The Pleura
- What is it:
- The pleura refers to a double-layered serous membrane that:
- Covers the lungs (visceral pleura).
- Lines the chest wall, diaphragm, and mediastinum (parietal pleura).
- It provides:
- A frictionless surface for lung movement during respiration.
- A sealed compartment for maintaining intrapleural pressure.
- The pleura refers to a double-layered serous membrane that:
- Etymology:
- Derived from the Greek word pleura, meaning “side” or “rib,” reflecting its anatomical position.
- Parts:
- Visceral pleura:
- Tightly adheres to the lung surface, extending into fissures.
- Parietal pleura:
- Lines the thoracic cavity, including:
- Costal pleura (adjacent to ribs).
- Diaphragmatic pleura (covers diaphragm).
- Mediastinal pleura (next to the mediastinum).
- Cervical pleura (extends into the thoracic inlet).
- Lines the thoracic cavity, including:
- Pleural cavity:
- A potential space between the two pleural layers, containing a small amount of lubricating fluid.
- Visceral pleura:
- Size and shape:
- Covers the entire thoracic cavity, adapting to the shape of the lungs and chest wall.
- Pleural cavity volume is small in normal conditions but may expand significantly in pathological states (e.g., effusion, pneumothorax).
- Position:
- Surrounds the lungs and lines the thoracic cavity.
- Character:
- A thin, elastic, and semitransparent membrane.
- Blood supply:
- Visceral pleura: Supplied by bronchial arteries and drained by pulmonary veins.
- Parietal pleura: Supplied by intercostal, internal thoracic, and phrenic arteries; drained by systemic veins.
- Lymphatic drainage:
- Visceral pleura: Drains into pulmonary and hilar lymph nodes.
- Parietal pleura: Drains into intercostal, parasternal, diaphragmatic, and mediastinal lymph nodes.
- Nerve supply:
- Visceral pleura: No somatic innervation (insensitive to pain).
- Parietal pleura: Richly innervated by intercostal nerves (costal pleura) and phrenic nerves (diaphragmatic and mediastinal pleura), making it sensitive to pain, pressure, and temperature.
- Embryology:
- Derived from the mesoderm, with the visceral pleura developing from the splanchnic mesoderm and the parietal pleura from the somatic mesoderm.
- Applied anatomy:
- Clinical significance:
- Pathologies affecting the pleura include:
- Pleural effusion: Excess fluid in the pleural cavity.
- Pneumothorax: Air in the pleural cavity causing lung collapse.
- Pleuritis: Inflammation of the pleura, often causing pain due to parietal pleural involvement.
- Mesothelioma: Malignant tumor of the pleura, often linked to asbestos exposure.
- Pathologies affecting the pleura include:
- Imaging application:
- Chest X-ray: Identifies pleural abnormalities such as effusions or thickening.
- Chest CT: Provides detailed visualization of pleural anatomy and pathology (e.g., nodularity, thickening, effusions).
- Ultrasound: Commonly used to assess pleural effusions and guide thoracentesis.
- Clinical significance:
Note
The visceral pleura, is intimately attached to the lung and follows the fissures, while the second component, the parietal layer, is intimately related to the thoracic cage mediastinum and diaphragm.
. The pleura have elastic qualities in order to accommodate the changes in size with the expansion and contraction of the chest cavity. During the respiratory cycle the two layers of pleura move in tandem gliding smoothly over each other, lubricated by a small amount of serous fluid. As the chest wall expands during inspiration, the parietal pleura moves with it, while the visceral pleura moves with the expansion of the lung, the two being held together by the negative pressure caused by capillary forces of the fluid that lies between the two smooth surfaces.
The two cannot be easily separated, unless a small amount of air can be introduced between the opposing surfaces
The cells lining the pleura are called mesothelial cells. They are responsible for the production of pleural fluid. Although we describe two components to the pleura, it is really one structure into which the developing lung bud grows, similar to a fist pushing its way into a balloon. At the hilum of the lung, the bronchovascular and lymphatic bundles acting as the fist, push their way into the pleura and become enveloped by the pleura, with the most distal progeny of the lung bud coming into intimate contact with the visceral pleura.
Despite the apparent single embryologic origin of the visceral and parietal pleura, they are in fact functionally and structurally different. The visceral pleura for example has no pain fibers whereas the parietal pleura is extremely sensitive to pain. The visceral pleura receives its nerve supply through the autonomic nervous system, whereas the parietal pleural innervation is via the somatic intercostal nerves and the phrenic nerve.
The blood supply of the visceral and parietal pleura is also different. The parietal pleura is supplied only by the systemic circulation from the intercostal arteries while the visceral pleura is supplied by the bronchial arteries and the pulmonary arteries.
The visceral pleura follows the lung surface and therefore will follow the fissures. The parietal pleura follows the chest wall and therefore will not follow the fissures of the lung. The pleural cavity is larger than the total lung volume, allowing the lung to expand during respiration. It is particularly obvious in the pleural recesses at the inferior aspect of the thoracic cavity.
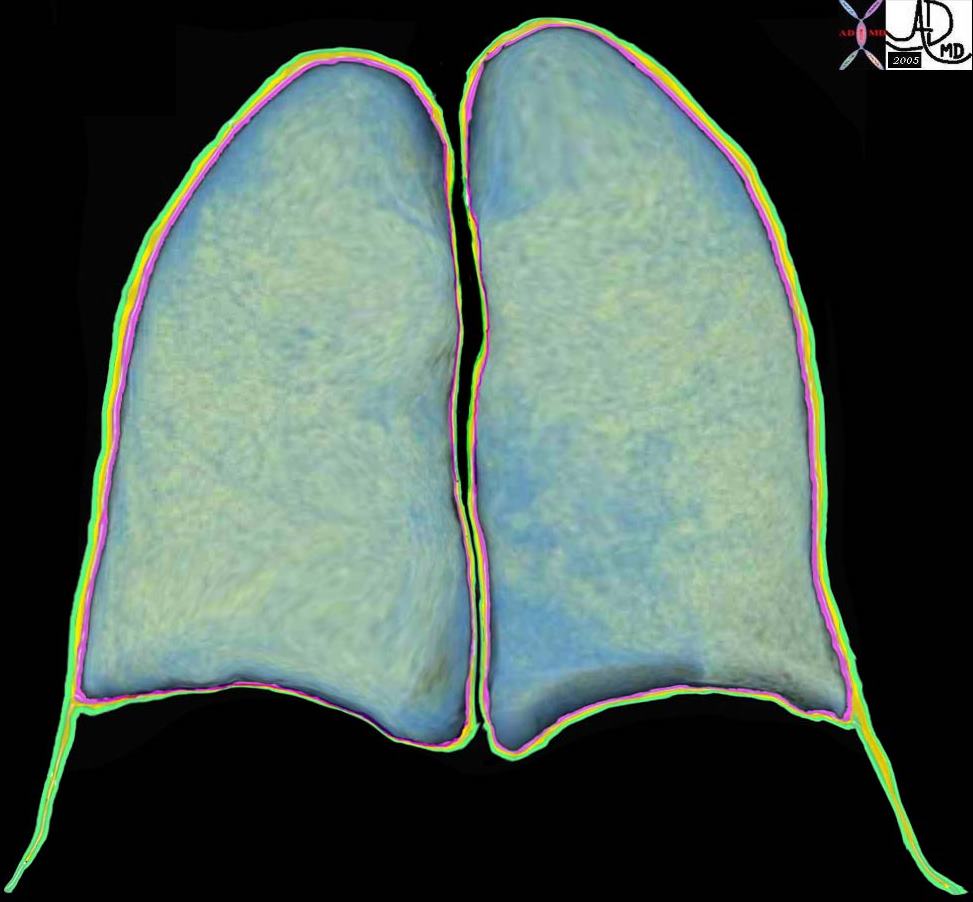
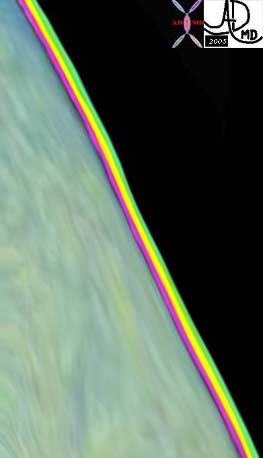
The coronally reformatted image of the lung parenchyma has been outlined with the visceral pleura, (pink) the pleural fluid in the pleural space, (orange) and the parietal pleura. (green) Note how at end expiration the parietal pleura in the costophrenic sulcus extends beyond the lung margin so that the visceral pleura is absent in the costophrenic sulcus and there are two layers of parietal pleura facing each other. During inspiration the lung expands into this space. 32634b10
Key Words lung pleura pulmonary
Ashley Davidoff MD TheCommonVein.net
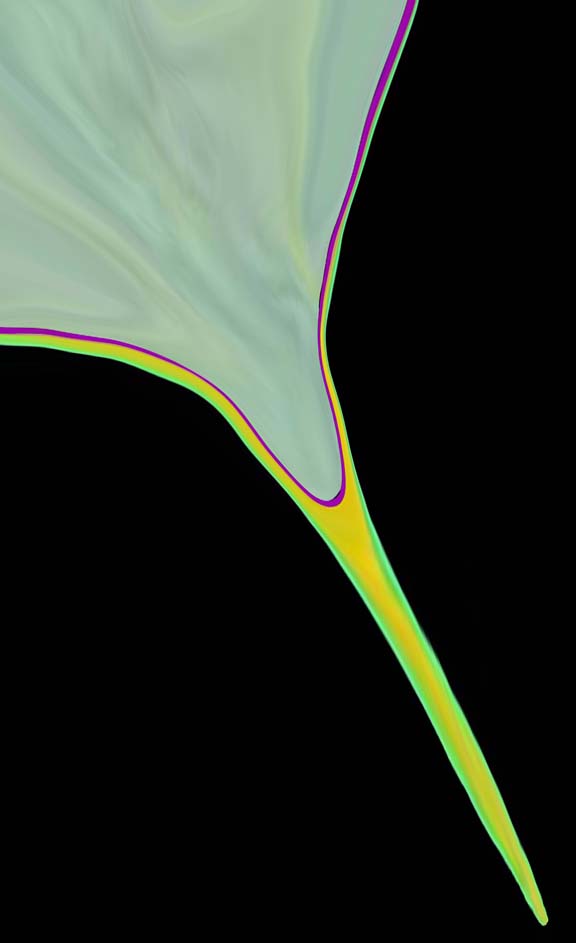
The inferior aspect of the left lung base is magnified in this image s. It shows the costophrenic sulcus where the visceral pleura is absent and two layers of parietal pleura face each other. Ashley Davidoff MD TheCommonVein.net 32634b11b04b
For the interventionalist it is important to remember how caudal the pleural space extends and therefore in planning a liver biopsy or drainage the low lying costophrenic sulcus that may fill with lung on inspiration must be taken into account.
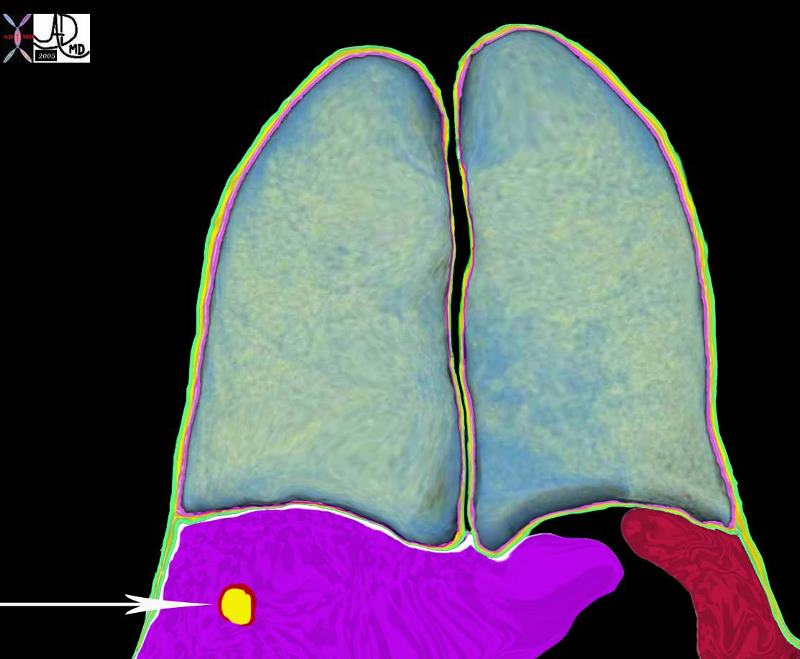
The white arrow points to the potential path of a needle to a lesion in the liver. To the observer it would seem low and out of range of the pleura and lung. Since the costophrenic sulcus would not be visible to ultrasound nor CT interrogation it is difficult to know exactly where it lies. One just has to know that it may lie quite low, and that on inspiration the lung may in fact fill that space as well. Hence the potential complications include a pneumothorax from this approach, and if long term catheter drainage is contemplated transgression of the pleural space may cause an effusion or an infection resulting in an empyema.
Ashley Davidoff MD TheCommonVein.net 32634b15
The visceral pleura is subdivided into three distinct parts, including the mediastinal, the diaphragmatic, and the costal pleura.
There is continued production of pleural fluid by the mesothelial cells into the pleural space. There is also a continued drainage of the fluid by the sub pleural lymphatic system which lies between the visceral pleura and lung coursing into the interlobular septa.
Applied Anatomy
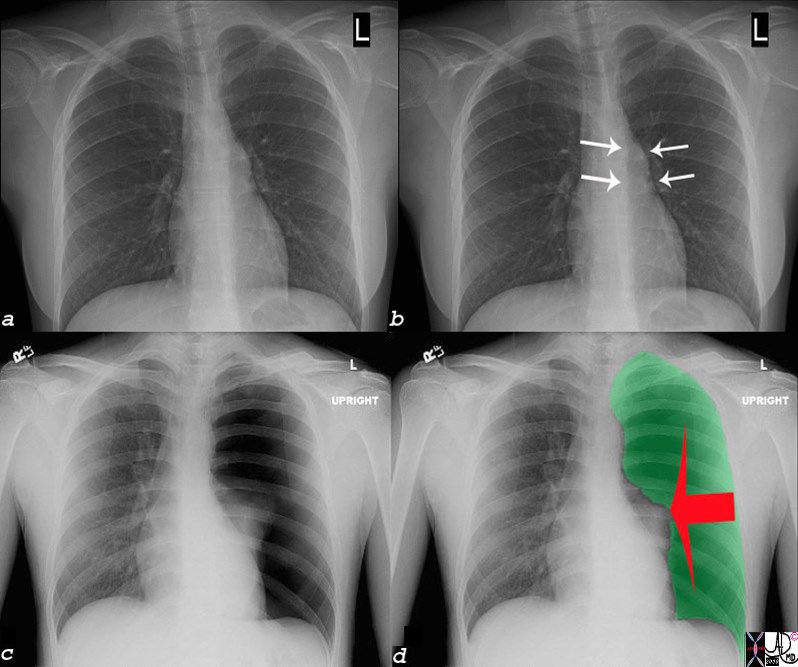
On a plain film of the chest the easiest method of identifying fluid is the lateral upright examination where fluid accumulates in the posterior pleural recesses and causes “blunting” of the posterior costophrenic angles. CT is far more sensitive in the detection of the fluid and to some extent in the characterization of the fluid. When the fluid layers with a meniscus that is parallel to the floor and falls into expected dependent positions (just as water would in a glass on a flat table top) then the effusion can be expected to be free flowing. If the fluid falls in a non-dependent fashion it is considered “loculated” and it is more likely to be complex. Under these circumstances the level is tilted. Ultrasound however is better able to identify septations and other soft tissue components of the fluid collection. Thoracentesis however is still necessary to enable the chemical evaluation of the fluid.
When there is an accumulation of fluid in the pleural space (pleural effusion) or air (pneumothorax) the underlying lung gets pushed away from the chest wall and the harmonious interaction of chest wall pleura and lung is lost. As the accumulation gets larger, the underlying lung collapses without the support mechanisms, and functional lung tissue is lost, with ensuing respiratory difficulty. The lungs are relatively forgiving in that they have enough reserve to accommodate effusions (even large) and moderate degrees of atelectasis, particularly when this occurs gradually, enabling compensatory mechanisms to evolve.
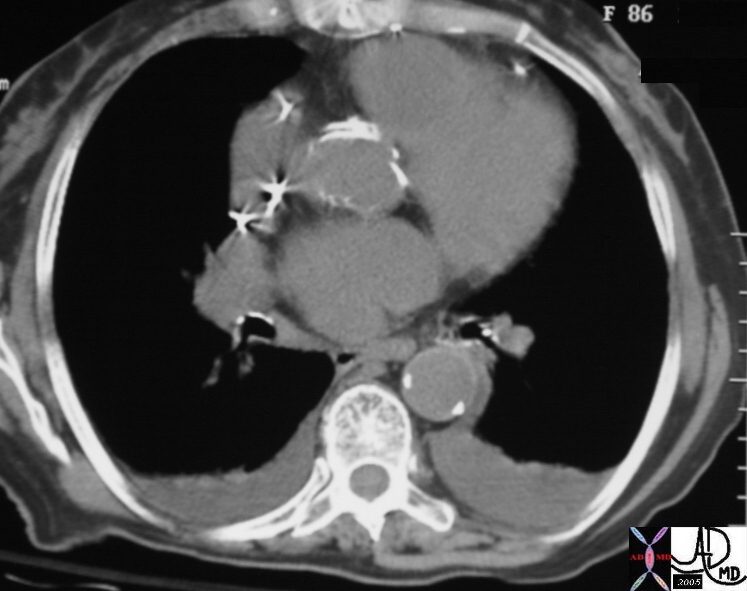
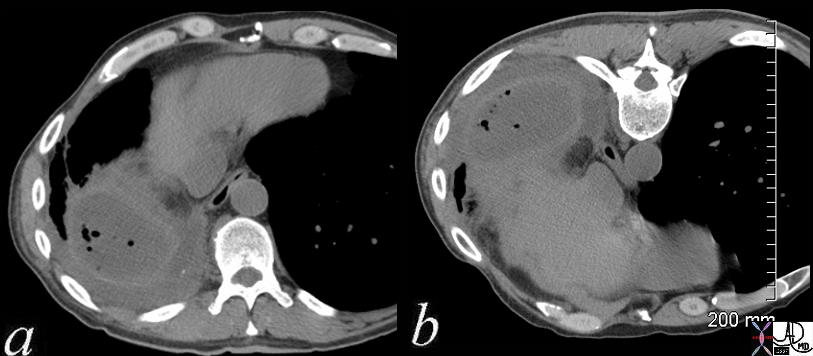
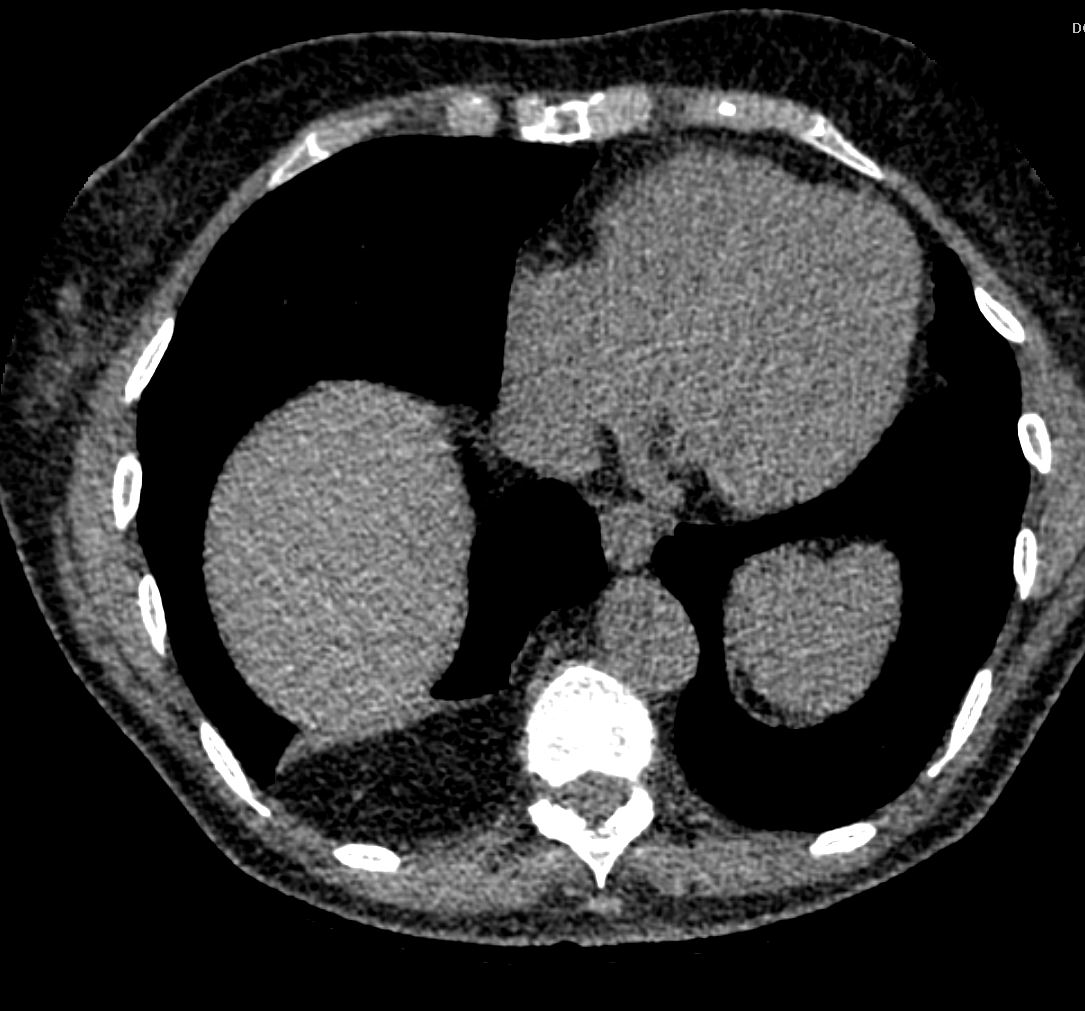
This CT through the chest shows a complex effusion on the left where the fluid level is not parallel with the table top as the medial level is higher than the lateral. This would indicate a form of loculation. On the left side the collection is mostly dependent but for the medial part which also climbs slightly higher than it should and hence it is also partially loculated.
Ashley Davidoff MD TheCommonVein.net 28769

keywords lung pleura effusions bilateral pleural effusions compressive atelectasis left atrial enlargement coronary artery calcification congestive heart failure CHF CTscan
Ashley Davidoff MD TheCommonVein.net 49454
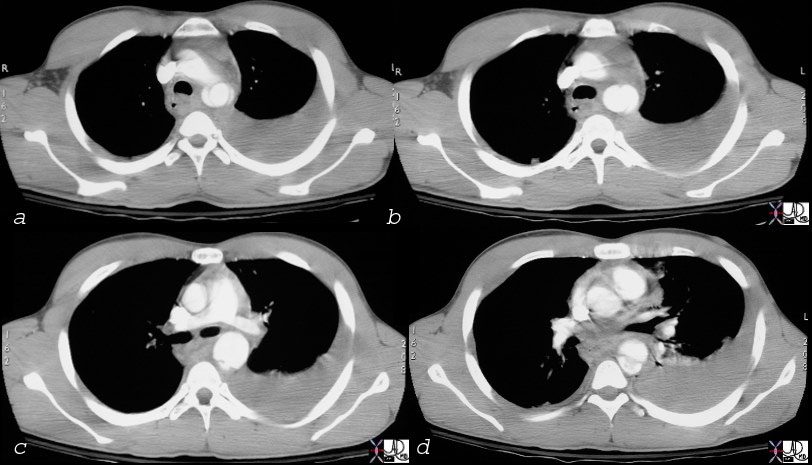
thorax thoracic aorta isthmus aortic laceration pseudoaneurysm leak contained rupture posterior mediastinal hematoma pleura pleural effusion hemothorax aortic laceration trauma traumatic tear trauma MVA CTscan C
Ashley Davidoff MD TheCommonVein.net 17540c02
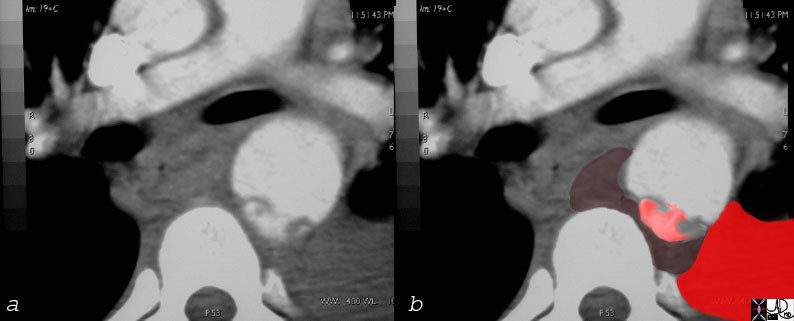
Overlay in red shows the site of the aortic laceration
keywords thorax thoracic aorta isthmus aortic laceration pseudoaneurysm leak contained rupture posterior mediastinal hematoma pleura pleural effusion hemothorax aortic laceration trauma traumatic tear trauma MVA CTscan
Ashley Davidoff MD TheCommonVein.net
17540c01
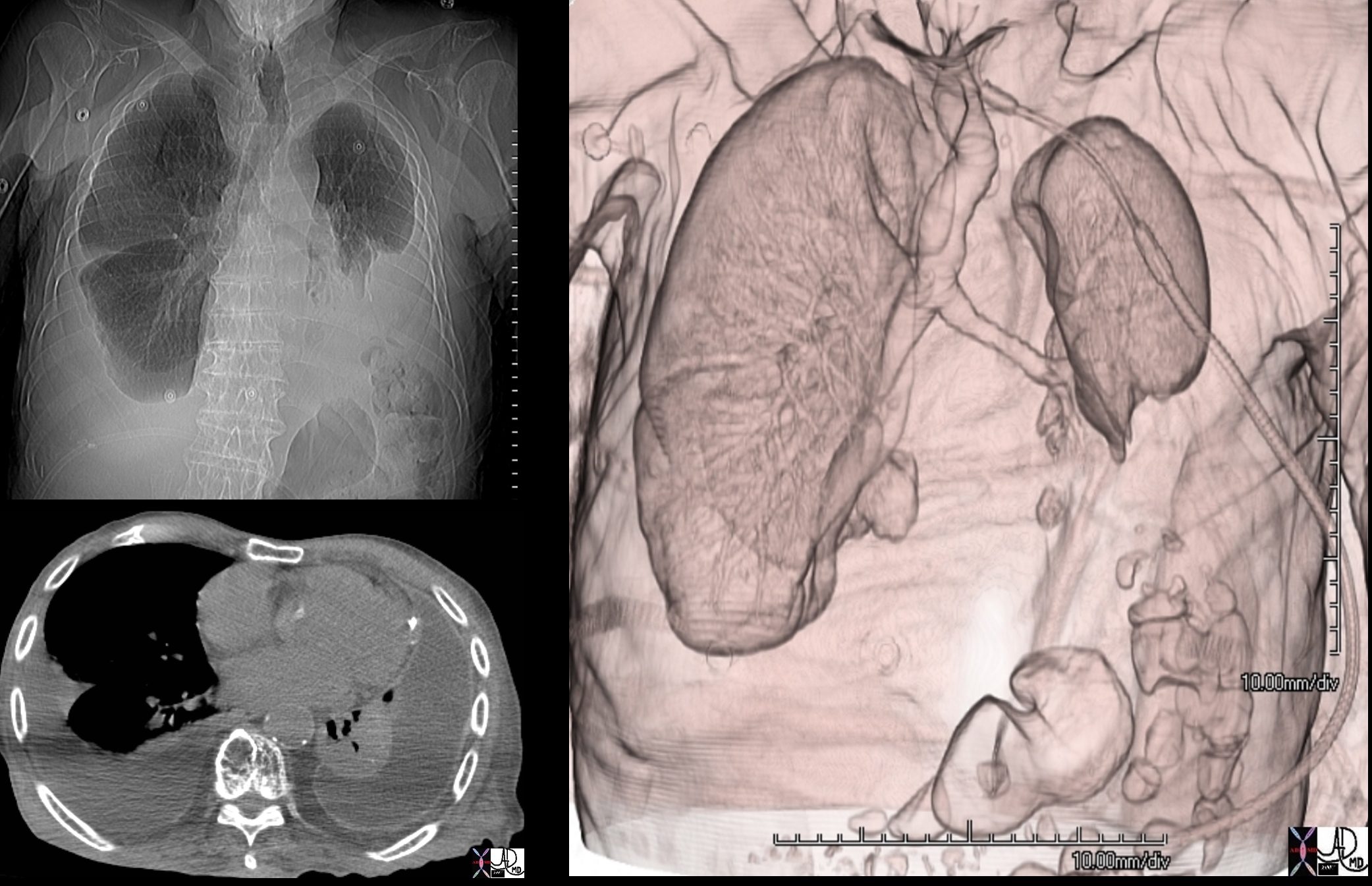
88 year old male with bilateral effusions shown on the CXR. Axial CT shows thickened pleura on the left with compressive atelectasis of the lower lobe and a smaller region of crescentic compressive atelectasis on the right. 3D reconstruction shows atelectasis of the left lower lobe and portion of the lingula
Ashley Davidoff MD TheCommonVein.net 74242c
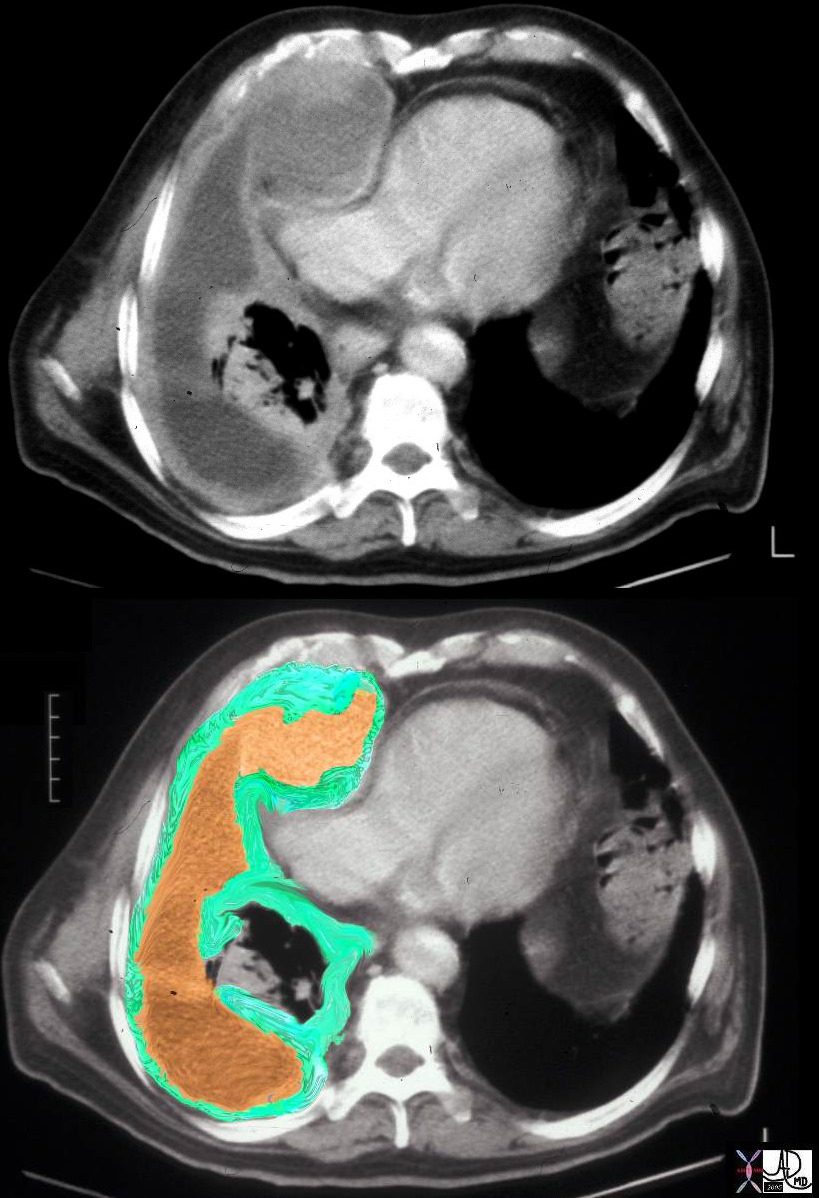
This CT scan represents a patient with a malignant tumor of the pleura called a mesothelioma. Note how thick the pleura is and how complex the associated effusion is. The lung is strangled and collapsed under the aggressive tumor. The right atrium is compressed by the tumor. In the image below the green overlay represents the tumor while the orange represents the loculated effusion.
Ashley Davidoff MD TheCommonVein.net 32639c01
Key Words lung pleura air air bubbles forces gravity fibrin complex loculated thickened pleura pleural thickening fluid accumulation trapped air dx empyema CTscan D
Ashley Davidoff MD TheCommonVein.net 71441c01
Tension pneumothorax
Tension pneumothorax is an acute life threatening event, where there is not only collapse of the lung from the pneumothorax but a pressure build up in the pleural space that causes the heart and great vessels to be compressed. This acute loss of support of the system, is life threatening and if not treated by emergency decompression will lead to death. It would only take a small open-ended needle placed into the pleural space to decompress the tension and save a life. Sometimes when a patient suddenly collapses, and the condition of tension pneumothorax is a clinical consideration, physicians emergently put a small needle into the chest wall even before the chest X-ray confirms their clinical suspicions. Many a life, hanging on with but a thread, has been saved by a quick thinking, astute, and an artful doctor, who with a single stick of a simple needle, turned the life on the thread back to health.
28 year old male with acute chest pain and respiratory distress
Ashley Davidoff MD TheCommonVein.net
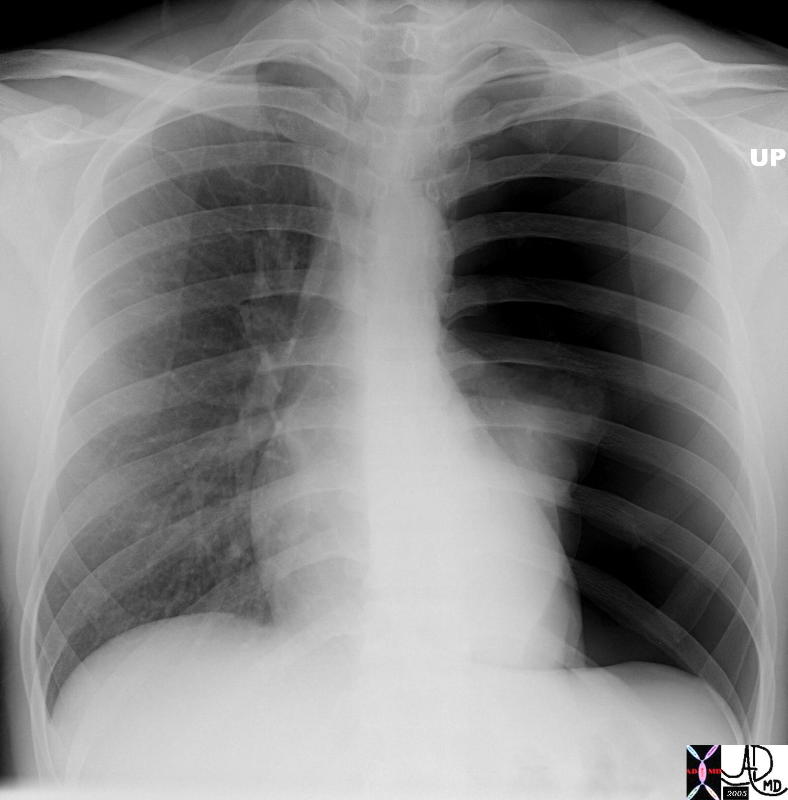
Spontaneous rupture tension pneumothorax, total collapse.
Ashley Davidoff MD TheCommonVein.net 42106b
Ashley Davidoff MD TheCommonVein.net

Diaphragm Intact
Ashley Davidoff MD TheCommonVein.net
CLINICAL ASPECTS
Acute inflammatory conditions of the pleura, results in pleuritic chest pain. When the patient inspires the inflamed pleural surfaces rub against each other causing exquisite localized pain. The motion of the pleura becomes restricted by fibrinous exudates, and may cause a pleural “rub” – a squeaking sound caused by the restricted motion. As the pleural effusion enlarges the chances of contact of the two surfaces becomes less likely, and hence the pleural rub cannot be heard. Instead the large effusion compresses the adjacent lung causing a condition called “compressive atelectasis.” Percussion of the fluid results in dullness and auscultation results in amplification of sound called egophony.
In the laboratory it is important to distinguish between a transudative effusion and an exudative effusion. This is done by evaluating the concentration of protein in the fluid. A transudate usually results from pulmonary congestion and contains limited protein and no fibrin, whereas an exudate is more complex and contains fibrin. Empyema is an infected pleural effusion and one of its hallmarks is the relatively low PH of the fluid.