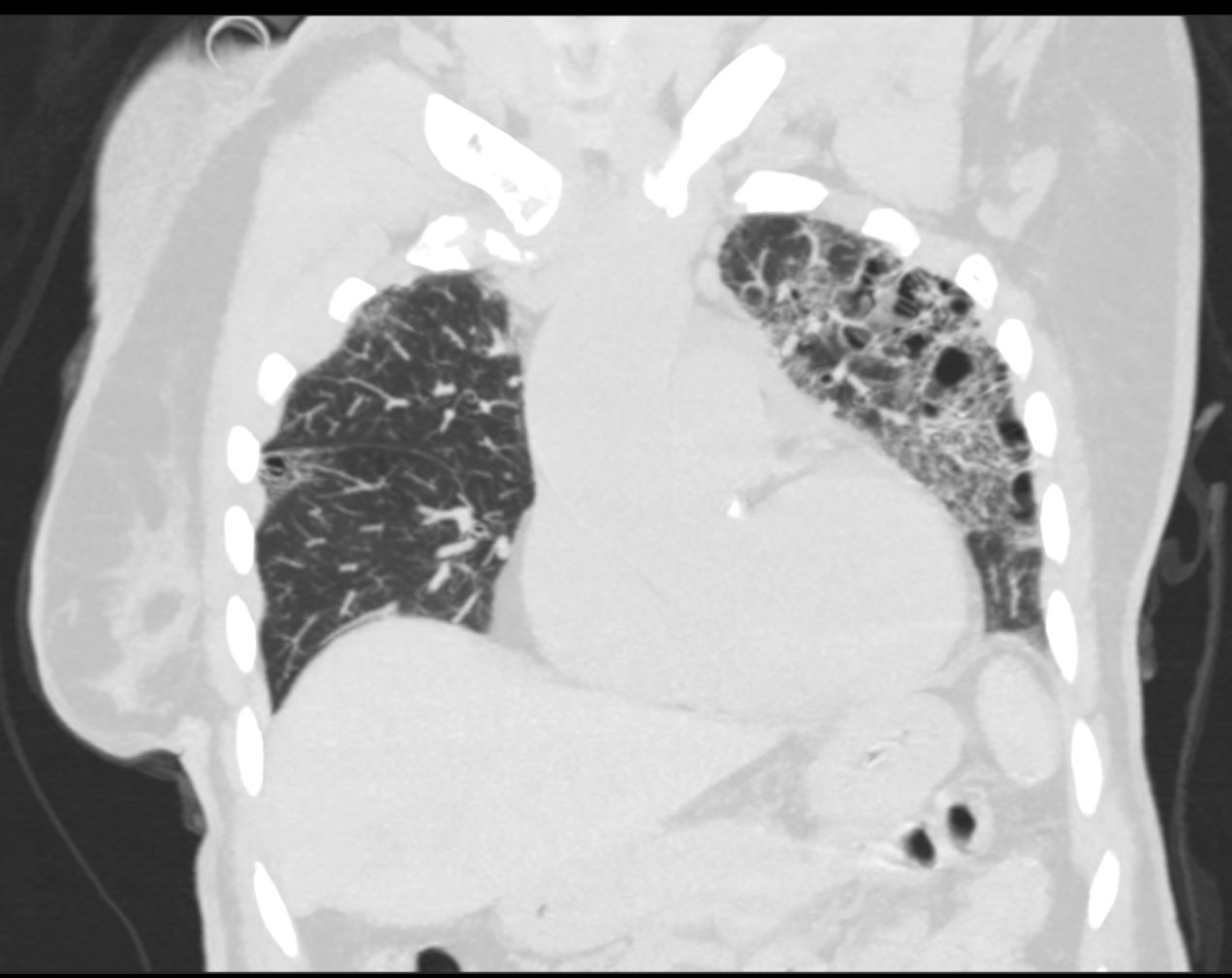
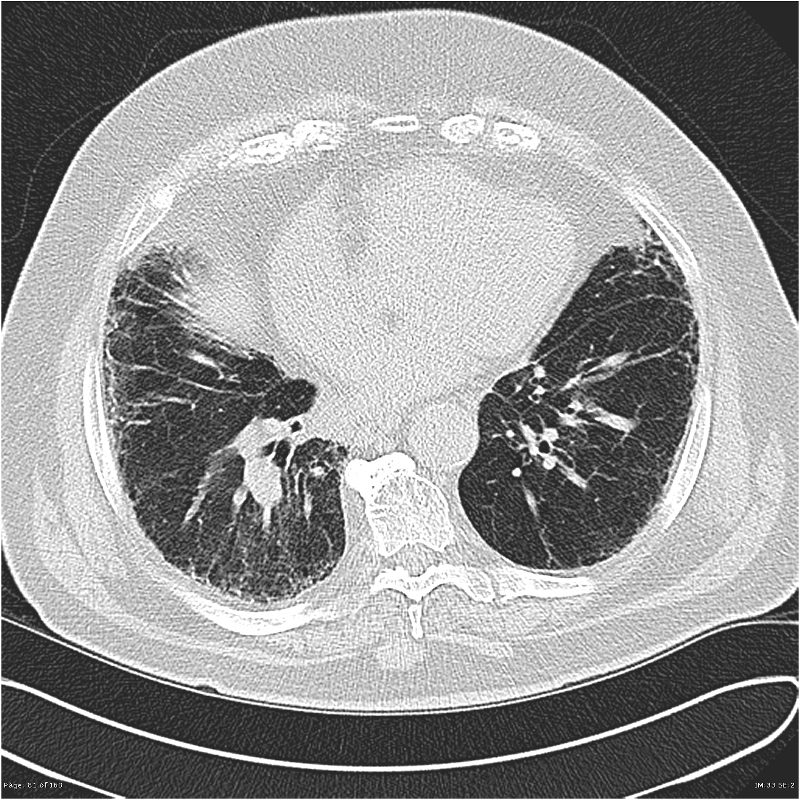
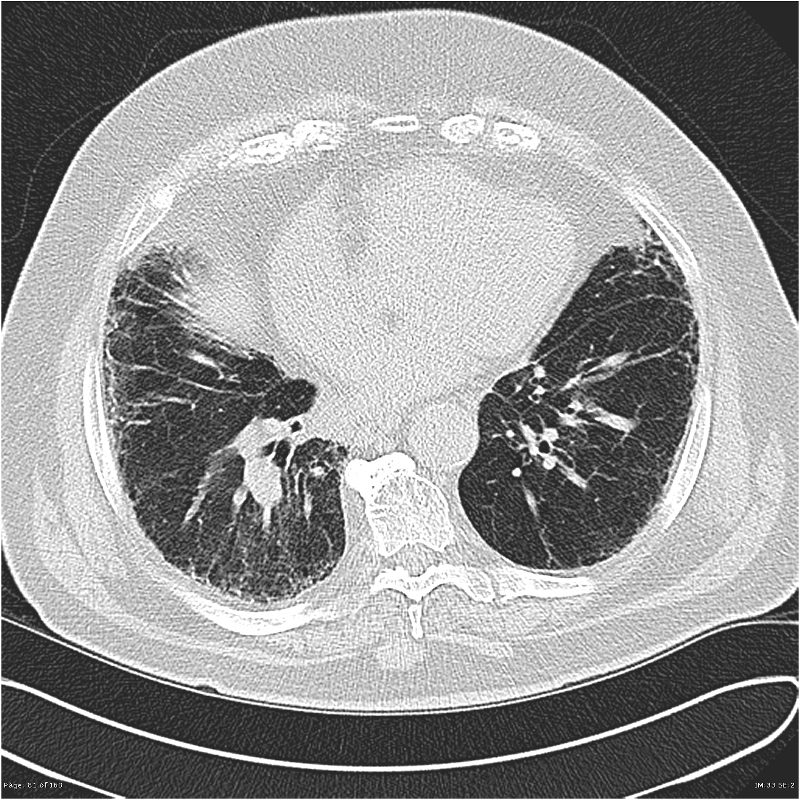
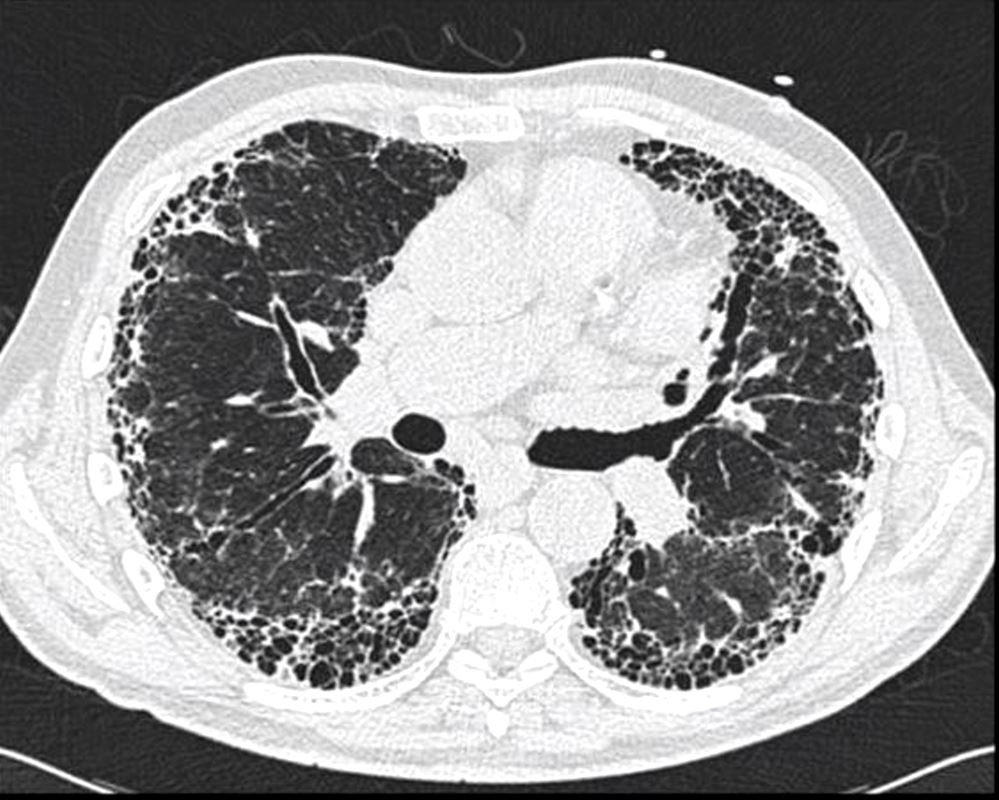
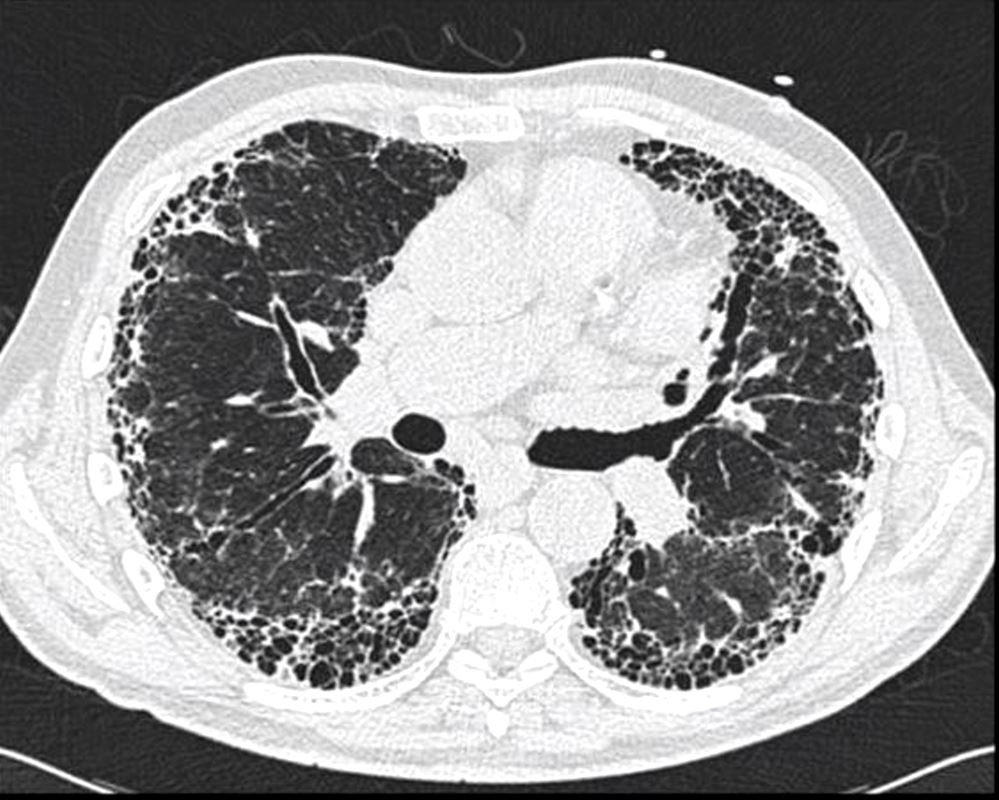
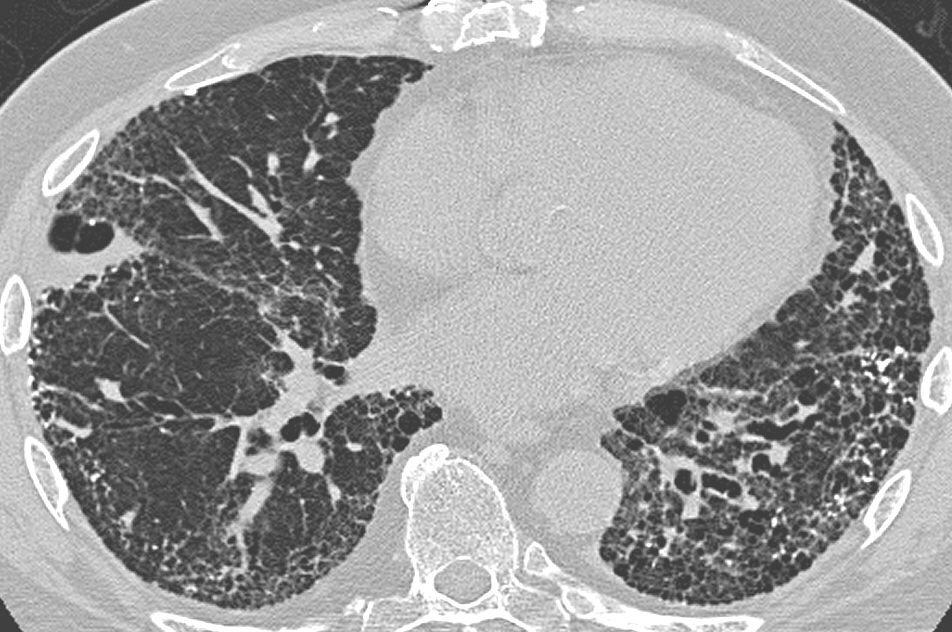
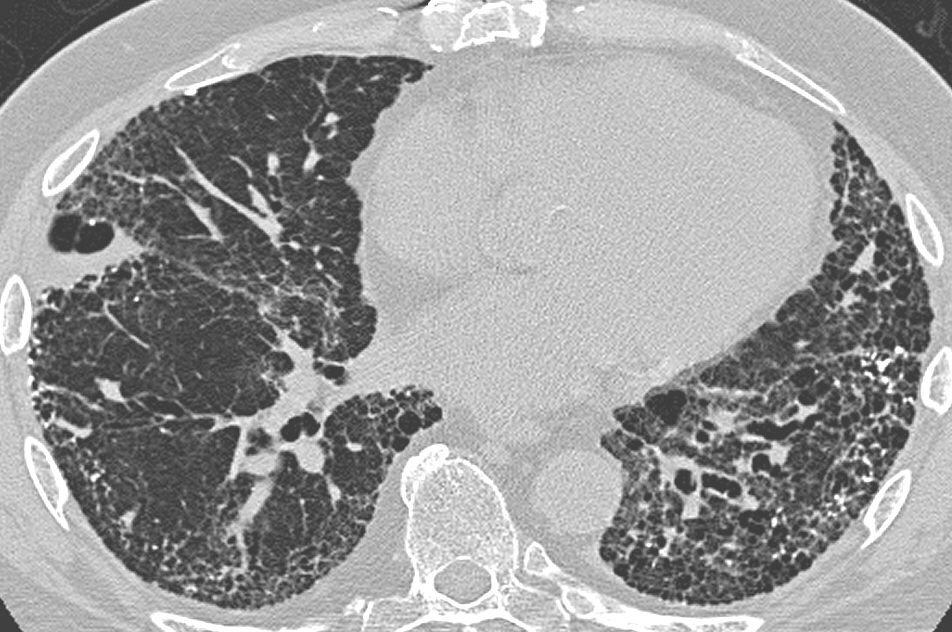
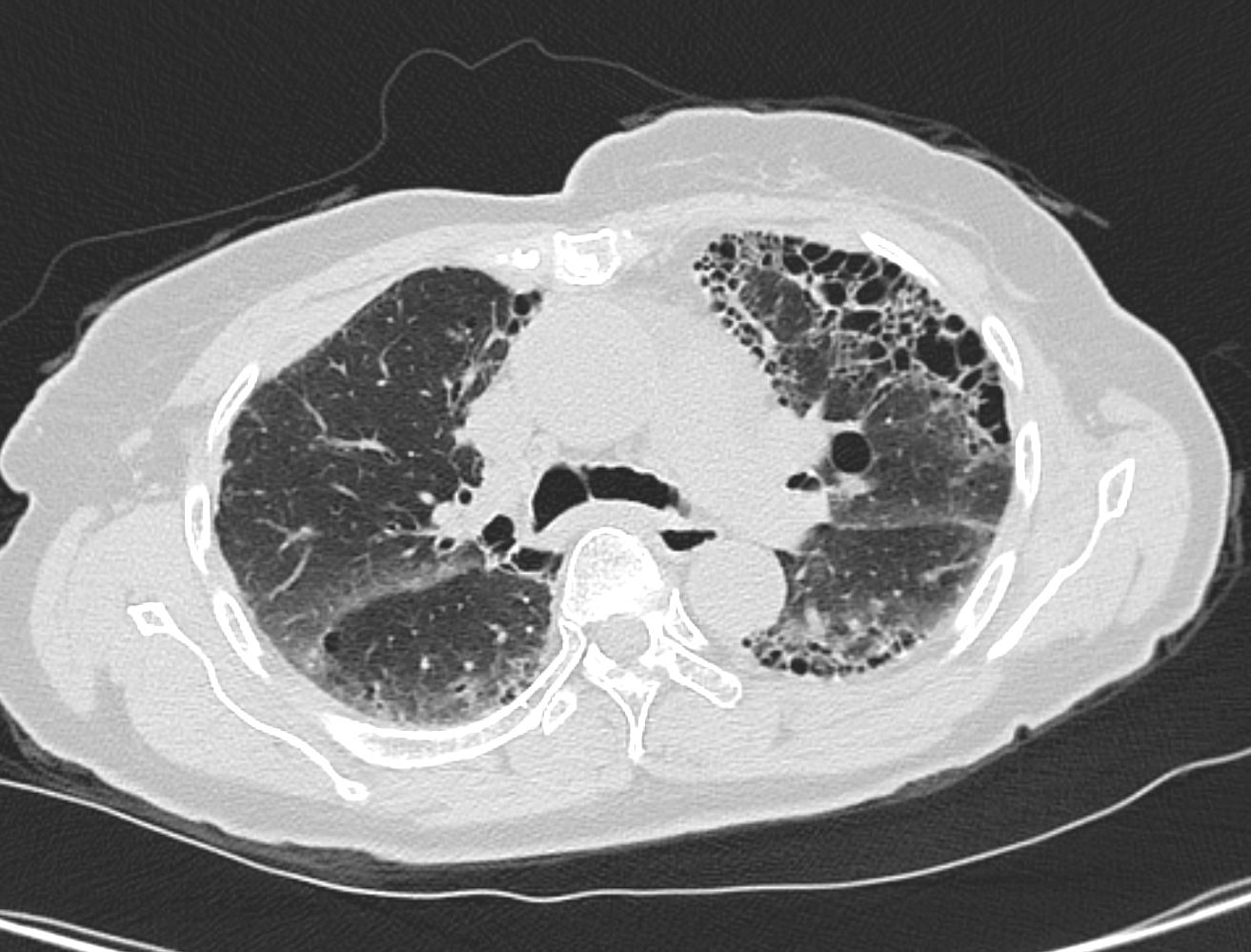
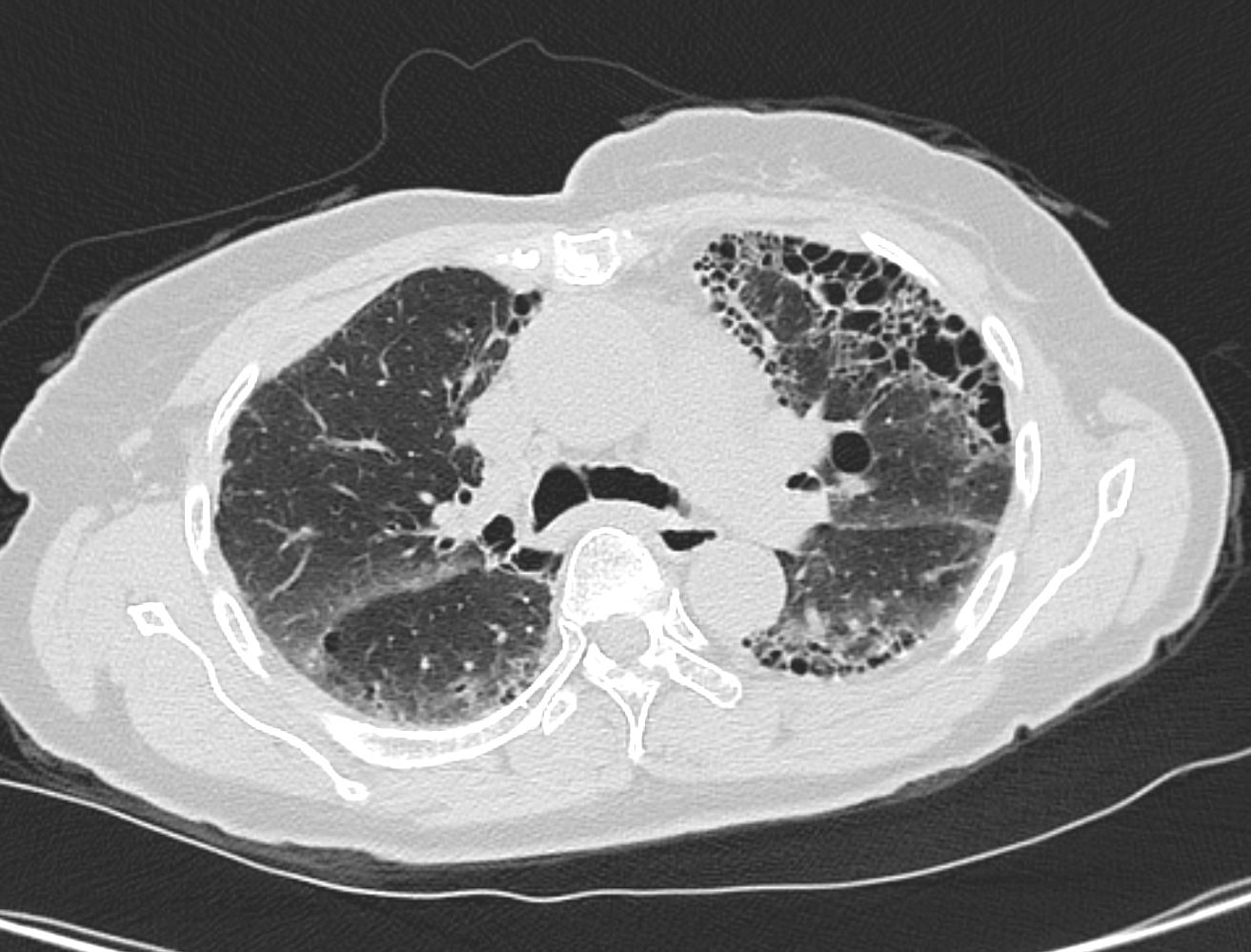
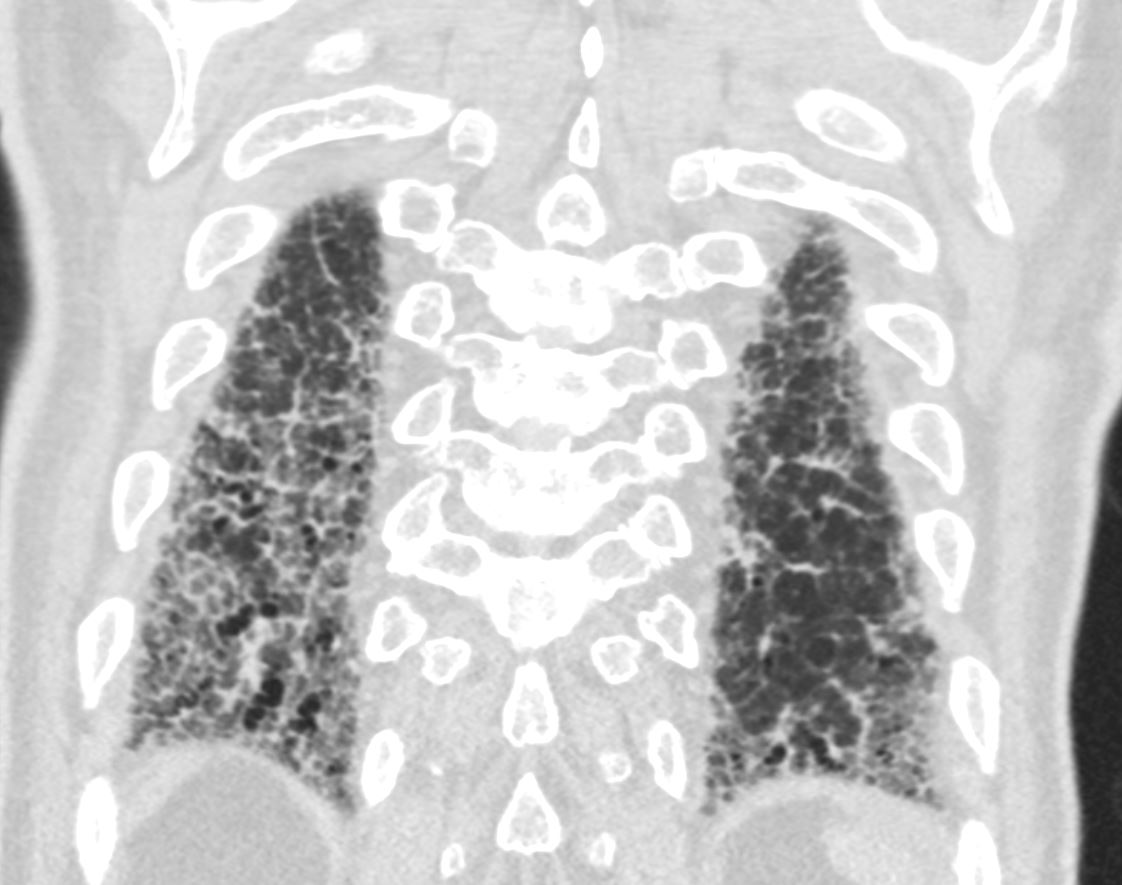
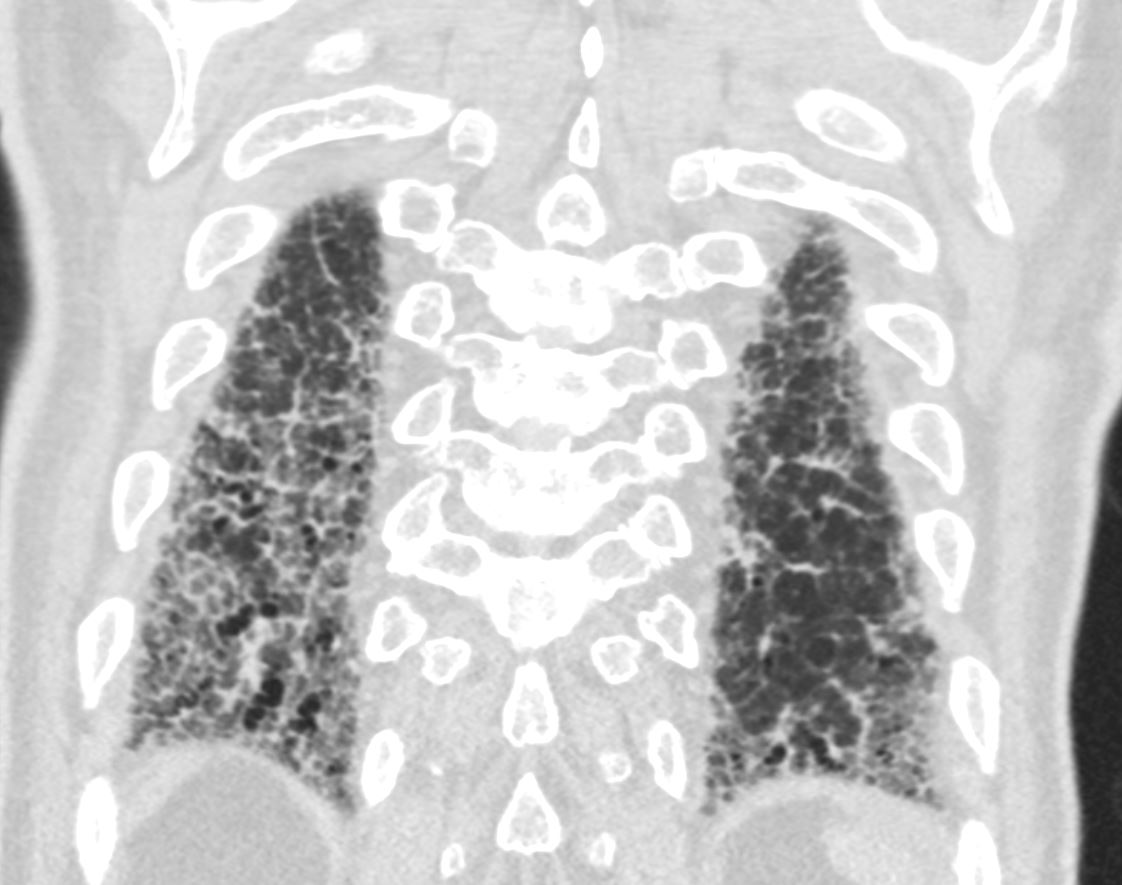
70 year old male with UIP showing extensive dominantly bibasilar and peripheral reticulation
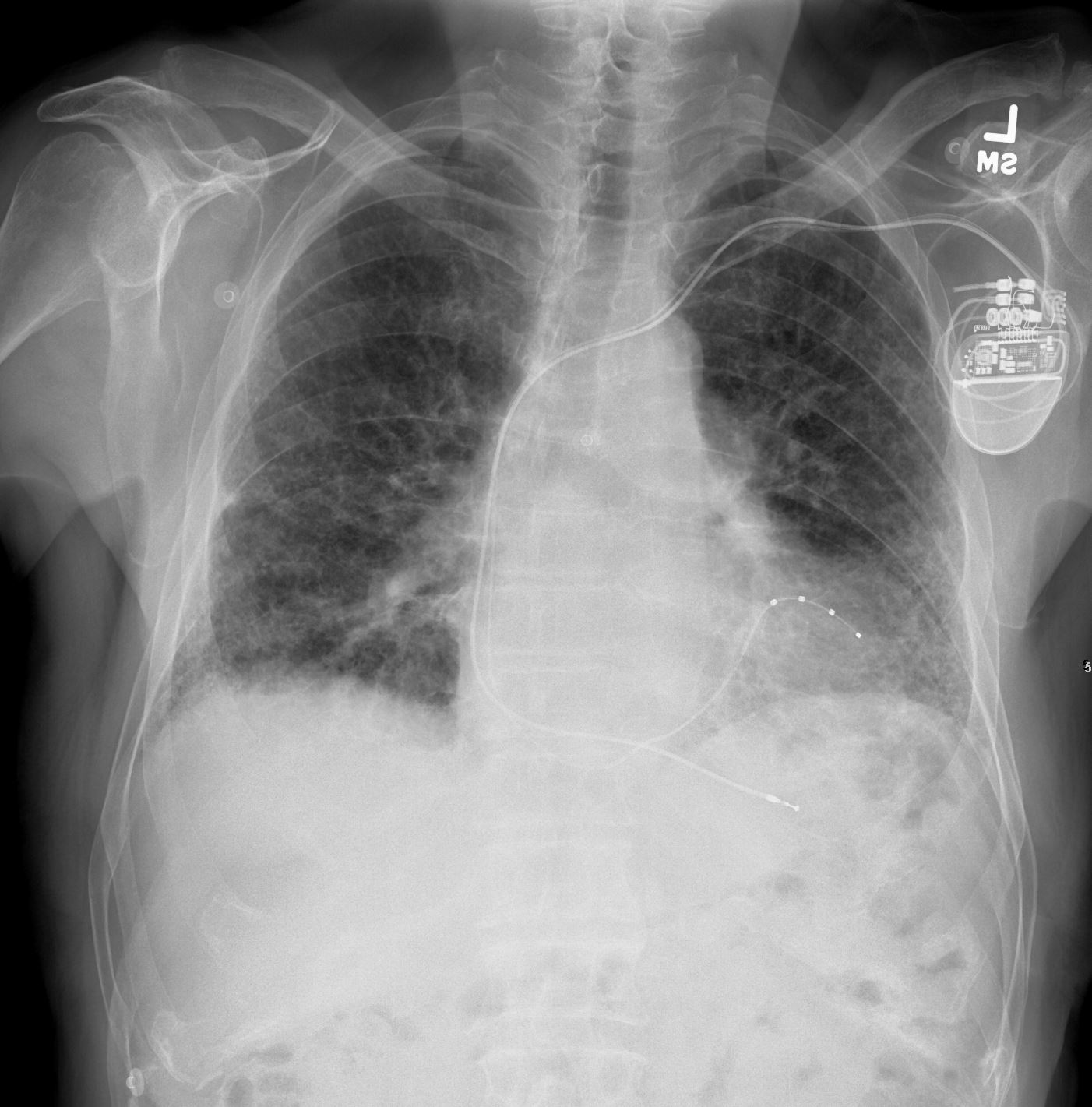
70 year old male with UIP showing extensive dominantly bibasilar and peripheral reticulation
Ashley Davidoff MD TheCommonVein.net
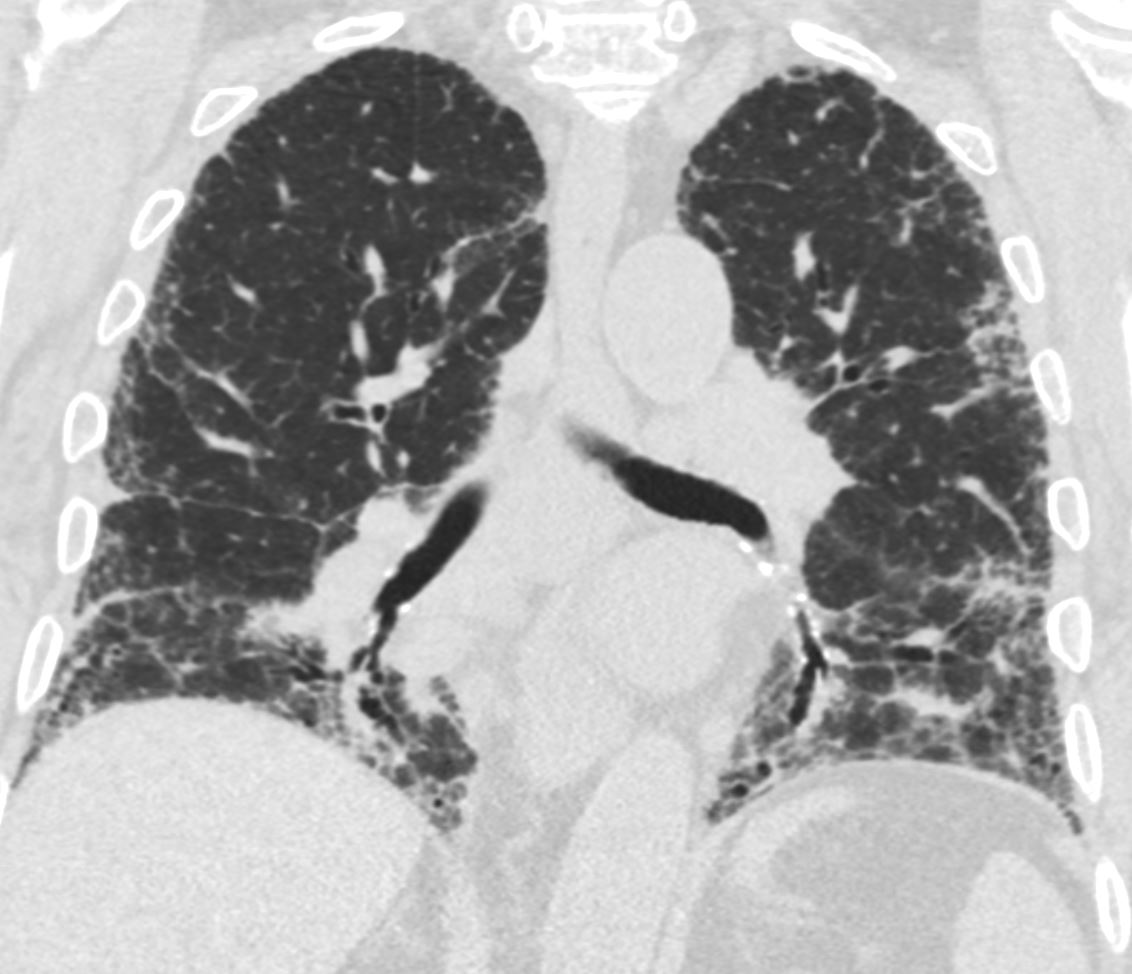
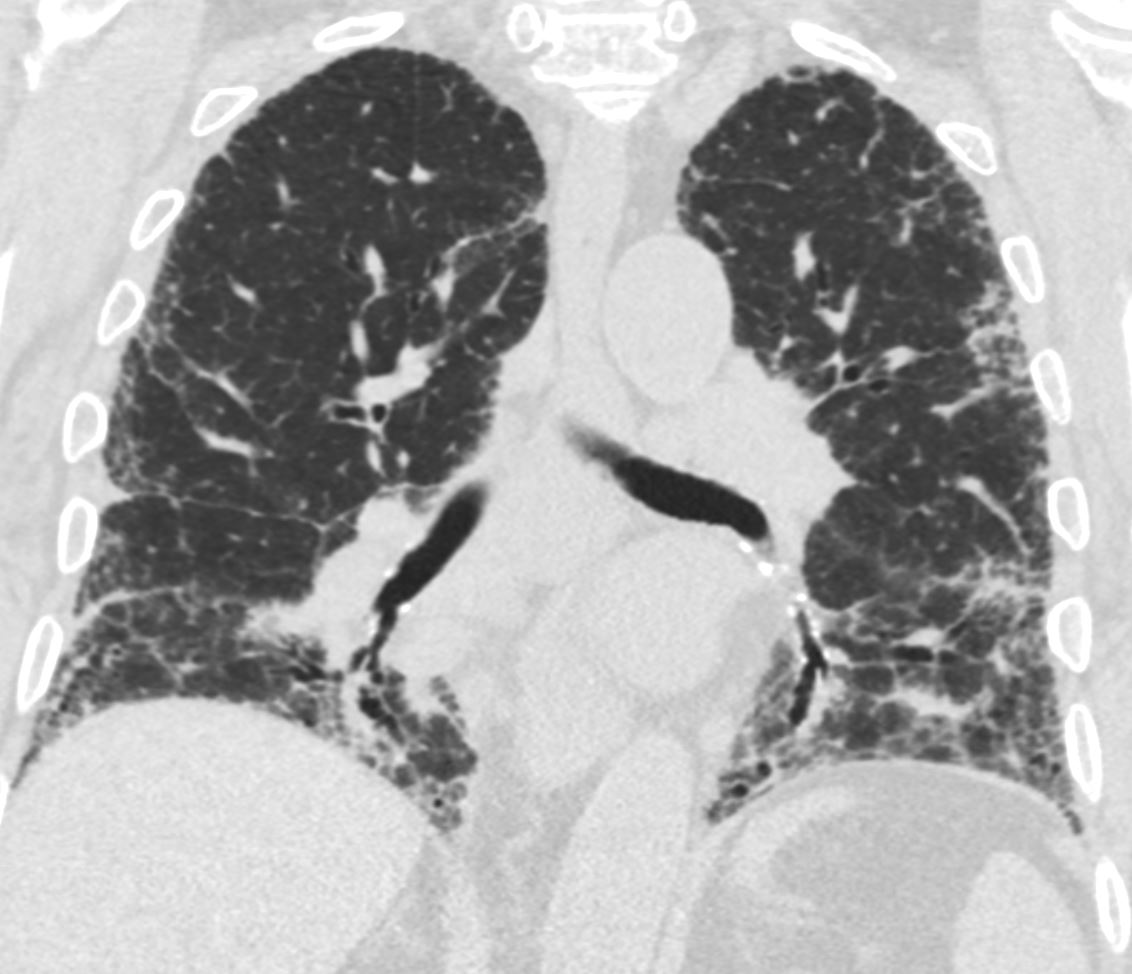
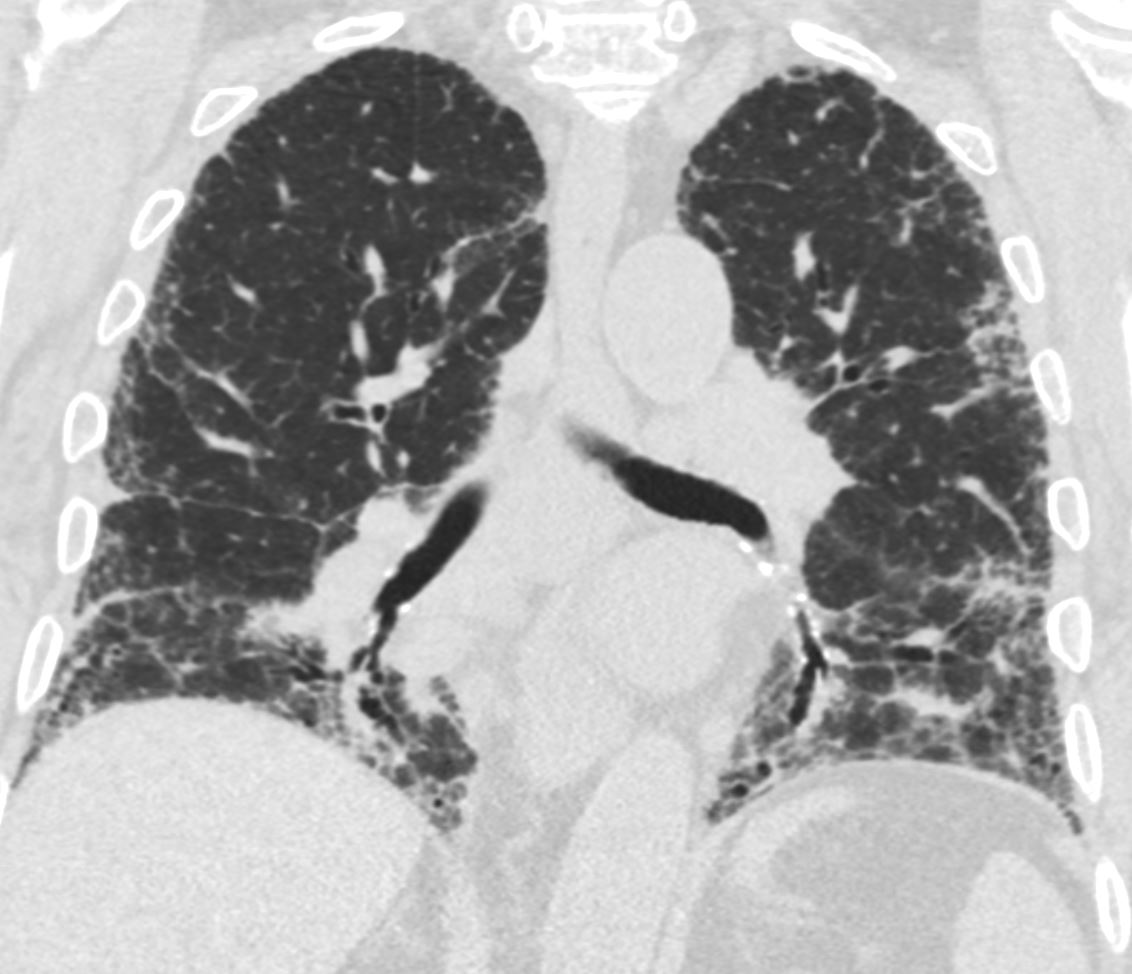
70 year old male with UIP showing extensive dominantly bibasilar and peripheral reticulation
Ashley Davidoff MD TheCommonVein.net uip-002
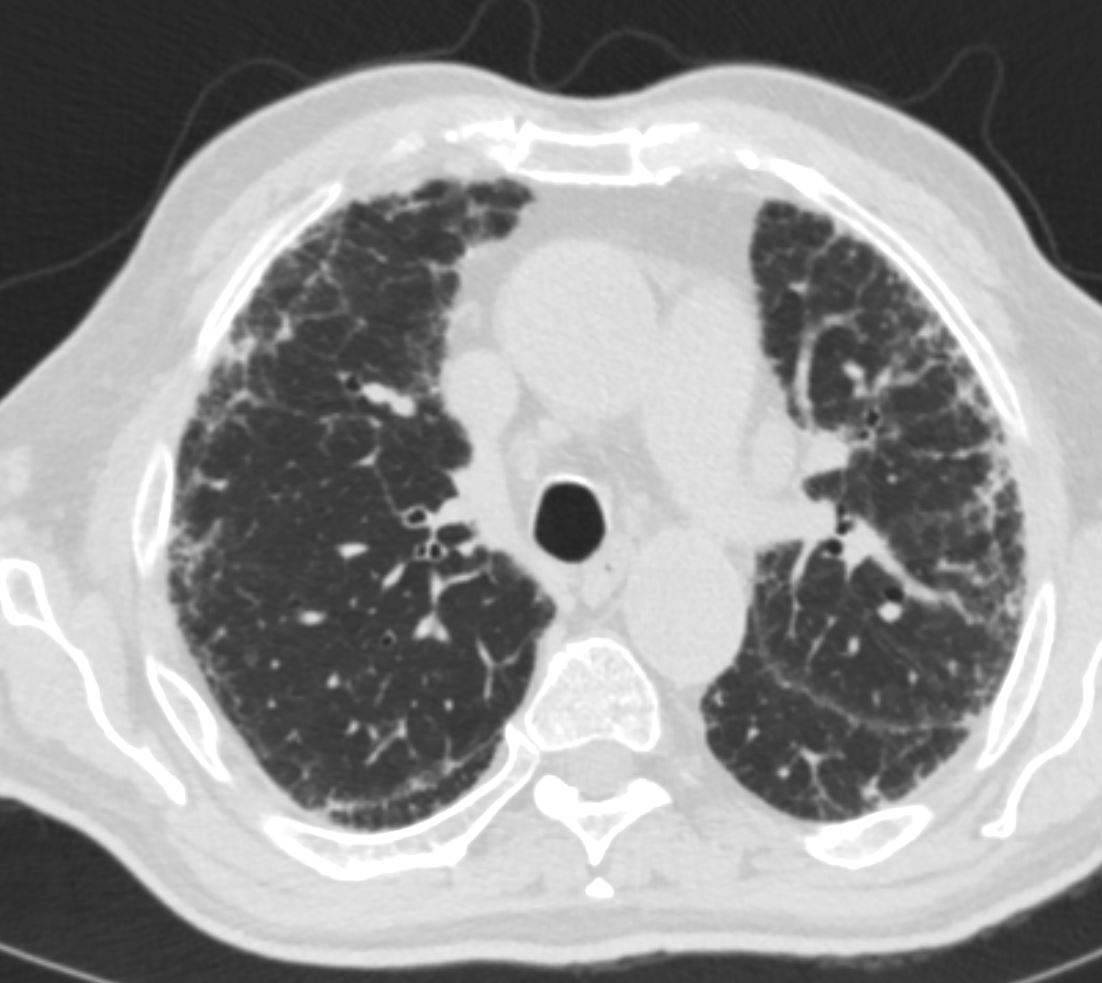
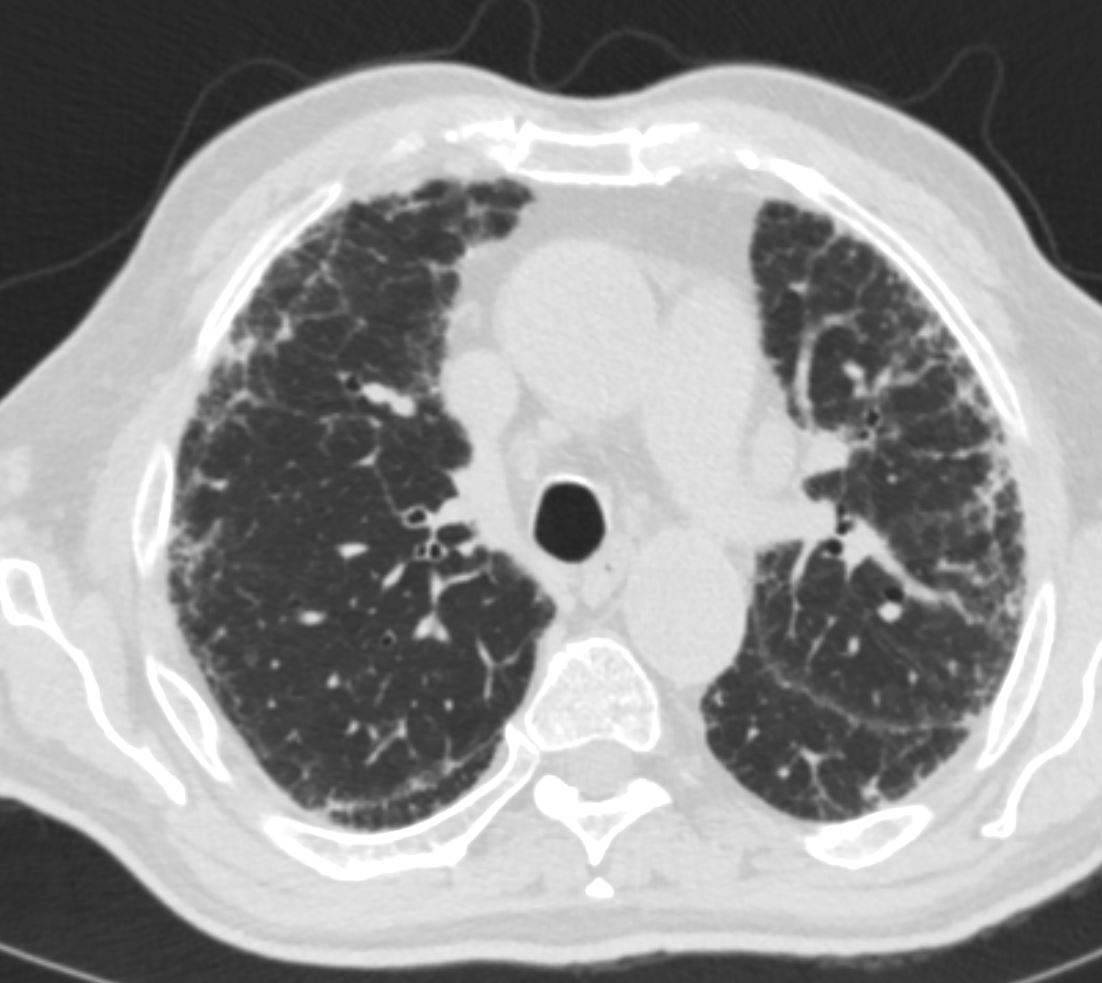
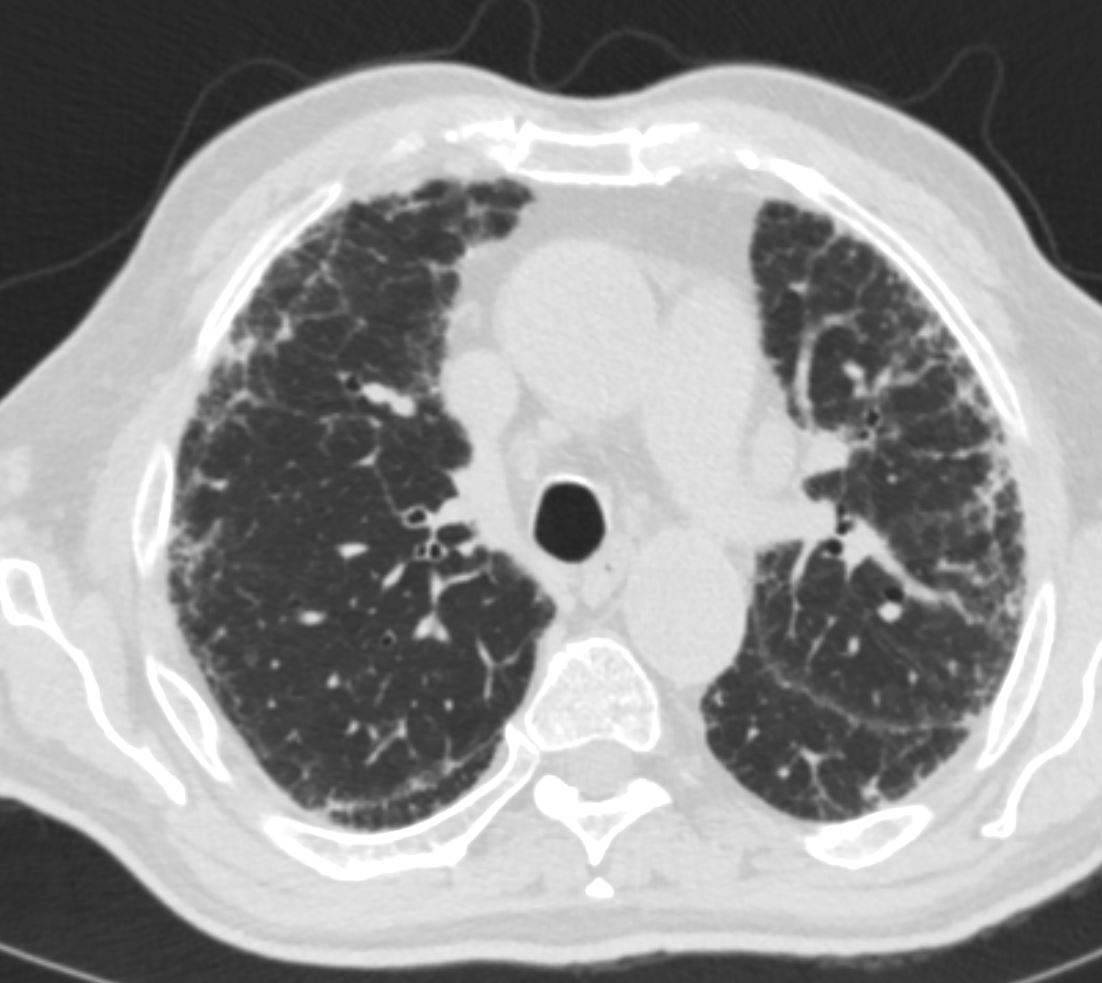
70 year old male with UIP showing extensive dominantly bibasilar and peripheral reticulation
Ashley Davidoff MD TheCommonVein.net uip-005



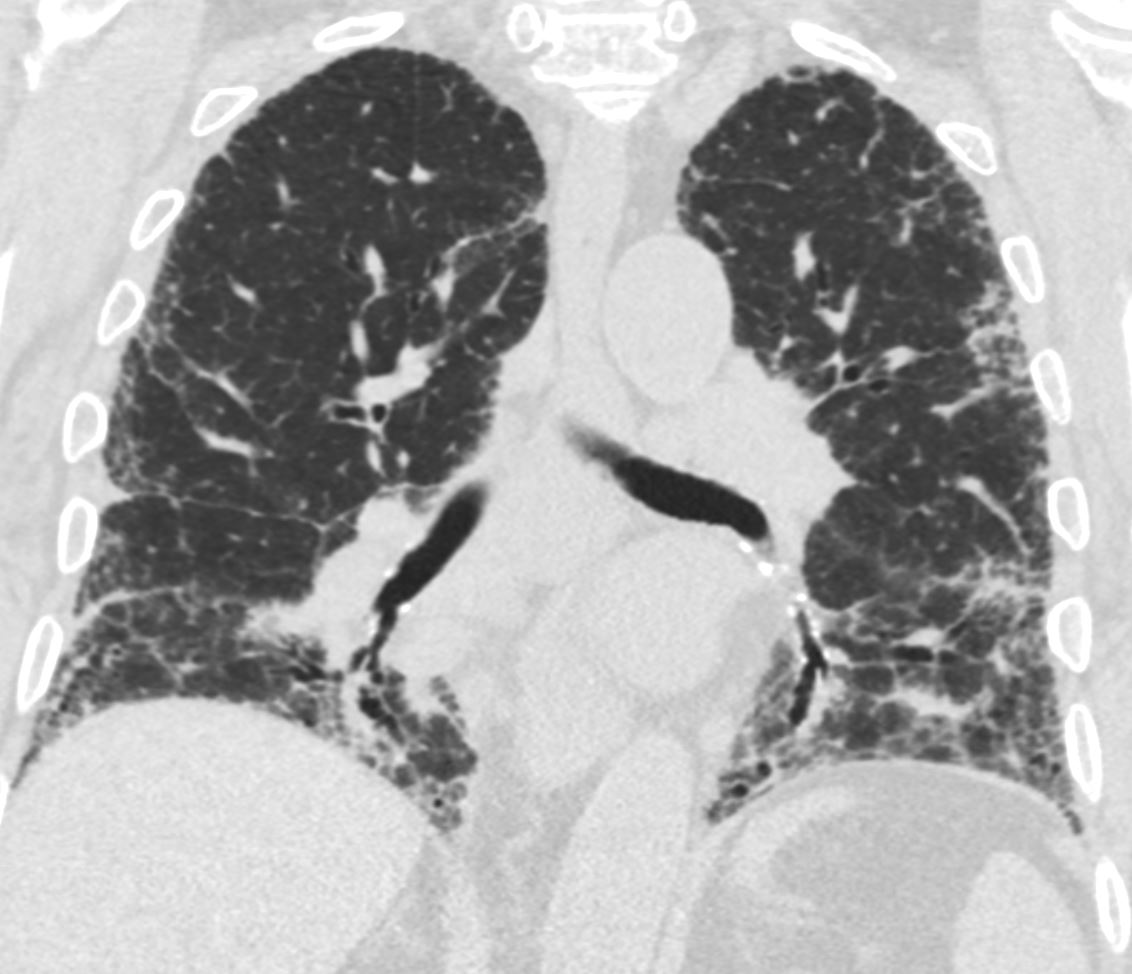
70 year old male with UIP showing extensive dominantly bibasilar peripheral reticulation, and bronchiolectasis in the medial basal segment of the right lower lobe
Ashley Davidoff MD TheCommonVein.net uip-003
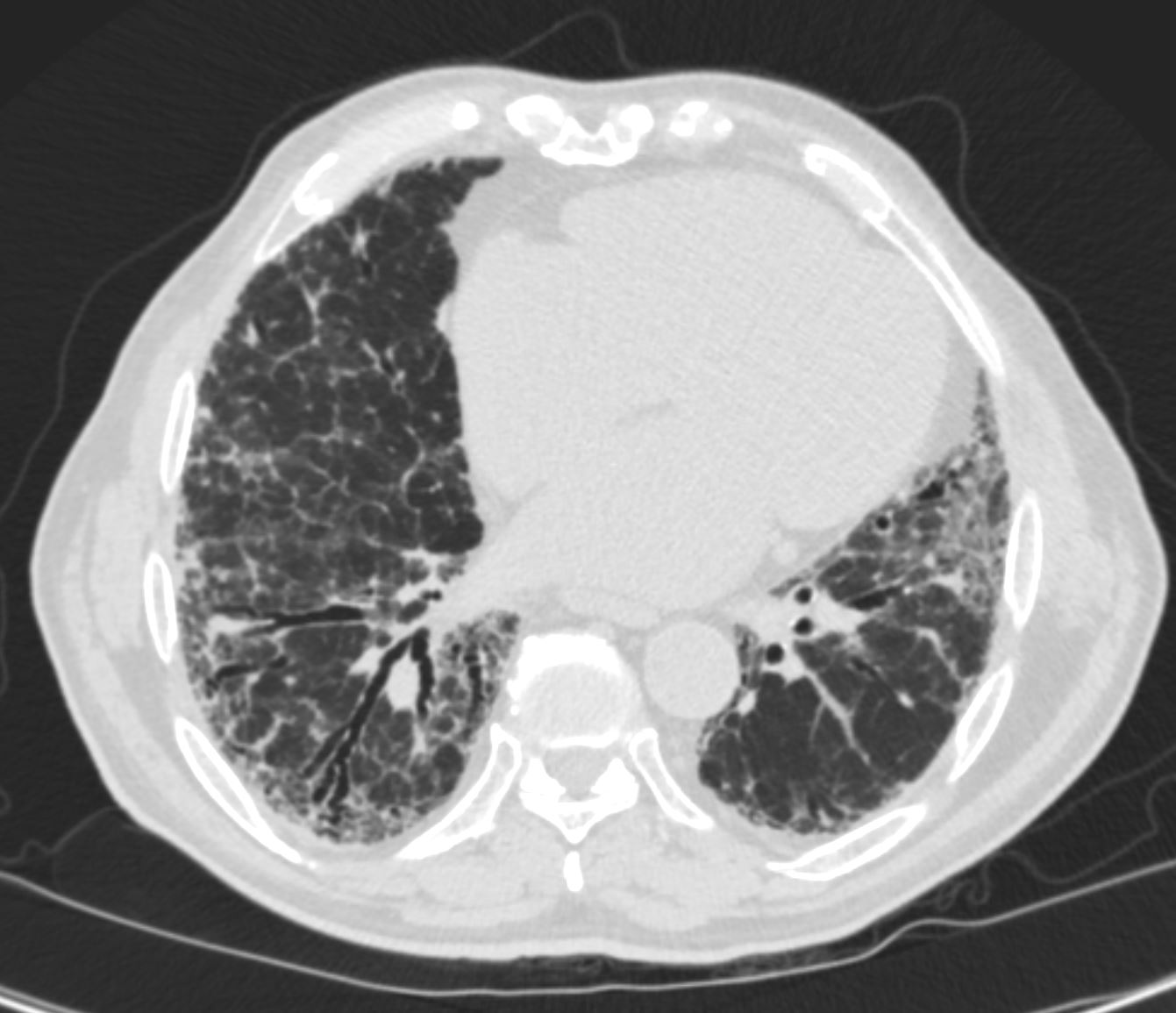
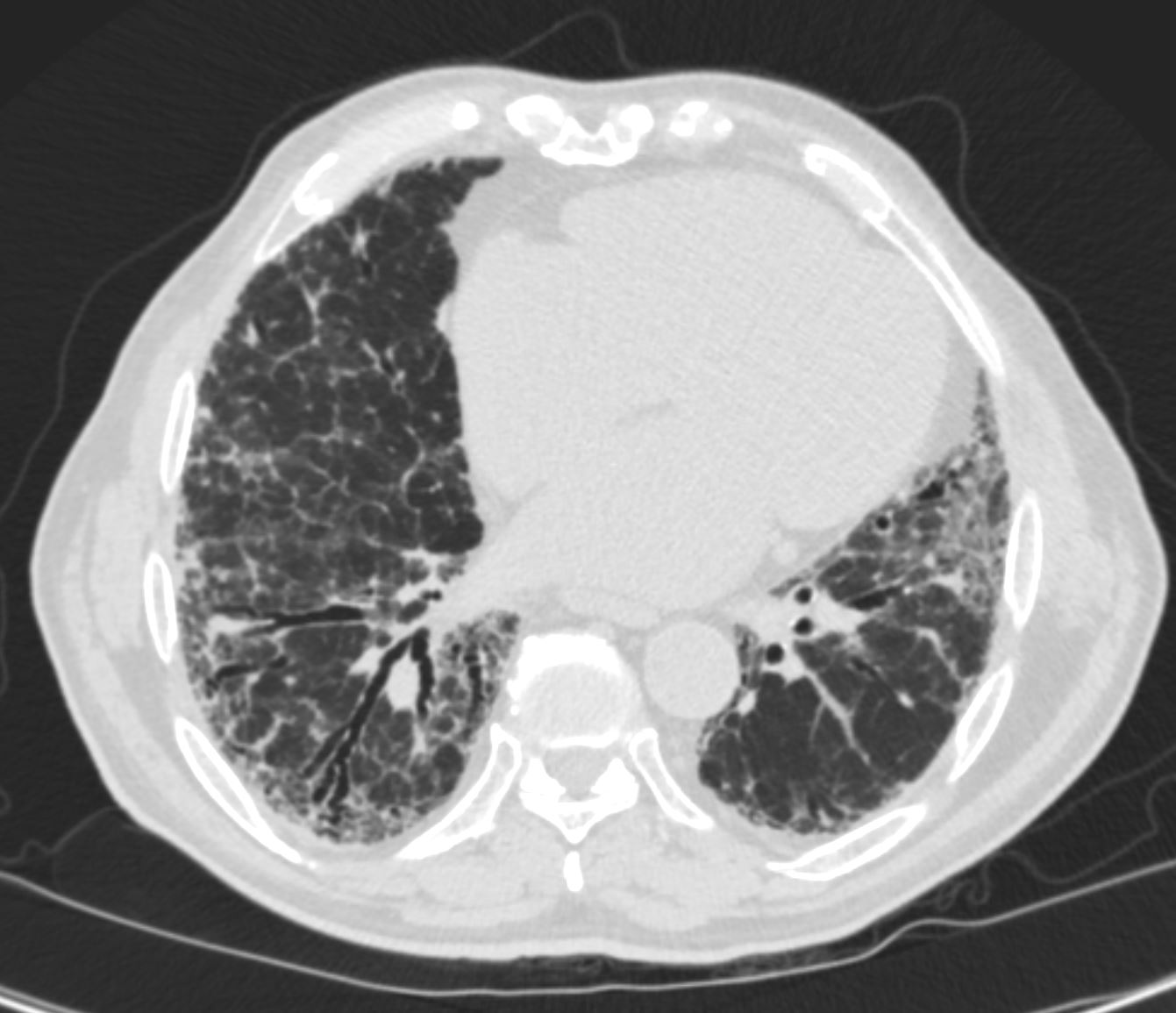
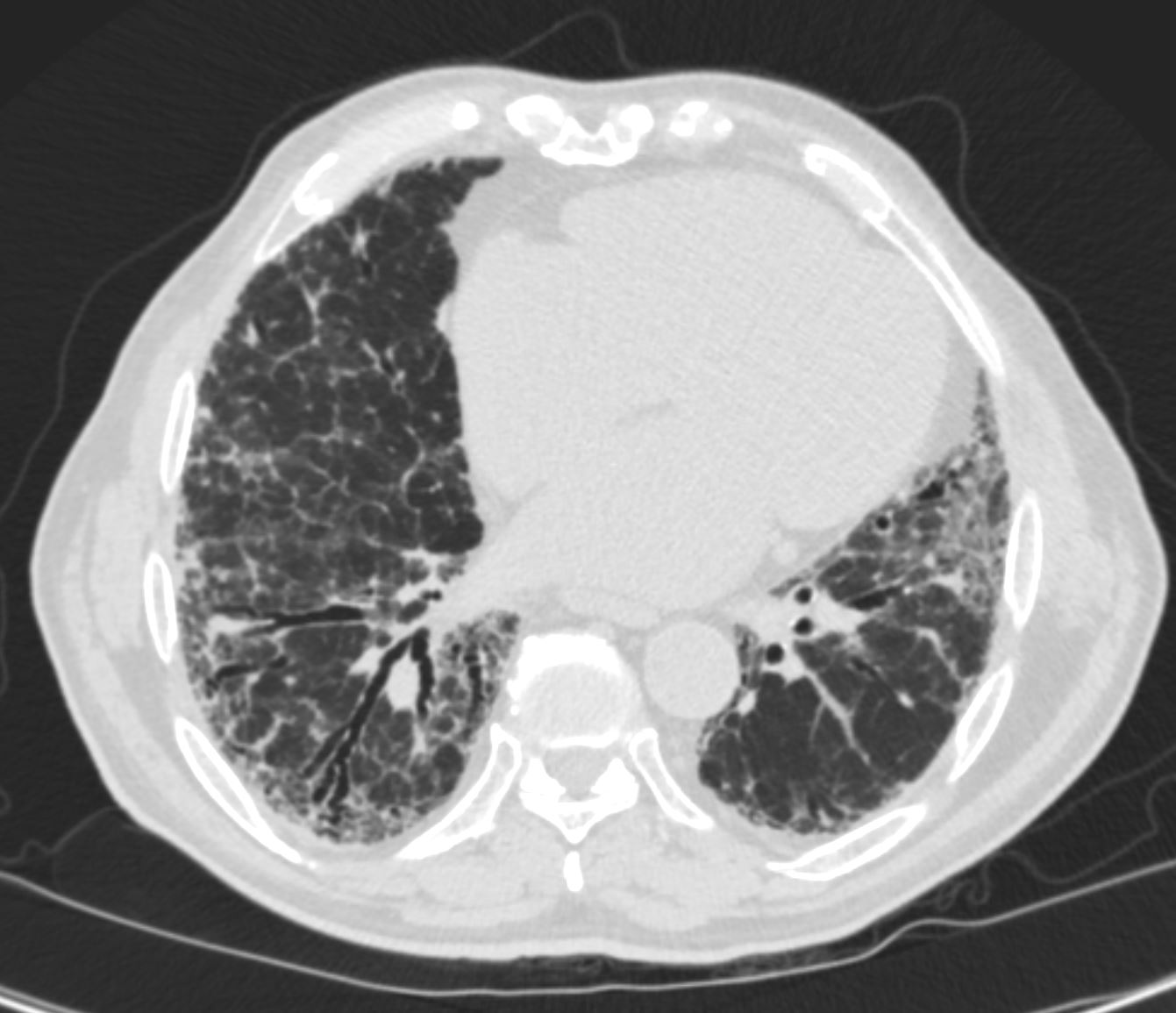
70 year old male with UIP showing extensive, dominantly bibasilar peripheral reticulation, and bronchiolectasis in the medial basal segment of the right lower lobe
Ashley Davidoff MD TheCommonVein.net uip-007
Interstitial Fibrosis
-
-

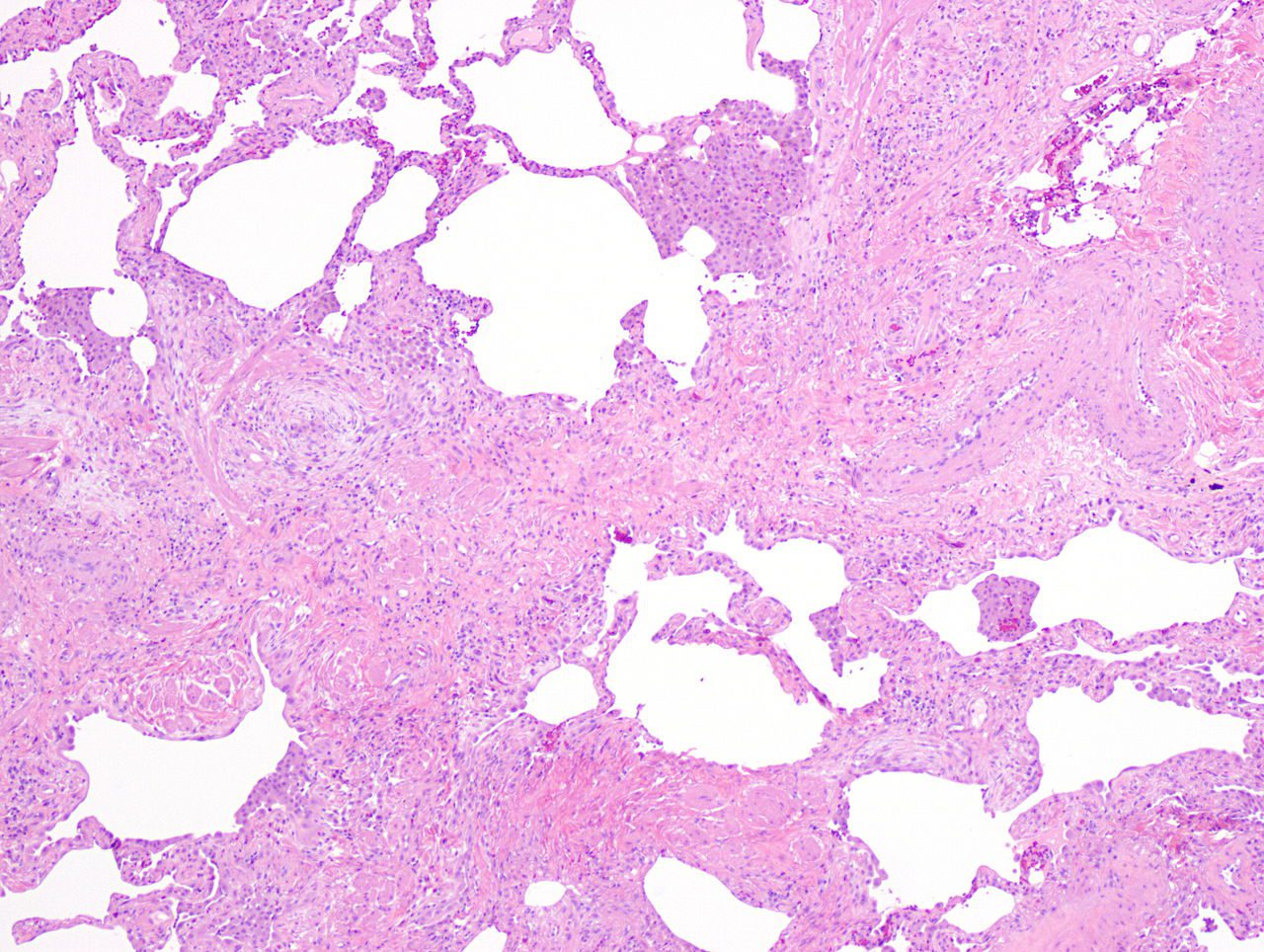
Appearance of usual interstitial pneumonia (UIP) in a surgical lung biopsy at low magnification. The tissue is stained with hematoxylin (purple dye) and eosin (pink dye) to make it visible. The pink areas in this picture represent lung fibrosis (collagen stains pink). Note the “patchwork” (quilt-like) pattern of the fibrosis.
Source Public Domain
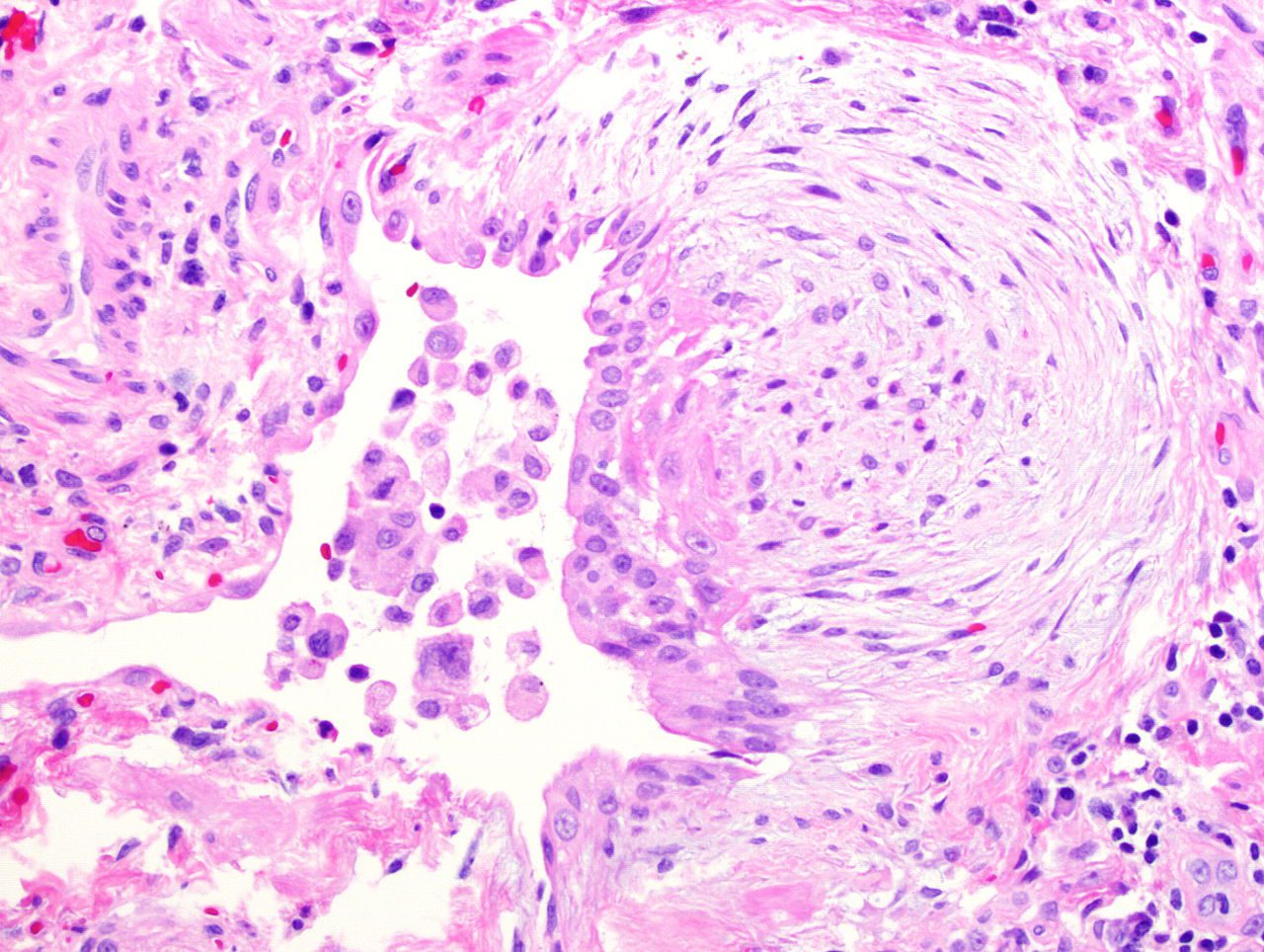
A fibroblast focus in a surgical lung biopsy of UIP. Hematoxylin-eosin stain, high magnification. The white space to the left is an airspace. The pale area to the right is a fibroblast focus. It is an area of active fibroblast proliferation within the interstitium of the lung.
Source Public Domain
-
Progression of Disease


As the disease progresses the lower disease becomes more extensive and the disease progresses into the periphery of the upper lobes as well
Ashley Davidoff MD TheCommonvein.net lungs-0769c
The Interstitial Fibrotic Process Progresses – Resulting in Honey Comb Lung and May Involve the Small Airways as Well
Honey Comb Lung
The honeycomb change in usual interstitial pneumonia (UIP) is thought to be the end result of chronic interstitial inflammation and fibrosis.
In UIP, there is chronic inflammation and injury to the lung tissue, leading to the accumulation of scar tissue (fibrosis) and destruction of normal lung architecture. The honeycomb change refers to the presence of cystic airspaces lined by thickened fibrous tissue and surrounded by areas of dense fibrosis, resembling a honeycomb. These cystic airspaces are the result of progressive destruction of normal lung tissue and the replacement of the destroyed tissue by fibrosis.
The exact mechanism underlying the honeycomb change in UIP is not fully understood, but it is believed to be the result of a combination of factors, including:
- Persistent lung injury: Chronic injury to the lung tissue leads to the accumulation of scar tissue and destruction of normal lung architecture.
- Abnormal wound healing: Abnormal wound healing response to the chronic lung injury leads to the formation of dense fibrosis.
- Altered surfactant metabolism: Altered metabolism of surfactant, which is a substance that helps to keep the air sacs in the lungs open, can lead to collapse of the air sacs and the formation of cystic airspaces.
- Impaired regeneration: Impaired regeneration of lung tissue due to aging or other factors may also contribute to the development of honeycomb change in UIP.
In summary, the honeycomb change in UIP is the result of chronic interstitial inflammation and fibrosis, which leads to the destruction of normal lung tissue and the formation of cystic airspaces surrounded by areas of dense fibrosis.
Honeycomb lung is subpleural in location because the subpleural area is more susceptible to injury and fibrosis than other areas of the lung.
The subpleural area is the region just beneath the pleura, which is a thin membrane that lines the surface of the lungs and the inside of the chest wall. The subpleural area is the site where the alveoli (air sacs) are located and is involved in gas exchange between the lungs and the bloodstream.
In usual interstitial pneumonia (UIP), which is the most common cause of honeycomb lung, there is chronic inflammation and fibrosis of the lung tissue. The subpleural area is more exposed to environmental insults, such as inhaled irritants, viral infections, or autoimmune processes, that can lead to chronic inflammation and injury of the lung tissue. The subpleural area is also more susceptible to mechanical stress, such as the strain that occurs during breathing, which can contribute to the development of fibrosis.
Furthermore, the subpleural area is relatively poorly vascularized and has less supportive tissue than other areas of the lung, making it more prone to injury
In patients with interstitial lung disease, the inflammatory process and interstitial fibrotic disease progresses and the walls between the alveoli are destroyed causing large subpleural, variably sized, subpleural, thick walled, stacked, cystic spaces . The appearance is reminiscent of a honeycomb and indicates end stage fibrosis
Ashley Davidoff MD thecommonvein.net lungs-0738bh
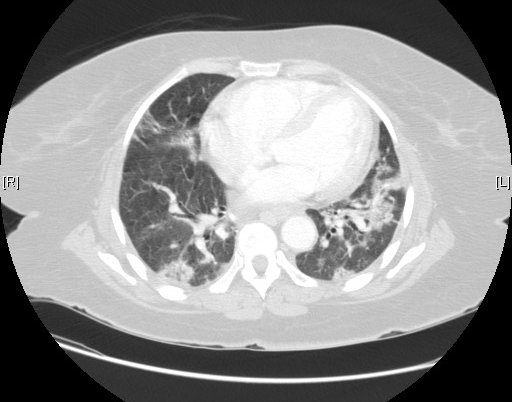
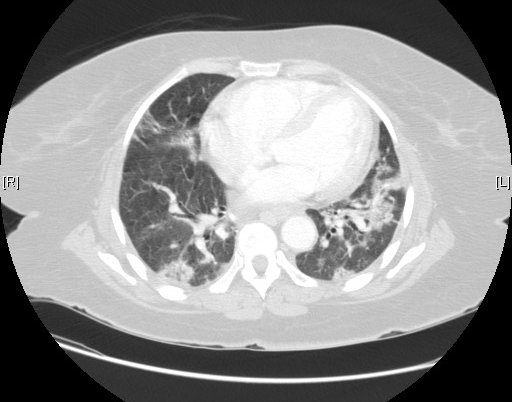
Imaging in an 81F with End Stage UIP


Ashley Davidoff TheCommonVein.net 81f lungs uip 003
Ashley Davidoff TheCommonVein.net 81f lungs uip 004
Ashley Davidoff
TheCommonVein.net
Ashley Davidoff MD TheCommonVein.net
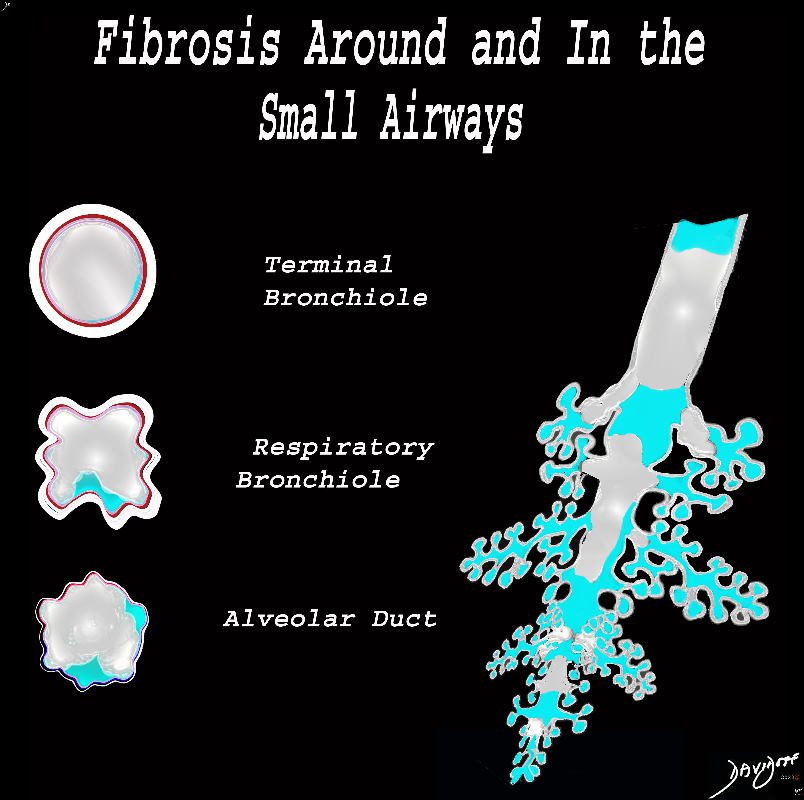
Small Airway Disease
- While UIP is primarily a disease of the lung interstitium, it can also affect the airways to varying degrees.
- Small airway involvement in UIP can contribute to symptoms such as cough, wheezing, and shortness of breath.
- Small airway involvement can also be a predictor of more rapid disease progression and worse outcomes.
- Small airway involvement is also a feature of other interstitial lung diseases, such as nonspecific interstitial pneumonia (NSIP) and respiratory bronchiolitis-associated interstitial lung disease (RB-ILD).
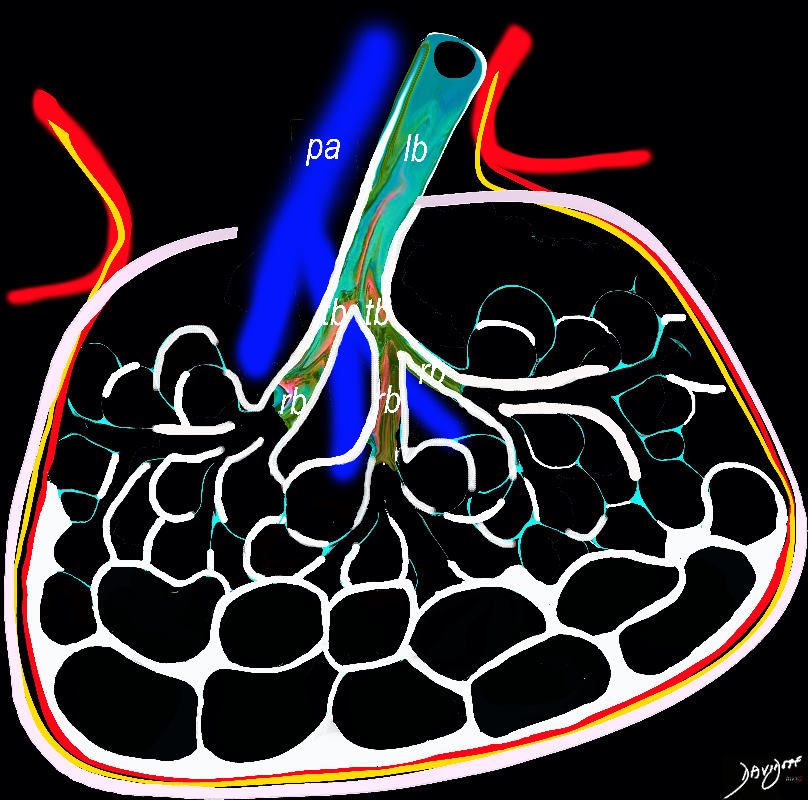
Small Airway Fibrosis
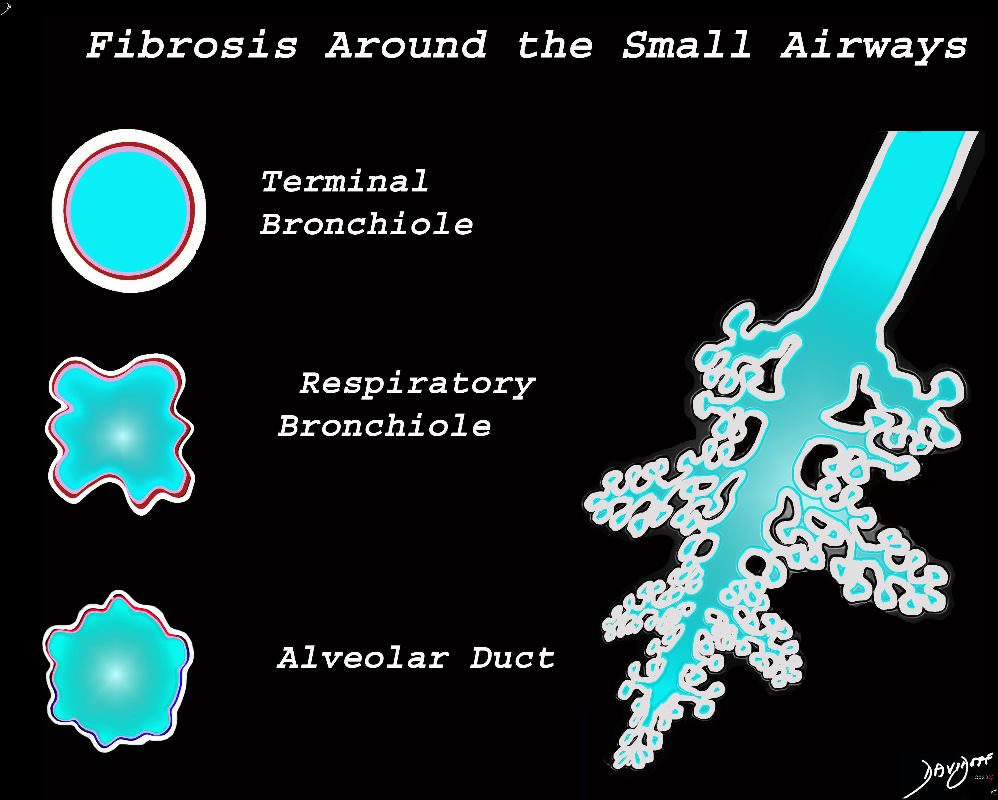
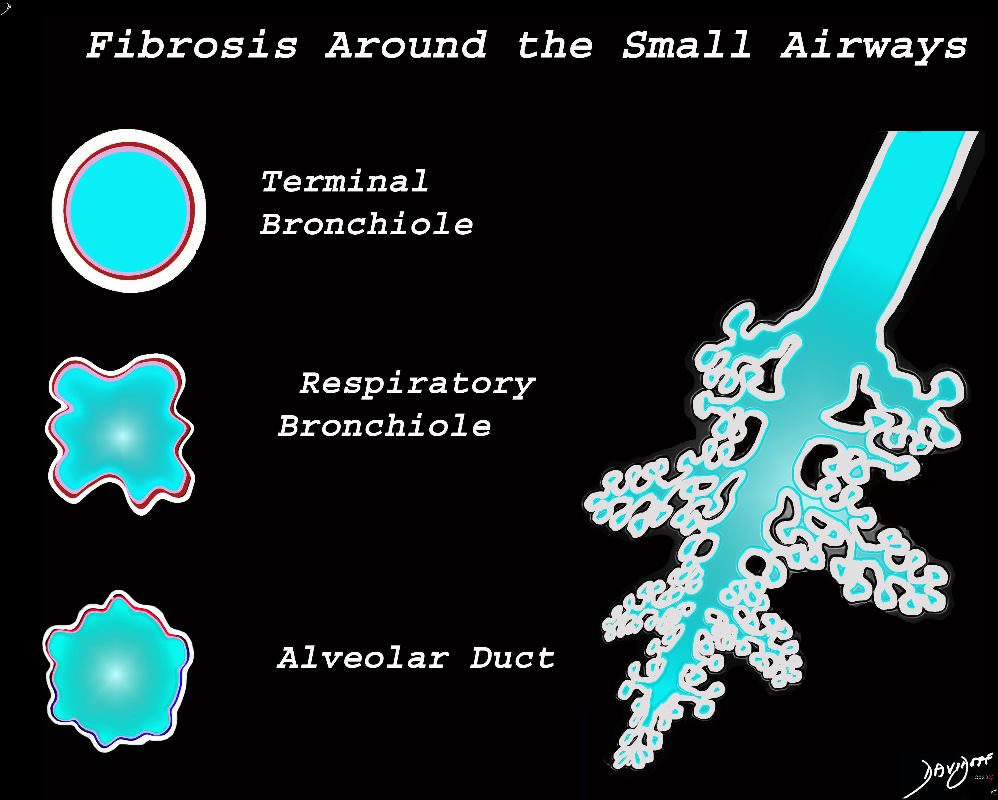
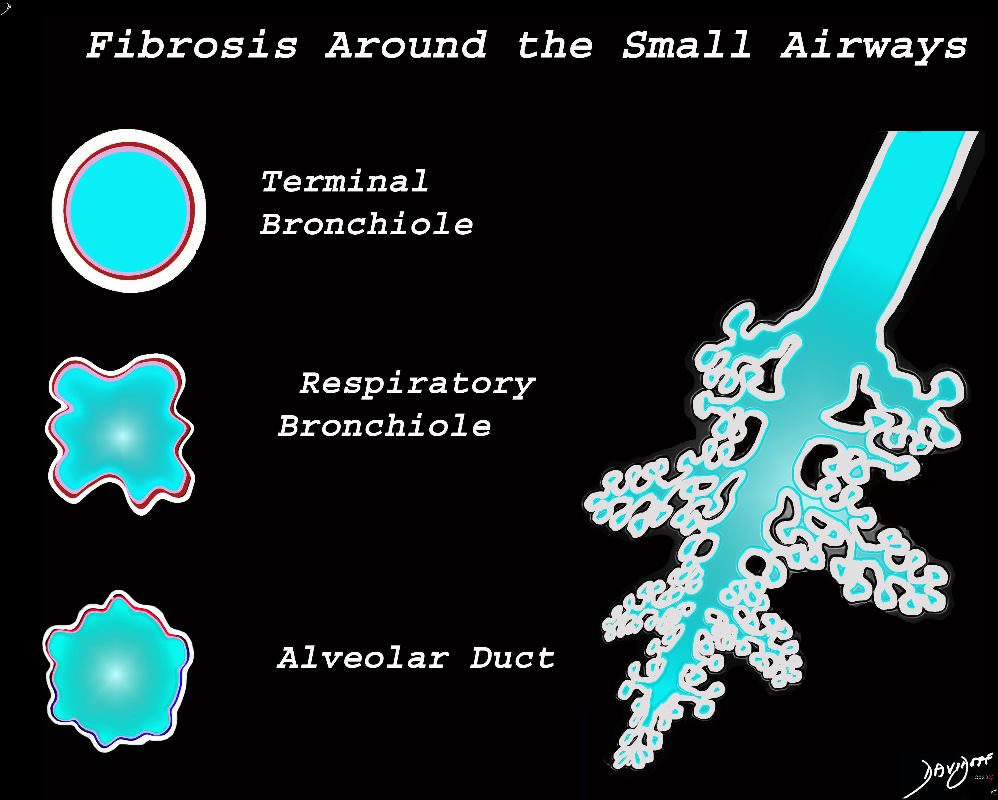
The diagram shows fibrotic changes around the small airways including the terminal bronchiole, respiratory bronchiole and the alveolar duct. In this instance the increase density from the fibrotic tissue would result in ground glass changes in the parenchyma and ground glass centrilobular nodules. Since the airways are patent there would be no air trapping.
Ashley Davidoff MD TheCommonVein.net lungs-0777
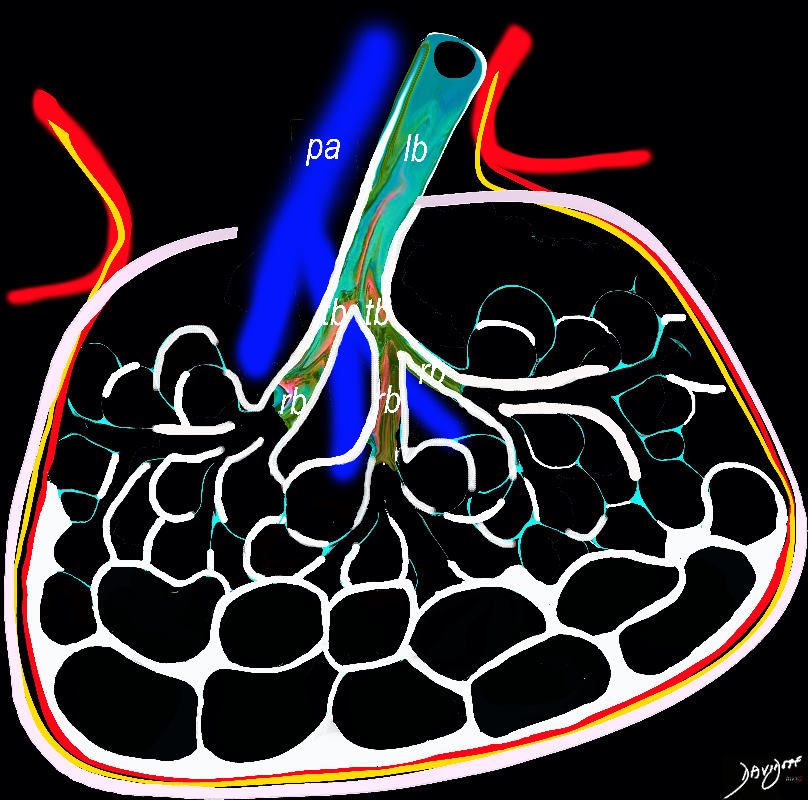
Small Airway Fibrosis and Luminal Narrowing or Obstruction
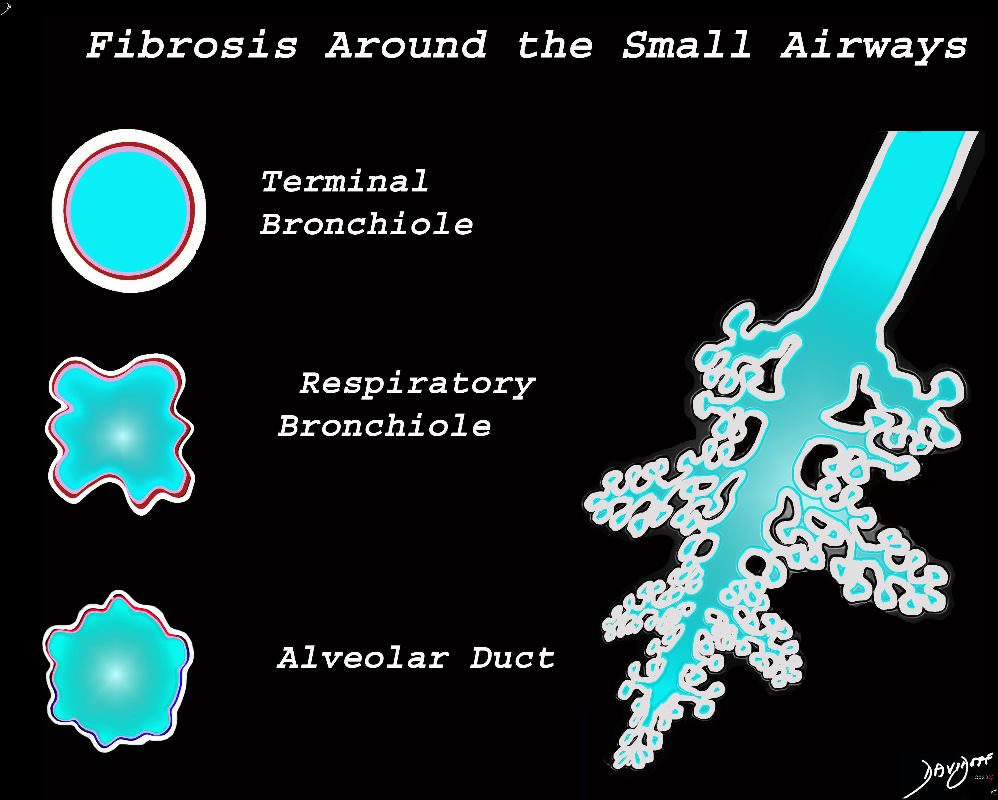
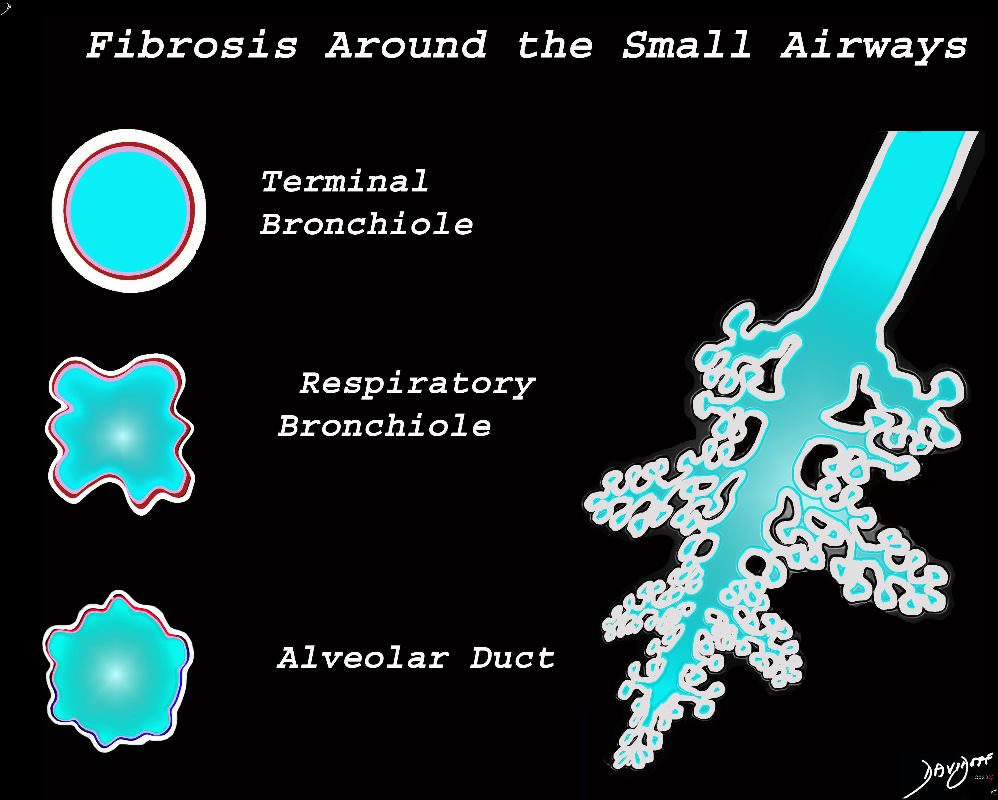
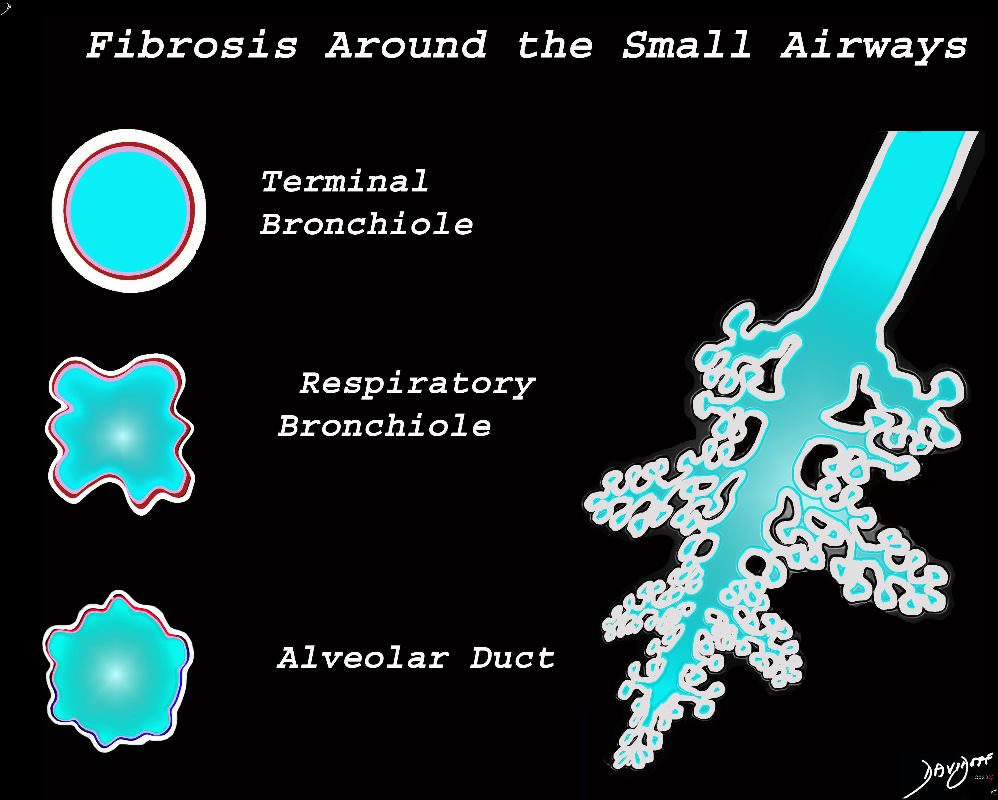
The diagram shows fibrotic changes around the small airways including the terminal bronchiole, respiratory bronchiole and the alveolar duct. In this instance the increase density from the fibrotic tissue would result in ground glass changes in the parenchyma and ground glass centrilobular nodules. Since the airways are patent there would be no air trapping.
Ashley Davidoff MD TheCommonVein.net lungs-0777
UIP and Small Airway Disease on CT scan
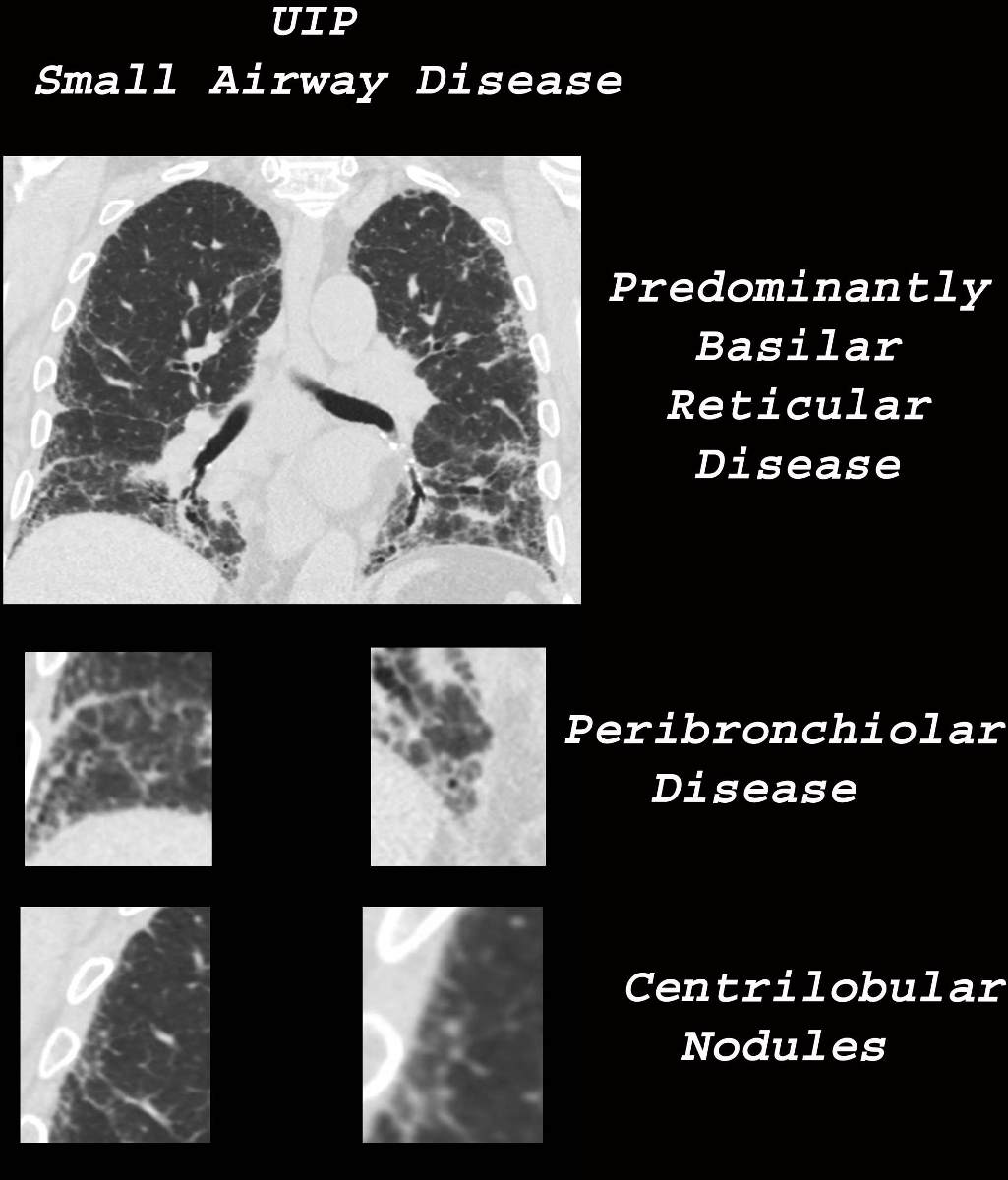
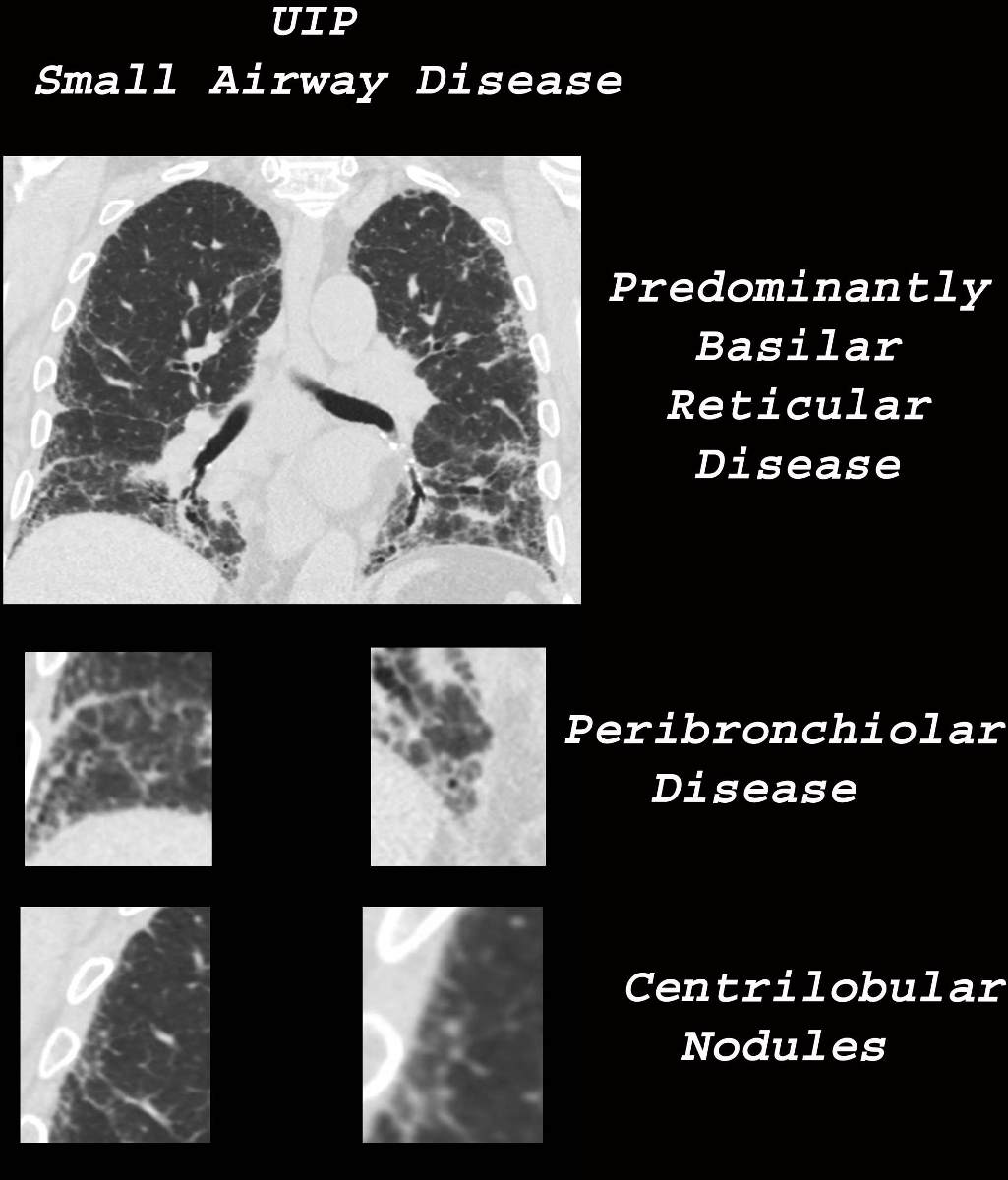
Ashley Davidoff MD TheCommonVein.net uip-002c-CT
CT in the coronal projection from a patient with UIP (upper image) shows predominantly basilar reticular disease with some extension to the upper lobes. In the middle magnified images there is thickening of the wall of a few of the visualized bronchioles The lower magnified images show solid centrilobular nodules. No air trapping was identified
Ashley Davidoff MD TheCommonVein.net lungs-0778
-
- UIP Patterns
- small but prominent mediastinall nodes
- Less common
- ground glass
- consolidation
- lung cancer
- pneumomediastinum
- ptx
- Less common
-
- 4 patterns
- Honeycombing, with or without peripheral traction bronchiectasis or bronchiolectasis
- Often heterogenous distribution, being occasionally diffuse, and may be asymmetrical
reticulation subpleural
Case courtesy of Royal Melbourne Hospital Respiratory, Radiopaedia.org
Honeycomb changes in ILD is a feature on CT of interstitial lung disease and is characterised by clusters of stacked cystic air spaces in the periphery and predominantly posteriorly at the bases of the lungs . These findings are most commonly seen in UIP. They likely represent small airways that have been denuded of the their alveoli apparatus. It is most commonly associated with idiopathic pulmonary fibrosis (IPF) and its radiological equivalent UIP – usual interstitial pneumonia.
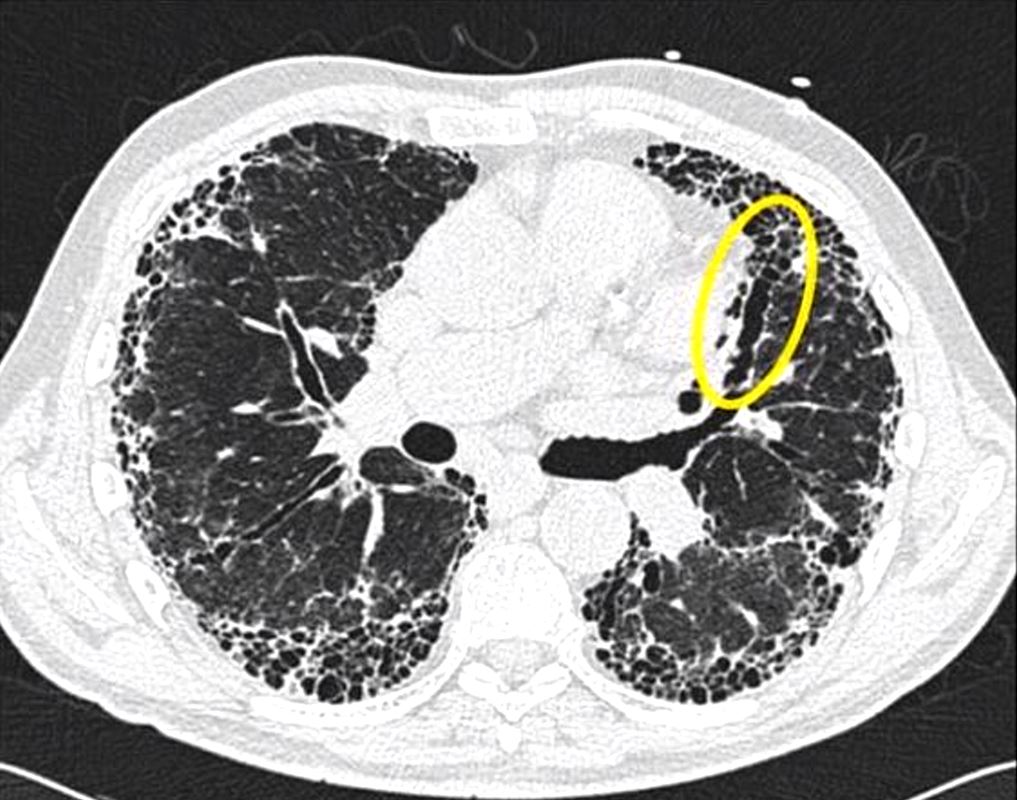
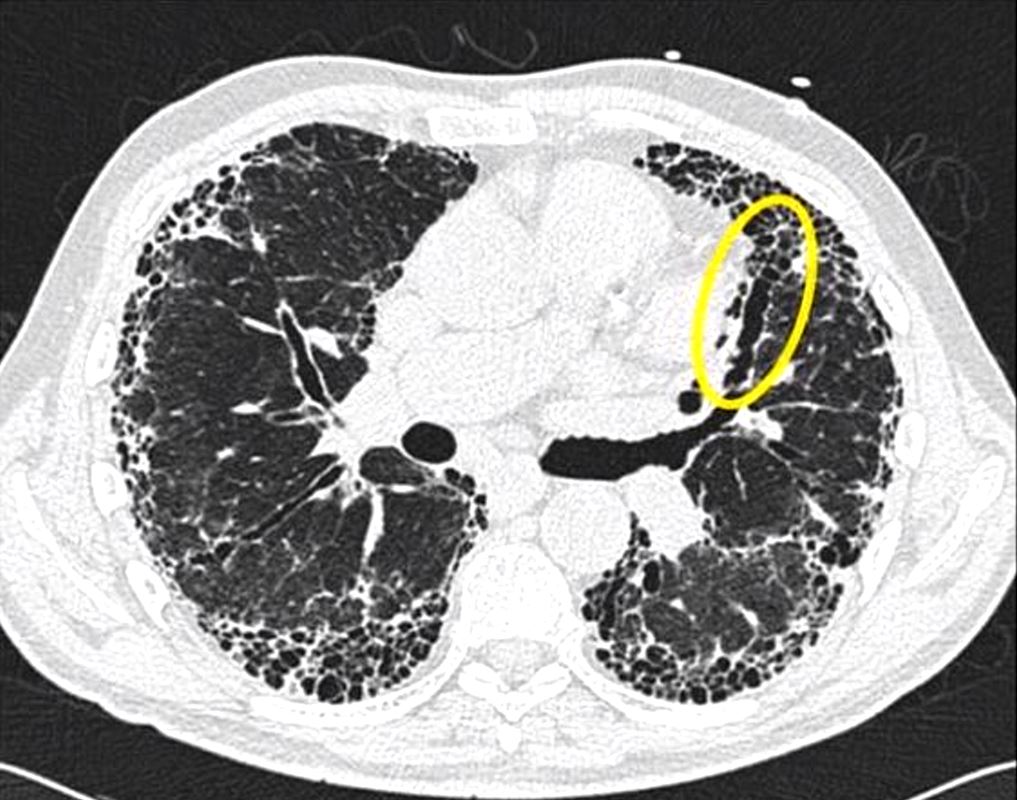
Traction bronchiectasis and bronchiolectasis (yellow ring) is as a result of fibrotic traction on the airways.
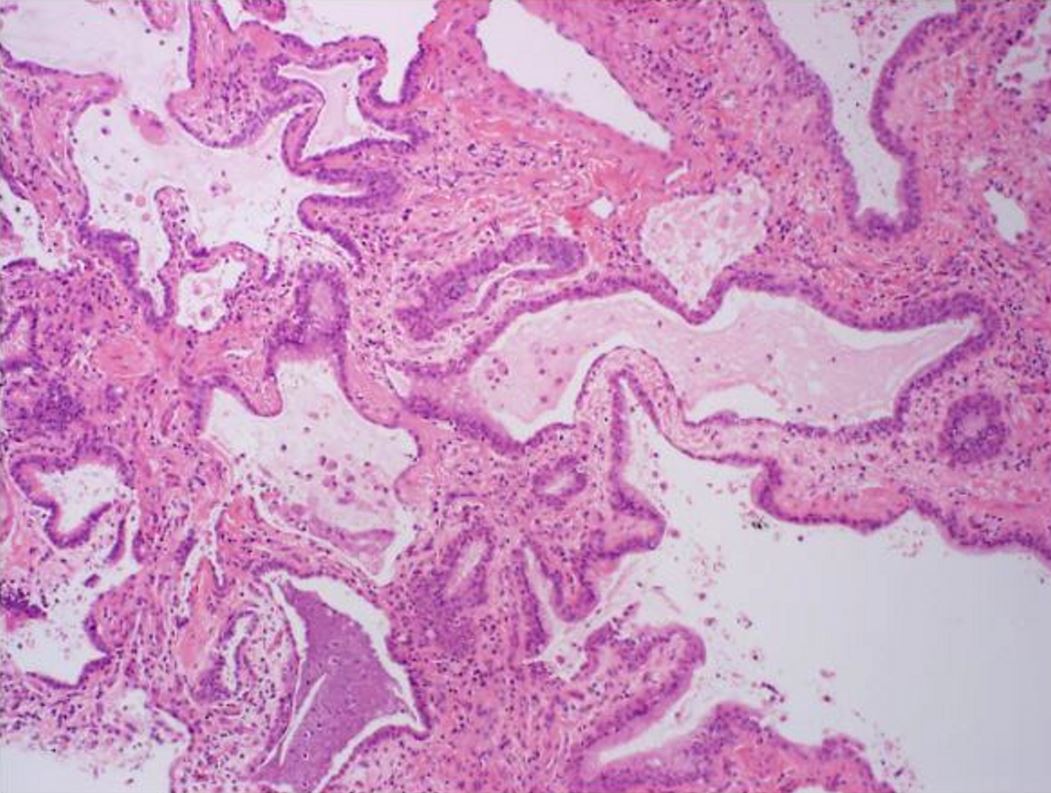
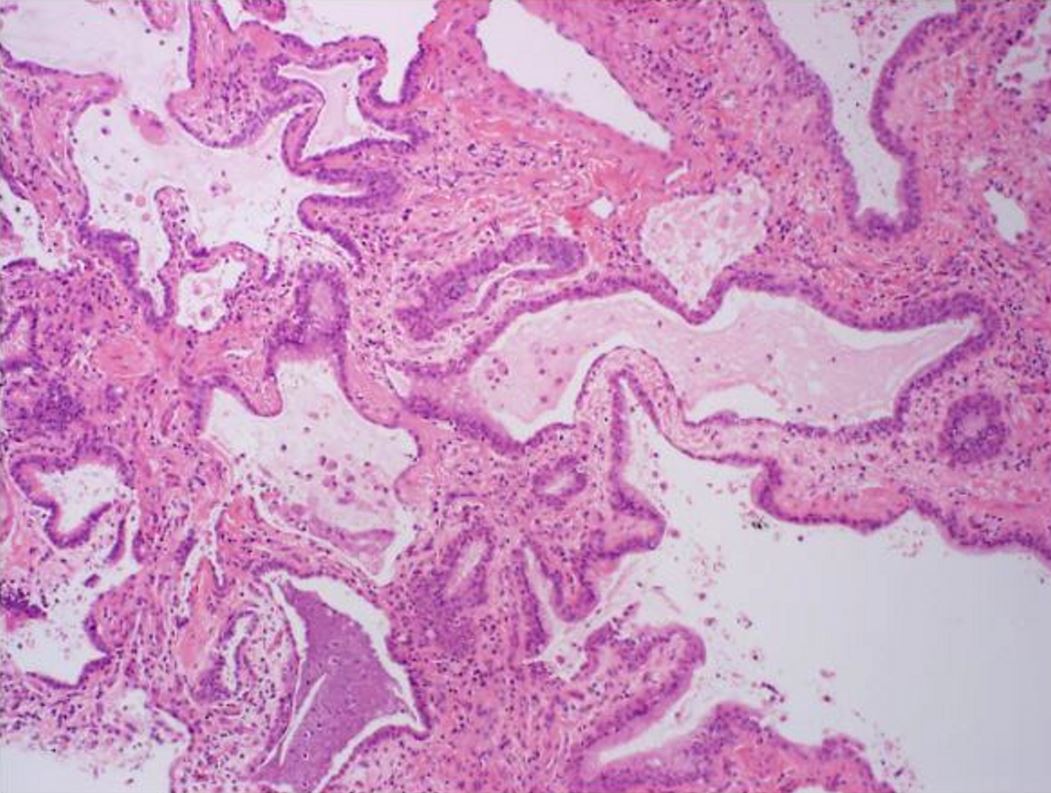
Histologic specimen shows dilated air spaces lined by bronchiolar type epithelium and surrounding fibrosis consistent with microscopic honeycomb change. Courtesy Medscape


Typical histological finding of spatial heterogeneity in usual interstitial pneumonia (UIP) with an abrupt transition from honeycomb change (left) to normal lung (right) using trichrome stain, X40)
Courtesy Medscape eMedicine
…………………………………………………………………………………………..
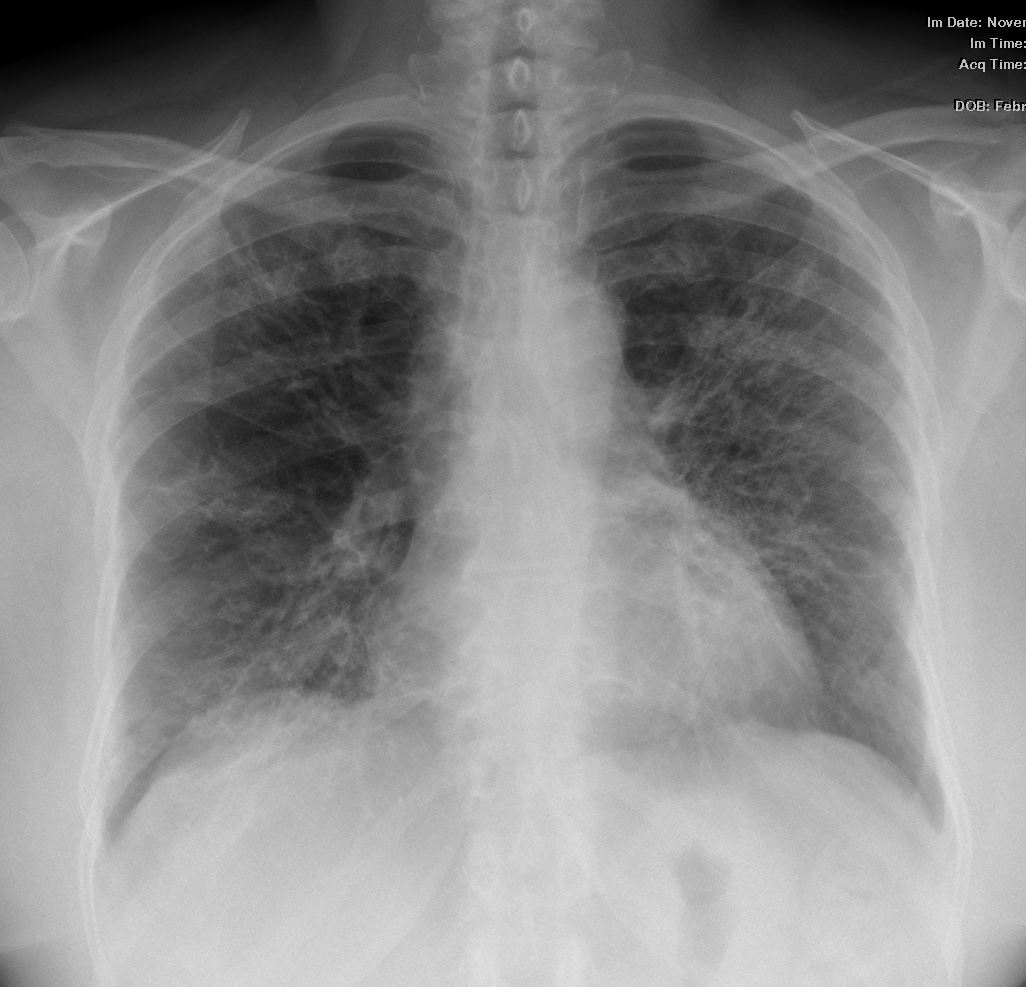
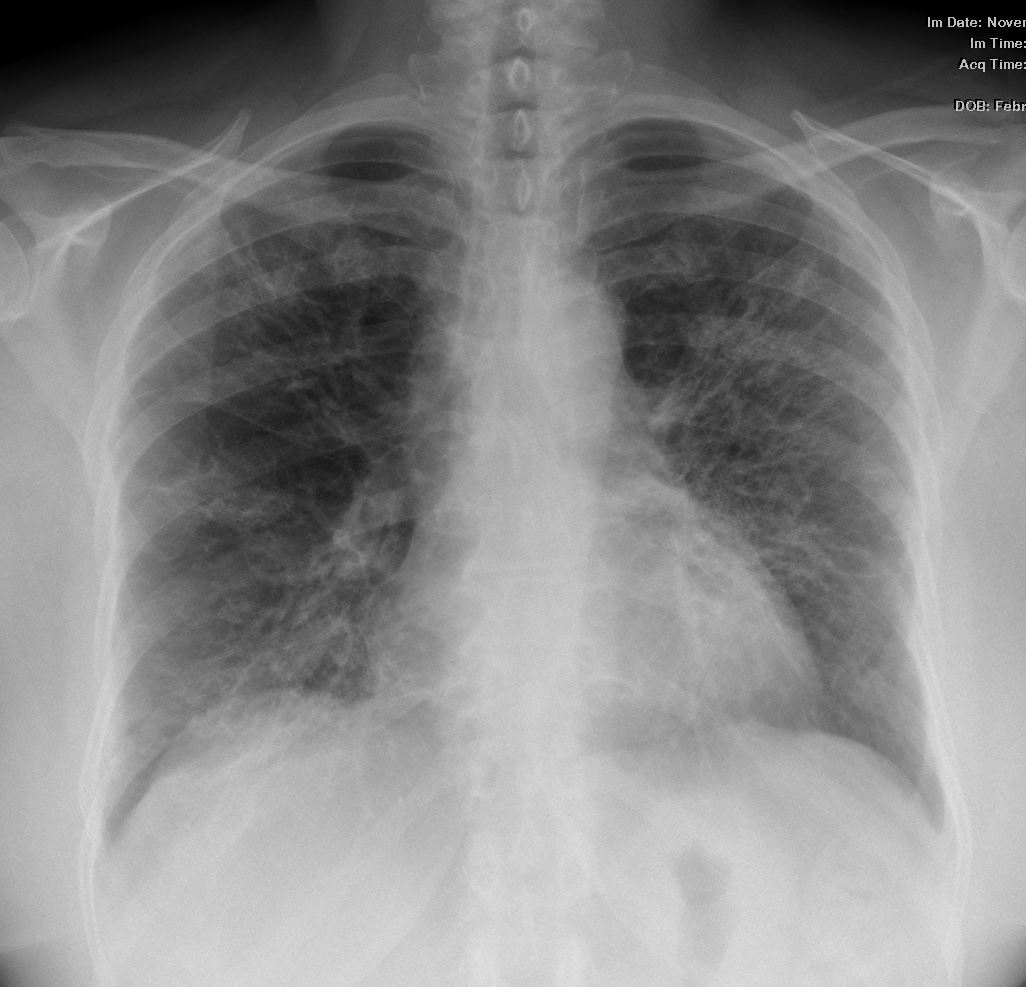
CXR from a 54 year old female with dyspnea shows diffuse retiicular changing dominantly involving the lower lobes but also to the upper lobes to lesser extent.
Ashley Davidoff MD


Axial CT through the base of the lungs shows honeycombing change sin the posterior segment of the left lower lobe characterized by the stacking of cystic spaces.
Ashley Davidoff MD


Coronal reconstruction CT through the posterior portion of the lungs shows honeycombing change sin the posterior segment of the left lower lobe characterized by the stacking of cystic spaces.
Ashley Davidoff MD
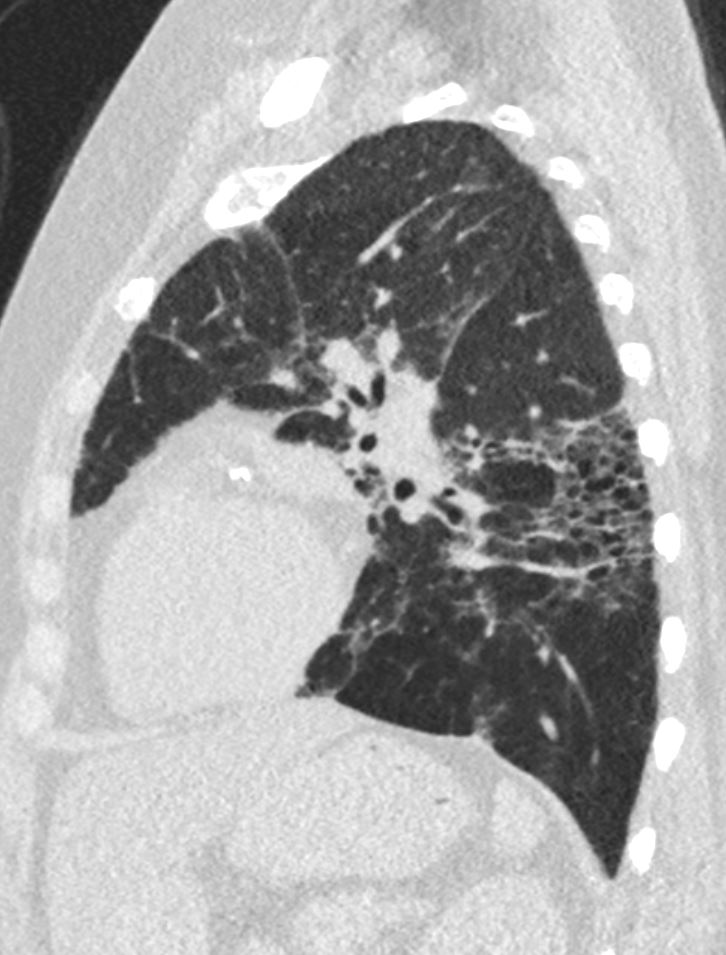
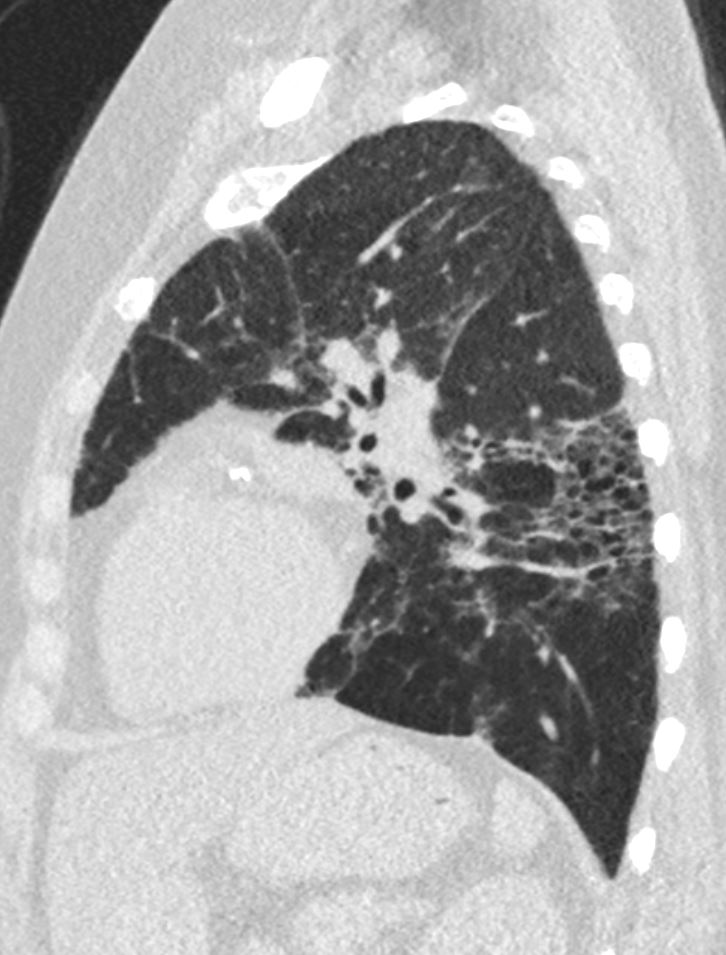
Sagittal reconstruction CT through the posterior portion of the lungs shows honeycombing change sin the posterior segment of the left lower lobe characterized by the stacking of cystic spaces.
Ashley Davidoff MD


Coronal reconstruction of a CT from a 55 year old female with dyspnea shows an asymmetric pattern of multicentric reticular interstitial fibrotic pattern with ground glass change, Bronchial wall thickening is noted in the right lower lobe..
Ashley Davidoff MD
Predominantly subpleural and basal
Traction bronchiectasis
Honeycombing
When cause is unknown it is called IPF ( idiopathic pulmonary fibrosis)
Causes collagen vascular disease connective tissue diseases (primarily rheumatoid arthritis), drug toxicity, chronic hypersensitivity pneumonitis, asbestosis and Hermansky–Pudlak syndrome.[2]
Darel Heitkamp, MD
Ashley Davidoff
TheCommonVein.net
Yale Rosen
UIP and CHF in a 70 year old male
Reticular Pattern Exemplified
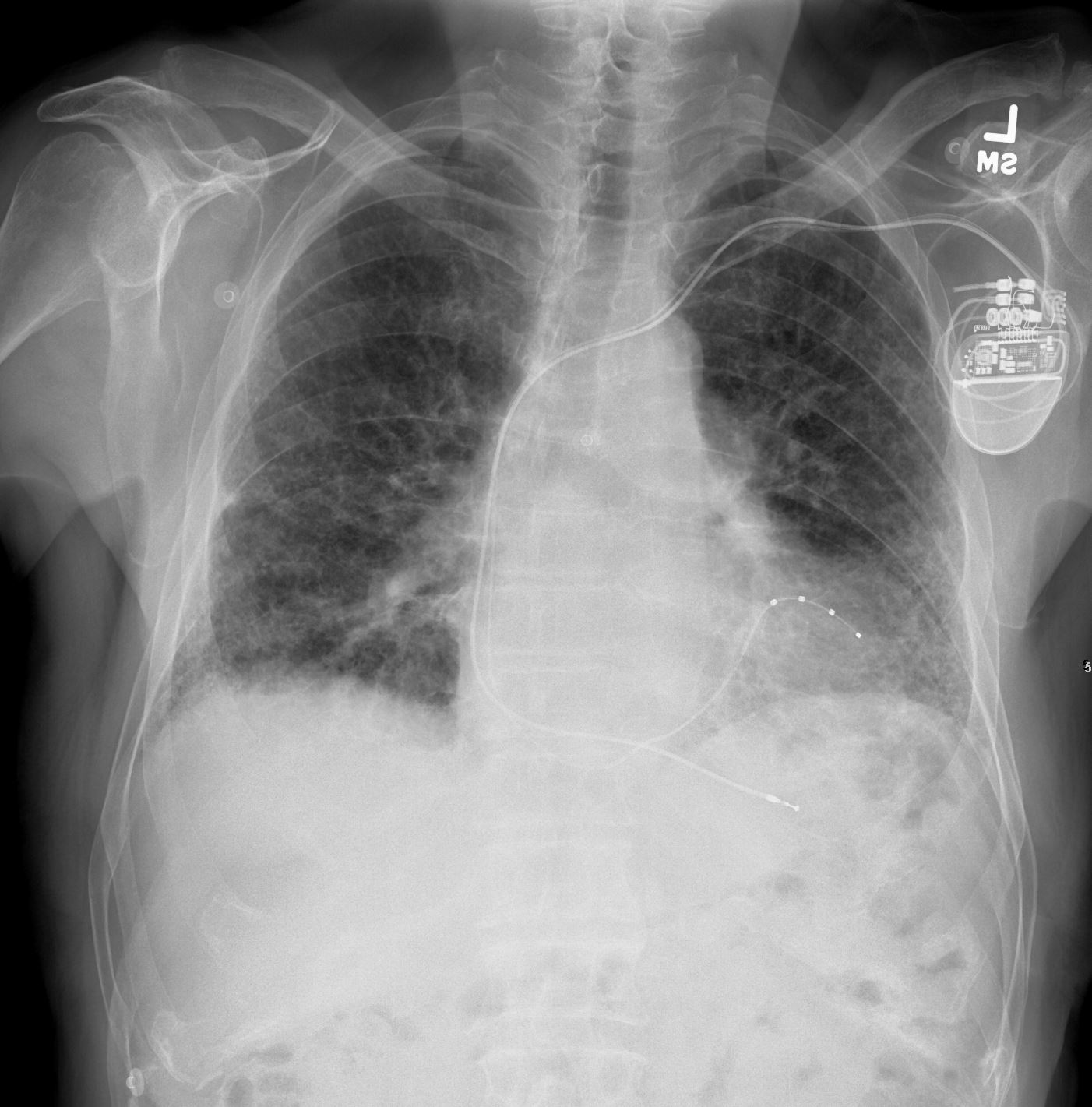
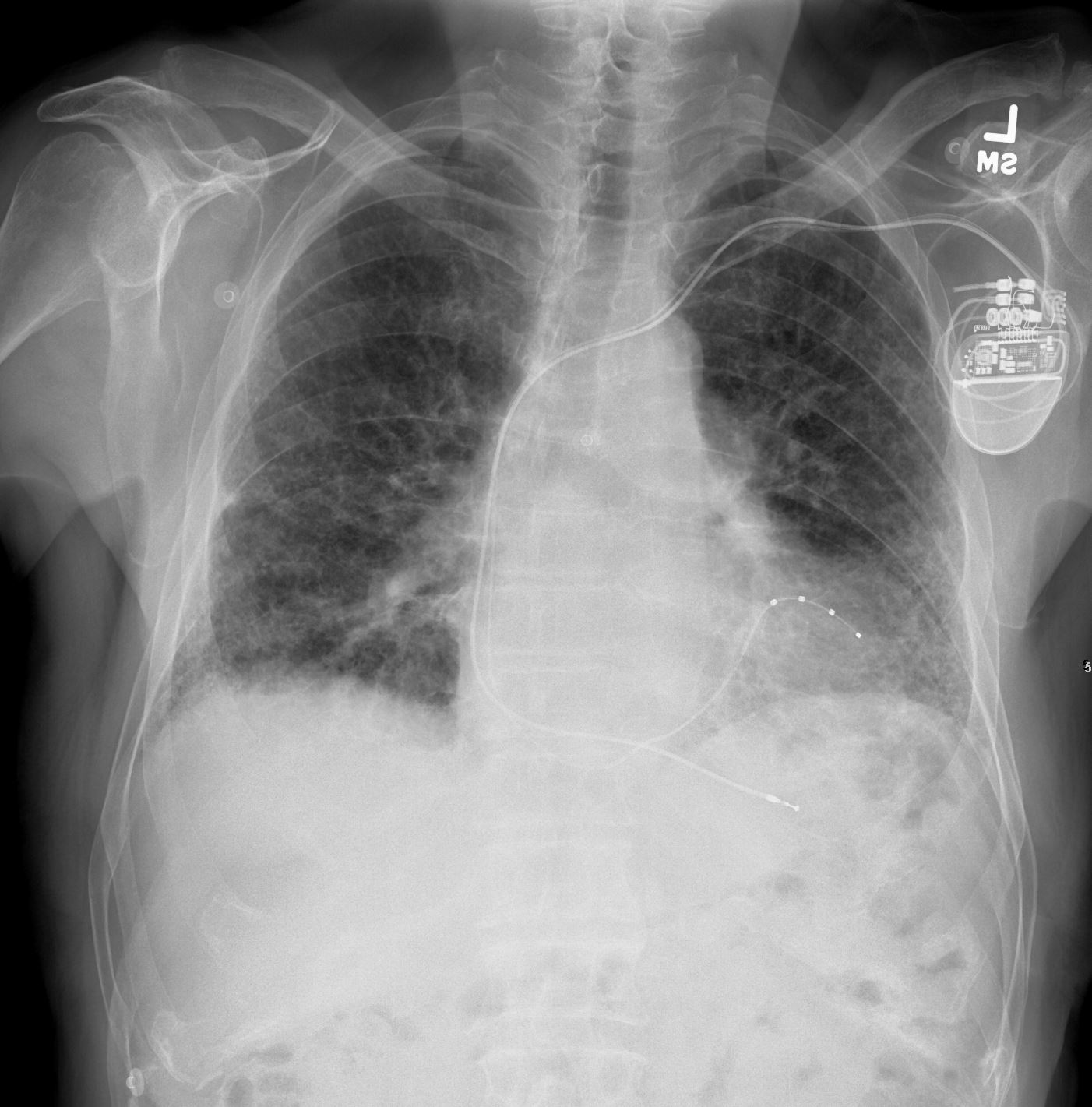
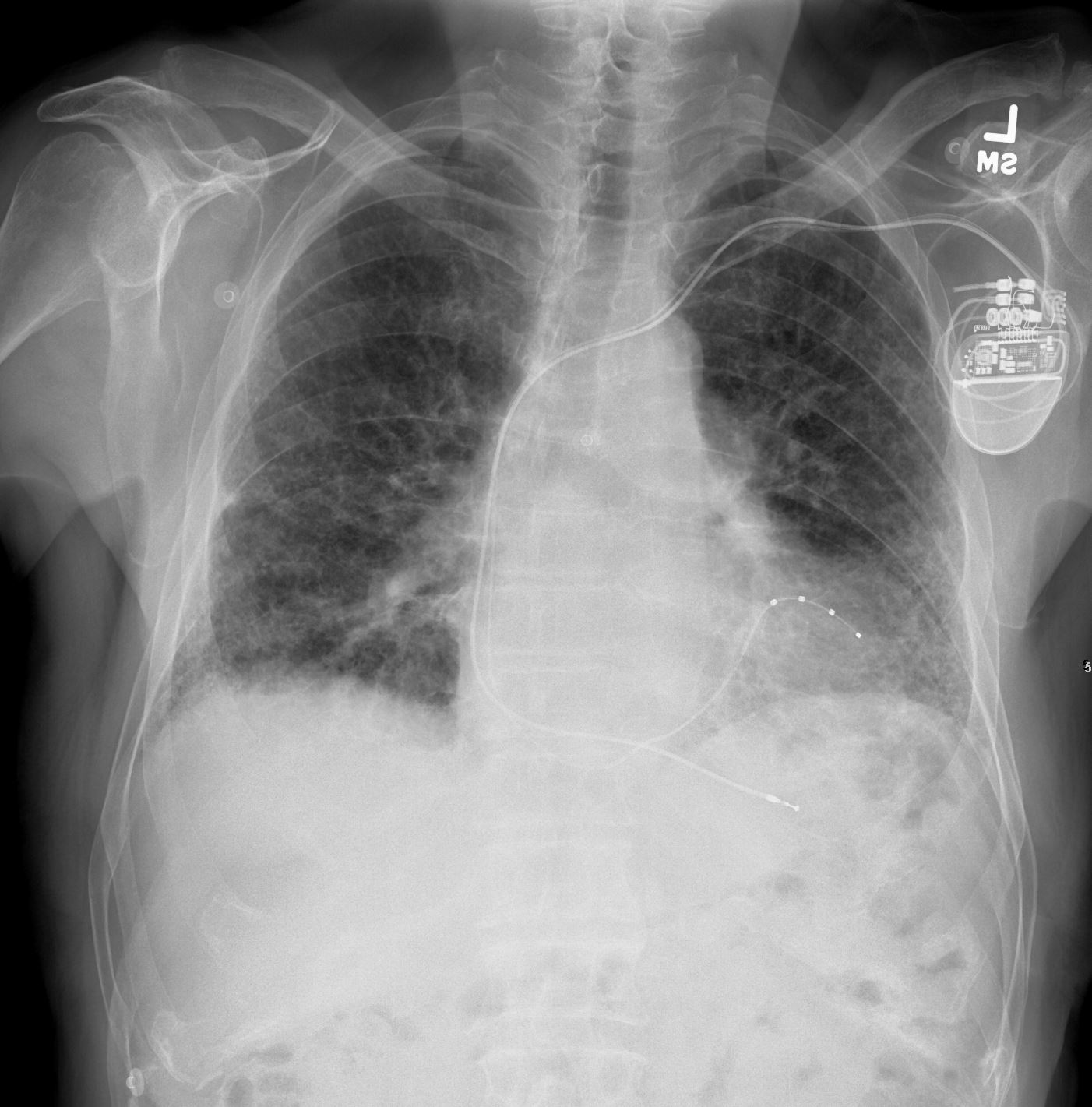
70 year old male with UIP showing extensive dominantly bibasilar and peripheral reticulation
Ashley Davidoff MD TheCommonVein.net
CT UIP and Reticular Pattern Thickened Interlobular Septa
70 year old male with UIP showing extensive dominantly bibasilar and peripheral reticulation
Ashley Davidoff MD TheCommonVein.net uip-004



70 year old male with UIP showing extensive dominantly bibasilar and peripheral reticulation
Ashley Davidoff MD TheCommonVein.net uip-003
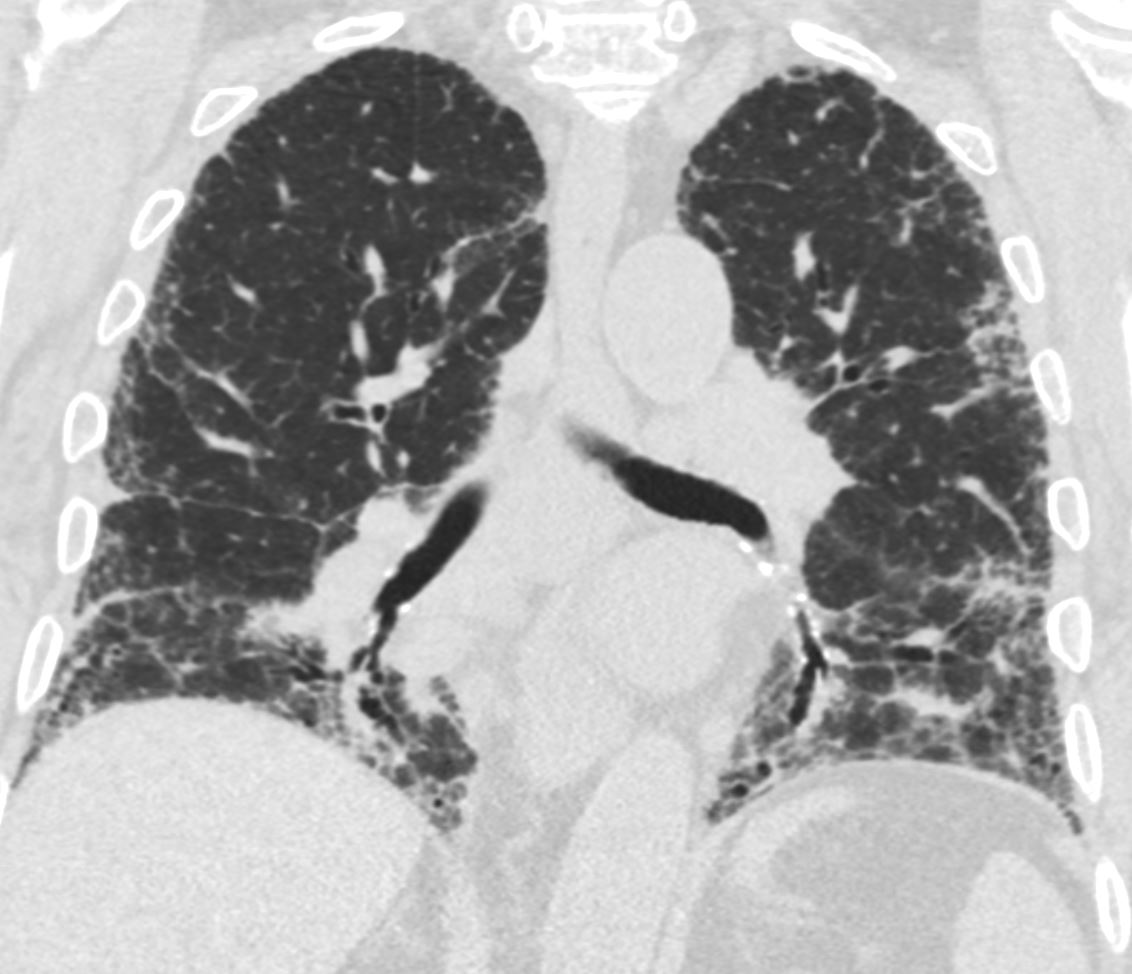
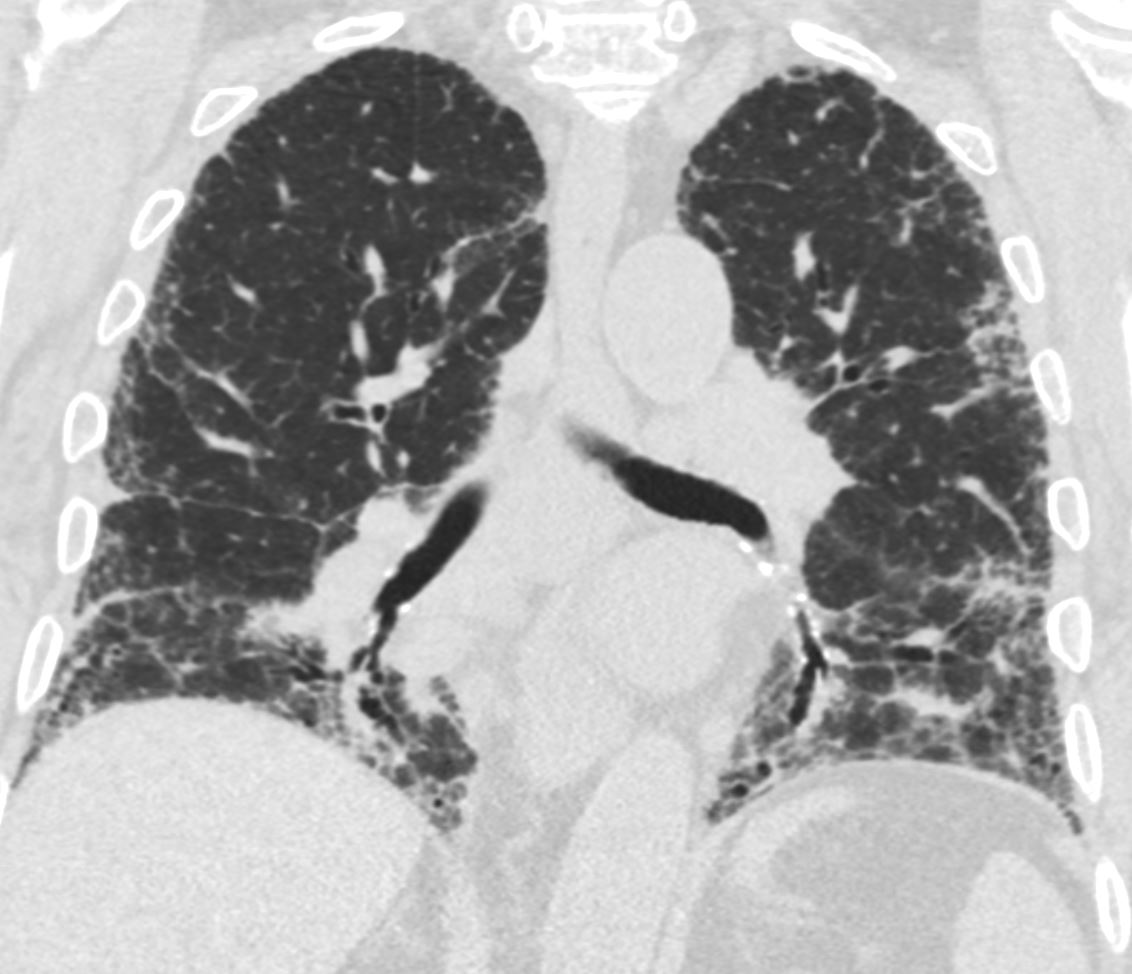
70 year old male with UIP showing extensive dominantly bibasilar and peripheral reticulation
Ashley Davidoff MD TheCommonVein.net uip-002
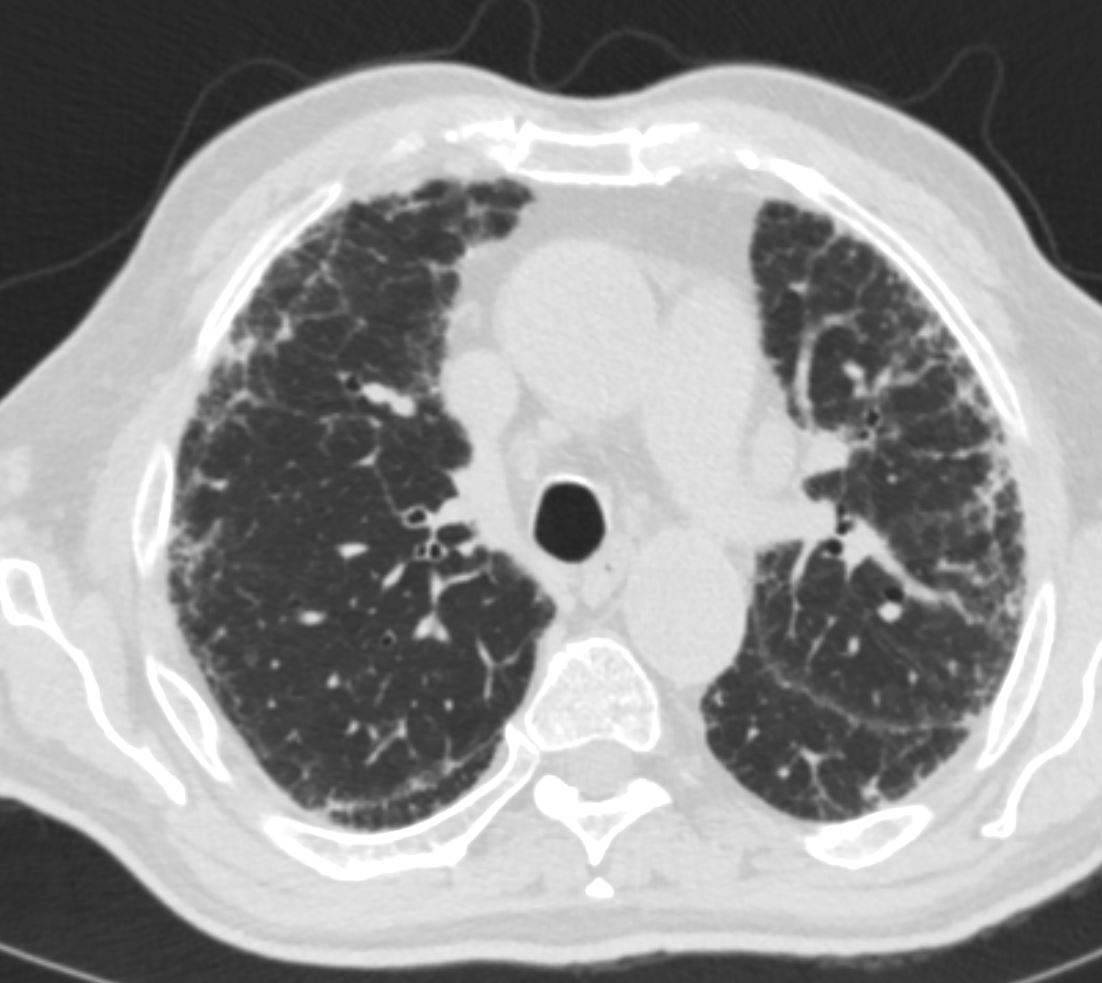
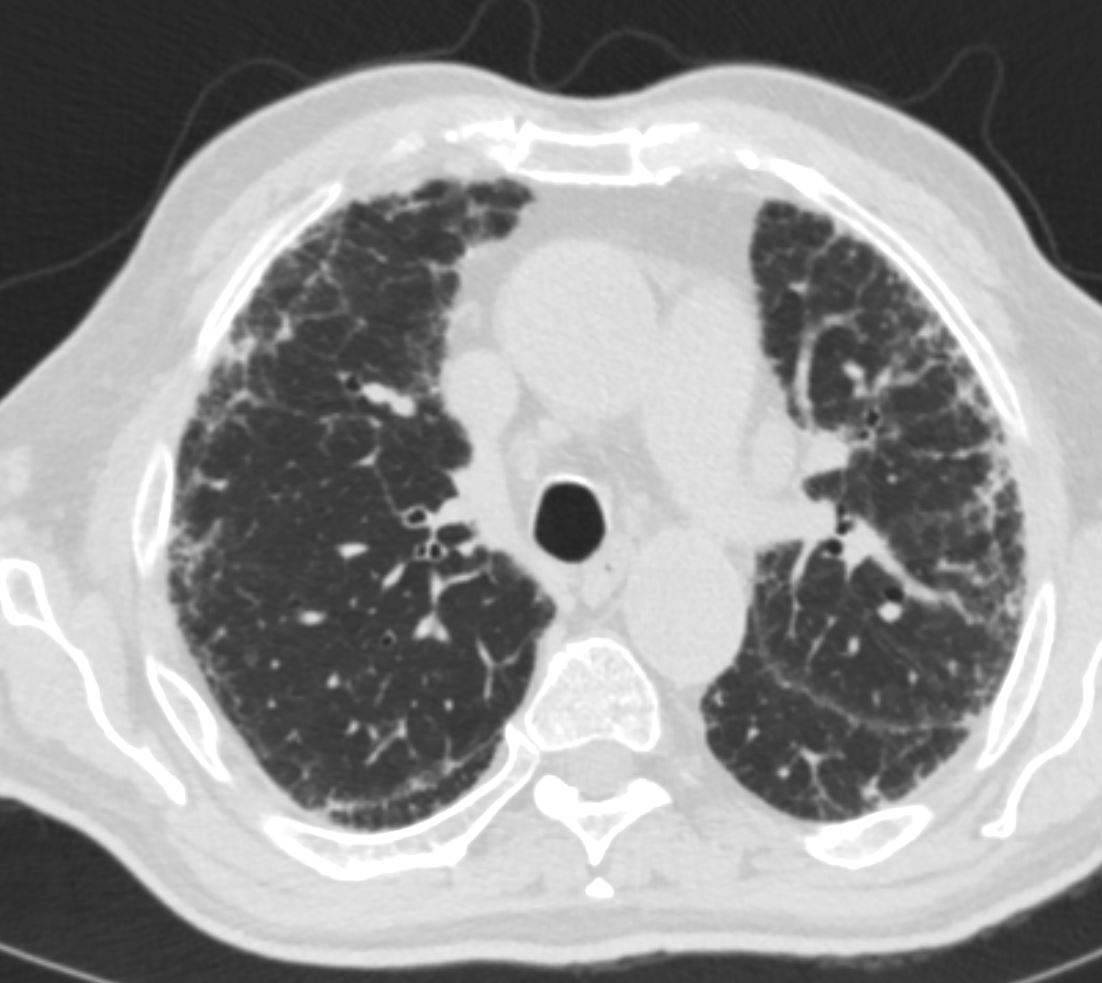
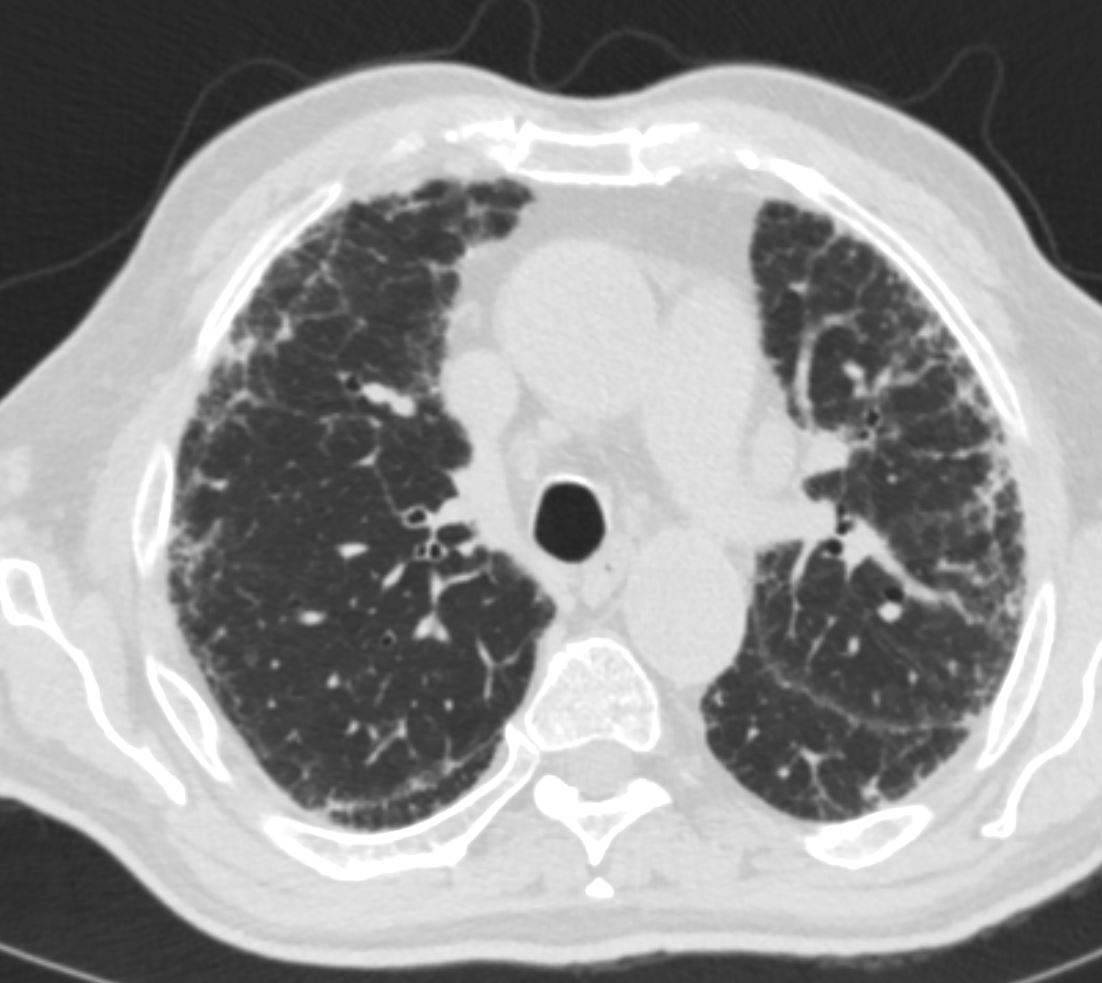
70 year old male with UIP showing extensive dominantly bibasilar and peripheral reticulation
Ashley Davidoff MD TheCommonVein.net uip-005


70 year old male with UIP showing extensive dominantly bibasilar and peripheral reticulation
Ashley Davidoff MD TheCommonVein.net uip-006
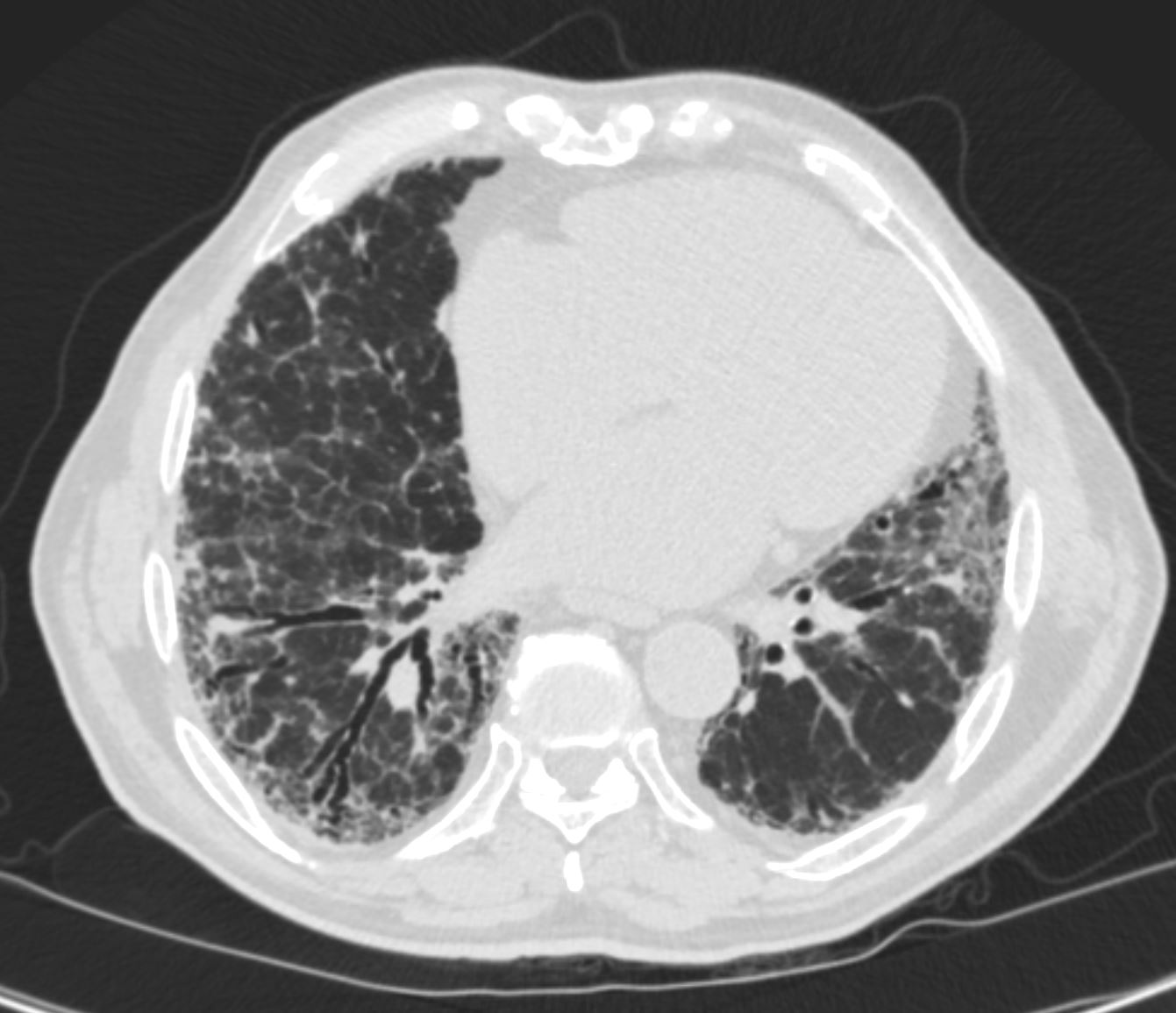
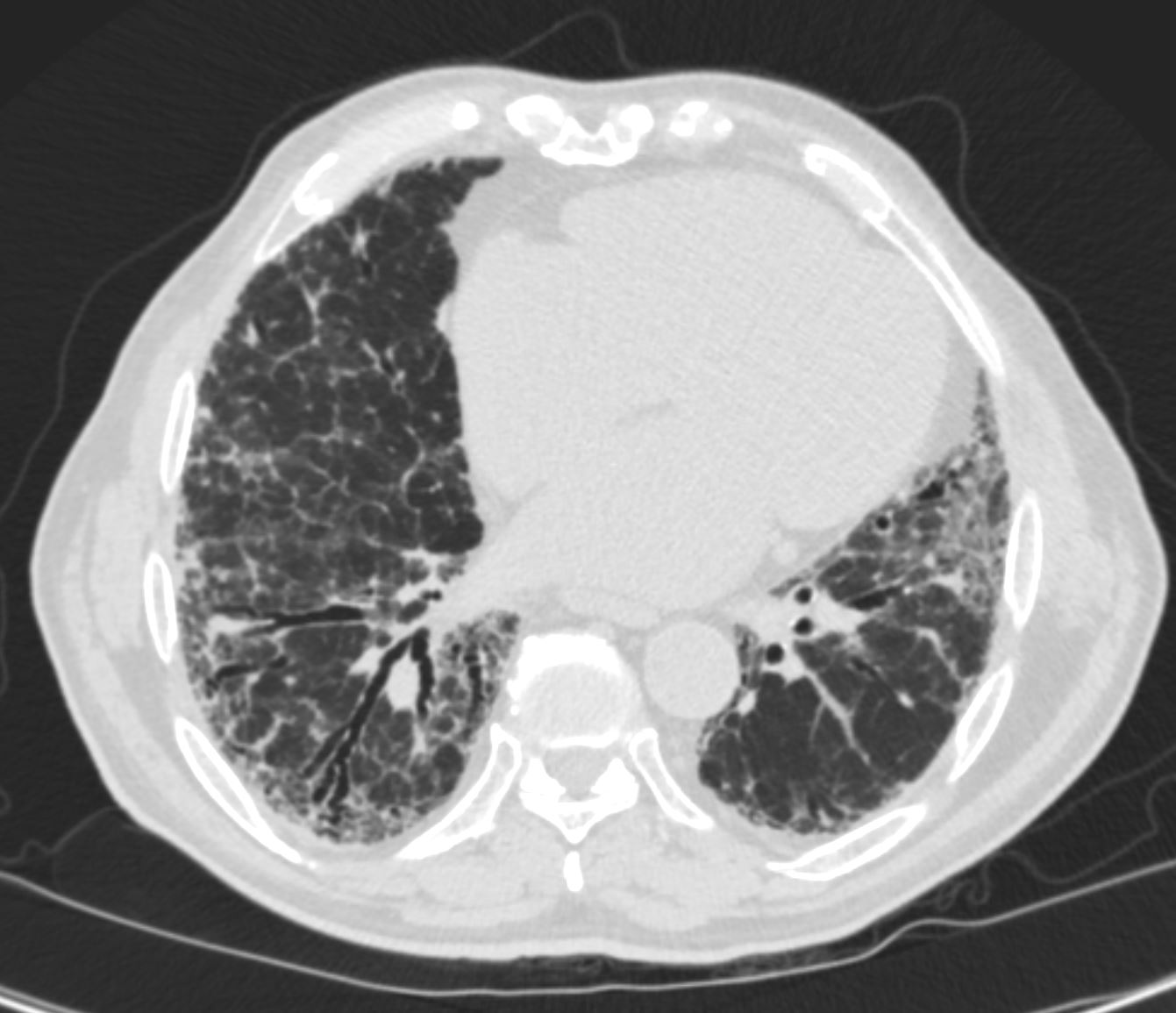
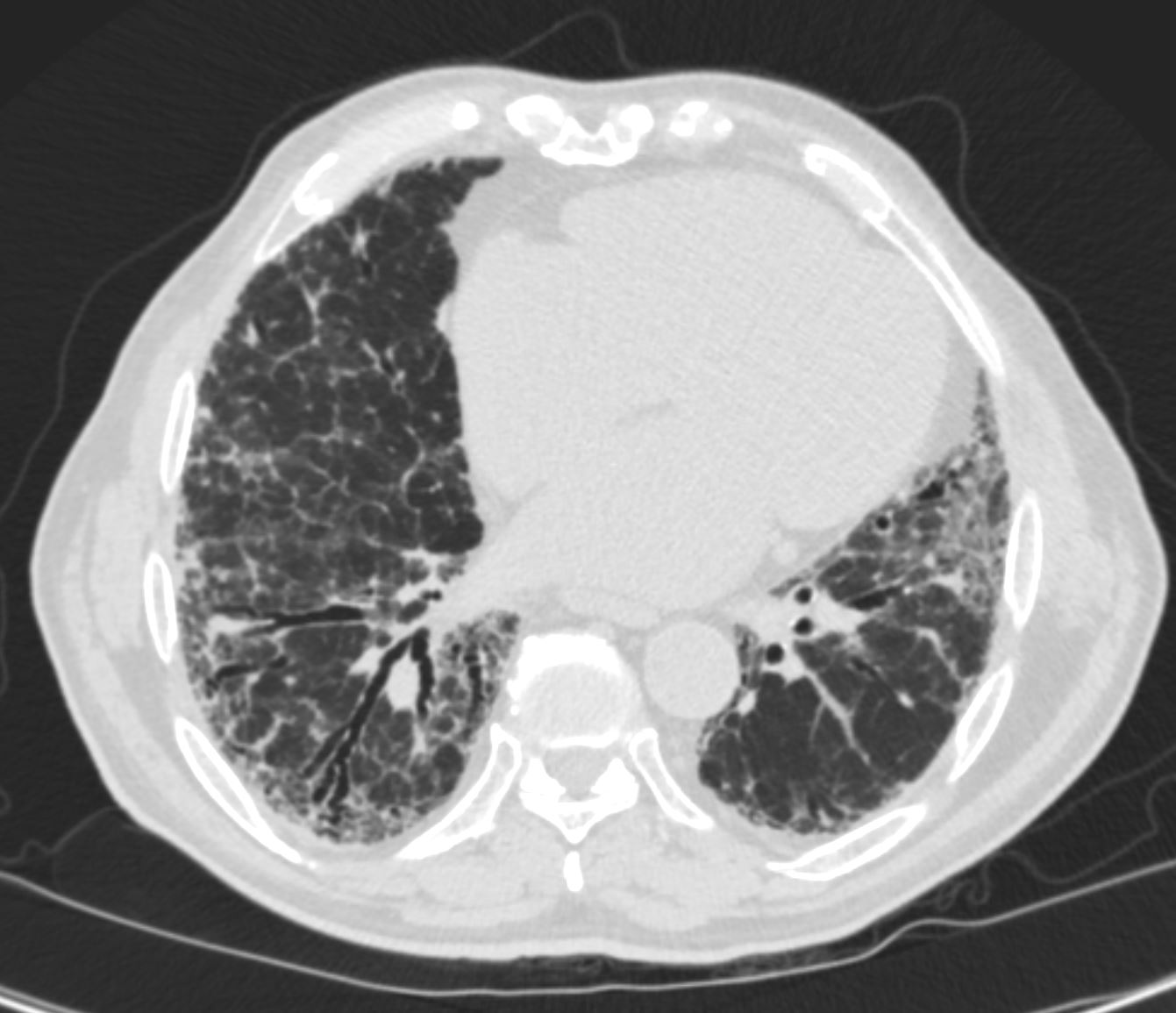
70 year old male with UIP showing extensive dominantly bibasilar and peripheral reticulation
Ashley Davidoff MD TheCommonVein.net uip-007
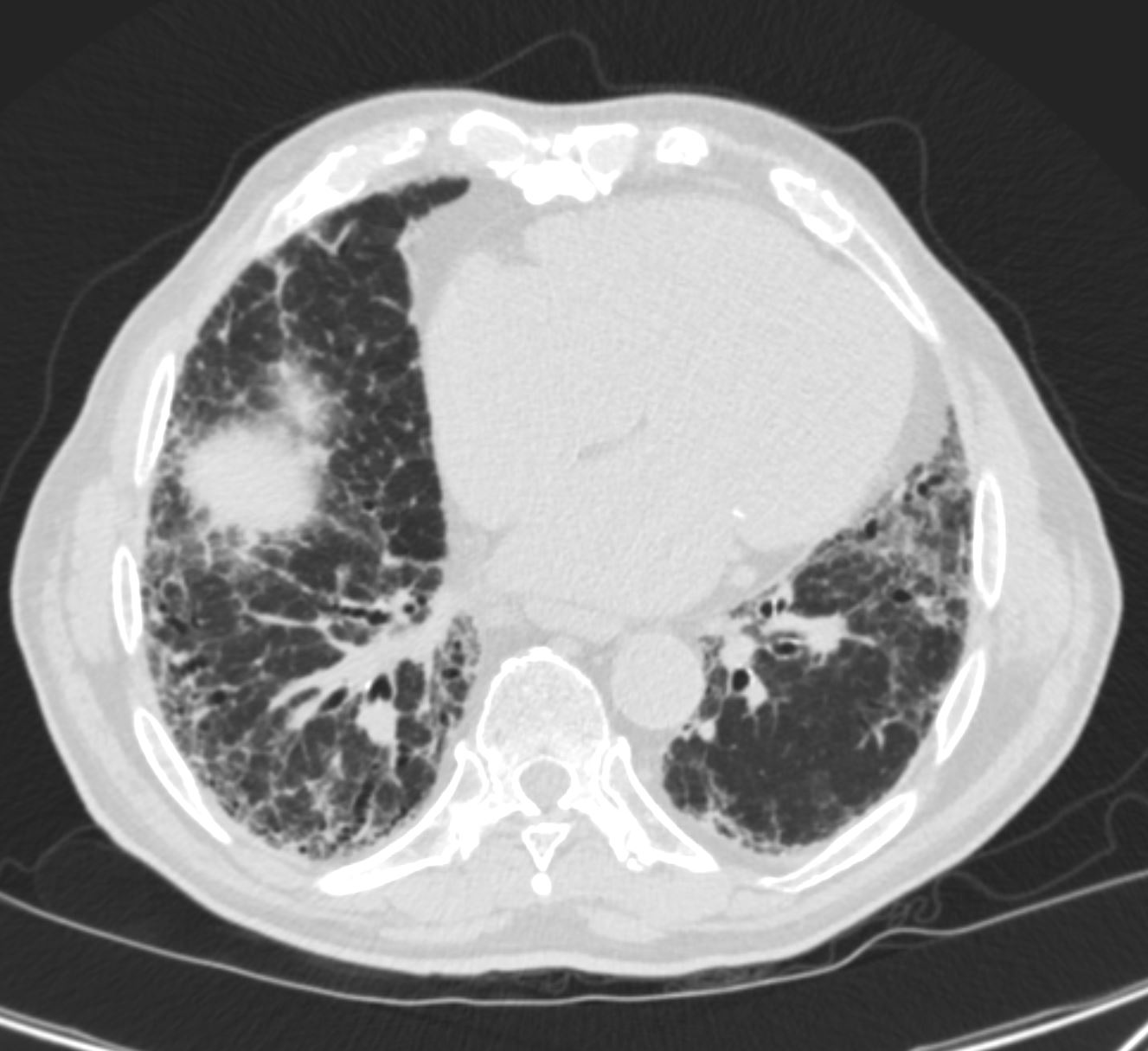
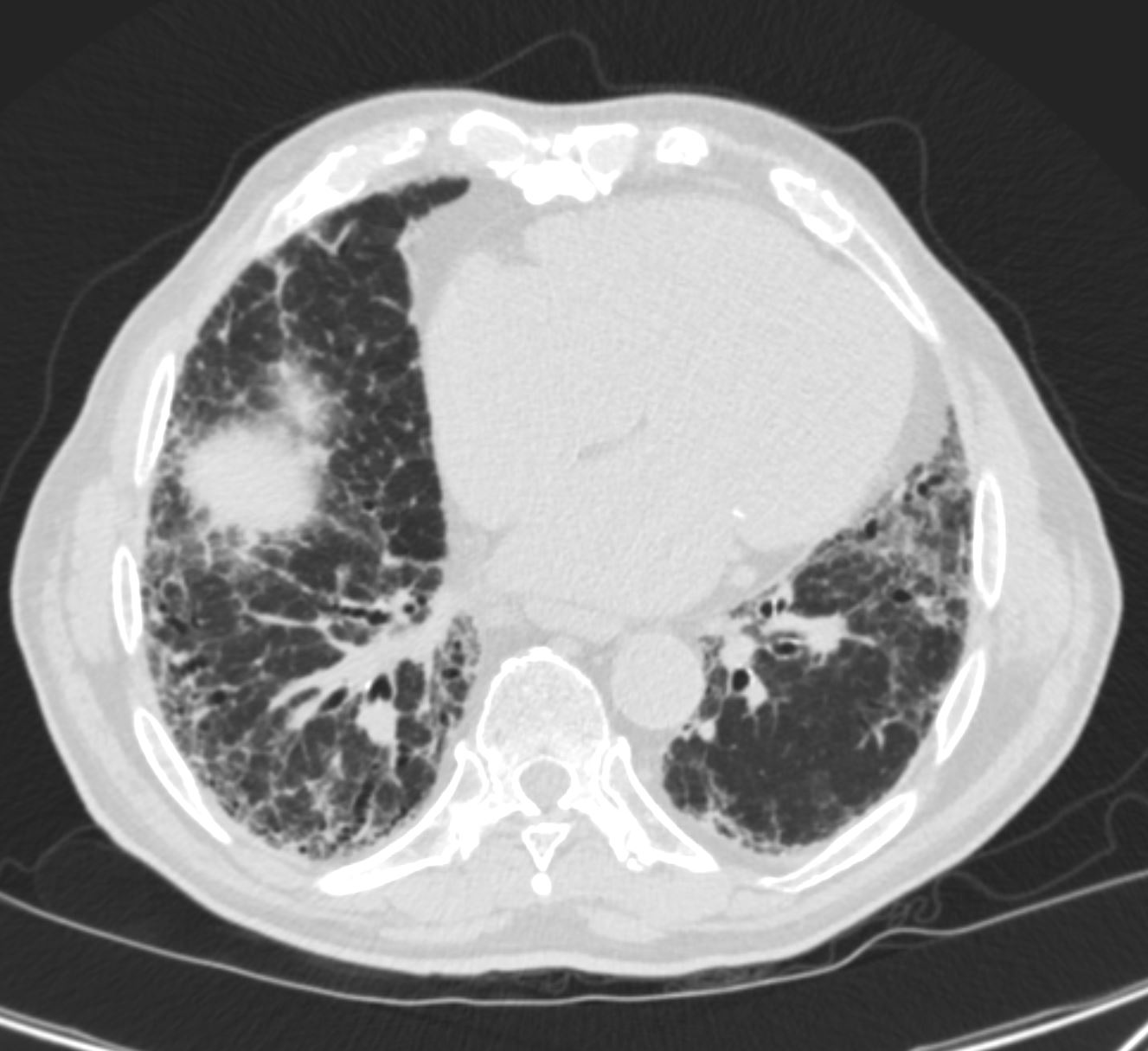
70 year old male with UIP showing extensive dominantly bibasilar and peripheral reticulation
Ashley Davidoff MD TheCommonVein.net uip-008
Honeycombing has prognostic significsnce
with median survival 2.1 years
without 5.8years
Accelerated Deterioration in IPF
Lung Cancer in UIP 5-10%
-
- INTERSTITIAL PNEUMONIA , IP
-
- Usual interstitial pneumonia (UIP)
- Nonspecific interstitial pneumonia (NSIP)
- Cryptogenic organizing pneumonia (COP)
- Desquamative interstitial pneumonia (DIP)
- Respiratory bronchiolitis-interstitial lung disease (RB-ILD)
- Acute interstitial pneumonia (AIP)
- Lymphoid interstitial pneumonia (LIP)
- Idiopathic pleuroparenchymal fibroelastosis (PPFE)
-
- INTERSTITIAL PNEUMONIA , IP
References and Links
UIP Wiki
Links and References
- Videos
- AUR
Title web link Current Guidelines in the Dx of UIP and IPF AUR Cardiothoracic Imaging
- AUR