-
Etymology
- Derived from the term bronchiolitis, indicating inflammation of the small airways, and interstitial lung disease (ILD), referring to a group of disorders affecting the lung interstitium. RB-ILD is named for its association with respiratory bronchiolitis and its progression into interstitial lung pathology.
AKA
- RB-ILD
- Smoking-related interstitial lung disease
What is it?
- RB-ILD is a smoking-related interstitial lung disease characterized by inflammation and macrophage accumulation in the respiratory bronchioles and adjacent alveoli, progressing to interstitial changes in susceptible individuals. It is considered a clinical-pathologic entity distinct from simple respiratory bronchiolitis.
Caused by:
- Most common cause:
- Cigarette smoking
- Less common causes:
- Inflammation:
- Chronic exposure to secondhand smoke
- Other:
- Possible genetic predisposition in some individuals
- Inflammation:
Resulting in:
- Diffuse interstitial inflammation and fibrosis
- Chronic cough and dyspnea
- Reduced gas exchange
Structural Changes:
- Pigmented macrophage accumulation in respiratory bronchioles
- Peribronchiolar and interstitial inflammation
- Mild to moderate fibrosis in chronic cases
Pathophysiology:
- Chronic exposure to cigarette smoke leads to macrophage activation in the respiratory bronchioles, with subsequent inflammation and damage to surrounding alveoli and interstitial tissues. Persistent inflammation can result in interstitial fibrosis and impaired pulmonary function.
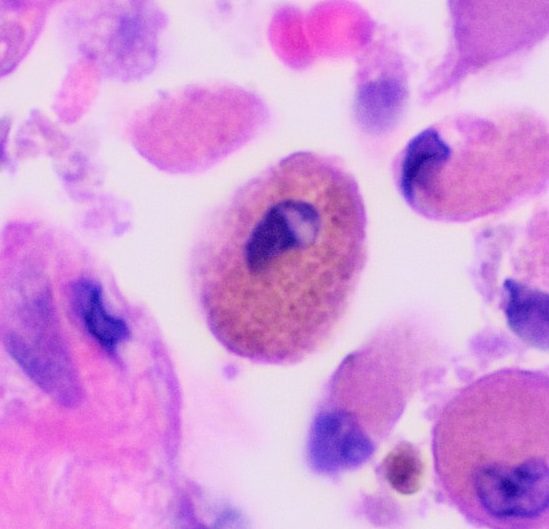
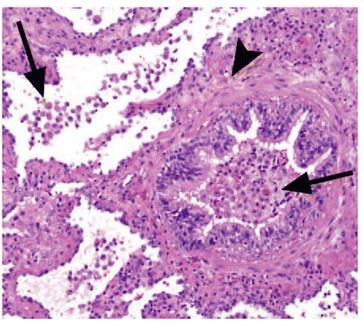
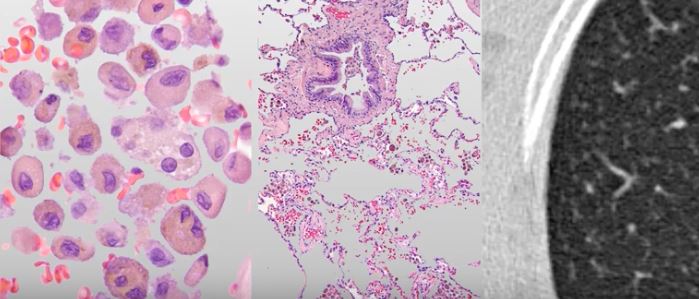
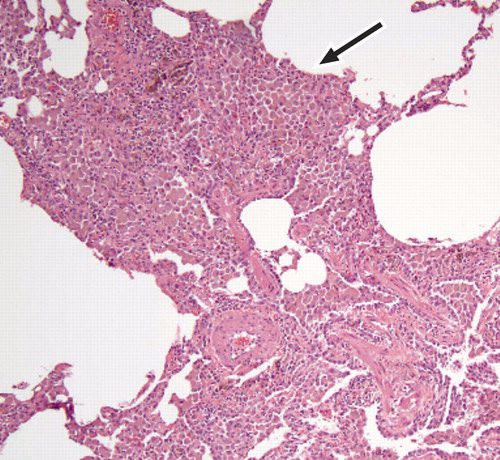
Pathology:
- Accumulation of pigmented macrophages (smoker’s macrophages) in bronchioles and alveoli
- Interstitial thickening with lymphocytic infiltration
- Mild fibrosis and alveolar wall remodeling
Diagnosis
Clinical:
- Symptoms include:
- Insidious onset of dyspnea
- Persistent cough, often with sputum production
- History of significant cigarette smoking
- Physical examination:
- Fine crackles on auscultation
- Cyanosis or clubbing in advanced cases
Radiology:
- CXR:
- Diffuse reticulonodular opacities
- Often subtle and non-specific
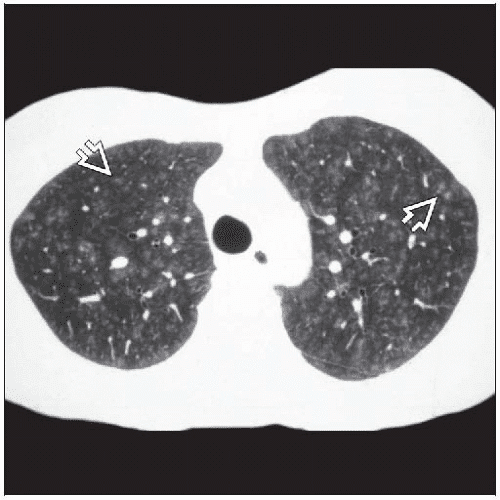
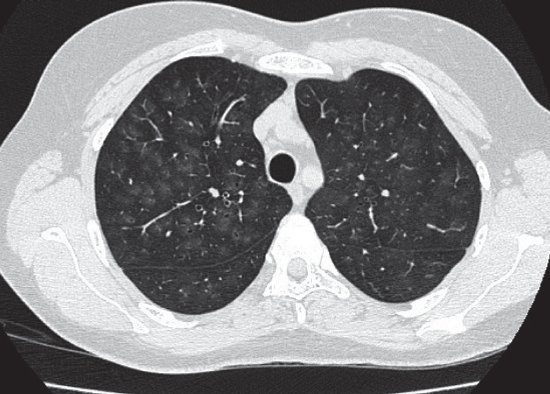
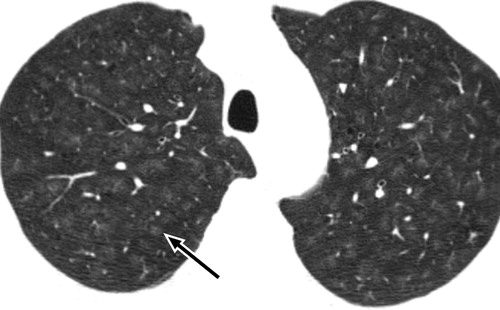
- CT of the Chest:
- Centrilobular nodules
- Ground-glass opacities
- Peribronchiolar thickening
- Mild interlobular septal thickening
Labs:
- Rarely diagnostic but may include:
- ABG abnormalities in advanced disease
- Autoimmune panel to exclude other ILDs
Management:
- Smoking cessation:
- The cornerstone of management, often halting disease progression
- Supportive care:
- Supplemental oxygen in hypoxemic patients
- Pulmonary rehabilitation for symptomatic improvement
- Immunomodulation:
- Corticosteroids in severe or progressive cases
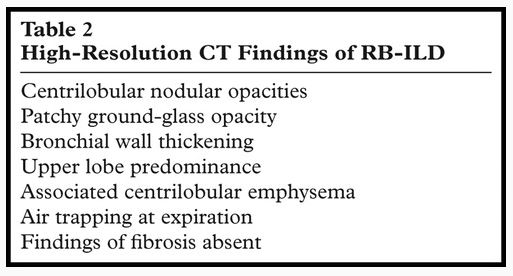
Radiology Detail
CXR
Findings:
- Reticulonodular opacities, more prominent in the mid and upper lung zones
- Hyperinflation in some cases due to coexisting emphysema
Associated Findings:
- Subtle peribronchiolar changes
CT of the Chest
Parts:
- Respiratory bronchioles and adjacent alveoli
Size:
- Centrilobular nodules measuring 1-3 mm
Shape:
- Nodular, ground-glass, or patchy opacities
Position:
- Predominantly upper lobe involvement
Character:
- Peribronchiolar thickening with ground-glass attenuation
Time:
- Chronic, with potential stabilization after smoking cessation
Associated Findings:
- Coexisting emphysema in heavy smokers
- Subtle fibrosis in advanced disease
Other relevant Imaging Modalities
MRI/PET CT/NM/US/Angio:
- MRI: Rarely used but may demonstrate inflammatory changes
- PET-CT: May show low-level metabolic activity in inflammatory areas
Pulmonary Function Tests (PFTs):
- Mild to moderate restrictive pattern
- Decreased diffusion capacity (DLCO) in advanced disease
Recommendations:
- CT of the Chest is the imaging modality of choice for assessing RB-ILD
- Encourage smoking cessation as a primary intervention
- Monitor disease progression with serial pulmonary function tests and imaging
Key Points and Pearls:
- RB-ILD is a smoking-related interstitial lung disease distinct from simple respiratory bronchiolitis.
- CT findings include centrilobular nodules and ground-glass opacities, with upper lobe predominance.
- Smoking cessation is the most critical intervention and can prevent further disease progression.
- Coexisting emphysema may complicate the clinical picture and management.
Etiology Cigarette Smoke
Difference between RB , RB ILD and desquamative interstitial pneumonia (DIP) is that RB has centrilobular findings while RB ILD has centrilobular changes and ground glass changes and DIP has centrilobular findings ground glass changes and cysts.
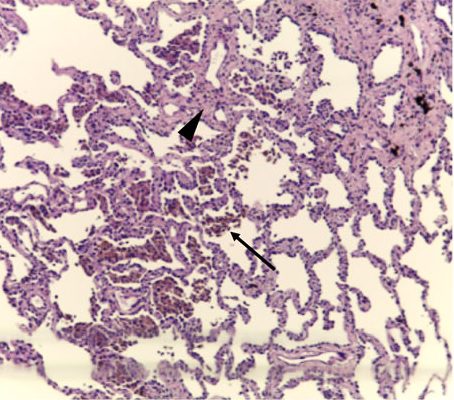
Courtesy Wiki
web lungs 437
Prior permission from The Radiological Society of North America.
Sieminska A, et al Respiratory bronchiolitis-interstitial lung disease Orphanet Journal of Rare Diseases volume 9: 106 (2014)
Courtesy Wiki
web lungs 438
Courtesy Radiology Key
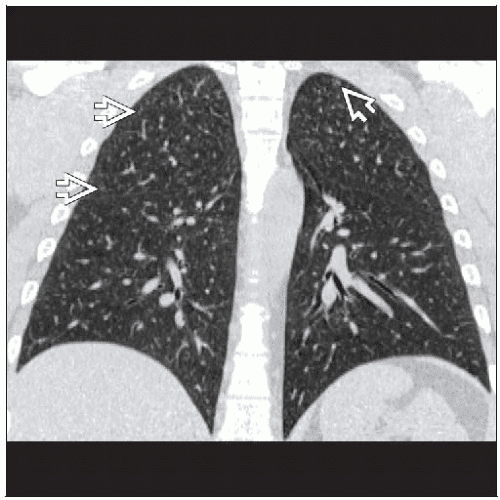
Smoking-Related Interstitial Lung Disease
January 2015Deutsches Ärzteblatt International 112(4):43-50 Hagmeyer L et al
Attili, A.K etal Smoking-related Interstitial Lung Disease: Radiologic-Clinical-Pathologic Correlation RadioGraphics Vol. 28, No. 5 2008
Attili, A.K etal Smoking-related Interstitial Lung Disease: Radiologic-Clinical-Pathologic Correlation RadioGraphics Vol. 28, No. 5 2008
- Histopathology characterized by
-
- pigmented macrophages and
- respiratory bronchioles and alveoli
- mild interstitial inflammatory
- alveolar septa in the peribronchial may be mildly thickened
- no significant fibrosis
-
DIP is similar to RB-ILD,
-
- DIP and RB-ILD are a spectrum
- differing in compartments involved
- DIP not bronchiolocentric.
- hyperplasia of the alveolar type II cells
- distribution pattern more homogeneous a
- mild peribronchial fibrosis
Buzz
Use your words
respiratory bronchiolitis = inflammation of the respiratory bronchioles.
dirty lung appearance
centrilobular lung nodules
ground glass
air trapping
emphysema
Respiratory Bronchiole
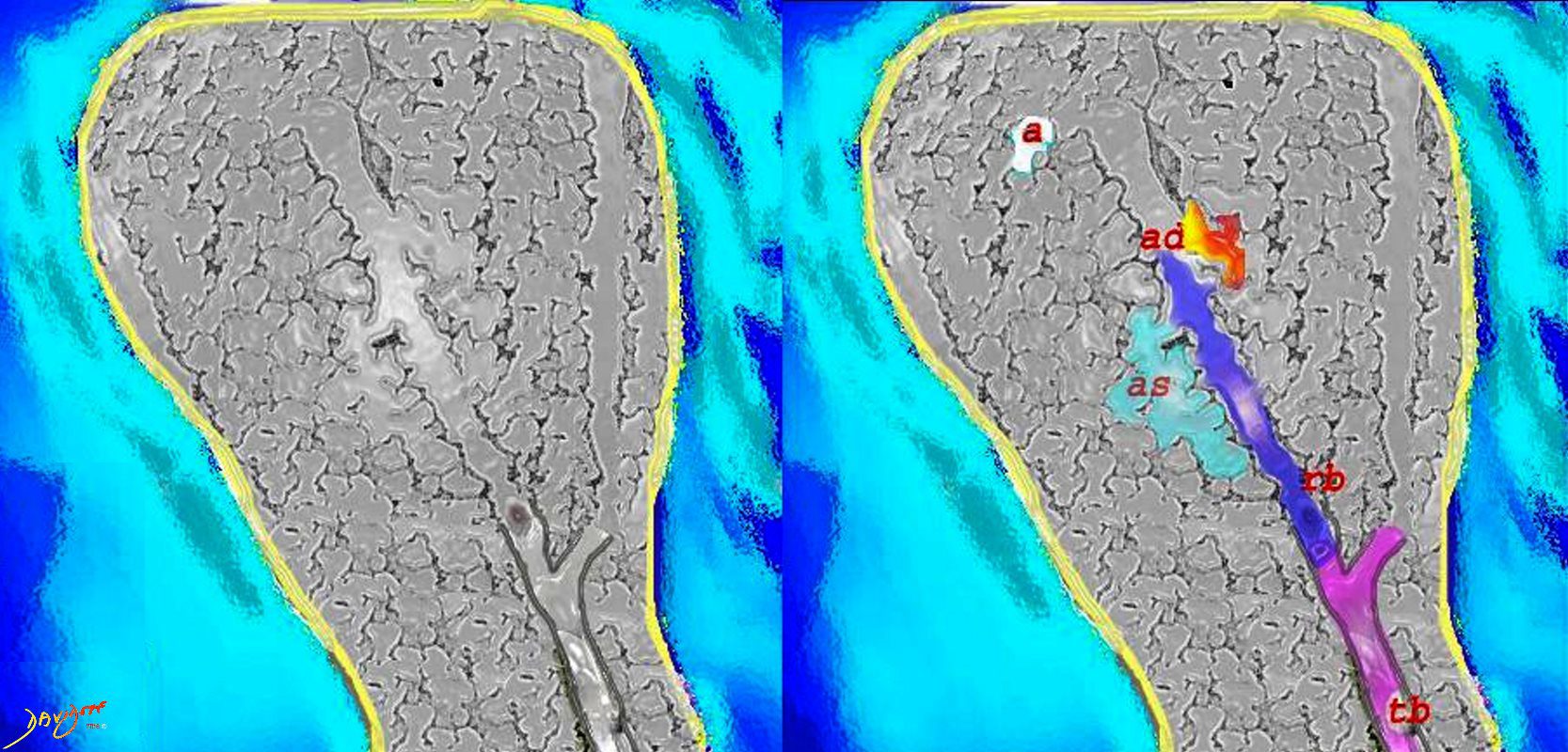
Courtesy Ashley Davidoff MD
lungs-0028-low res
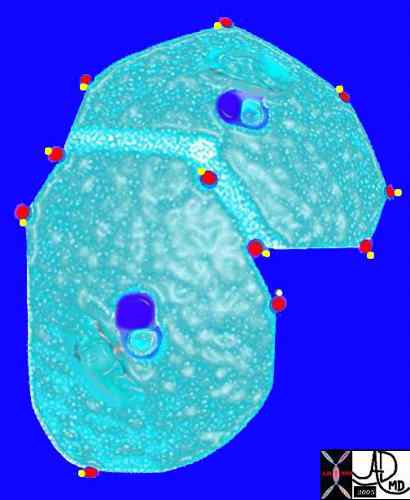
Pulmonary venules (red) and lymphatics (yellow). lie in the periphery of the lobule
42440b03
Davidoff Art Courtesy Ashley Davidoff MD
Secondary Lobule
Inhalation – Upper Lobes
centrilobular ground glass nodules
-
Videos