- What is it:
- Pleural effusion refers to:
- The accumulation of excess fluid in the pleural cavity,
- resulting from an imbalance in fluid production and absorption.
- It may present as:
- Transudative effusion (caused by systemic factors like increased hydrostatic pressure or decreased oncotic pressure).
- Exudative effusion (caused by local factors such as inflammation, infection, or malignancy).
- Pleural effusion refers to:
- Etymology:
- Derived from the Greek word pleura (side or rib) and the Latin word effusio (to pour out), describing fluid accumulation in the pleural space.
- AKA:
- Fluid in the pleural space, Pleural fluid accumulation.
- How does it appear on each relevant imaging modality:
- Chest X-ray:
- Classification of effusions:
- Mild effusion: Blunting of the costophrenic angle; corresponds to fluid volumes of 200–300 mL.
- Moderate effusion: Extends up to the hemithorax but spares the apices; corresponds to volumes of 500–1,000 mL.
- Large effusion: Fills the entire hemithorax with mediastinal shift away from the effusion; corresponds to volumes >1,000 mL.
- Supine view:
- Veiling opacity: Diffuse increased density over the affected hemithorax caused by layering of fluid, often obscuring normal lung markings.
- Classification of effusions:
- Chest CT:
- Classification of effusions (volumetric):
- Mild effusion: Small fluid collections limited to the posterior costophrenic sulcus.
- Moderate effusion: Fluid extends along the lateral pleural space but does not occupy the entire hemithorax.
- Large effusion: Fluid occupies most or all of the pleural cavity with significant mediastinal shift.
- Shape:
- Free (non-loculated): Fluid layers in dependent portions of the pleural cavity.
- Loculated: Encapsulated fluid collections within the pleural cavity;
- Often visible with thickened pleura.
- May demonstrate the split pleura sign: separation of visceral and parietal pleura due to inflammation or exudative processes.
- Associated compressive atelectasis:
- Seen as passive collapse of adjacent lung tissue caused by large effusions exerting pressure on the lung.
- Classification of effusions (volumetric):
- Ultrasound:
- Hypoechoic or anechoic fluid collection in the pleural space.
- Can identify septations or loculations, especially in exudative effusions.
- Chest X-ray:
- These findings reflect:
- Systemic factors (transudative effusion):
- Congestive heart failure (most common cause).
- Cirrhosis (hepatic hydrothorax).
- Nephrotic syndrome (low oncotic pressure).
- Local factors (exudative effusion):
- Infection:
- Parapneumonic effusion: Occurs adjacent to bacterial pneumonia; can progress to complicated effusion or empyema if untreated.
- Tuberculosis.
- Inflammation:
- Rheumatoid arthritis or lupus pleuritis.
- Neoplasm:
- Primary lung cancer or metastatic disease.
- Trauma:
- Hemothorax or chylothorax.
- Infection:
- Systemic factors (transudative effusion):
- Differential diagnosis:
- Transudative causes:
- Congestive heart failure.
- Hypoalbuminemia (e.g., cirrhosis, nephrotic syndrome).
- Constrictive pericarditis.
- Exudative causes:
- Parapneumonic effusion or empyema.
- Malignancy (e.g., mesothelioma, metastatic cancer).
- Tuberculosis.
- Connective tissue diseases (e.g., rheumatoid arthritis, lupus).
- Special types:
- Hemothorax: Blood in the pleural space.
- Chylothorax: Milky lymphatic fluid, often due to thoracic duct injury.
- Transudative causes:
- Recommendations:
- Perform thoracic ultrasound for bedside evaluation and to guide thoracentesis.
- Analyze pleural fluid via thoracentesis to classify effusion as transudative or exudative (Light’s criteria).
- Use Chest CT to assess loculations, pleural thickening, associated compressive atelectasis, and lung abnormalities.
- Treat underlying causes (e.g., diuretics for heart failure, antibiotics for infection).
- Monitor parapneumonic effusions closely to identify progression to empyema, which may require chest tube drainage.
- Key points and pearls:
- Transudative effusions are typically bilateral and associated with systemic conditions like heart failure or cirrhosis.
- Exudative effusions often require further evaluation for infection, malignancy, or inflammatory diseases.
- Loculated effusions may show the split pleura sign and require advanced imaging or interventions for diagnosis and drainage.
- Large effusions may cause compressive atelectasis, leading to dyspnea.
- Parapneumonic effusions adjacent to pneumonia should be treated promptly to prevent progression to empyema.
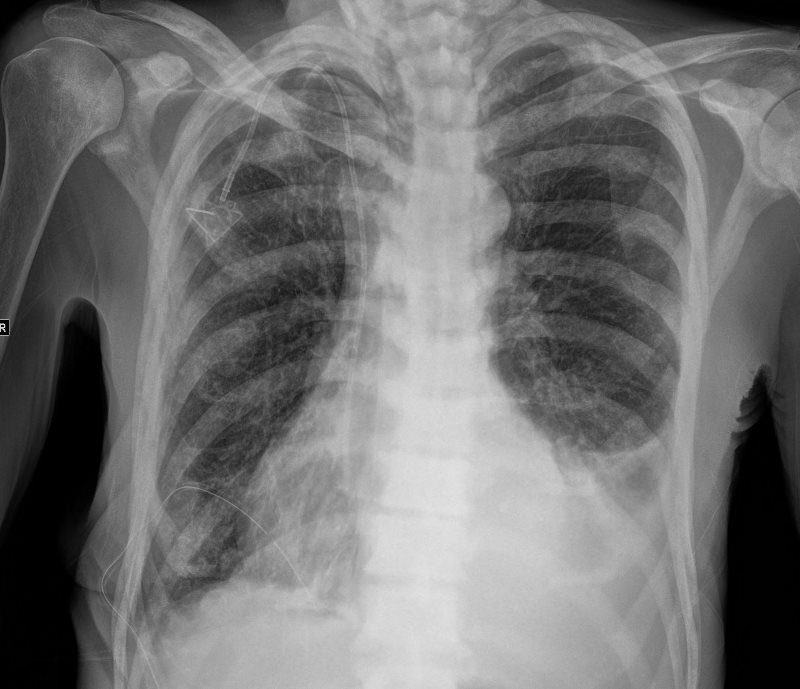
Right Sided Pleural Effusion In CHF
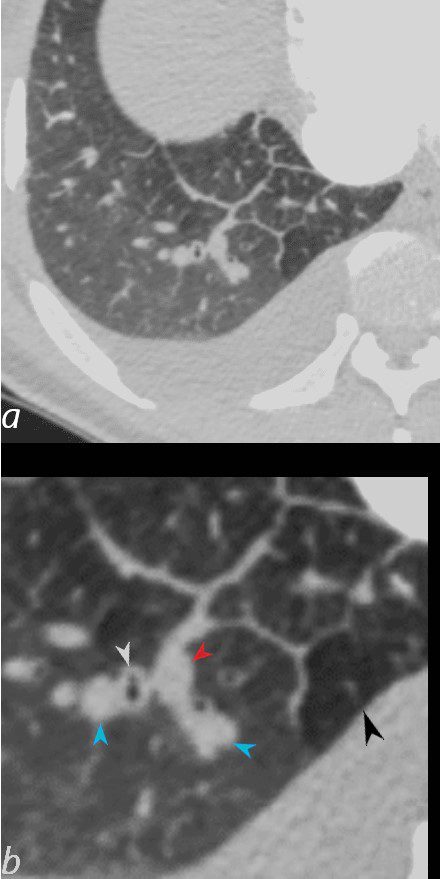
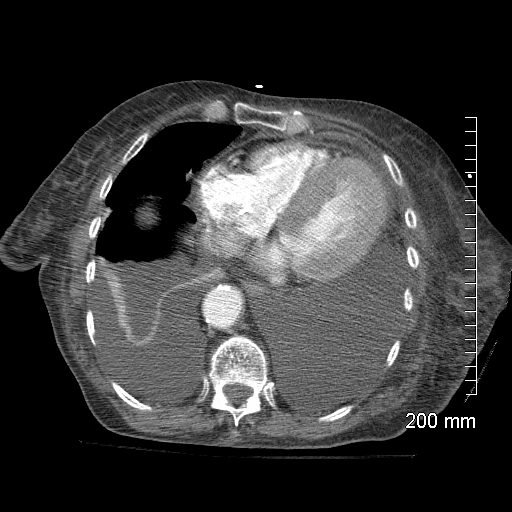
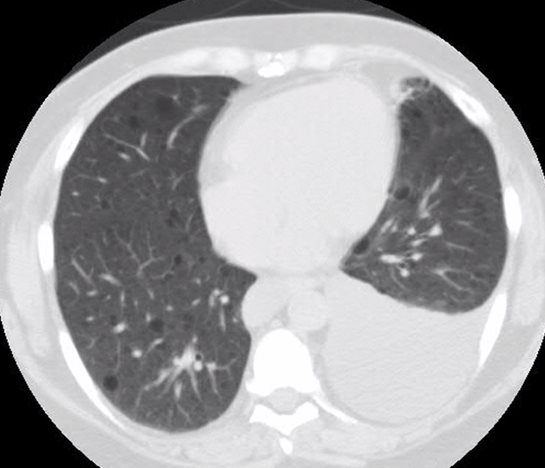
50-year-old female with diabetes, chronic renal failure and congestive heart failure. CT in the axial plane through the right posterior recess, shows thickened interlobular septa at the right base, congested arterioles (light blue arrowheads, b), alongside the bronchioles, peribronchial cuffing (white arrowheads, b), a congested pulmonary venule in the interlobular septum (red arrowhead arrowheads, b), ground glass changes and a secondary lobule demonstrating mosaic attenuation (black arrowhead arrowheads, b). The IVC is dilated and a small complex effusion is present.
Ashley Davidoff MD TheCommonvein.net 135783cL 193Lu

Ashley Davidoff MD TheCommonvein.net 50-010-CT
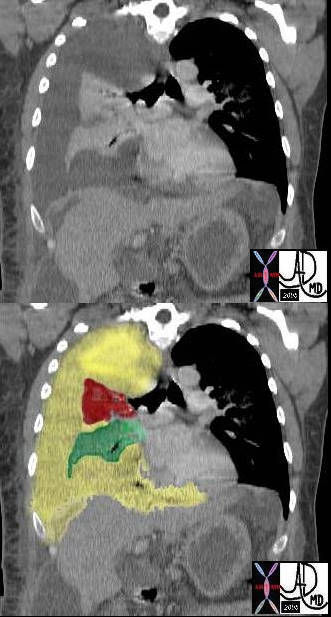
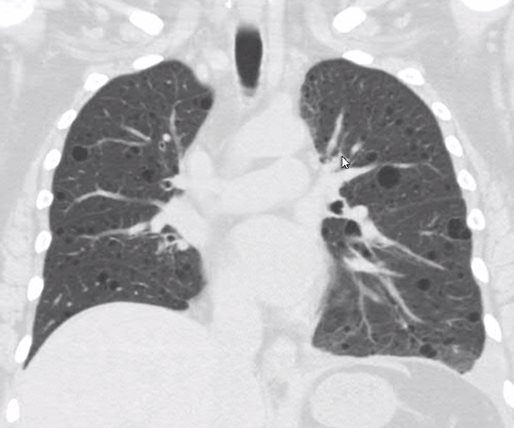
In this case there a large right sided pleural effusion (yellow) with secondary atelectasis of the right lung. (red and green) This coronal CT of the chest at the level of the left ventricle shows a large right pleural effusion which lies between the visceral and parietal pleura. Once the effusion is large enough to weaken the capillary forces that hold the parietal and visceral pleura together, it fail, and the lung collapses which is what is noted on this image – ie total lung collapse because of loss of cohesive adhesive forces.
Courtesy of: Ashley Davidoff, M.D. TheCommonvein.net 42558c
CXR and Pleural Effusion – Blunting of the Costophrenic Angle
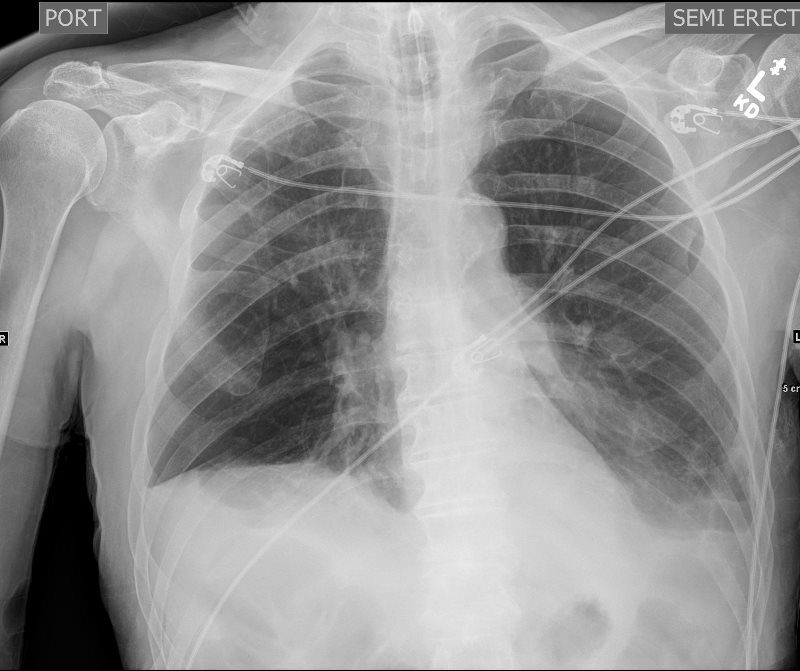
Ashley Davidoff MD
thecommonvein.net
Not Obvious when the Effusion is Small

92-year-old female presents with a dyspnea. CXR shows a moderate sized right effusion. CT scan shows bilateral pleural effusions. On the right there is a moderate effusion with compressive atelectasis and on the left, there is a small effusion with a minor degree of atelectasis with atelectasis of the left lung.
Ashley Davidoff MD TheCommonVein.net
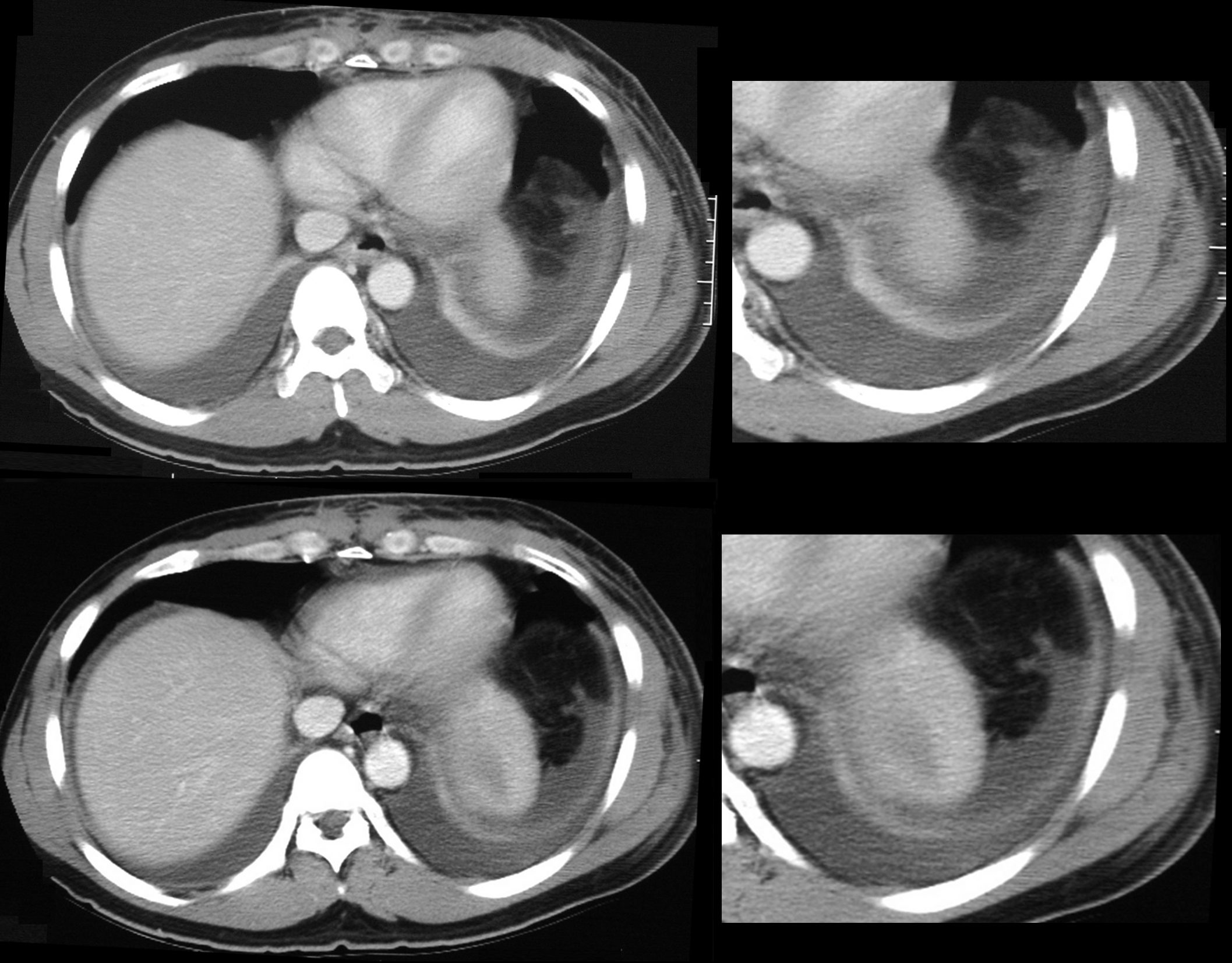
58year old male presents with dyspnea. CT scan shows bilateral pleural effusions with crescentic region of compressive atelectasis in the left lower lobe
Ashley Davidoff MD TheCommonVein.net
79 year-old female with bilateral simple pleural effusions and compressive atelectasis with a variation in the shape of the atelectasis in the right lower lobe.
Ashley Davidoff MD TheCommonVein.net
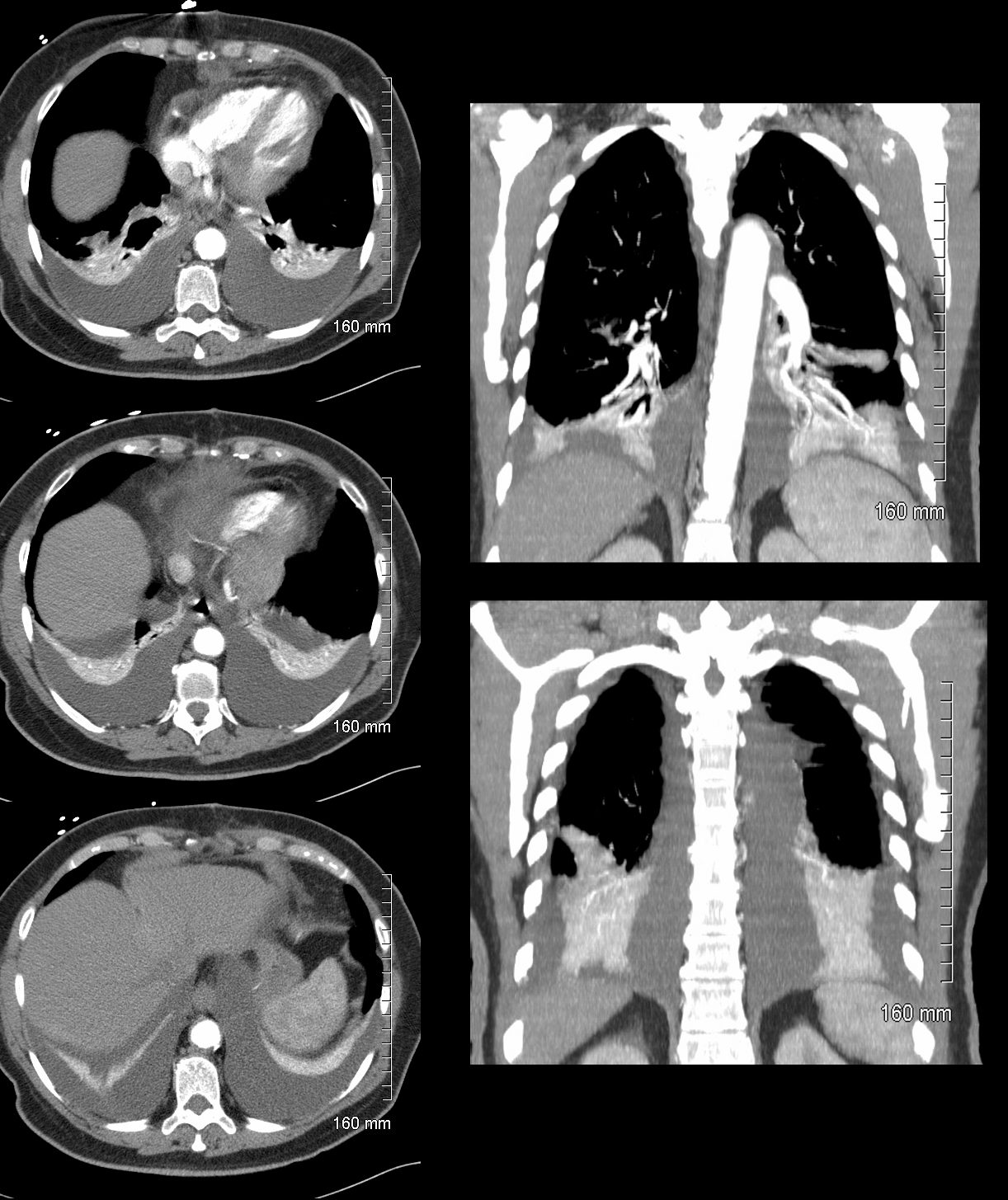
66 year-old female with bilateral simple pleural effusions and compressive atelectasis
Ashley Davidoff MD TheCommonVein.net

86 year-old female presents with a dyspnea. US shows a left effusion with compressive atelectasis. CT scan shows bilateral pleural effusions with atelectasis of the left lung.
Ashley Davidoff MD TheCommonVein.net
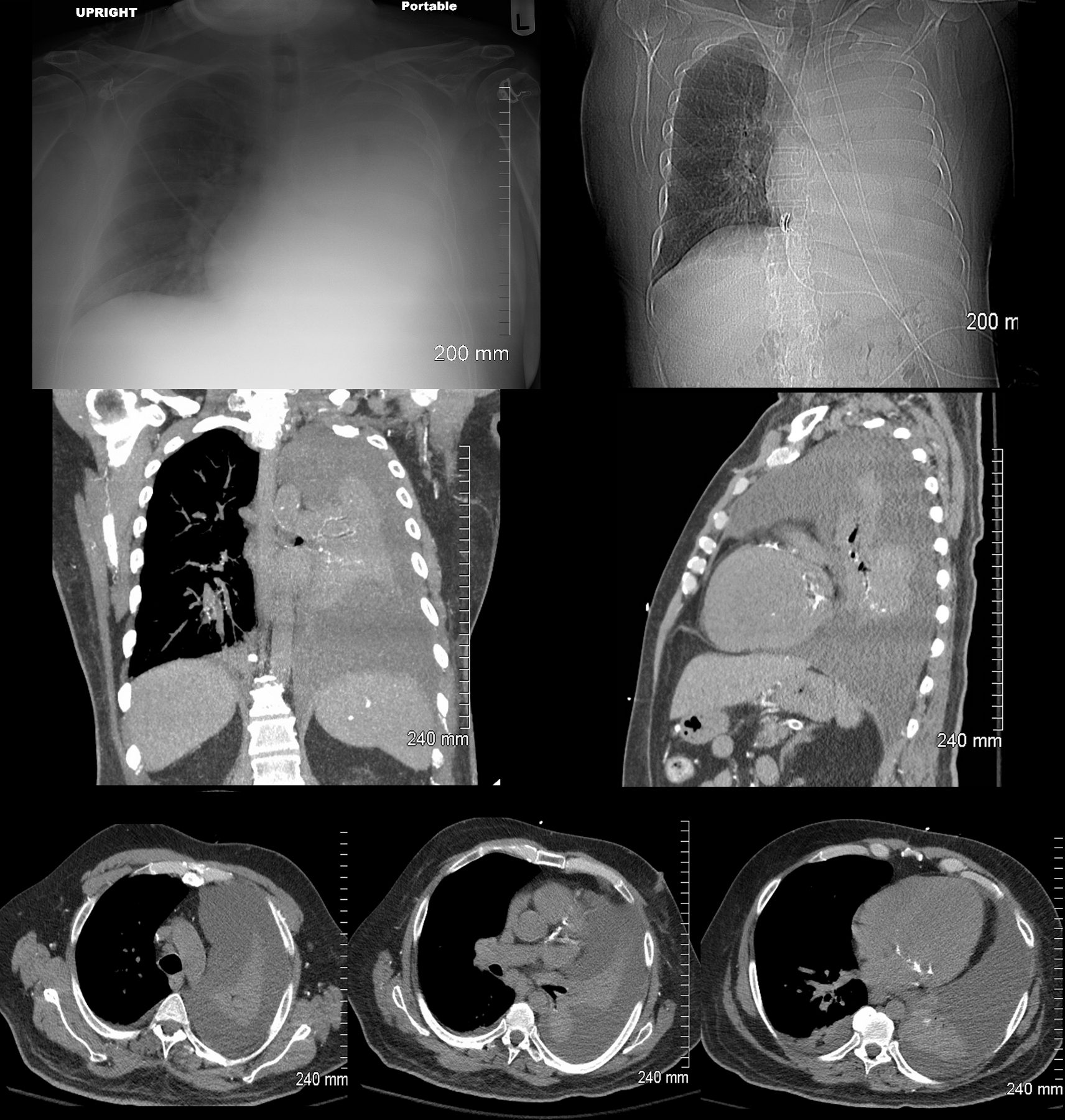
48 year-old male presents with a dyspnea. CXR shows a total white out of the left chest with pulmonary congestion. CT scan shows a large left pleural effusion with total atelectasis of the left lung. Incidental note is made of premature calcific coronary artery disease.
Ashley Davidoff MD TheCommonVein.net
Ashley Davidoff MD TheCommonVein.net
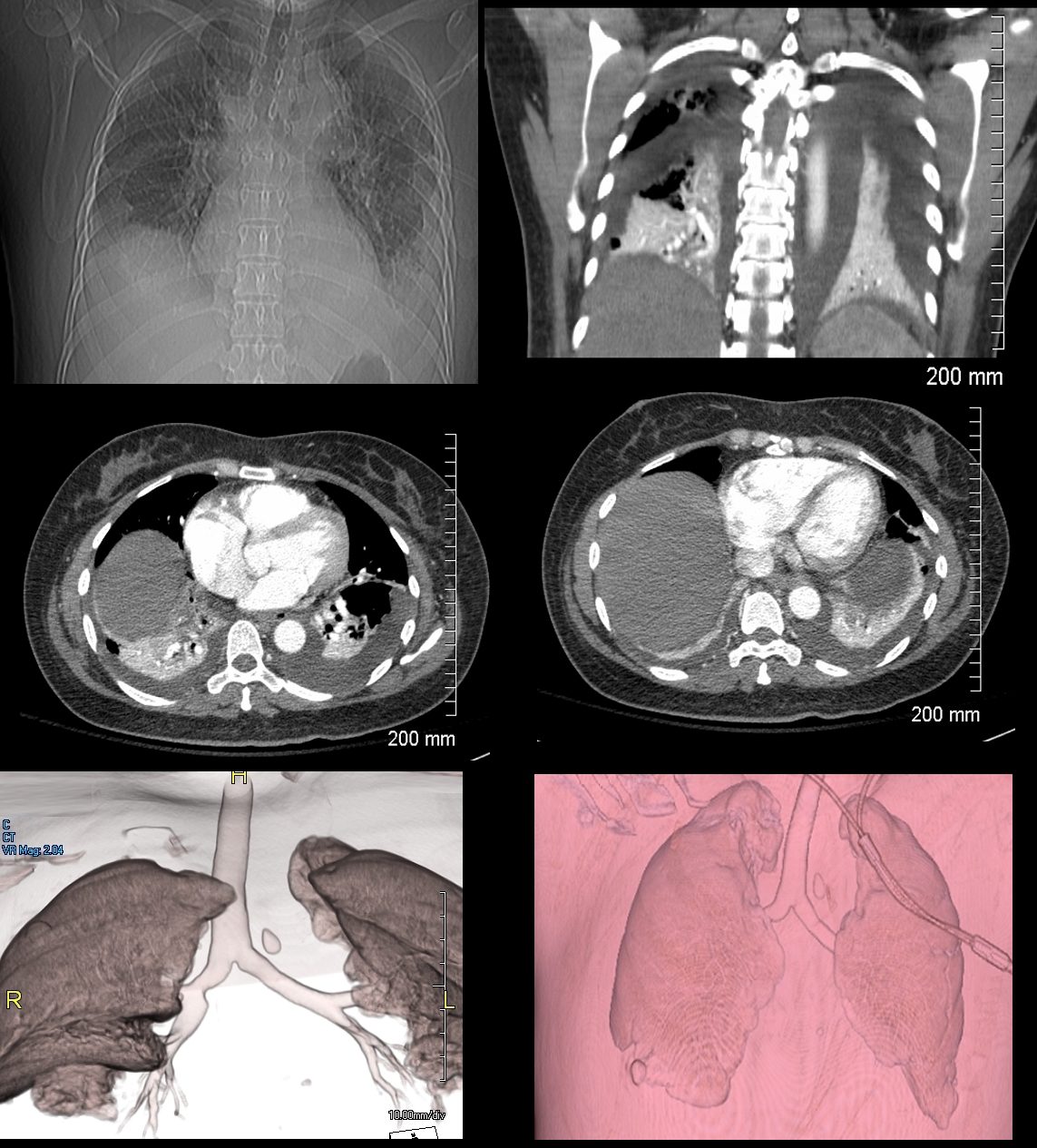
46-year-old female presents with a dyspnea and a cough. Imaging of the chest shows cardiomegaly with bilateral moderate sized pleural effusion with crescentic region of compressive atelectasis noted on the axial images at the bases and crowding of the bronchovascular bundles best evaluated on the coronal image. The 3D reconstructions show functionally “bare” lower lobe segmental airways.
Ashley Davidoff MD TheCommonVein.net
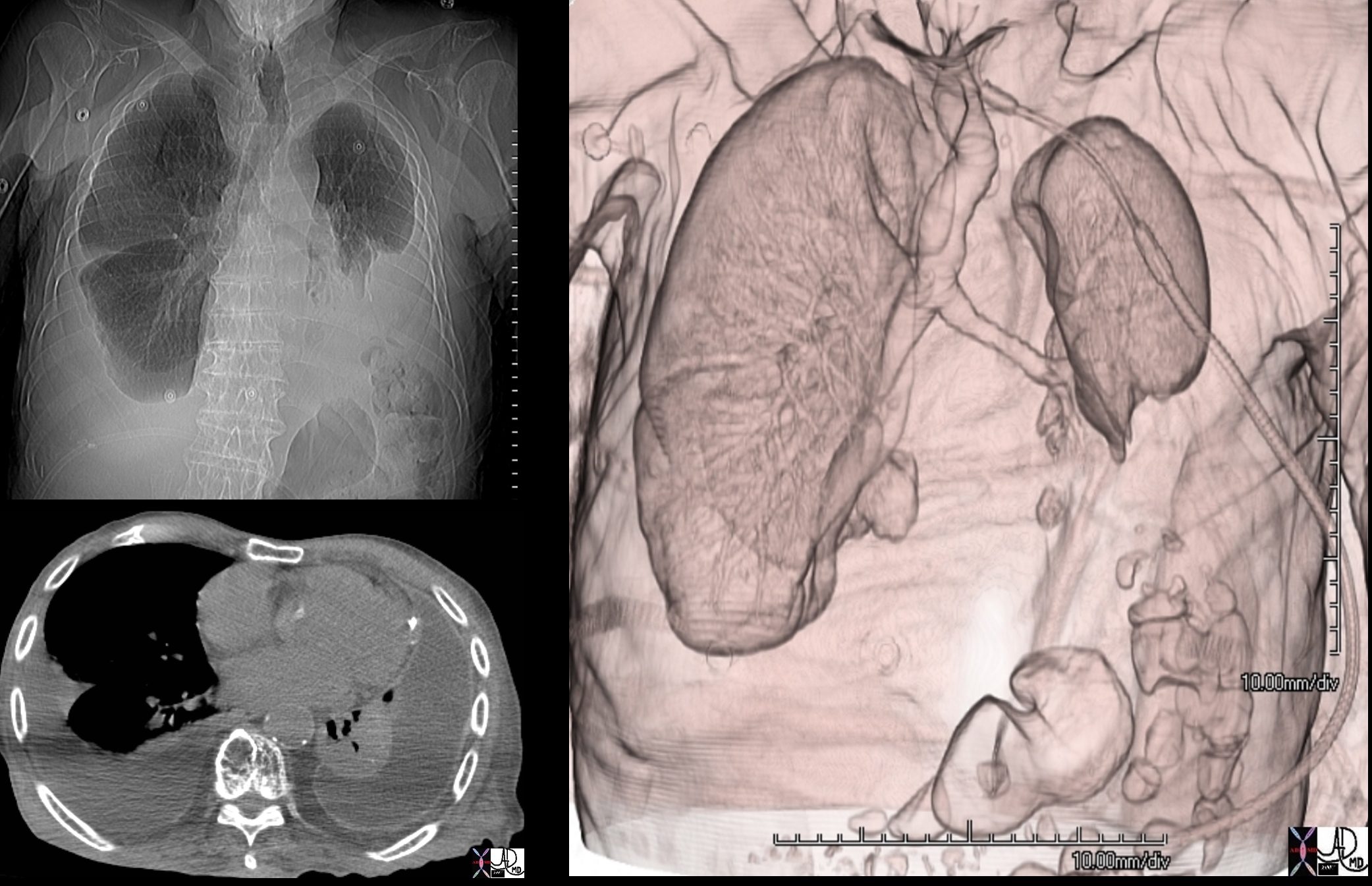
88 year old male with bilateral effusions shown on the CXR. Axial CT shows thickened pleura on the left with compressive atelectasis of the lower lobe and a smaller region of crescentic compressive atelectasis on the right. 3D reconstruction shows atelectasis of the left lower lobe and portion of the lingula
Ashley Davidoff MD TheCommonVein.net
Ashley Davidoff MD
Tension Hydrothorax
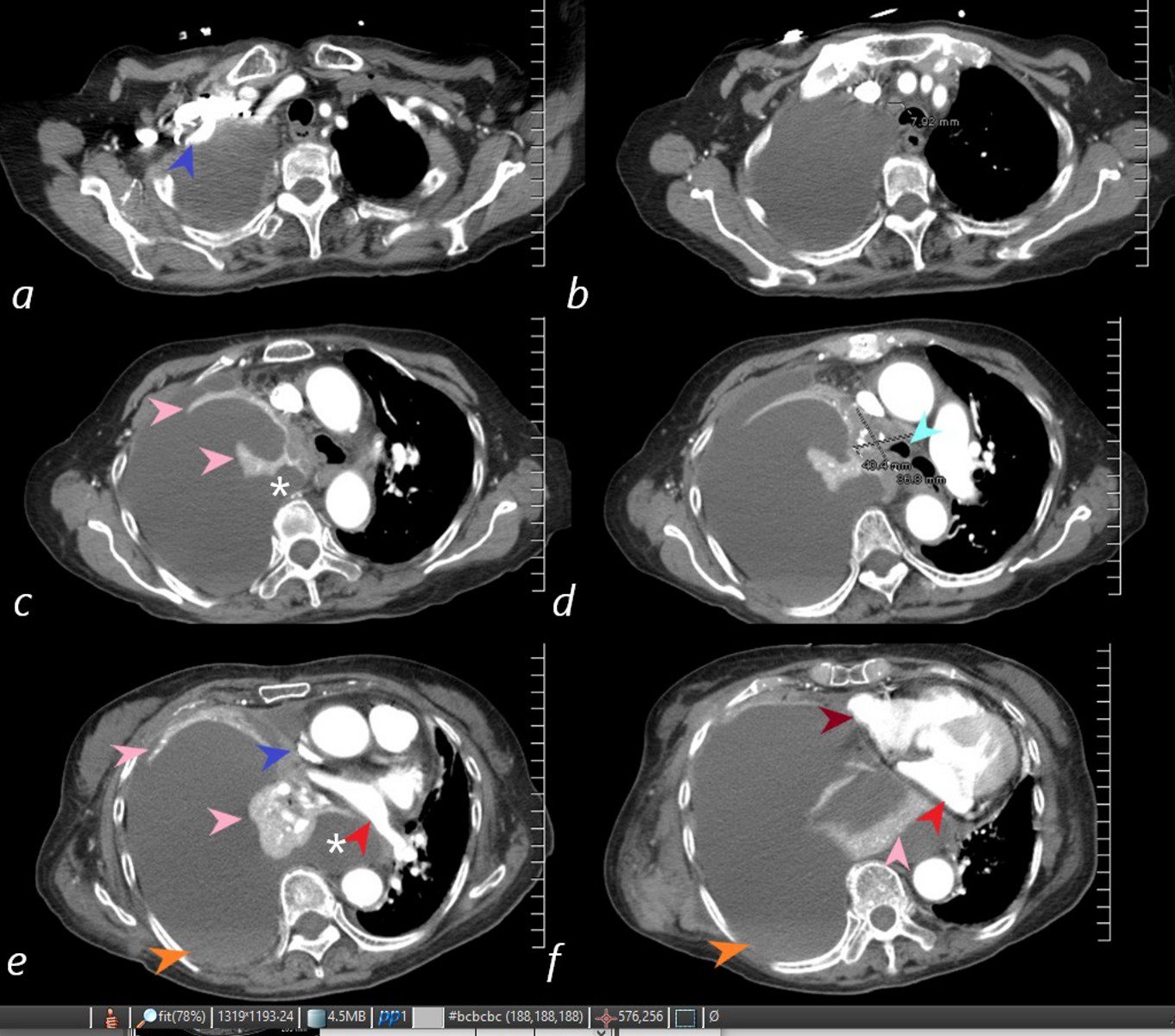
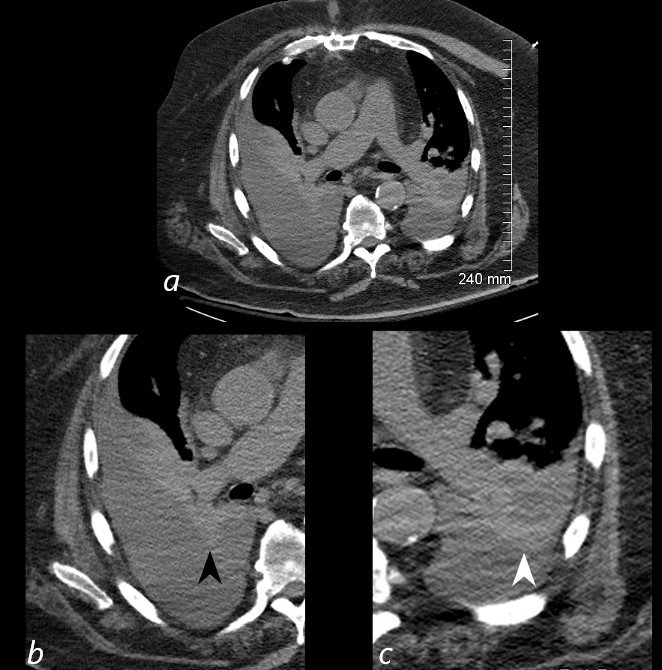
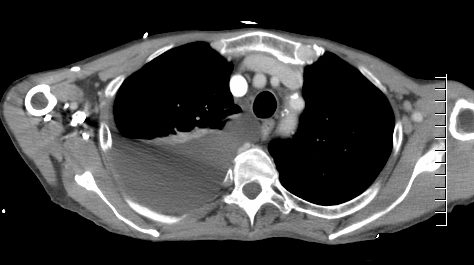
85-year-old female with a history of lung cancer, presents with a dyspnea and hypotension. CT scan shows a large right pleural effusion under pressure, suggestion of blood in the pleural cavity (orange arrowheads e, f) and mediastinal shift to the right. In addition, there is compression of the heart with back up of venous return due the pressure effect on the heart and vascular structures. Among the structures showing compressive effects are the SVC (blue arrowhead, c) with venous distension on right sided upper limb veins (blue arrowhead a). There is also pressure effect on the trachea with narrowing (light blue arrow d) The effusion in the right pleural cavity with atelectatic lung herniates into the left hemithorax, (white asterisk c, e). There is a dense sediment in the pleural fluid (orange arrowheads, e and f) suggesting blood in the pleural cavity. The left atrium is compressed (red arrowhead, e, f), and the right atrium is compressed (maroon arrow f).
Ashley Davidoff MD TheCommonVein.net 106Lu 118450cL

85-year-old female with a history of lung cancer, presents with a dyspnea and hypotension. Reconstruction of the CT scan in the coronal plane, shows a large right pleural effusion under pressure with herniation into the left chest (white asterisk e,and f) , with mediastinal shift to the left (yellow arrowhead b, c, d). In addition, there is compression of the heart with back up of venous return due the pressure effect on the heart and vascular structures. Among the structures showing venous distension are the SVC (blue arrowhead, c) right sided upper limb veins (blue arrowhead d) and the left upper pulmonary veins (red arrowhead, d and f). The density of the systemic venous abd arterial systems is similar, but vascular structures as noted by the green arrowhead in a could represent venous collaterals.
Ashley Davidoff MD TheCommonVein.ne 106Lu 118467cL
Ashley Davidoff MD
thecommonvein.net
Chylous Effusion
Cystic lung disease and an effusion
LAM Diffuse Cysts Chylous Effusion
Imaging of Cystic Lung Disease Thomas Hartman MD Mayo Clinic Video on Imaging Cystic Lung Disease Society of Thoracic Radiology
LAM Diffuse Cysts Chylous Effusion
Imaging of Cystic Lung Disease Thomas Hartman MD Mayo Clinic Video on Imaging Cystic Lung Disease Society of Thoracic Radiology
