- What is it:
- Pneumonia
- typically associated with infection
- BUT
- is a relatively non-specific term,
- refers to:
- A radiological finding characterized by
- lung parenchymal opacities,
- A radiological finding characterized by
- The term “pneumonia” historically referred to
- any lung inflammation before the infectious etiology was established.
- many ILDs for example are considered “pneumonias” and share overlapping imaging features
- e.g.,
- consolidation
- ground-glass opacities,
- fluid accumulation
- interstitial process
- fibrosis
- contributing to diagnostic confusion.
- Pneumonia
-
- typically associated with
-
-
-
- infection (e.g., bacteria, viruses, fungi),
- but other pneumonias include
- non-infectious inflammatory processes.:
- e.g.,
- aspiration, or
- radiation injury).
- also used to label interstitial lung disease (ILD) patterns, including:
- Non-Specific Interstitial Pneumonia (NSIP),
- Usual Interstitial Pneumonia (UIP).
- Lymphocytic Interstitial Pneumonia (LIP),
- Cryptogenic Organizing Pneumonia (COP)
- Acute Interstitial Pneumonia (AIP)
- Desquamative Interstitial Pneumonia (DIP)
- Eosinophilic Pneumonia (EP)
- non-infectious inflammatory processes.:
-
-
-
- Clinical, laboratory, and microbiological correlation is essential to establish the underlying etiology.
- typically associated with
- Etymology:
- Derived from the Greek word pneumon (lung) and the suffix -ia (condition), meaning “condition of the lung.”
- AKA:
- Pulmonary infection, Lung inflammation (when non-infectious).
- How does it appear on each relevant imaging modality:
- Chest X-ray:
- Lobar pneumonia:
- Homogeneous opacity confined to one lobe or segment.
- May show the air bronchogram sign (air-filled bronchi within consolidated lung).
- Bronchopneumonia:
- Patchy, peribronchial opacities scattered throughout both lungs.
- Interstitial pneumonia:
- Reticular or ground-glass opacities, often bilateral and diffuse.
- Associated findings:
- Pleural effusion, cavitation, or lymphadenopathy in complicated cases.
- Lobar pneumonia:
- Chest CT:
- Parts:
- Involves alveoli, interstitium, or both.
- Size:
- Localized (lobar or segmental) or diffuse (multifocal or bilateral).
- Shape:
- Confluent, patchy, or reticular depending on the type.
- Position:
- Lobar: Often unilateral and segmental.
- Bronchopneumonia: Diffuse, peribronchial distribution.
- Interstitial: Diffuse, peripheral, or lower lobe predominant.
- Character:
- Consolidation (dense opacity with air bronchograms).
- Ground-glass opacities (less dense, representing alveolar/interstitial filling).
- Time:
- Resolves with treatment but may evolve into complications (e.g., abscess, fibrosis).
- Parts:
- Ultrasound:
- Useful for detecting:
- Subpleural consolidations.
- Associated pleural effusions.
- Useful for detecting:
- MRI:
- Rarely used but may highlight soft-tissue involvement in cases of necrotizing pneumonia or empyema.
- Chest X-ray:
- These findings reflect:
- Infectious pneumonia:
- Bacterial:
- Streptococcus pneumoniae (lobar pneumonia).
- Staphylococcus aureus (abscess, pneumatoceles).
- Viral:
- Influenza, RSV, or COVID-19 (diffuse, interstitial opacities).
- Fungal:
- Aspergillus or Histoplasma (nodular or cavitary lesions).
- Bacterial:
- Non-infectious inflammatory pneumonia:
- Organizing pneumonia (e.g., cryptogenic or secondary to autoimmune disease).
- Aspiration pneumonia (dependent lobe involvement).
- Infectious pneumonia:
- Differential diagnosis:
- Non-infectious lung disease:
- Pulmonary edema (cardiogenic or non-cardiogenic).
- Atelectasis (volume loss with shift of structures).
- ARDS (acute respiratory distress syndrome).
- Infectious mimics:
- Tuberculosis.
- Fungal infections (e.g., histoplasmosis, coccidioidomycosis).
- Malignant mimics:
- Bronchoalveolar carcinoma.
- Lymphoma with pulmonary involvement.
- Non-infectious lung disease:
- Recommendations:
- Correlate imaging findings with clinical symptoms (e.g., fever, cough, dyspnea) and laboratory markers (e.g., elevated WBC count, positive cultures).
- Perform Chest CT if:
- Findings are atypical or diagnostic uncertainty persists.
- Consider bronchoscopy or lung biopsy in cases of non-resolving pneumonia to exclude malignancy or non-infectious etiologies.
- Use follow-up imaging to confirm resolution, particularly in high-risk patients.
- Key points and pearls:
- Pneumonia findings on imaging are non-specific and require clinical correlation to establish the etiology since it spans a broad group of findings that include
- consolidation
- ground-glass opacities,
- fluid accumulation
- interstitial process
- fibrosis
- Air bronchograms are a hallmark of consolidation and strongly suggest alveolar filling.
- Lobar pneumonia is often bacterial, while interstitial patterns suggest viral or atypical organisms.
- Pneumonia may mimic or co-exist with malignancies or chronic lung diseases; persistent findings warrant further evaluation.
- Ultrasound is particularly valuable for bedside assessment in critically ill patients.
- Pneumonia findings on imaging are non-specific and require clinical correlation to establish the etiology since it spans a broad group of findings that include
Pneumonia Etmology
- The word “pneumonia”
- from the Greek word
- “pneumon,” which means “lung.” and
- “-ia,” which is a suffix used to indicate a condition or state.
- from the Greek word
- Therefore, “pneumonia” translates to
- “lung condition” or
- “lung disease” in Greek. This is fitting given that pneumonia is a respiratory condition characterized by inflammation of the lungs, often caused by infection.
Infection
- Pneumonia
- general term
- filling the alveoli.
- usually purulent, (ie infection)
- generally caused by infecction but entities such as DIP (Desquamative Interstitial Pneumonia), LIP (Lymphocytic Interstitial Pneumonia), NSIP (Nonspecific Interstitial Pneumonia), UIP (Usual Interstitial Pneumonia), COP (Cryptogenic Organizing Pneumonia), and OP (Organizing Pneumonia)—refer to specific patterns of interstitial lung diseases and are called pneumonia but they fall under the broader category of pneumonitis, or inflammation of the lung tissue.
- general term
Pneumonias can be classified by:
- etiology
- infective agent
- bacterial (pyogenic) pneumonia
- cavitating bacterial pneumonia
- fungal pneumonia
pneumocystis pneumonia (PCP)
mycobacterial pneumonia
viral pneumonia
coronavirus
COVID-19
Middle East respiratory syndrome (MERS) infection
severe acute respiratory syndrome (SARS)
varicella pneumonia
setting of infection
community-acquired pneumonia
hospital-acquired pneumonia (HAP)
ventilator-associated pneumonia (VAP)
healthcare-acquired pneumonia (HCAP)
aspiration pneumonia
lipid: lipoid pneumonia
method of spread (a pathological description)
bronchopneumonia
lobar pneumonia
multilobar pneumonia
radiographic appearance
atypical pneumonia
round pneumonia
cavitating pneumonia
hemorrhagic pneumonia
- bacterial (pyogenic) pneumonia
- infective agent
TB
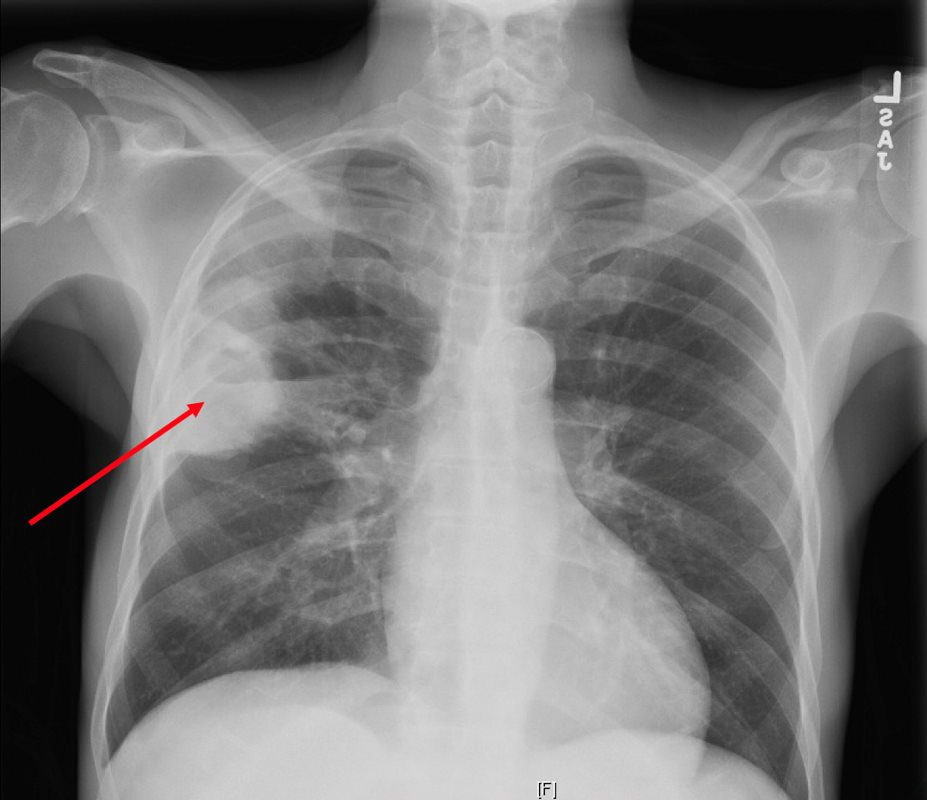
CXR reveals a dense consolidation in the right upper lobe (red arrow) with questionable air-fluid level. No pneumothorax. No pleural effusions. Differential includes right upper lobe pneumonia or tuberculosis. CT is recommended for further evaluation if there is concern for a cavity.
Courtesy Joseph Cannella,
Dr. Christina LeBedis, MD, MS
Courtesy Joseph Cannella,
Dr. Christina LeBedis, MD, MS
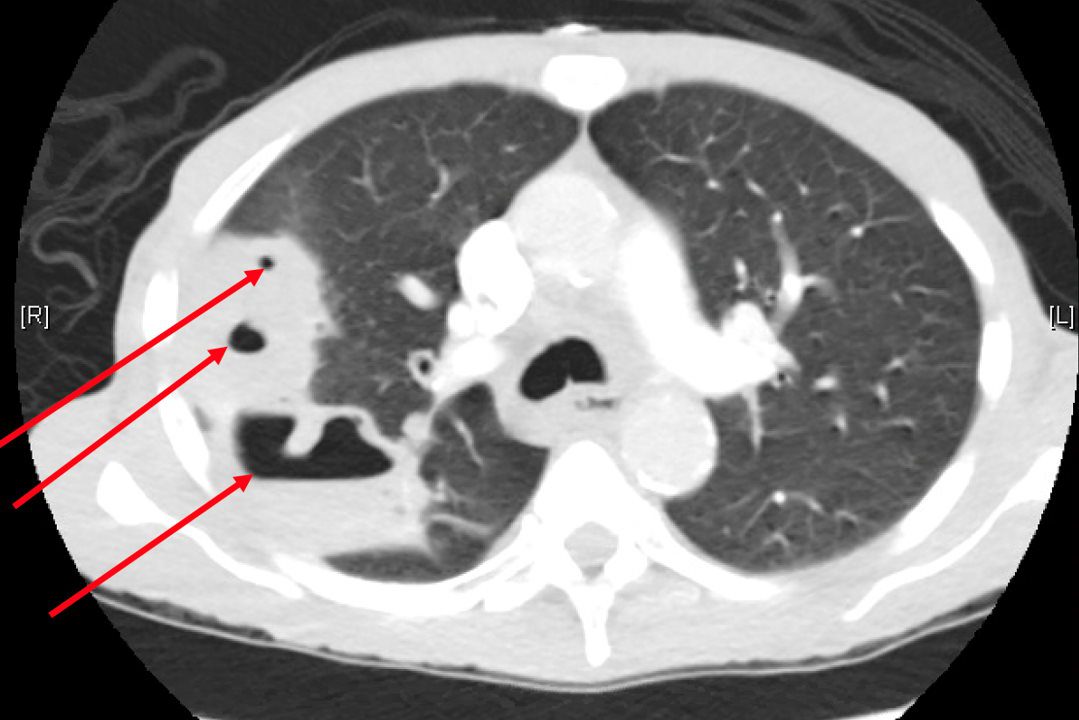
 Bronchopneumonia- Centrilobular
Bronchopneumonia- Centrilobular
lung axial interstitium bronchioles connective tissue fx bronchial plugging peribronchial halo peribronchial thickening dx bronchopneumonia CTscan Davidoff MD 47614c01
Links and References
- Videos
- AUR
Title web link Infection in the Immuno-competent Patient AUR Cardiothoracic Imaging Infection in the Immuno-compromised Patient AUR Cardiothoracic Imaging
- AUR
