Etymology
- Nodule: Derived from the Latin word nodulus, meaning “small knot.”
- Interlobular septa: Refers to the thin connective tissue boundaries of the secondary pulmonary lobule.
AKA
- Septal nodules
- Beaded septum sign
What is it?
Nodules on the interlobular septa are small, localized opacities along the thin connective tissue walls that separate secondary pulmonary lobules. These nodules are associated with perilymphatic or vascular processes affecting the septal lymphatics or vessels. The beaded septum sign describes their appearance as beads along the septal lines on imaging.
Caused by:
Common Causes
- Sarcoidosis: Hallmark finding with perilymphatic nodules along interlobular septa.
- Lymphangitic carcinomatosis: Tumor spread along lymphatic pathways.
Other Causes
- Infection:
- Granulomatous diseases such as tuberculosis and fungal infections.
- Inflammation:
- Rheumatoid nodules with septal involvement.
- Idiopathic:
- Idiopathic interstitial pneumonias, including nonspecific interstitial pneumonia (NSIP).
Resulting in:
- Nodular thickening along the interlobular septa.
- Beaded appearance on imaging.
- Potential associated septal thickening or lymphadenopathy.
Structural Changes:
- Thickened interlobular septa with nodules.
- Lymphatic vessel involvement along the septa.
Pathophysiology:
Nodular processes along interlobular septa result from lymphatic, vascular, or inflammatory involvement. In malignancy, tumor cells spread via lymphatics, while in sarcoidosis, granulomas form within the lymphatic pathways.
Pathology:
- Sarcoidosis: Non-caseating granulomas involving septal lymphatics.
- Lymphangitic carcinomatosis: Tumor emboli in lymphatic channels.
- Granulomatous infection: Caseating granulomas in the septal lymphatics.
Diagnosis:
- Imaging: HRCT to identify perilymphatic nodules and associated findings.
- Laboratory Tests: ANA/ANCA for autoimmune conditions; microbial serologies for infections.
- Biopsy: For tissue confirmation of granulomatous disease or malignancy.
Clinical:
- May be asymptomatic.
- Symptoms depend on the underlying cause, including cough, dyspnea, or systemic symptoms like fever or weight loss.
Radiology Detail:
CXR
- Findings: Subtle reticular patterns in cases of septal thickening.
- Associated Findings: Lymphadenopathy or pleural effusions.
CT
- Parts: Nodules along the interlobular septa.
- Size: Typically small (<1 cm).
- Shape: Round or oval, with smooth or irregular margins.
- Position: Distributed along the septa in a perilymphatic pattern.
- Character: Ground-glass attenuation or calcifications depending on the cause.
- Time: Stable in benign conditions; progressive in malignancy.
- Associated Findings: Septal thickening, lymphadenopathy.
Other Relevant Imaging Modalities:
- PET-CT: Assess metabolic activity for malignancy or inflammation.
Pulmonary Function Tests (PFTs):
- Often normal unless associated with diffuse interstitial processes.
Management:
- Imaging: HRCT and PET-CT for characterization.
- Laboratory Workup: Autoimmune panels and infectious serologies.
- Biopsy: For indeterminate cases or suspected malignancy.
Recommendations:
- Conduct HRCT for detailed imaging.
- Perform PET-CT if malignancy is suspected.
- Biopsy or lavage to confirm diagnosis.
Key Points and Pearls:
- The beaded septum sign strongly suggests a perilymphatic distribution, seen in sarcoidosis and lymphangitic carcinomatosis.
“The beaded septum sign, seen in sarcoidosis and lymphangitic spread of malignancy, reflects nodules along the interlobular septa.” Radiopaedia
- Calcified nodules often indicate healed granulomatous infections.
“Calcifications within septal nodules are frequently associated with prior granulomatous disease such as tuberculosis or histoplasmosis.” Radiology Key
- Concomitant lymphadenopathy is a strong clue for sarcoidosis or malignancy.
“Lymphadenopathy combined with interlobular septal nodules is highly suggestive of sarcoidosis or metastatic lymphatic spread.” Radiographics
- A multidisciplinary approach, combining imaging, laboratory results, and clinical history, is crucial for diagnosis.
“Integration of clinical, imaging, and laboratory findings is essential for accurate diagnosis of septal nodules.” Radiopaedia
 Para-septal and Centrilobular Nodules
Para-septal and Centrilobular Nodules
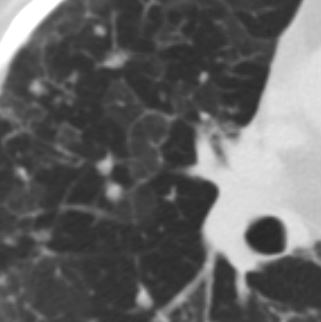
77F with long history of dyspnea and cough showing medium and small airway disease, centri-lobular nodules, para-septal nodules ground glass changes and mosaic attenuation Diagnosis includes Stage 3 sarcoidosis
Ashley Davidoff
TheCommonVein.net
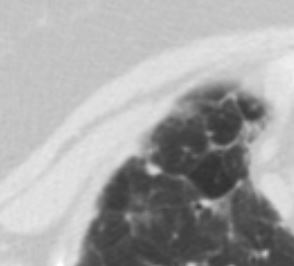
77F with long history of dyspnea and cough showing medium and small airway disease, centri-lobular nodules, para-septal nodules ground glass changes and mosaic attenuation Diagnosis includes Stage 3 sarcoidosis
Ashley Davidoff
TheCommonVein.net
