- Mosaic attenuation is an
- imaging pattern
- variable lung attenuation
- results in a heterogeneous appearance of the parenchyma.
- sometimes it is caused by air trapping
- sometimes by perfusion abnormalities
- sometimes normal
- imaging pattern
Nutshell Buzz
patchwork
differing pulmonary attenuation
Etymology
Derived from the Greek word mosaic, meaning a pattern made of diverse or variegated components, and attenuation, referring to the reduction in the intensity of X-ray beams as they pass through tissues.
AKA
None commonly used.
What is it?
Mosaic attenuation is a radiologic pattern observed on high-resolution computed tomography (HRCT) of the chest. It describes regions of differing lung attenuation that form a patchwork appearance, with areas of increased attenuation (darker) and decreased attenuation (lighter).
Characterized by:
- Radiologic pattern:
- Decreased attenuation areas: Represent hypoperfused or hypoventilated lung tissue.
- Differentiating features:
- Sharp demarcation between high and low attenuation regions.
- Associated findings, such as air trapping on expiratory scans, are crucial for interpretation.
- Head cheese sign:
- Refers to a combination of mosaic attenuation, ground-glass opacities, and areas of normal lung, commonly seen in hypersensitivity pneumonitis.
- Radiologic pattern:
- Increased attenuation areas: Typically indicate abnormal lung parenchyma due to alveolar filling, interstitial thickening, or vascular engorgement.
- Decreased attenuation areas: Represent hypoperfused or hypoventilated lung tissue.
- Radiologic pattern:
- Refers to a combination of mosaic attenuation, ground-glass opacities, and areas of normal lung, commonly seen in hypersensitivity pneumonitis.
- Differentiating features:
- Sharp demarcation between high and low attenuation regions.
- Associated findings, such as air trapping on expiratory scans, are crucial for interpretation.
Caused by:
- Most common causes:
- Small airway diseases (e.g., bronchiolitis obliterans): Air trapping due to obstruction of small airways.
- Pulmonary vascular diseases: Patchy hypoperfusion secondary to vascular abnormalities (e.g., chronic thromboembolic pulmonary hypertension, vasculitis, or congestive heart failure (CHF)).
- Infections: Fungal or atypical pneumonias.
Congenital: Swyer-James syndrome (post-infectious bronchiolitis with unilateral air trapping).
Resulting in:
- Abnormal lung function due to localized or diffuse parenchymal or vascular abnormalities.
- Hypoxemia in severe cases due to ventilation-perfusion mismatch.
Structural changes:
- Alternating areas of normal, hyperinflated, or consolidated lung parenchyma.
- Redistribution of blood flow leading to patchy perfusion.
Pathophysiology:
- Small airway disease:
- Air trapping leads to overinflation of specific lung regions.
- Hypoventilated areas appear as decreased attenuation zones during inspiration and persist during expiration.
- Inspiratory-expiratory HRCT distinction: Persistent air trapping in decreased attenuation areas confirms small airway disease.
- Pulmonary vascular disease:
- Segmental or subsegmental hypoperfusion creates areas of low attenuation, particularly in chronic thromboembolic pulmonary hypertension.
- Inspiratory-expiratory HRCT distinction: Mosaic attenuation disappears on expiration as perfusion equilibrates.
- Small airway disease:
- Air trapping leads to overinflation of specific lung regions.
- Hypoventilated areas appear as decreased attenuation zones during inspiration and persist during expiration.
- Pulmonary vascular disease:
- Segmental or subsegmental hypoperfusion creates areas of low attenuation, particularly in chronic thromboembolic pulmonary hypertension CHF.
Pathology:
- Histopathological findings depend on the underlying etiology:
- Small airway diseases: Fibrosis or inflammation of terminal and respiratory bronchioles.
- Vascular diseases: Occlusion or stenosis of pulmonary arteries CHF.
Diagnosis:
- Clinical correlation:
- Symptoms: Dyspnea, cough, or signs of chronic lung disease.
- History of occupational exposure, recurrent infections, or autoimmune disorders.
- Imaging:
- HRCT is the gold standard:
- Inspiratory and expiratory imaging is essential to evaluate for air trapping.
- Heterogeneous attenuation pattern with well-demarcated regions.
- Ventilation-perfusion (V/Q) scan:
- Patchy perfusion defects support pulmonary vascular involvement.
- HRCT is the gold standard:
- Pulmonary function tests (PFTs):
- May show obstructive or restrictive patterns, depending on the etiology.
Management:
- Underlying cause treatment:
- Small airway disease: Bronchodilators, corticosteroids, or immunosuppressants.
- Pulmonary vascular disease: Anticoagulation or pulmonary vasodilators.
- Supportive therapy:
- Oxygen therapy for hypoxemia.
- Pulmonary rehabilitation for functional improvement.
Radiology Detail:
- CXR:
- Poor sensitivity; may show non-specific patchy opacities.
- CT:
- Parts: Heterogeneous lung parenchyma with alternating areas of attenuation.
- Size: Patchy, segmental, or diffuse involvement.
- Shape: Sharp demarcations between affected and normal lung regions.
- Position: Random distribution or segmental pattern.
- Character:
- Low attenuation: Air trapping (small airways or vascular hypoperfusion).
- High attenuation: Consolidation, interstitial thickening, or alveolar filling.
- Time: Persistent pattern, though can evolve with treatment.
- Associated Findings: Air trapping on expiratory CT, traction bronchiectasis in ILDs.
- Other relevant Imaging Modalities:
- V/Q scans: Helpful for pulmonary vascular disease.
- MRI: Rarely used but can assess pulmonary perfusion.
Pulmonary Function Tests (PFTs):
- Obstructive pattern in small airway disease.
- Restrictive pattern in interstitial lung disease.
Recommendations:
- Perform HRCT with inspiratory and expiratory phases to confirm air trapping.
- Correlate imaging findings with clinical history and PFTs.
- Consider multidisciplinary evaluation for complex cases (pulmonologist, radiologist, and pathologist).
Key Points and Pearls:
- Mosaic attenuation is a descriptive HRCT finding, not a diagnosis.
- Differentiation between small airway, vascular, and interstitial causes requires clinical and radiologic correlation.
- Expiratory imaging is critical for identifying air trapping in small airway diseases, where mosaic attenuation persists during expiration.
- In pulmonary vascular diseases, mosaic attenuation reflects patchy perfusion defects that disappear on expiration.
- The head cheese sign is a hallmark finding in certain interstitial lung diseases, such as hypersensitivity pneumonitis.
- Mosaic attenuation is a descriptive HRCT finding, not a diagnosis.
- Differentiation between small airway, vascular, and interstitial causes requires clinical and radiologic correlation.
- Expiratory imaging is critical for identifying air trapping in small airway diseases.
- In pulmonary vascular diseases, mosaic attenuation reflects patchy perfusion defects.
Follicular Bronchiolitis,
Mosaic Attenuation, Air Trapping
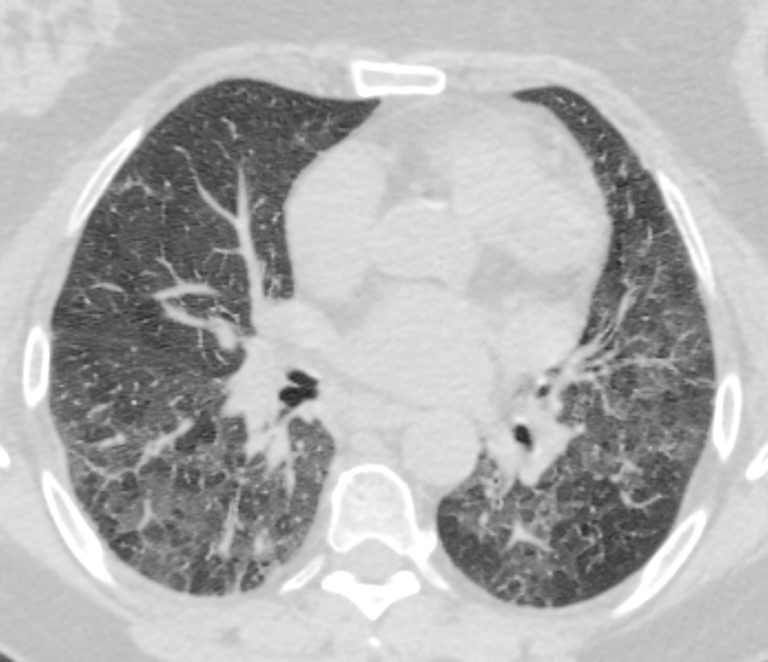
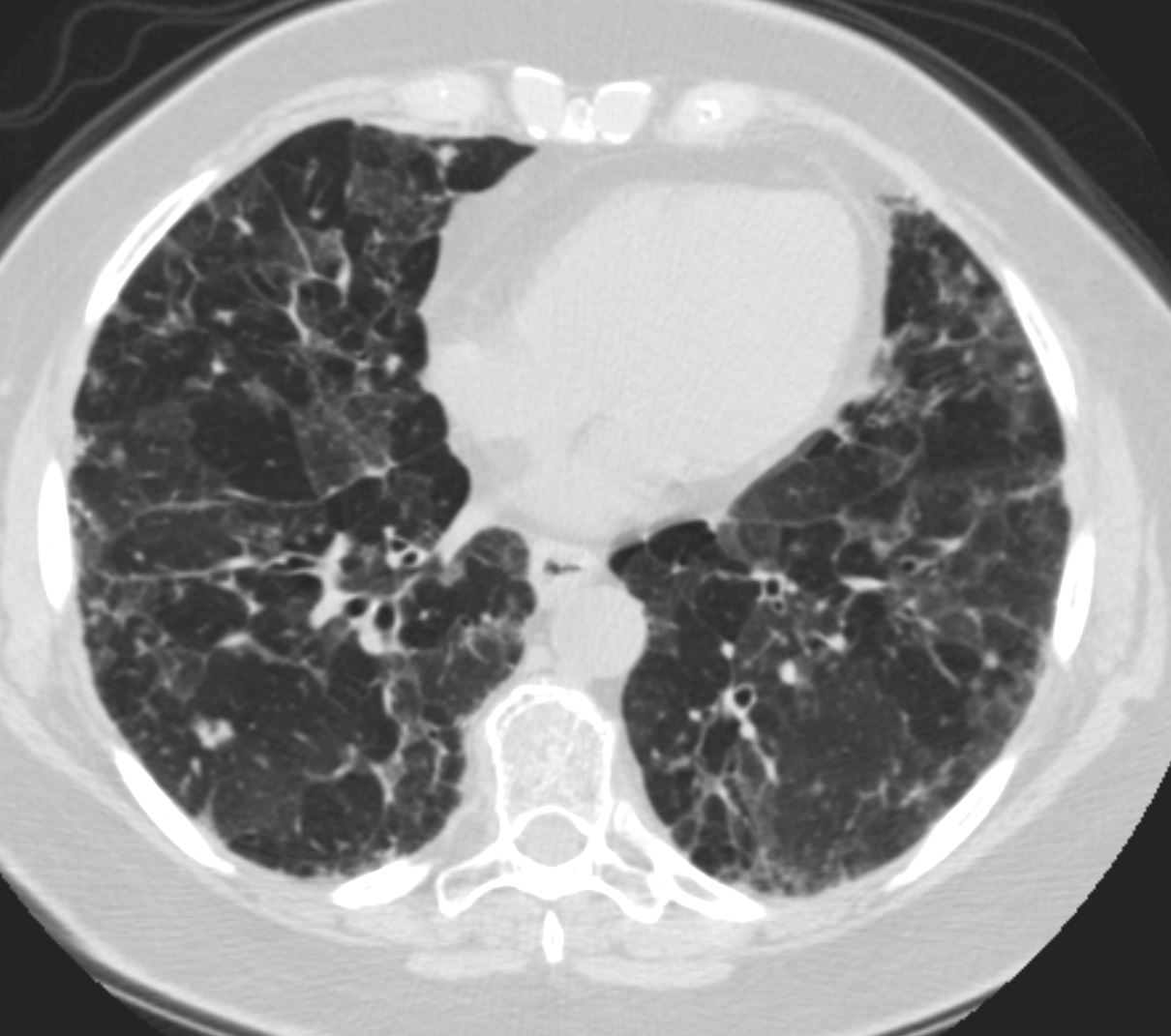
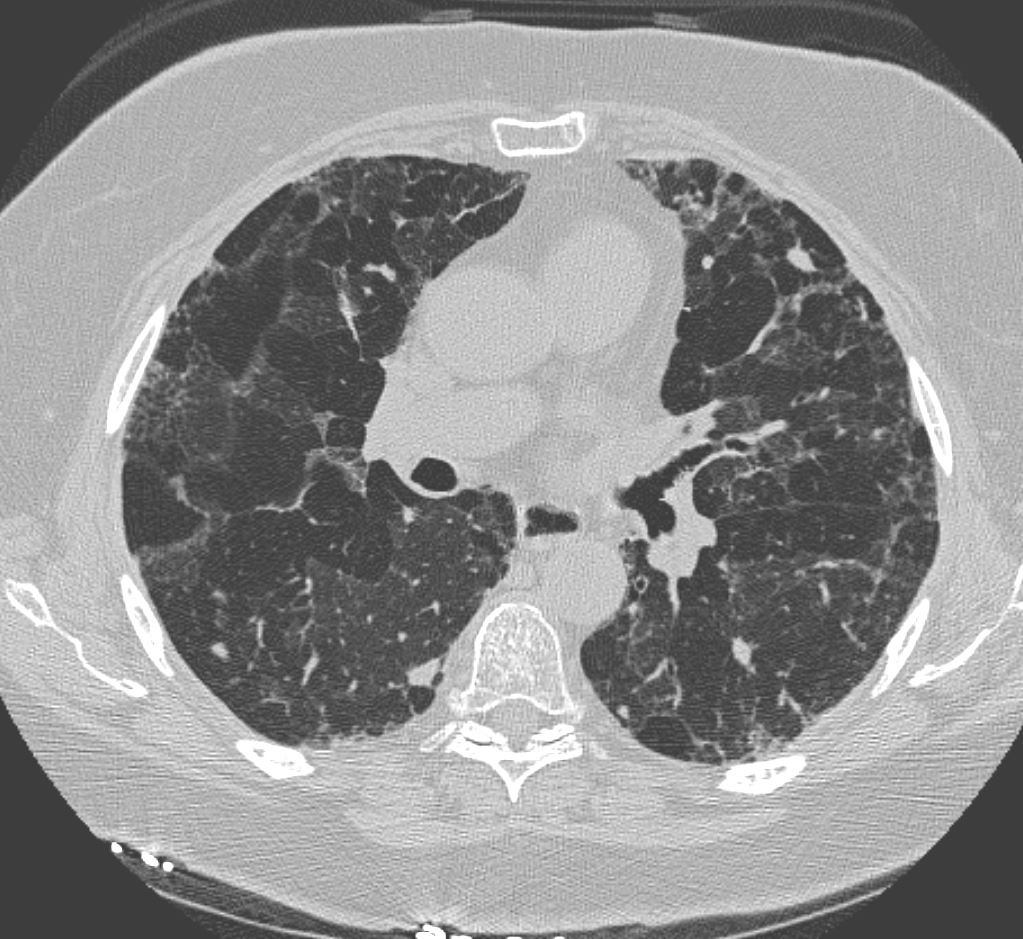
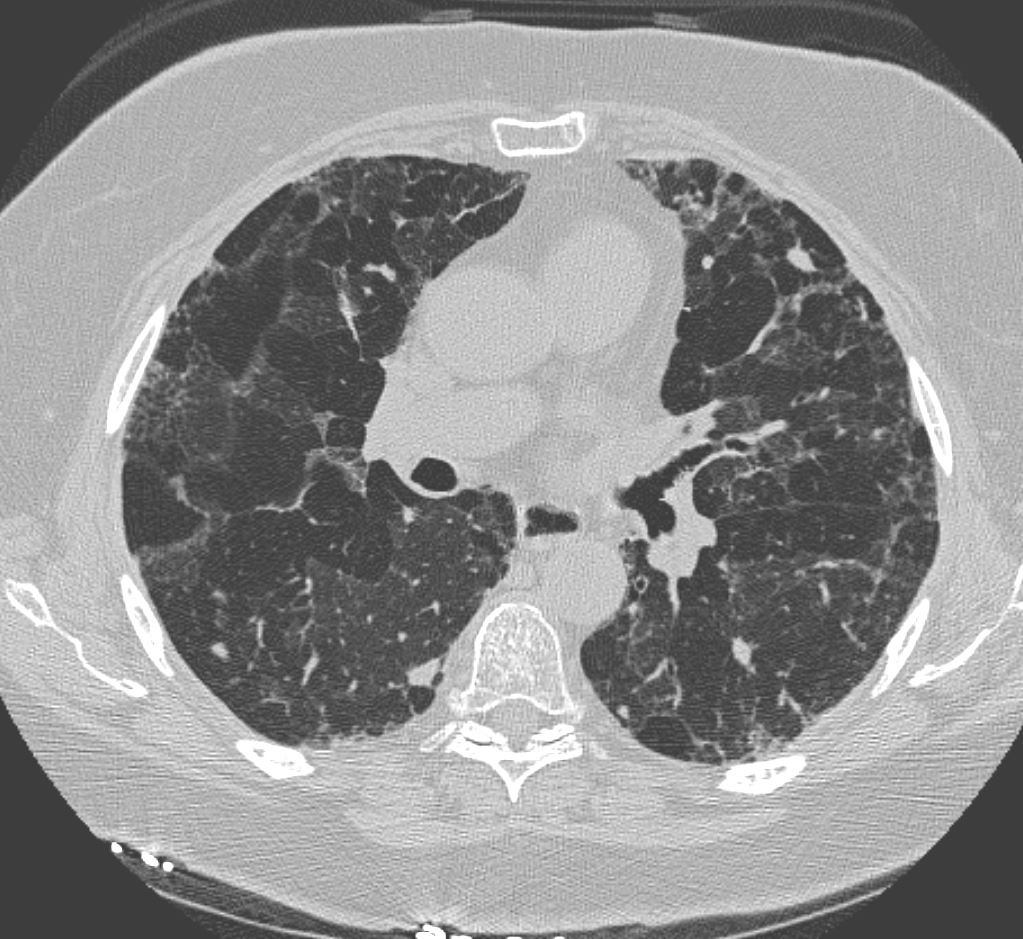
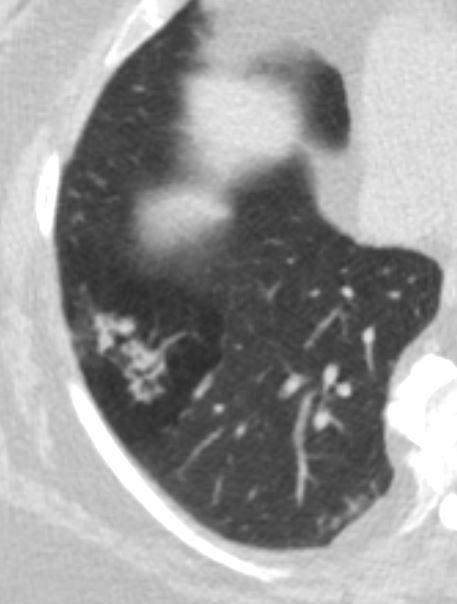
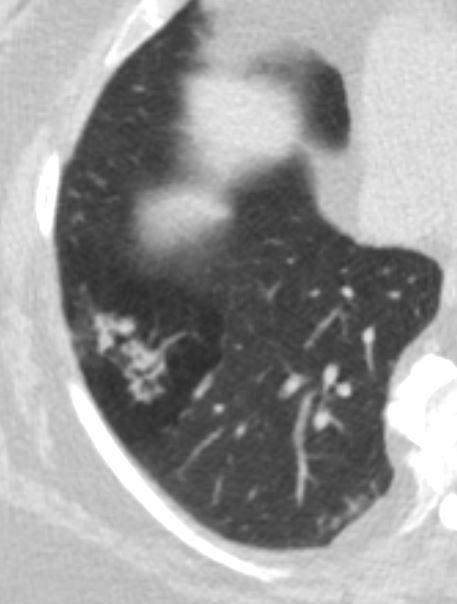
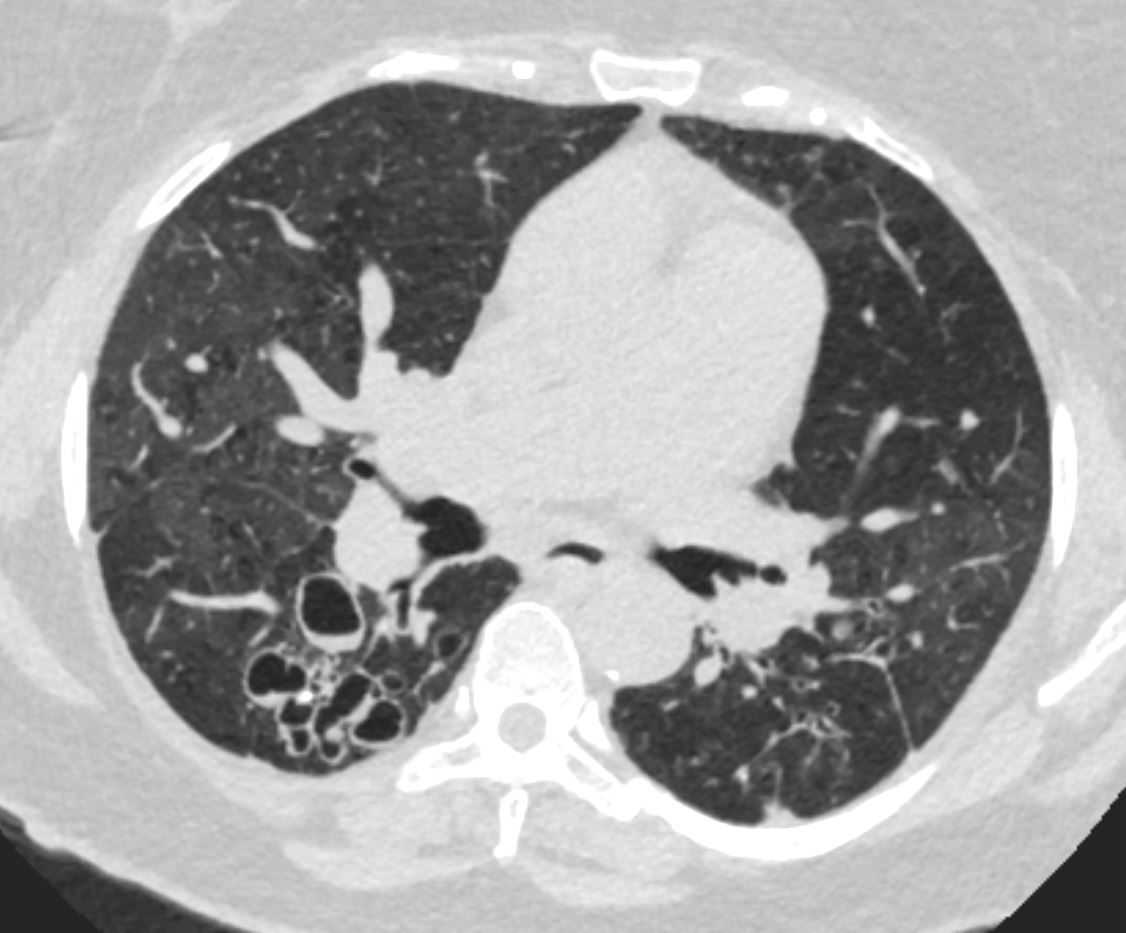
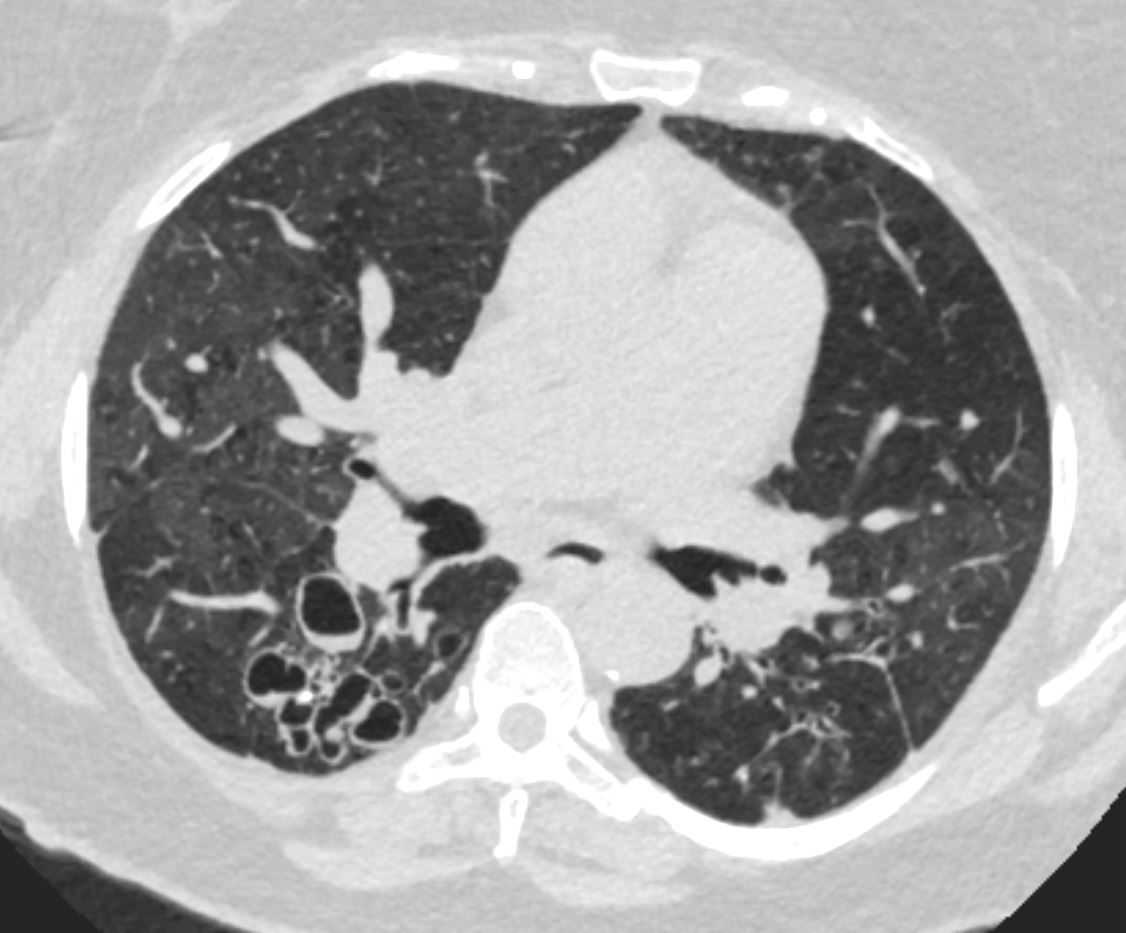
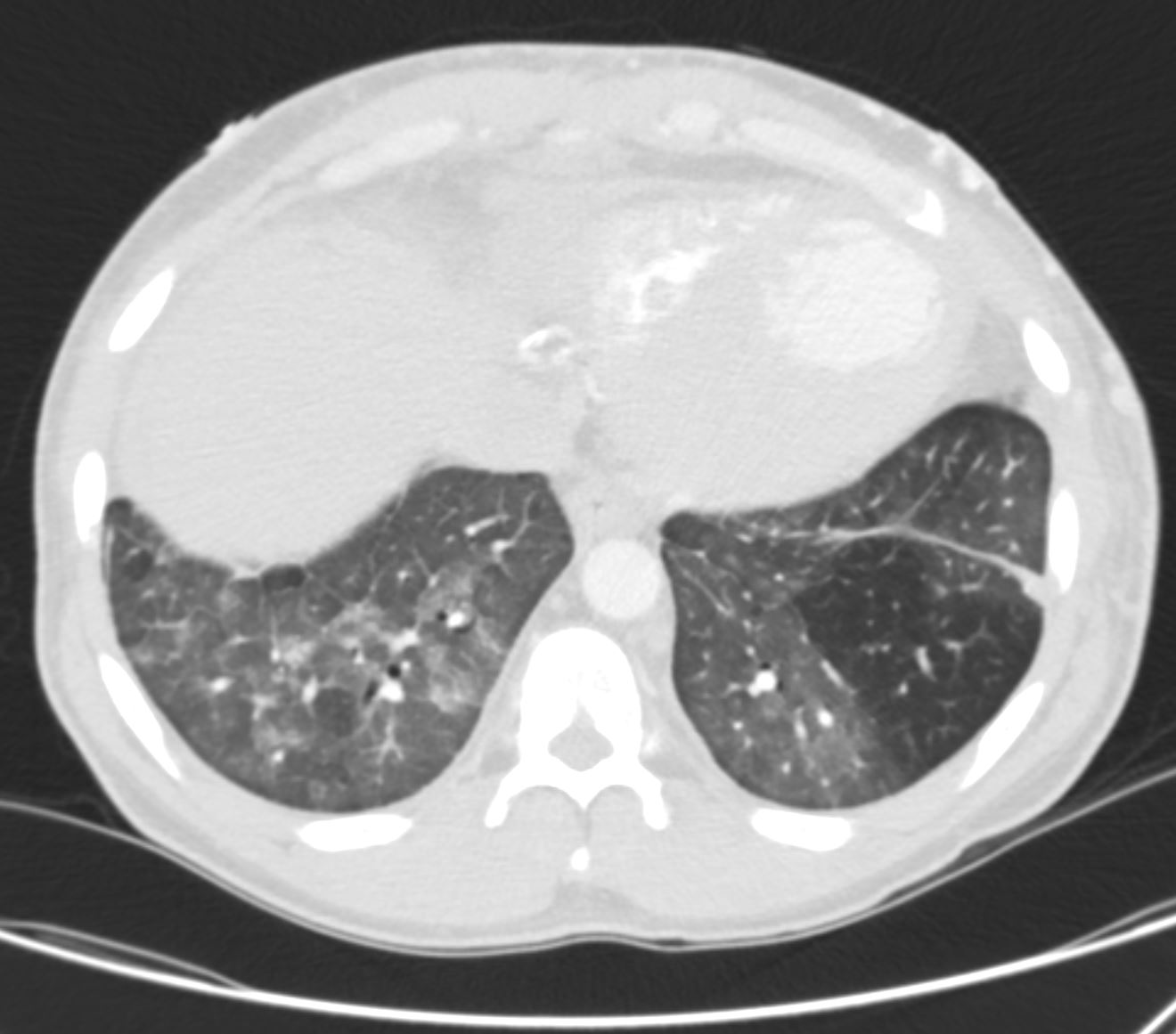
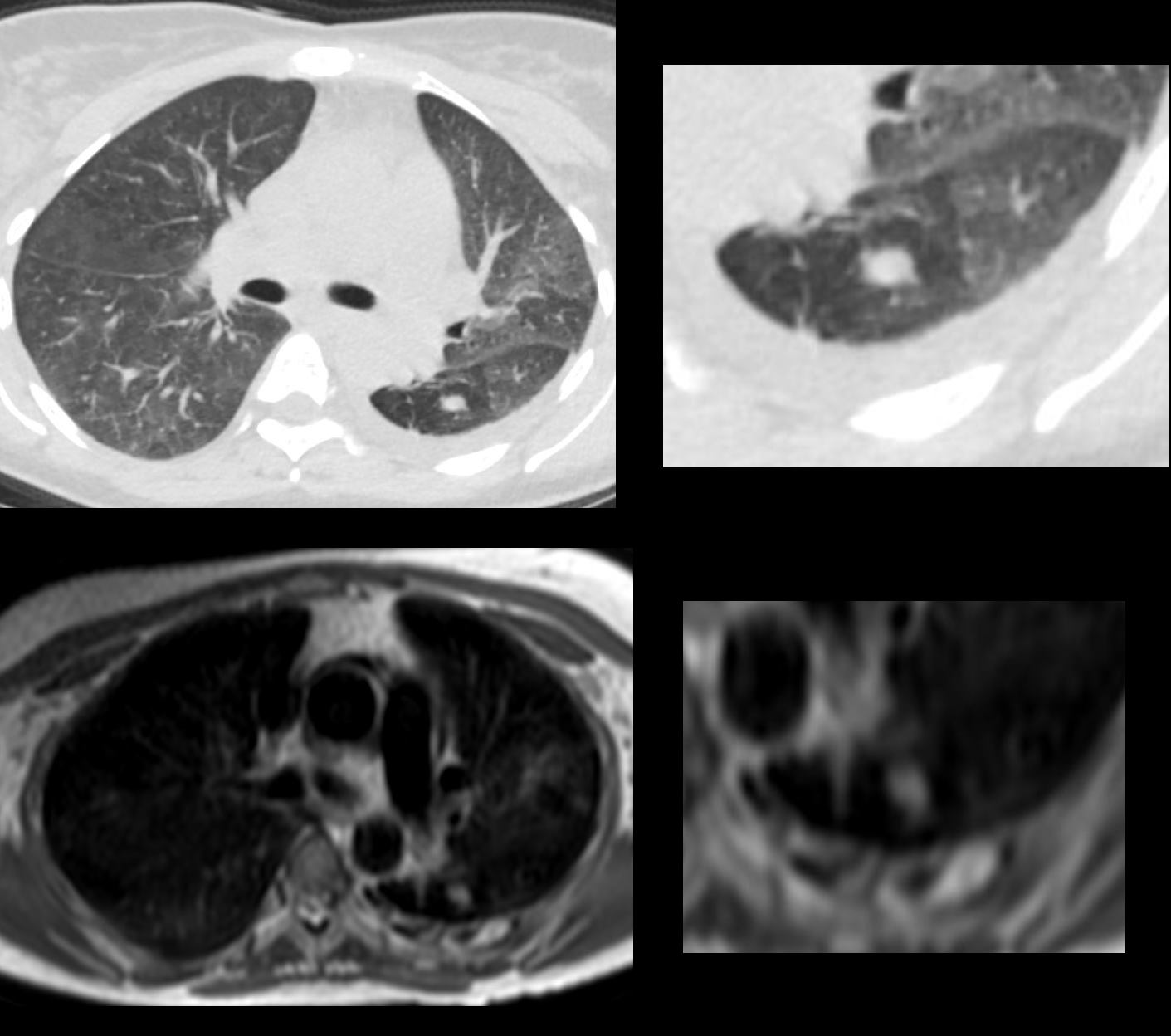
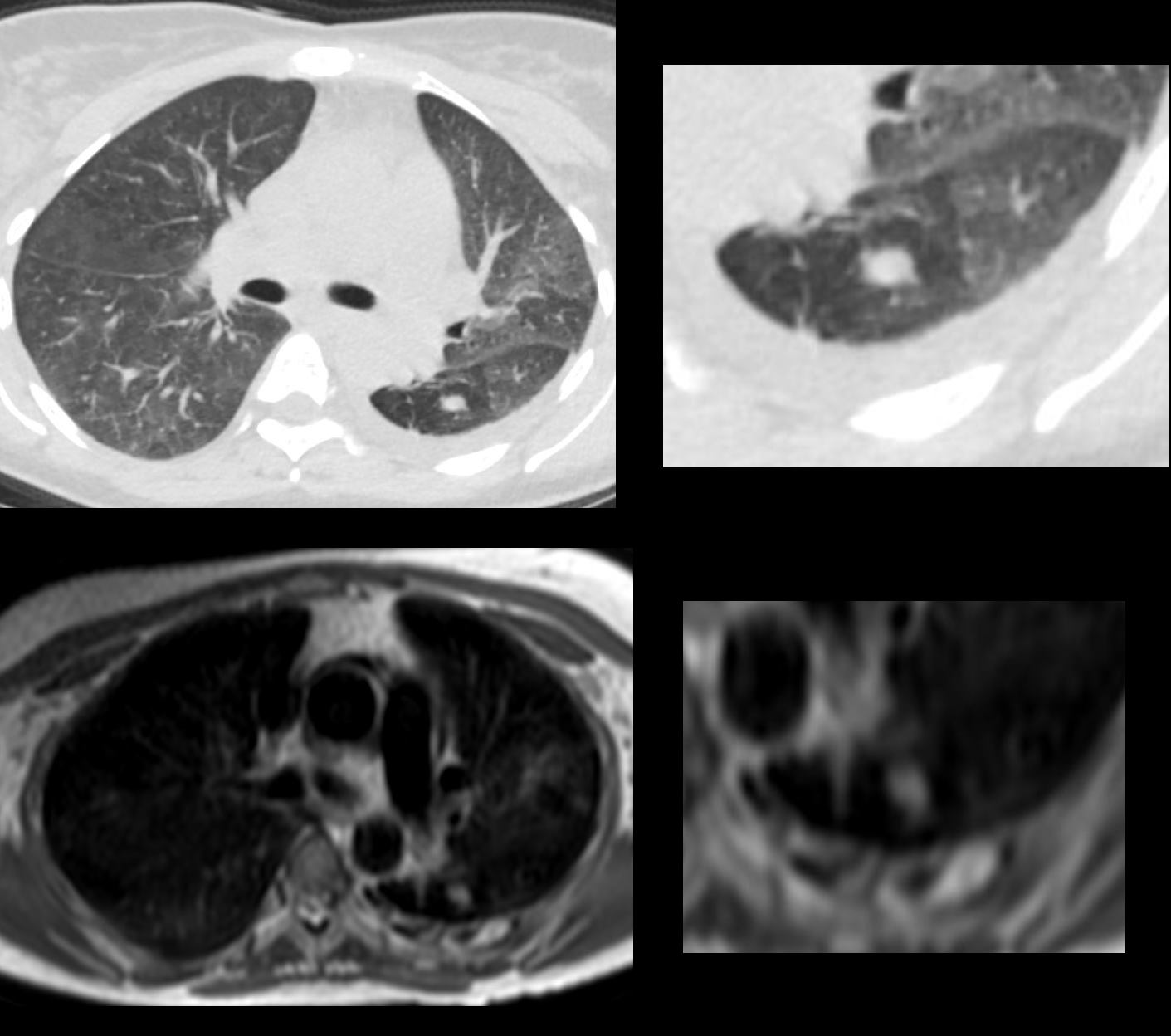
70-year-old female former smoker with long standing history of RA presents with chronic dyspnea.
Axial CT of the chest at the level of the lower lung fields reveals centrilobular nodules, ground-glass opacities, and mosaic attenuation (likely due to air trapping in this context). In the context of a patient with rheumatoid arthritis a diagnosis of follicular bronchiolitis is likely. However radiologically fibrotic hypersensitivity pneumonitis (HP) is included in the differential diagnosis
Ashley Davidoff MD TheCommonVein.net 132Lu 136657
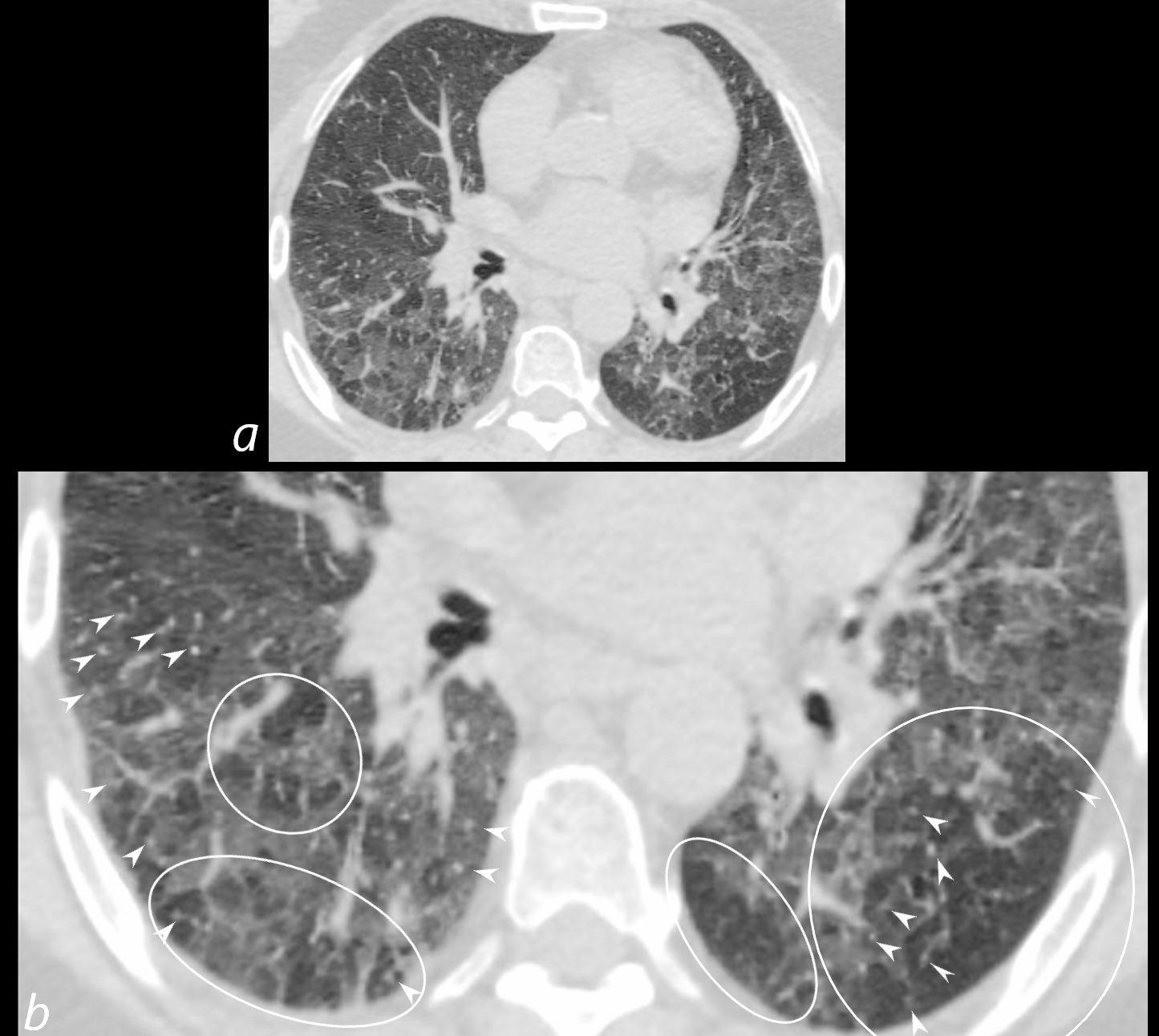
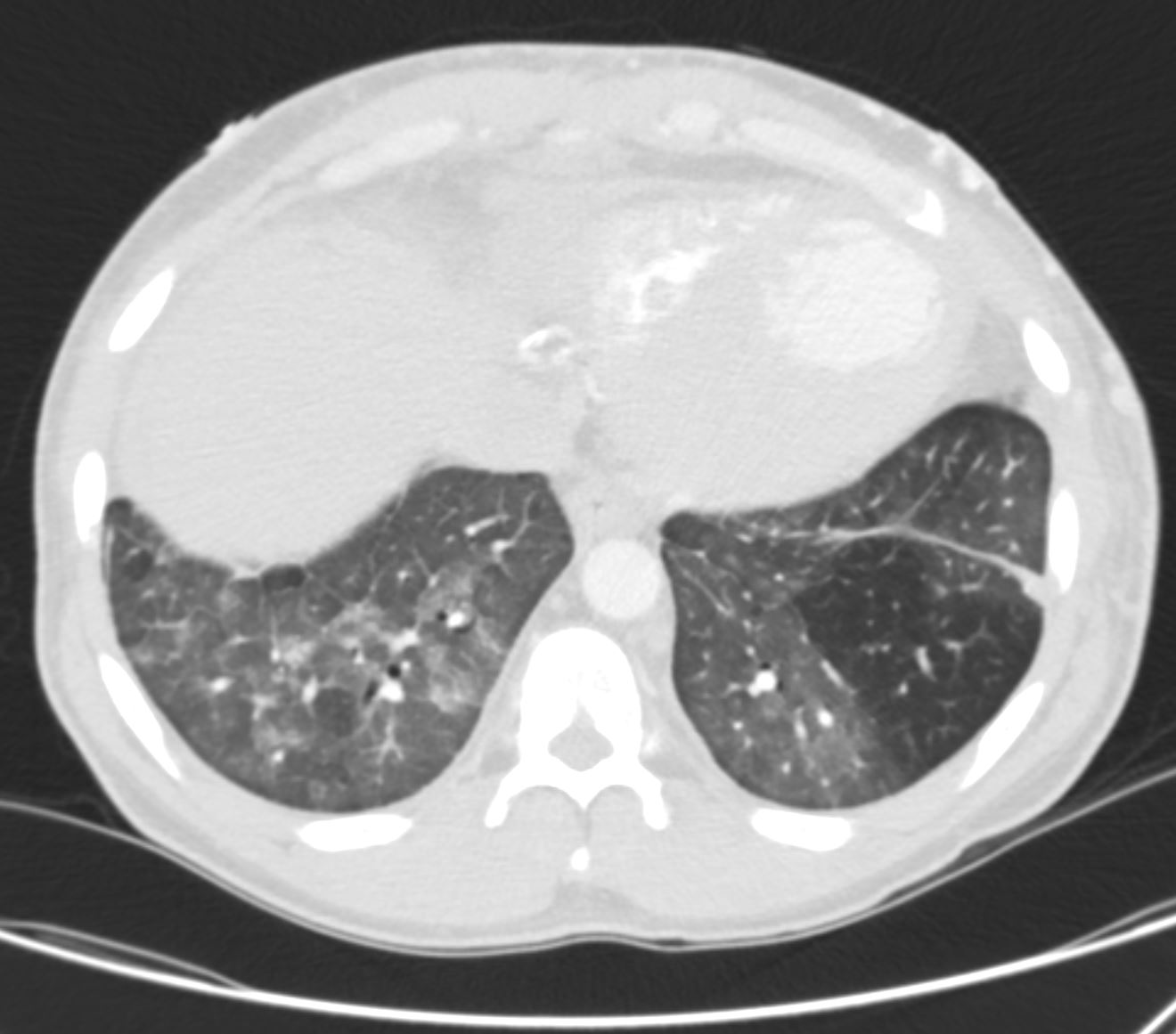
70-year-old female former smoker with long standing history of RA presents with chronic dyspnea.
Axial CT of the chest at the level of the lower lung fields reveals centrilobular nodules (b white arrowheads), ground-glass opacities, and mosaic attenuation (b, white rings) likely due to air trapping in this context.
In the context of a patient with rheumatoid arthritis a diagnosis of follicular bronchiolitis is likely. However radiologically fibrotic hypersensitivity pneumonitis (HP) is included in the differential diagnosis
Ashley Davidoff MD TheCommonVein.net 132Lu 136657cL
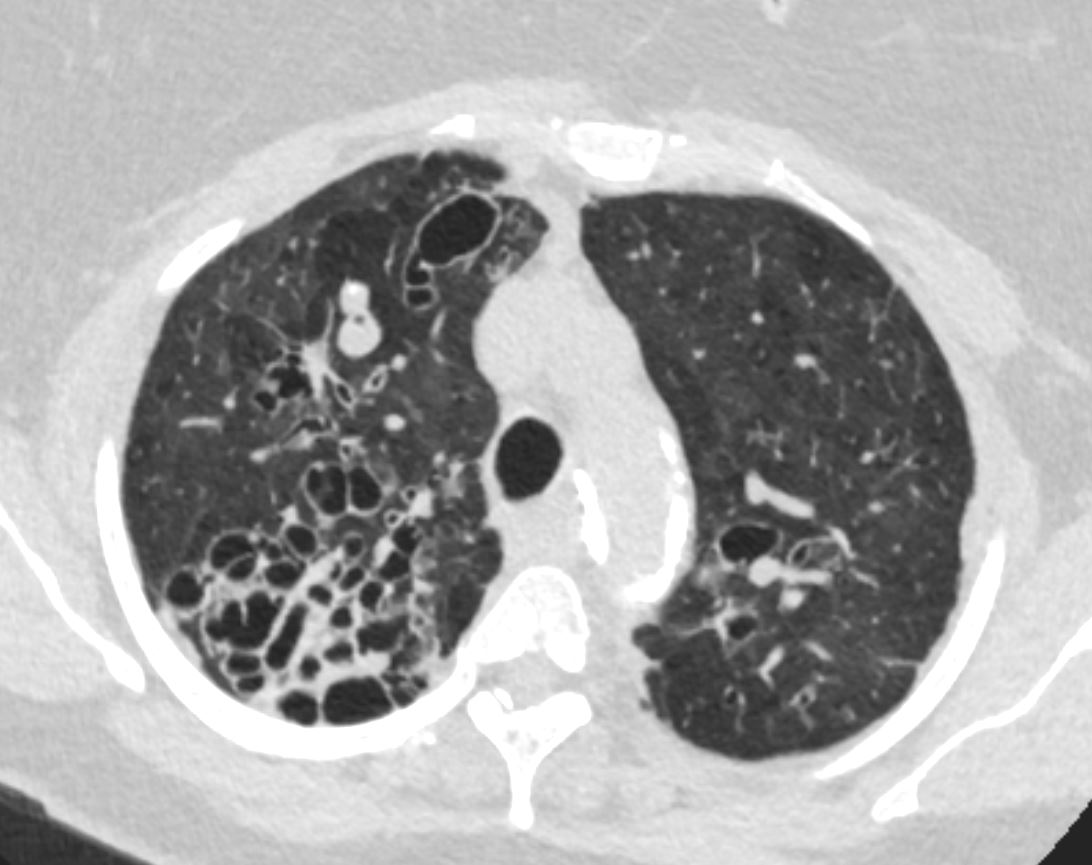
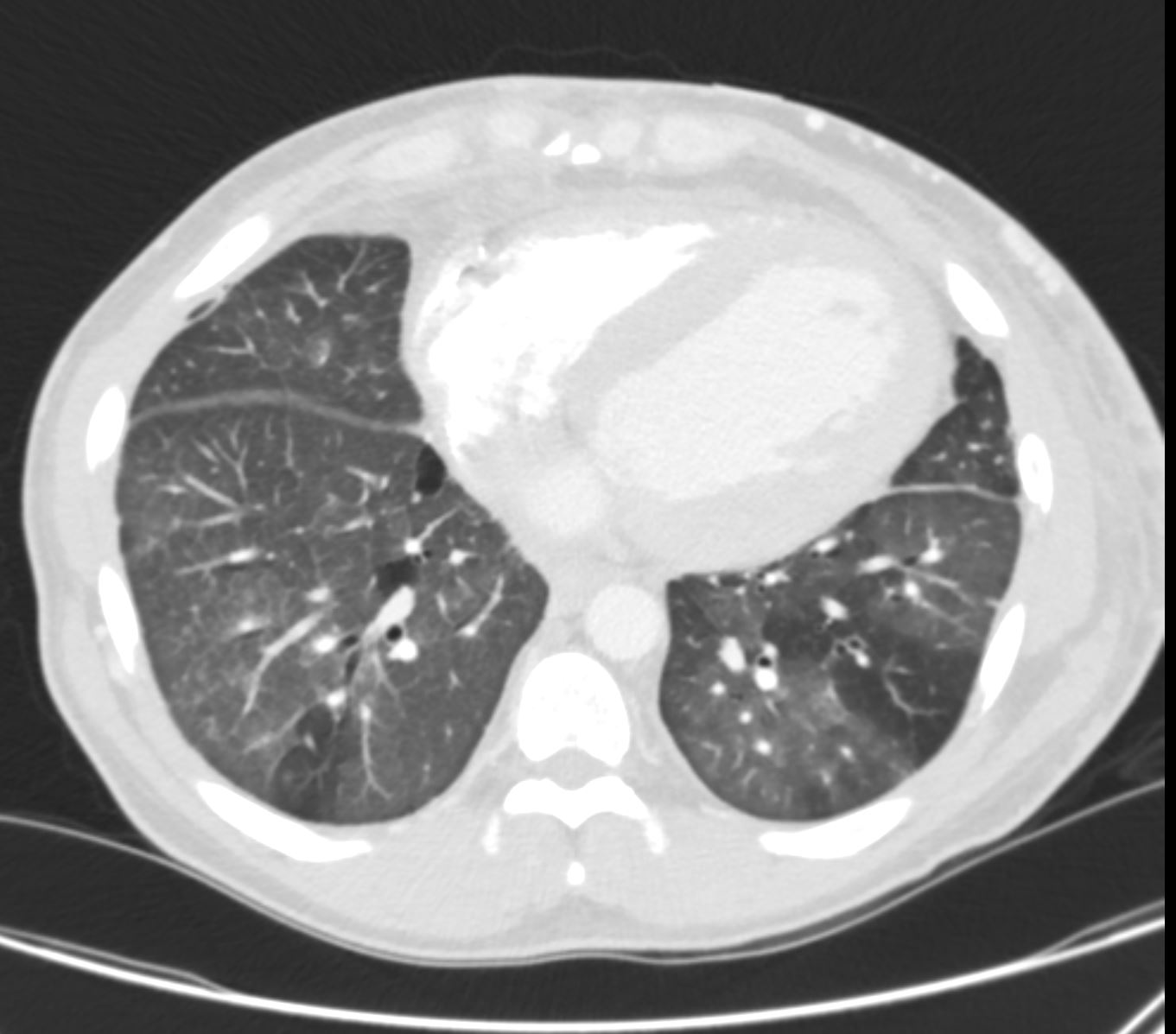
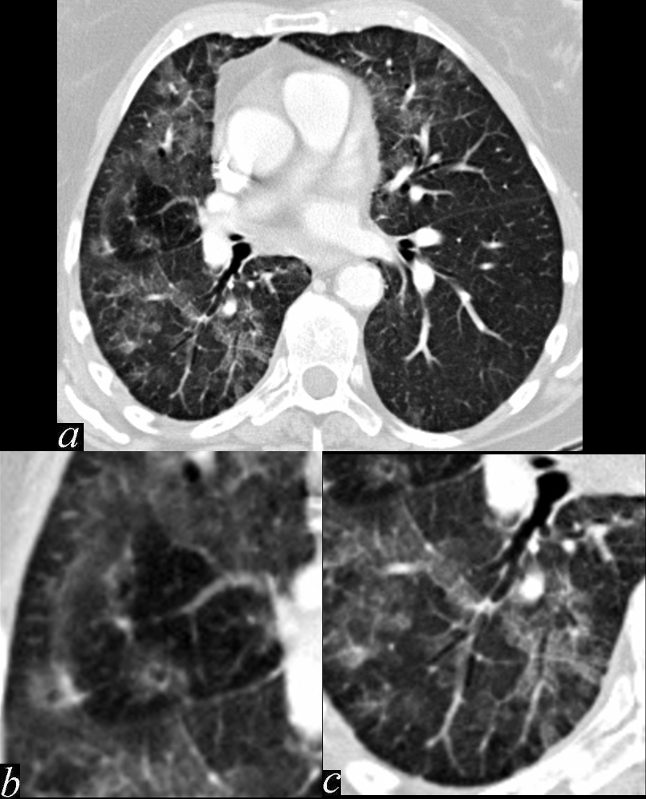
Inspiration Expiration to
Distinguish Between
Small Airway Disease and Small Blood Vessel Disease
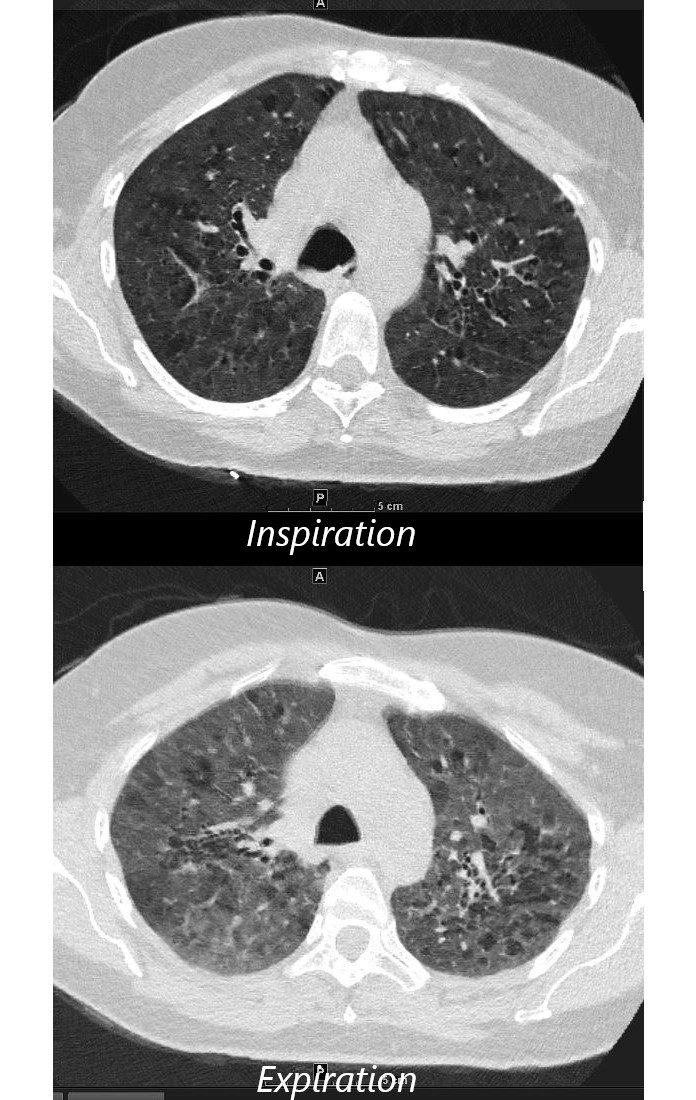
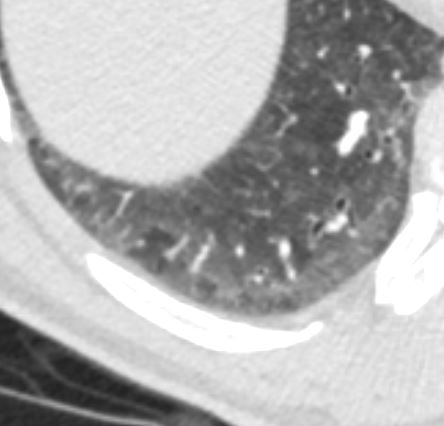
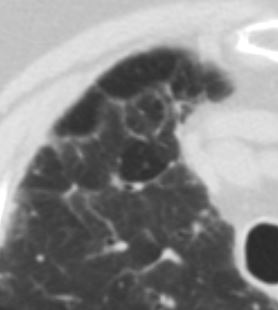
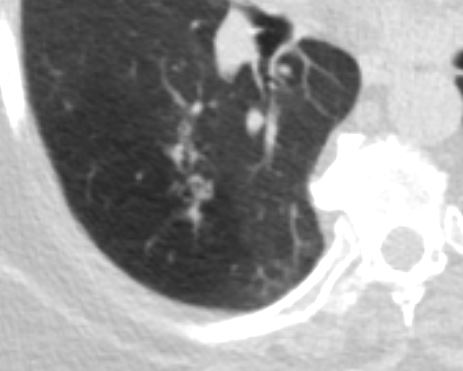
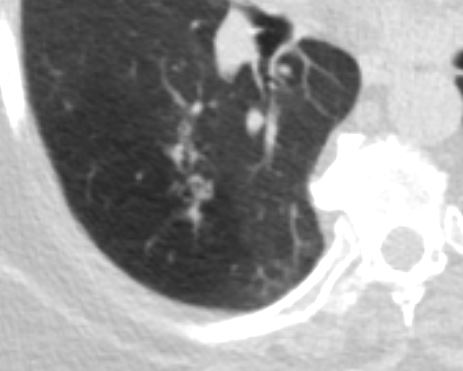
55-year-old female with shortness of breath. She keeps birds for pets Axial CT through the mid lung fields on inspiration, shows diffuse ground glass changes with a combination of mosaic attenuation and normal lung giving the appearance of the head cheese sign.
On the expiration phase the mosaic attenuation remains indicating air trapping and inferring small airway disease
Ashley Davidoff MD TheCommonVein.net 242Lu 13551aL
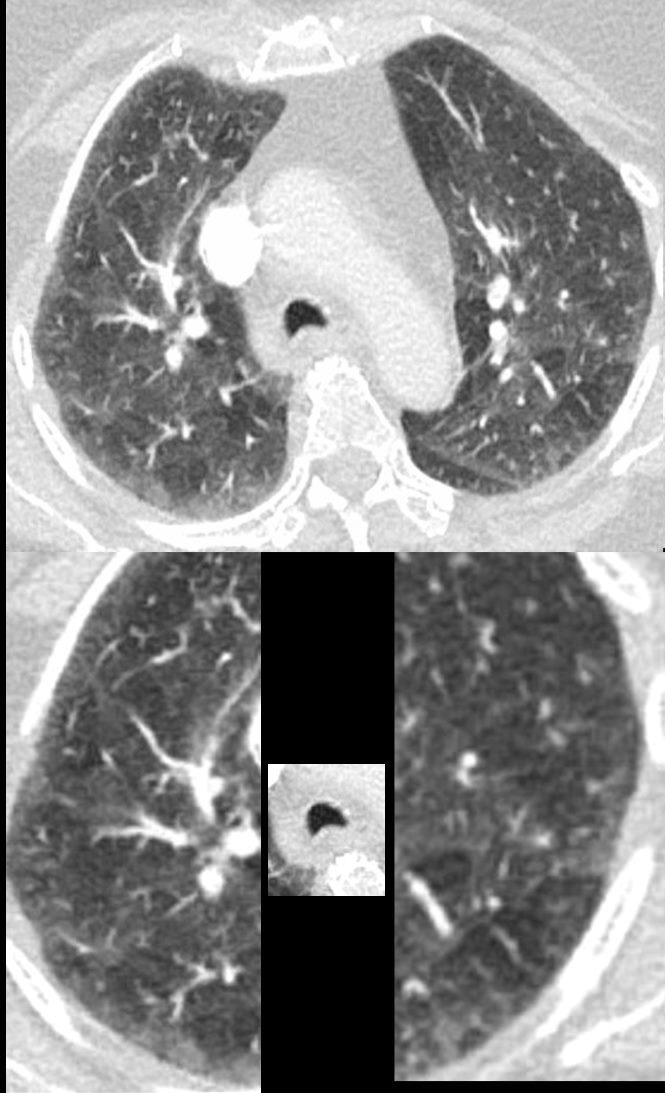
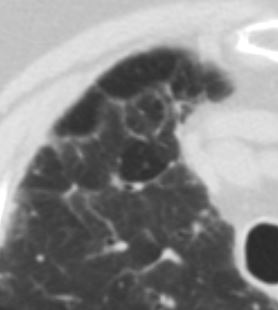
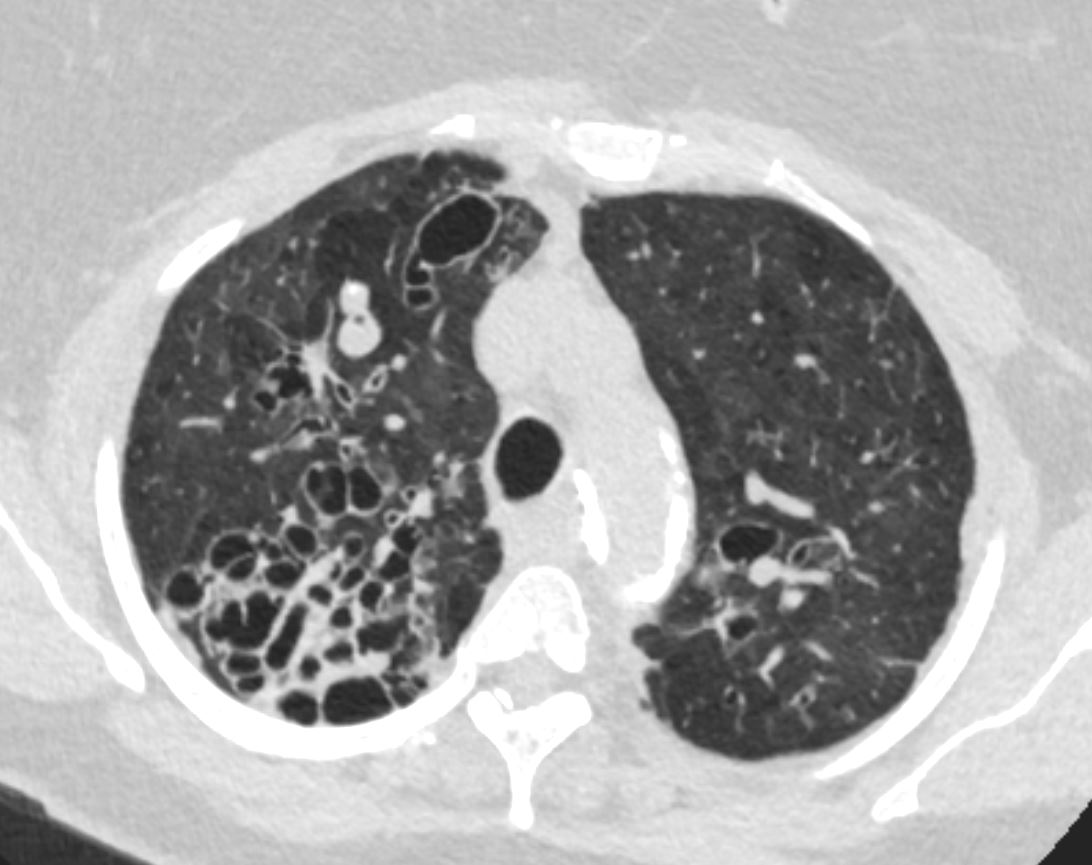
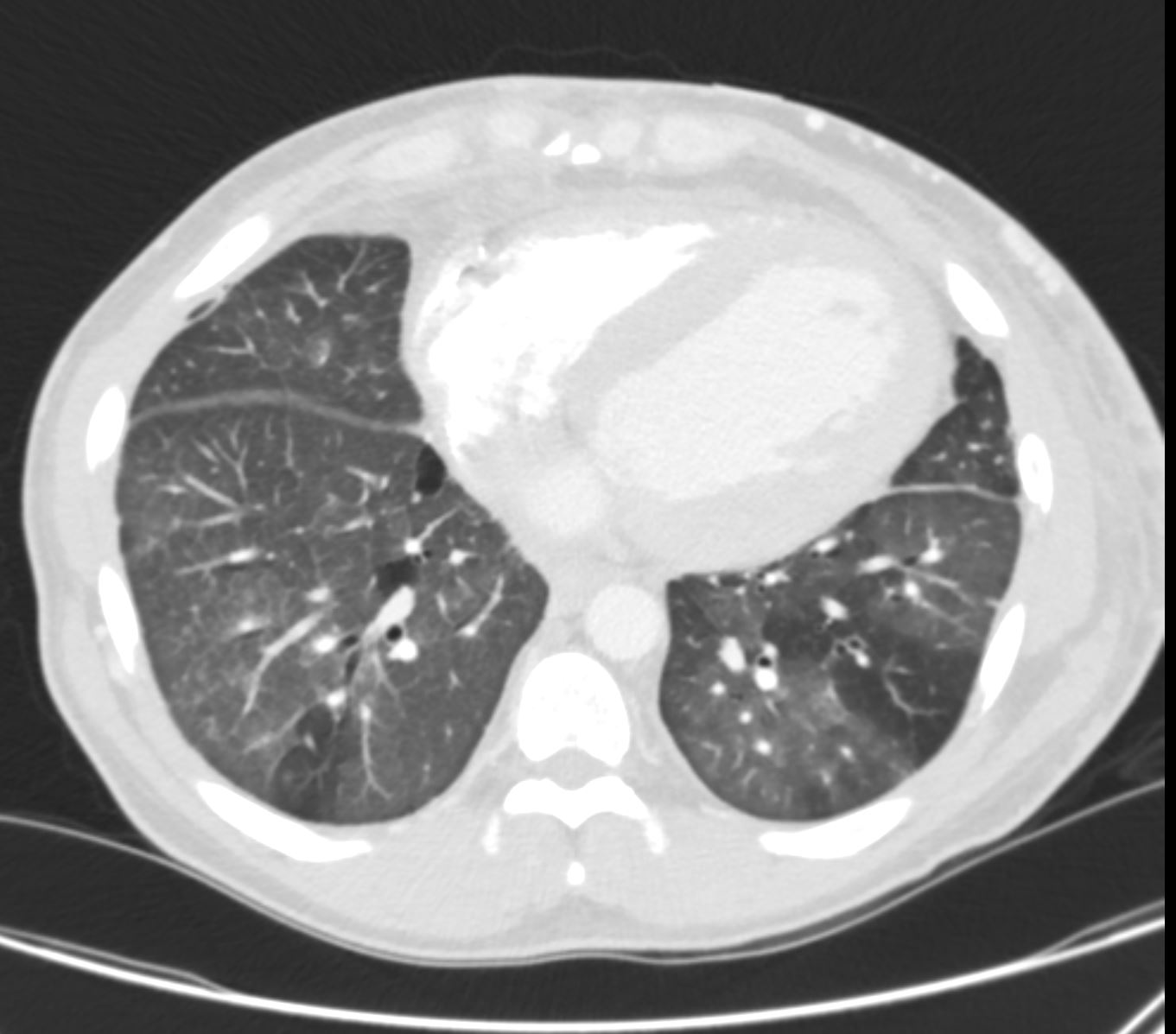
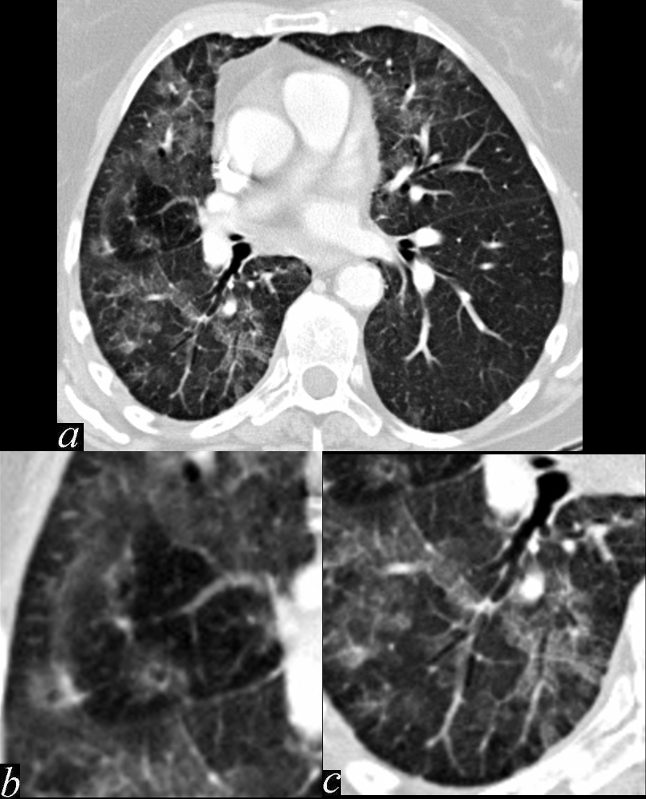
70-year-old female presents with dyspnea
CT performed in expiration shows multicentric foci of differing densities that include ground glass (seen on inspiration images) normal, and mosaic attenuation with air trapping and prominent centrilobular nodules These findings confirm small airway disease and in the appropriate clinical context are consistent with hypersensitivity pneumonitis (HP)
Ashley Davidoff MD TheCommonvein.net 135792c 144Lu
Head Cheese Sign
Hypersensitivity Pneumonitis
Ashley Davidoff MD TheCommonvein.net head cheese sign 006
Mosaic Attenuation Due to Small Blood Vessel Disease
CHF

Ashley Davidoff MD TheCommonVein.net
Mosaic Attenuation Caused by Obstruction of Small Airways
- Air trapping on the other hand
- is an imaging and physiologic term to
- retained air in a part or parts of the lung
- more easily identified during expiration
- caused by
- obstruction
Mosaic Attenuation of a Secondary Lobule
77F with long history of dyspnea and cough showing medium and small airway disease, centri-lobular nodules, para-septal nodules ground glass changes and mosaic attenuation Diagnosis includes Stage 3 sarcoidosis
Ashley Davidoff
TheCommonVein.net
77F with long history of dyspnea and cough showing medium and small airway disease, centri-lobular nodules, para-septal nodules ground glass changes and mosaic attenuation Diagnosis includes Stage 3 sarcoidosis
Ashley Davidoff TheCommonVein.net
Mosaic Attenuation -Due to Mucoid Impaction COPD


Ashley Davidoff TheCommonVein.net bronchioles 004


Ashley Davidoff TheCommonVein.net bronchioles 003
in a patient with COPD – Small Airways are obstructed and air is trapped
Ashley Davidoff MD TheCommonVein.net bronchioles 002
Small Airways are filled with mucus in a patient with COPD – Note centrilobular impaction of mucus Small Airways are obstructed and air is trapped
Ashley Davidoff TheCommonVein.net bronchioles 001
Mosaic Attenuation with Bronchiectasis
Ashley Davidoff MD TheCommonVein.net bronchiectasis 006
Ashley Davidoff MD TheCommonVein.net bronchiectasis 009
Mosaic Attenuation in CHF


Ashley Davidoff MD TheCommonvein.net 50-005-CT


Ashley Davidoff MD TheCommonvein.net 50-006-CT
Mosaic Attenuation in a patient with SLE thought to represent small vessel disease
Ashley Davidoff TheCommonVein.net
Ashley Davidoff TheCommonVein.net
This series of images shows some subtle changes that reflect the local control of blood flow to a small segment of the right middle lobe. Note that in image a, there is a small area of increased lucency (blacker) in the right lung just lateral to the vessels of the right hilum. This region is highlighted in b. Note also that in b, the rapid diminution of the size of the blood vessel to that subsegment when compared to the size change of the vessels in the image in c. The lucent appearance of the lung suggests air trapping and the vasoconstriction reflects decreased perfusion – ie with decreased ventilation there is an associated consequent associated decrease in perfusion.
47170c01.800 bronchocentric inflammation lung bronchovascular bundle chest inflammation peribronchial halo air trapping mosaic perfusion ground glass changes alveolar change air bronchogram acute bronchovascular inflammation ddx allergic collagen vascular disease infection CTscan
Ashley Davidoff MD TheCommonVein.net


Ashley Davidoff MD TheCommonVein.net
Ashley Davidoff MD TheCommonVein.net
Ashley Davidoff MD TheCommonVein.net 002-CT-mucoid-impaction
Examples
