-
-
Etymology
- Derived from the Latin words obliterare, meaning “to erase,” and the Greek words bronchion, meaning “small airway,” and -itis, meaning “inflammation.” The term refers to inflammation and scarring of the bronchioles leading to their obliteration.
AKA
- Constrictive bronchiolitis
- Bronchiolitis obliterans
What is it?
- Obliterative bronchiolitis is a chronic inflammatory and fibrotic condition characterized by progressive narrowing and obliteration of the bronchioles due to inflammation, fibrosis, and scarring.
Caused by:
- Most common causes:
- Post-transplant complications (e.g., lung, bone marrow, or hematopoietic stem cell transplants)
- Inhalational injuries (e.g., toxic fumes, gases)
- Less common causes:
- Infection:
- Adenovirus, Mycoplasma pneumoniae, or post-viral bronchiolitis
- Inflammation:
- Autoimmune diseases (e.g., rheumatoid arthritis, inflammatory bowel disease)
- Immune:
- Chronic rejection in organ transplantation
- Trauma:
- Inhalational exposure to irritants (e.g., chlorine, ammonia)
- Other:
- Idiopathic obliterative bronchiolitis
- Infection:
Resulting in:
- Airflow limitation and obstructive pulmonary dysfunction
- Progressive dyspnea and hypoxemia
- Severe ventilation-perfusion mismatch
Structural Changes:
- Submucosal fibrosis and inflammation within bronchioles
- Obliteration of bronchiolar lumens
- Collateral air trapping and hyperinflation
Pathophysiology:
- Obliterative bronchiolitis begins with inflammation of the bronchioles due to infectious, toxic, or immune-mediated insults. Chronic injury leads to fibrotic remodeling, luminal narrowing, and eventual obliteration of the airways. This results in distal air trapping, hypoxia, and progressive respiratory dysfunction.
Pathology:
- Submucosal and peribronchiolar fibrosis
- Luminal narrowing and obliteration of bronchioles
- Chronic inflammatory infiltrates
Diagnosis
Clinical:
- Symptoms include:
- Progressive dyspnea
- Chronic cough
- Wheezing (in some cases)
- History of prior transplant, toxic inhalational exposure, or viral infection
Radiology:
- CXR:
- Hyperinflation and small airway opacities
- Flattening of the diaphragm
- CT of the Chest:
- Mosaic attenuation and air trapping on expiratory imaging
- Bronchial wall thickening
- Subsegmental atelectasis
Labs:
- Autoimmune screening if connective tissue disease is suspected
- Viral serologies or cultures in post-infectious cases
Management:
- Supportive care:
- Oxygen therapy for hypoxemia
- Pulmonary rehabilitation
- Bronchodilators for symptomatic relief
- Targeted therapy:
- Corticosteroids and immunosuppressive agents for autoimmune or post-transplant causes
- Antiviral therapy in post-viral cases if indicated
- Advanced interventions:
- Lung transplantation in end-stage disease
Radiology Detail
CXR
Findings:
- Hyperinflation with flattening of the diaphragm
- Subtle reticular or nodular patterns
Associated Findings:
- Peribronchial thickening
- Atelectasis in advanced cases
CT of the Chest
Parts:
- Terminal and respiratory bronchioles
Size:
- Subtle thickening of small airways
Shape:
- Irregular, constricted lumens with mosaic attenuation
Position:
- Diffuse distribution, typically affecting lower lung zones
Character:
- Mosaic attenuation and air trapping
Time:
- Chronic progression with acute exacerbations
Associated Findings:
- Evidence of air trapping on expiratory imaging
- Fibrotic bands or subsegmental atelectasis
Other relevant Imaging Modalities
MRI/PET CT/NM/US/Angio:
- MRI: Rarely used but may identify associated soft tissue changes
- PET-CT: Useful in assessing inflammation or post-transplant complications
Pulmonary Function Tests (PFTs):
- Obstructive pattern with decreased FEV1/FVC ratio
- Air trapping and hyperinflation
Recommendations:
- High-resolution CT for detailed evaluation of small airway disease
- Biopsy for definitive diagnosis in uncertain cases
- Early referral to pulmonology or transplant specialists for management
Key Points and Pearls:
- Obliterative bronchiolitis is commonly associated with post-transplant rejection and inhalational injuries.
- High-resolution CT findings include mosaic attenuation and air trapping.
- Management focuses on supportive care and addressing the underlying cause, with lung transplantation being a final option in severe cases.
- Early diagnosis and intervention are critical to improving outcomes.
-
Obliterative Bronchiolitis aka (bronchiolitis obliterans is also known and constrictive bronchiolitis) association to lung transplant and bone marrow transplant
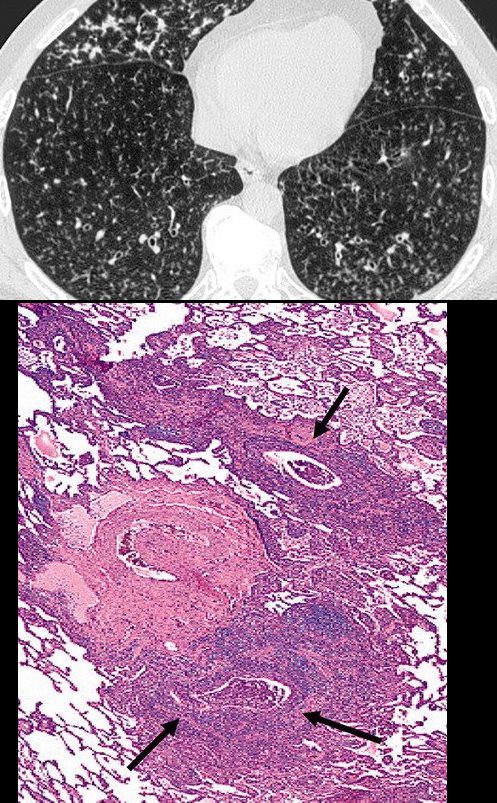
Obliterative bronchiolitis after bone marrow transplantation in a 47-year-old man with myeloma. (a) Expiratory high-resolution CT scan shows diffuse centrilobular nodules connected to branching linear opacities bilaterally. Note the air trapping in the right lower lobe. (b) Photomicrograph (original magnification, ×200; hematoxylin-eosin stain) of a specimen from open lung biopsy shows the bronchiolar walls surrounded by concentric chronic inflammatory infiltrates (arrows).
Rossi, SE et al Tree-in-Bud Pattern at Thin-Section CT of the Lungs: Radiologic-Pathologic Overview RadioGraphics Vol. 25, No. 3 2005
CT Scleroderma Obliterative Bronchiolitis vs
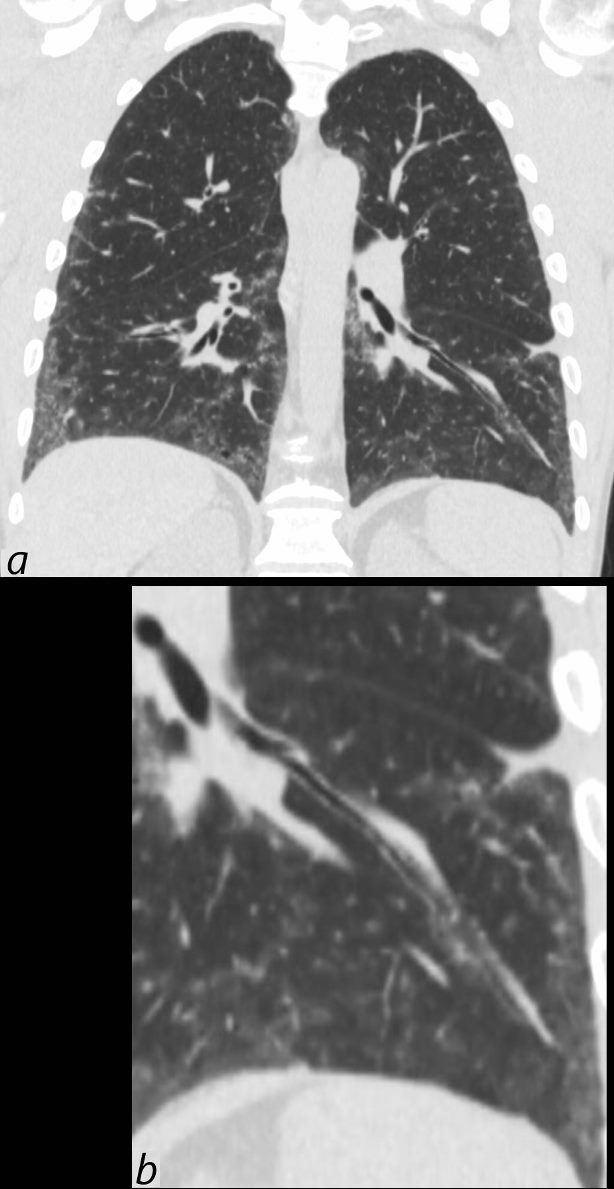
39-year-old-male with a history of scleroderma associated with ILD and digital vasculopathy with ulcers.
Coronal CT shows thickening of the segmental and subsegmental airway supplying the lateral basal segment of the left lower lobe. In addition there is a background of peripheral ground glass changes poorly defined ground glass centrilobular nodules and mild reticulation.
In this clinical setting obliterative bronchiolitis (aka bronchiolitis obliterans aka constrictive bronchiolitis) is suggested. Cellular NSIP is also a radiological consideration.
Ashley Davidoff MD TheCommonVein.net 132Lu 136669c
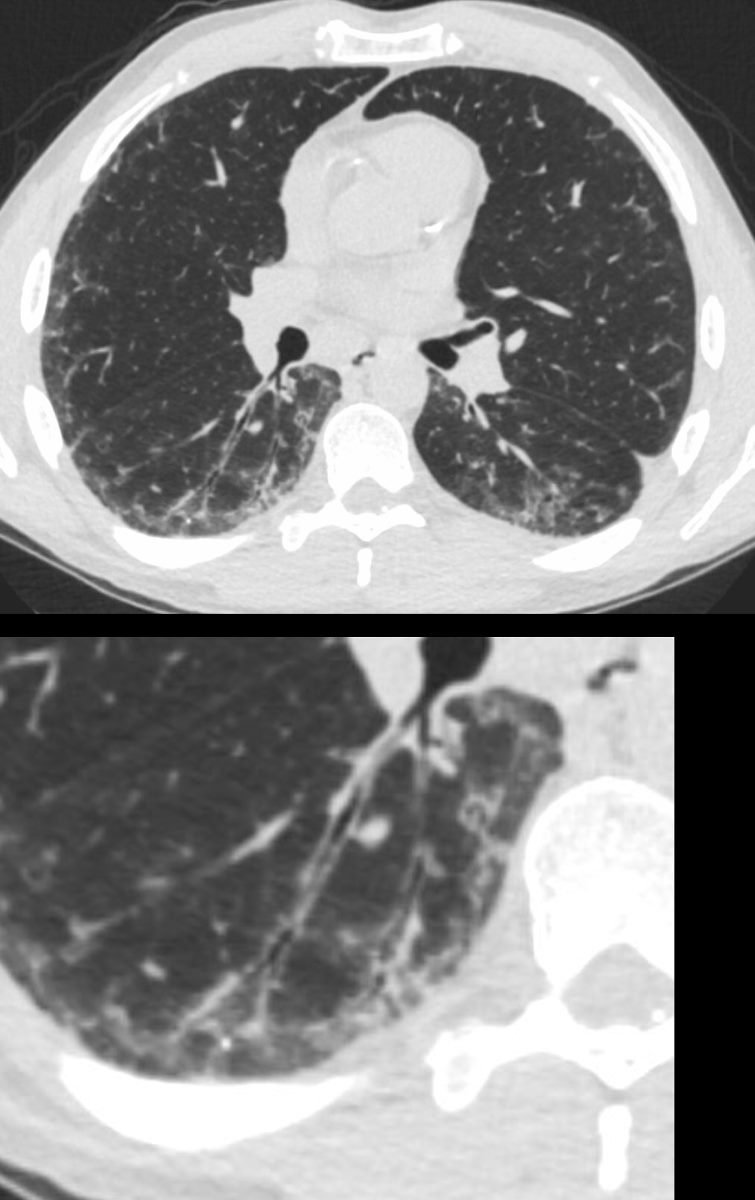
39-year-old-male with a history of scleroderma associated with ILD and digital vasculopathy with ulcers.
Axial CT shows thickening of the segmental, subsegmental and small airways supplying the posterior basal segment of the right lower lobe. In addition there is a background poorly defined ground glass changes and mild reticulation.
In this clinical setting obliterative bronchiolitis (aka bronchiolitis obliterans aka constrictive bronchiolitis) is suggested. Cellular NSIP is also a radiological consideration.
Ashley Davidoff MD TheCommonVein.net 132Lu 136669c

39-year-old-male with a history of scleroderma associated with ILD and digital vasculopathy with ulcers.
Coronal CT at the level of the spine shows extensive ground glass in the lower lung fields, with subpleural sparing better visualized on the left. Ill defined ground glass centrilobular nodules and mosaic attenuation suggest small airway disease.
In this clinical setting obliterative bronchiolitis (aka bronchiolitis obliterans aka constrictive bronchiolitis) and cellular NSIP are radiological considerations.
Ashley Davidoff MD TheCommonVein.net 132Lu 136667
References and Links
TCV
