- Etymology:
- The term “reticular” derives from the Latin word “reticulum,” meaning “net,” describing the net-like or lattice appearance seen in imaging studies of the lungs.
- AKA:
- Reticulonodular pattern (if nodules are also present).
-
What is it?
A reticular pattern refers to a network of interlacing linear opacities in the lungs, typically caused by thickening of the interstitial structures, such as septa or connective tissue.
- Characterized by:
- A fine, coarse, or irregular network of lines creating a web-like appearance.
- May indicate interstitial lung disease or other pathologies involving the lung interstitium.
- Anatomically affecting:
- Pulmonary interstitium, specifically:
- Interstitium of the Secondary Lobule
- The secondary pulmonary lobule is a functional unit of the lung that is typically defined by the structures supplied by a single small bronchiole. In fibrotic lung diseases with a reticular pattern on imaging, the involvement is often related to changes in specific structures within the secondary lobule. The primary structures affected include:
- Interlobular Septum: In the interlobular septa within the secondary pulmonary lobule.
- Involvement in Reticular Disease:
- Fibrosis or scarring of the interlobular septa can lead to
- thickening which can be irregular and incomplete
- increased opacity,
- Fibrosis or scarring of the interlobular septa can lead to
- Intralobular Septa:
- Fibrosis of the intralobular septa (interalveolar septa) can also contribute to the reticular pattern.
- Involvement in Reticular Disease:
- Interlobular Septum: In the interlobular septa within the secondary pulmonary lobule.
- Axial Interstitium: Peribronchovascular Interstitium
- Fibrosis in the peribronchovascular interstitium can lead to a reticular pattern,
- especially if it affects the connective tissue around small bronchioles.
- Subpleural Connective Tissue:
- Fibrosis in the subpleural connective tissue
- The secondary pulmonary lobule is a functional unit of the lung that is typically defined by the structures supplied by a single small bronchiole. In fibrotic lung diseases with a reticular pattern on imaging, the involvement is often related to changes in specific structures within the secondary lobule. The primary structures affected include:
- Pathophysiology:
- The reticular pattern arises due to fibrosis, inflammation, or fluid accumulation within the interstitial compartments of the lungs.
- Chronic conditions may lead to distortion of normal lung architecture and impaired gas exchange.
- Causes include:
-
- Most Common Causes:
- Circulatory:
- Pulmonary Edema (cardiogenic or non-cardiogenic).
- Infection:
- Viral pneumonias.
- Fungal infections.
- Inflammation:
- Idiopathic Pulmonary Fibrosis (IPF).
- Non-Specific Interstitial Pneumonia (NSIP).
- Sarcoidosis.
- Hypersensitivity Pneumonitis.
- Other Causes include:
- Neoplasm:
- Lymphangitic carcinomatosis.
- Inhalational Diseases:
- Asbestosis.
- Silicosis.
- Autoimmune Diseases:
- Rheumatoid arthritis.
- Systemic sclerosis.
- Infiltrative Diseases:
- Amyloidosis.
- Inherited and Congenital:
- Hermansky-Pudlak syndrome.
- Iatrogenic:
- Radiation-induced fibrosis.
- Idiopathic:
- Cryptogenic organizing pneumonia (COP).
- Neoplasm:
- Circulatory:
- Most Common Causes:
-
- Histopathology:
- The reticular pattern corresponds to interstitial thickening due to fibrosis, edema, inflammation, or cellular infiltration.
- Imaging
- Applied Anatomy:
- Parts:
- Interstitial structures, including septal interstitium intralobular interstitium, axial (bronchovascular), and peripheral interstitium
- Size:
- Fine, medium, or coarse reticulations depending on disease severity.
- Shape
- Linear or branching lines forming a net-like structure.
- Position:
- Varies based on etiology (e.g., diffuse or localized, upper lower lung zones).
- Character:
- Lines may be sharply defined or hazy, depending on associated changes (e.g., fibrosis, edema).
- Time:
- Acute (e.g., pulmonary edema) or chronic (e.g., pulmonary fibrosis).
- Parts:
- Applied Anatomy:
- CXR:
- Appears as a network of linear opacities that can be fine (e.g., early interstitial edema) or coarse (e.g., advanced fibrosis).
- Varies based on etiology (e.g., diffuse or localized, upper lower lung zones). ILD usually predominantly lower lobes
- May co-exist with nodular patterns or ground-glass opacities.
- CT:
- Provides detailed visualization of interstitial thickening.
- Fine reticulations are better seen in high-resolution CT (HRCT).
- Findings include:
- Interlobular septal thickening (e.g., in pulmonary edema).
- Subpleural reticulations (e.g., in idiopathic pulmonary fibrosis).
- Honeycombing in advanced fibrosis.
- Distribution helps narrow differential diagnosis
- e.g.,
- lower lobe in ILD,
- upper lobe in sarcoidosis).
- e.g.,
- MRI:
- Limited role but can identify gross interstitial changes.
- Best used for evaluating concurrent cardiac or mediastinal pathologies.
- PET-CT:
- May show increased metabolic activity in active inflammatory or fibrotic processes.
- Helps differentiate between active disease and stable fibrosis.
- Other:
- Ultrasound can identify pleural thickening or subpleural abnormalities but has limited utility in detecting reticular patterns.
- Differential Diagnosis:
- Interstitial Lung Disease (ILD):
- Idiopathic Pulmonary Fibrosis (IPF).
- Non-Specific Interstitial Pneumonia (NSIP).
- Sarcoidosis.
- Hypersensitivity Pneumonitis.
- Pulmonary Edema:
- Cardiogenic or non-cardiogenic.
- Infections:
- Viral pneumonias.
- Fungal infections.
- Autoimmune Diseases:
- Rheumatoid arthritis.
- Systemic sclerosis.
- Inhalational Diseases:
- Asbestosis.
- Silicosis.
- Recommendations:
- Correlate imaging findings with clinical presentation and laboratory tests (e.g., autoimmune markers, infection workup).
- High-resolution CT (HRCT) for detailed assessment.
- Pulmonary function tests (PFTs) to evaluate restrictive lung disease.
- Biopsy in cases of unclear etiology or to confirm specific interstitial lung diseases.
- Key Points and Pearls:
- A reticular pattern is a hallmark of interstitial involvement and may indicate a wide range of diseases.
- Lower lobe-predominant reticulations are characteristic of ILD , while upper lobe involvement suggests sarcoidosis or chronic hypersensitivity pneumonitis.
- Cardiomegaly on imaging would suggest interstitial edema, while elevated inflammatory markers could point to active infection or inflammation.
- Honeycombing on CT signifies advanced fibrosis and often poor prognosis.
- Early recognition and differentiation of causes are essential for targeted management.
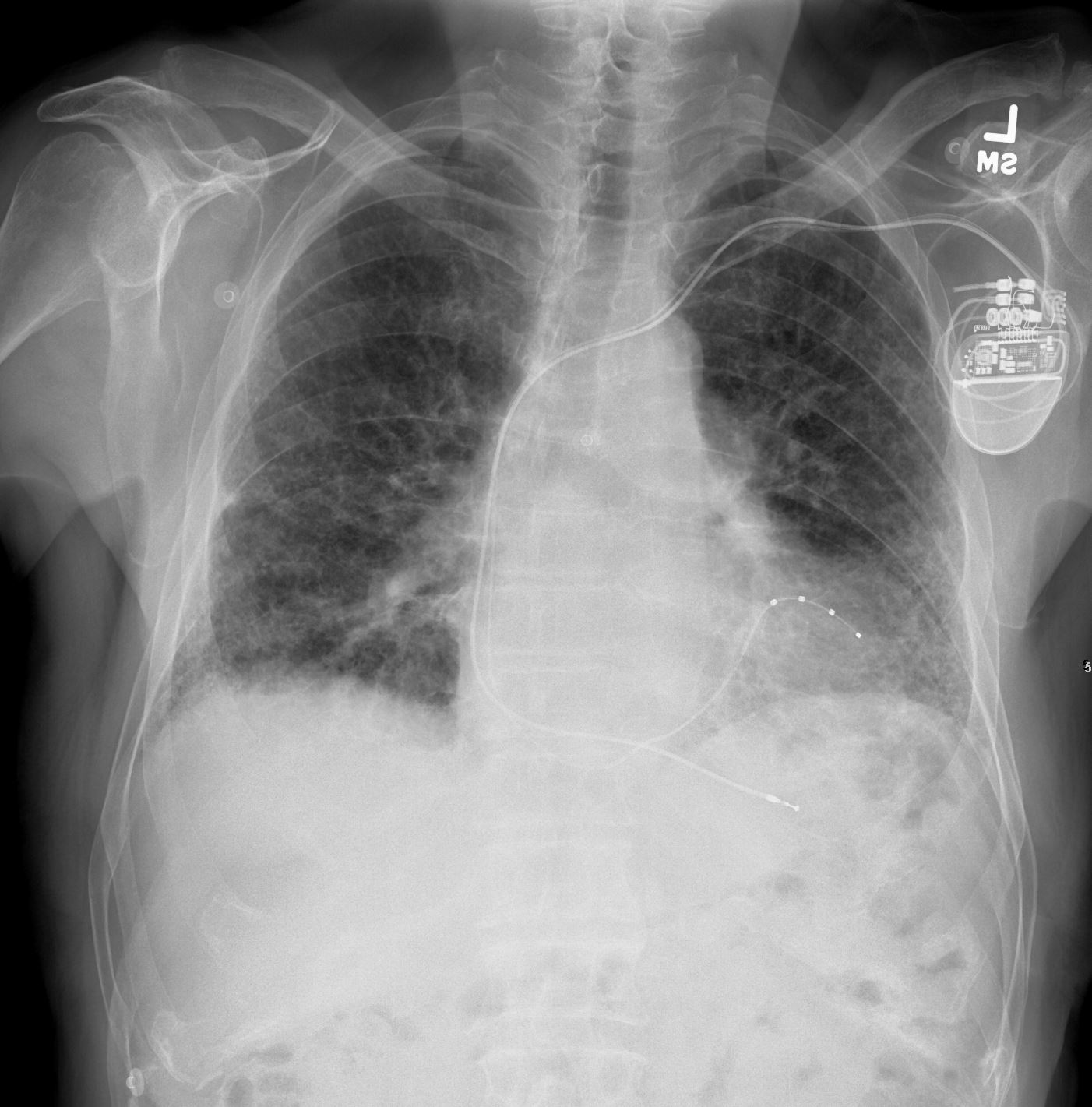
Reticular Pattern on CXR

Frontal CXR shows diffuse interstitial prominence with a reticular pattern with mild upper lobe lucency likely related to upper lobe centrilobular emphysema
Ashley Davidoff MD
The CommonVein.net 139244 28Lu
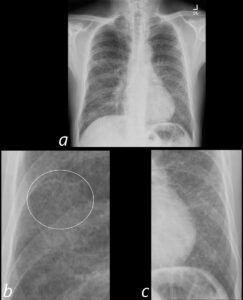
Frontal CXR shows diffuse interstitial prominence with a reticular pattern (ringed in b) resulting from thickening of the interlobular septa
Ashley Davidoff MD
The CommonVein.net 139244 28Lu
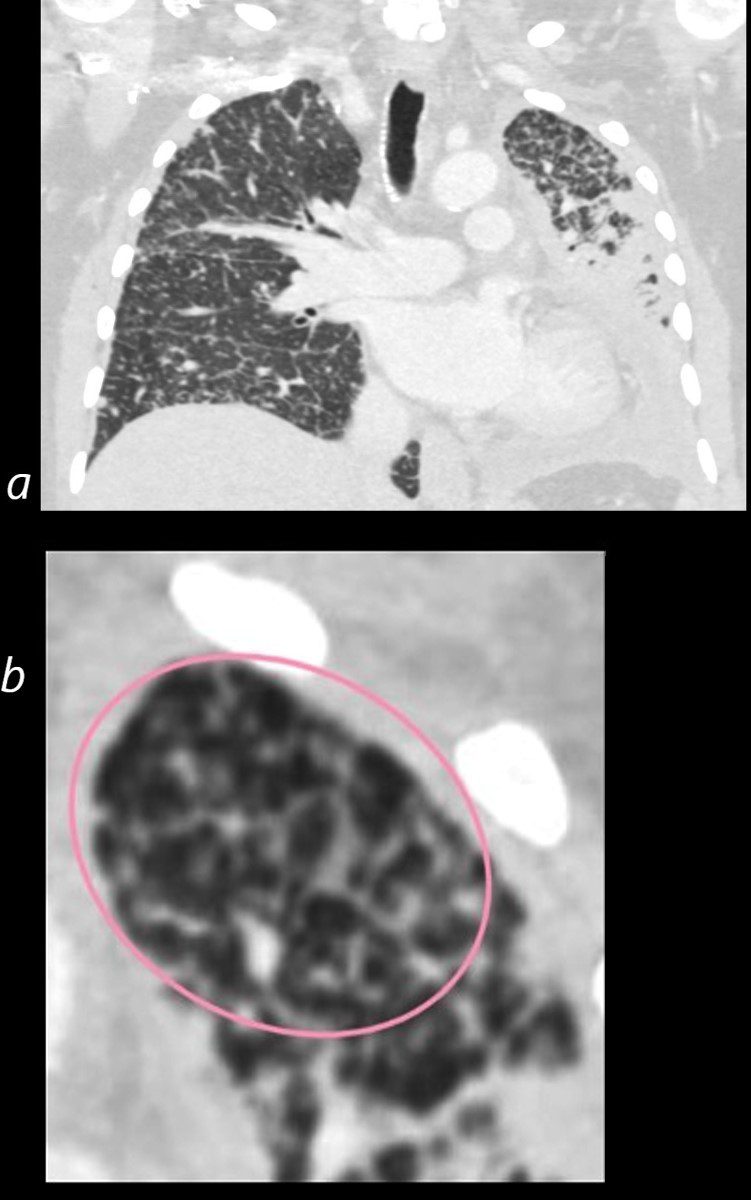
In this patient the reticular pattern is superimposed on centrilobular emphysema and is associated with new multifocal GGO’s as well as new small basilar cysts raising the possibility of LIP (HIV history)
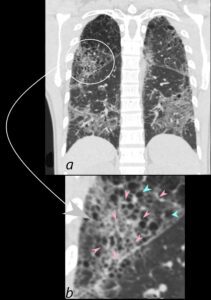
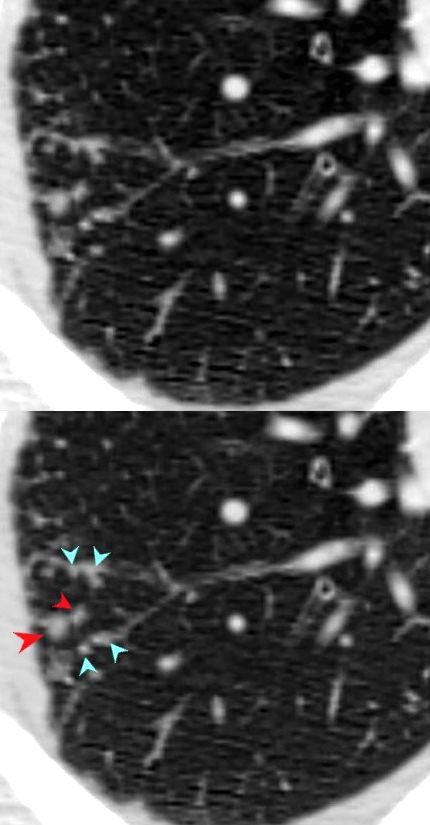
CT scan in coronal projection (a) shows multifocal regions of ground glass opacity in both the lower and upper lobes, associated with mild centrilobular emphysema. The right upper lobe changes are magnified in b and show a reticular pattern as a result of interlobular septal thickening (pink arrowheads in b) The cystic changes (teal blue arrowheads) are part of an underlying emphysematous process.
Ashley Davidoff MD
The CommonVein.net 139260c01L 28Lu
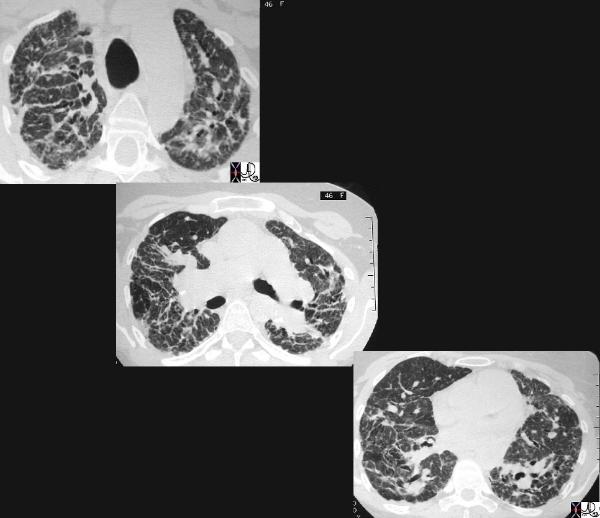
CT scan in coronal projection shows multifocal regions of ground glass opacity in both the lower and upper lobes, and mild centrilobular emphysema. The lower lobe changes are magnified in b and c and show multifocal regions of ground glass opacity , with thickening of the interlobular septa and the presence of new small bibasilar cysts (red arrowheads b and c)
LIP (lymphocytic interstitial pneumonia) is included in the radiological differential diagnosis
Ashley Davidoff MD
The CommonVein.net 139260c02L 28Lu

CT scan in shows multifocal regions of ground glass opacity in both the lower and upper lobes, mild progressive centrilobular emphysema but the presence of some small basilar cysts
LIP (lymphocytic interstitial pneumonia) is included in the radiological differential diagnosis
Ashley Davidoff MD
The CommonVein.net 139260cL 28Lu
Hemorrhage
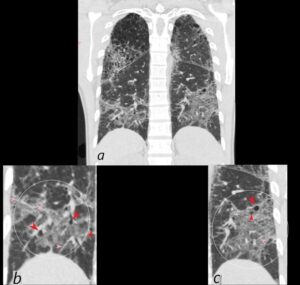
75-year-old man on blood thinners s/p aortic valve replacement, s/p trauma, presents with hemoptysis. He was afebrile and without an elevated white count
Axial CT at the level below the carina shows heterogenous changes of the secondary lobules. The changes in the posterior segment of the right upper lobe (a magnified below in b and c ) and show secondary lobules with ground glass changes (white rings) It is difficult to distinguish those with normal lung parenchyma and those with mosaic attenuation. It is hypothesized that those with prominent centrilobular nodules (black rings c) more than likely represent mosaic attenuation due to small airway disease. The lower density secondary lobules which do not have a prominent centrilobular nodule (c, purple rings), may either reflect normal parenchyma or mosaic attenuation. The orange rings likely reflect consolidation in side-by-side secondary lobules.
Ashley Davidoff MD TheCommonVein.net 165Lu 135854cL01
CHF
CT scan shows Diffuse ground glass pattern with thickening of the interlobular septa and manifesting as crazy paving pattern
Ashley Davidoff MD TheCommonVein.net 131742
Aspiration

Ashley Davidoff MD TheCommonVein.net crazy paving ICU 002
HIV ? Infection
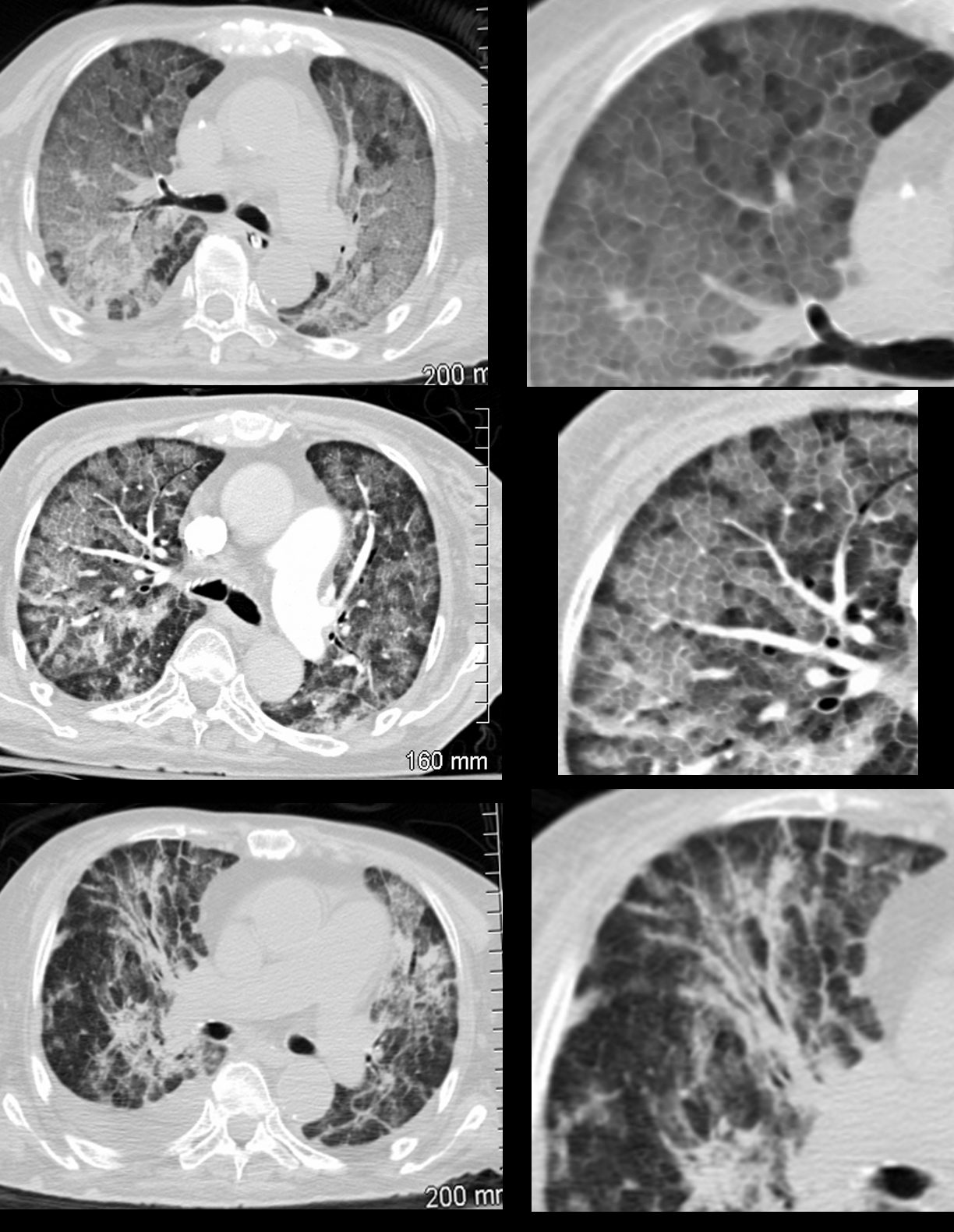
36 year old female with HIV presents with dyspnea. CT scan on presentation (upper images) show extensive disease with crazy paving pattern. Following adjunctive steroid therapy, the patient showed early mild improvement with persistence of crazy paving, peripheral sparing and regions of improved aeration (middle panel). Continued improvement continued subsequently with improved aeration, minimal residual crazy paving and bronchovascular infiltrate ( lower panel).
Ashley Davidoff MD TheCommonVein.net 30755c
Acute Eosinophilic Pneumonia vs COP
60 year old male presents with right sided pleuritic chest pain 15 months ago
CT shows multiple wedge shaped consolidations with some surrounding ground glass (RUL, LUL, LLL), focal nodules and regional segmental regions of ground glass consistent with multifocal pneumonia
Ashley Davidoff MD TheCommonVein.net
NSIP
71-year-old female presents with a history of scleroderma, ILD, hypothyroidism and dcSSc
CT of the lower lobes in the coronal plane, shows extensive ground glass changes with irregular thickening of the interlobular septa.
Ashley Davidoff MD TheCommonVein.net 196Lu 136616
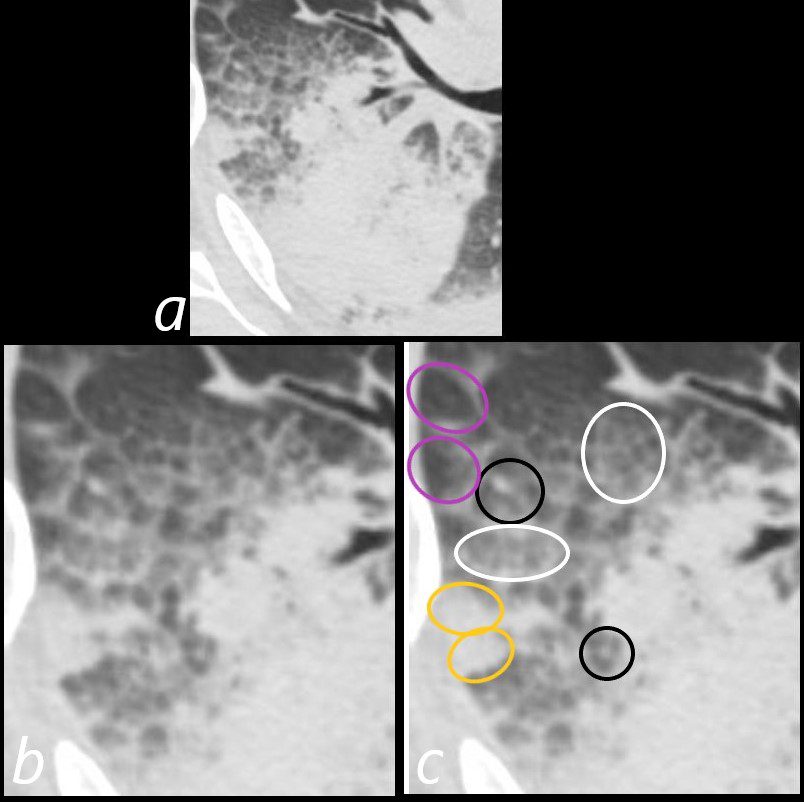
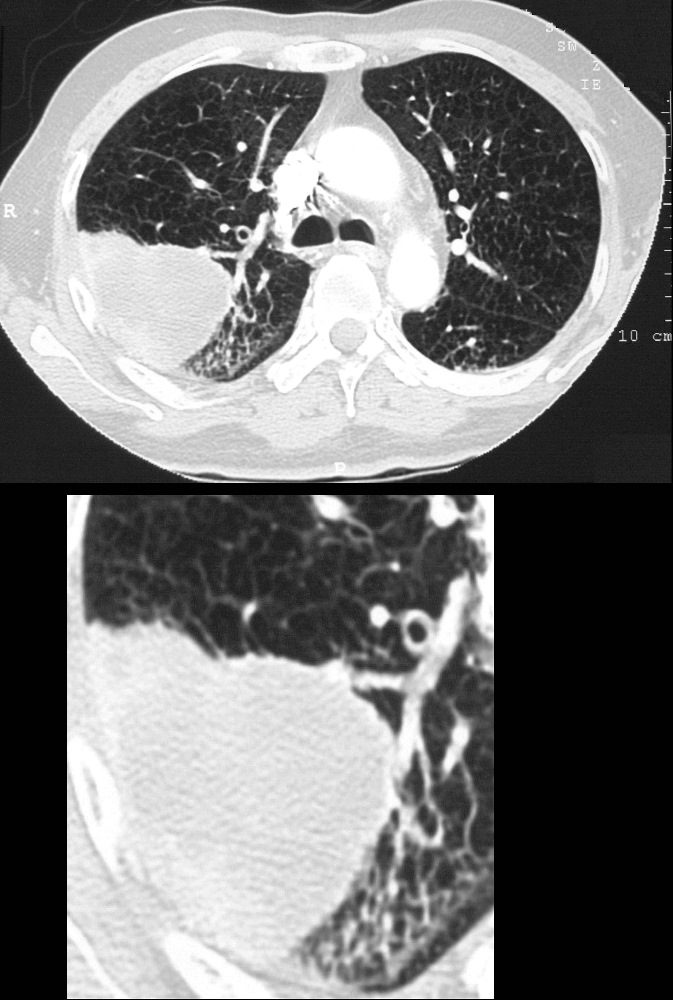
59-year-old male presents with history of scleroderma, Raynaud’s disease, and ILD
Axial CT shows extensive fibrotic change in the apical segments of the lower lobes and the anterior segments of the upper lobe.
There is volume loss architectural distortion, bronchiolectasis and subpleural sparing exemplified in the right lower lobe. peripheral reticular changes, ground glass, bronchiolectasis volume loss and subpleural sparing .
There are bands of fibrosis in the periphery of the right upper lobe with suggestion of intralobular fibrosis.
The spared secondary lobules in the right upper and right lower lobes have also undergone enlargement secondary to the fibrotic process
Ashley Davidoff MD TheCommonVein.net 110Lu 136596
Axial CT shows peripheral reticular changes, ground glass, bronchiolectasis at both lung bases, volume loss with crowding of the bronchovascular bundles posteriorly and subpleural sparing posteriorly. Note air-fluid level in the distended esophagus.
Ashley Davidoff MD TheCommonVein.net 110Lu 136598
59-year-old male presents with history of scleroderma, Raynaud’s disease, and ILD
Upper Image
Axial CT shows bibasilar ground glass, bronchiectasis, and bronchiolectasis with volume loss and with crowding of the bronchovascular bundles posteriorly. There is subpleural sparing. Note air-fluid level in the distended esophagus.
The lower image focuses on the peripheral sparing. The spared secondary lobules have also undergone enlargement secondary to the fibrotic process
Ashley Davidoff MD TheCommonVein.net 110Lu 136598c01
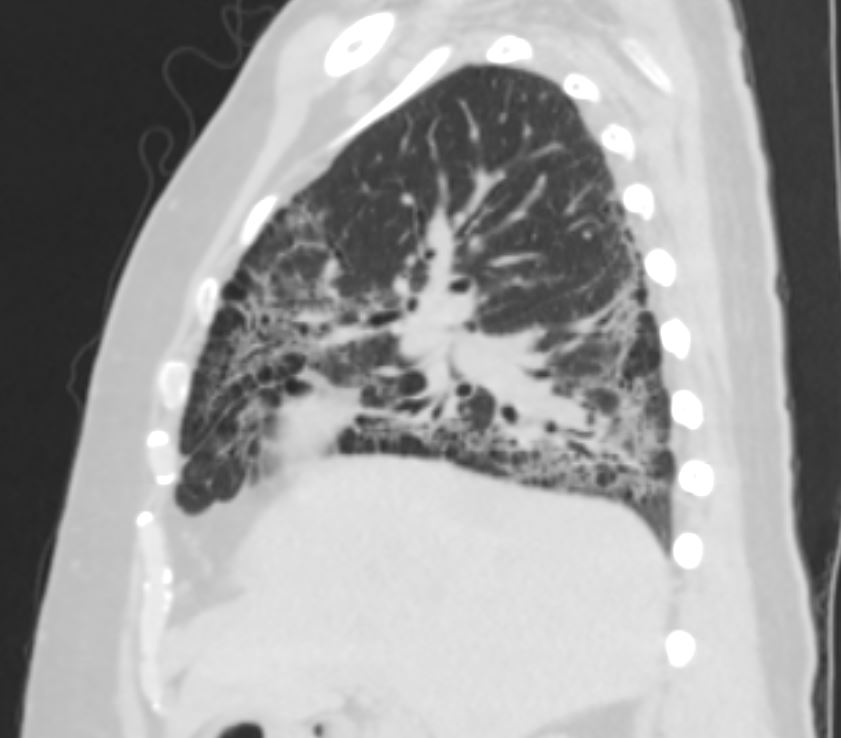
Sagittal CT shows, ground glass changes, bronchiolectasis at the lung base, volume loss with crowding of the bronchovascular bundles posteriorly.
Ashley Davidoff MD TheCommonVein.net 110Lu 136603
Alveolar Septal Amyloidosis
Scattered foci of nodular and calcified changes of secondary lobules involving the centrilobular region and interlobular septa. The affected secondary lobule in the right lower lobe abuts and involves the fissure
Ashley Davidoff TheCommonVein.net b11802
Alveolar Proteinosis
Excellent example of crazy paving
Ashley Davidoff TheCommonVein.net 117625
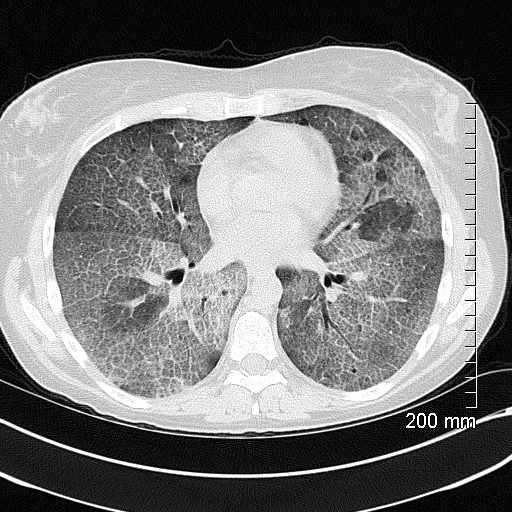
Acute Moderate CHF with Interstitial Edema
50-year-old female with diabetes, chronic renal failure and congestive heart failure. CT in the axial plane through the right posterior recess, shows thickened interlobular septa at the right base, congested arterioles (light blue arrowheads, b), alongside the bronchioles, peribronchial cuffing (white arrowheads, b), a congested pulmonary venule in the interlobular septum (red arrowhead arrowheads, b), ground glass changes and a secondary lobule demonstrating mosaic attenuation (black arrowhead arrowheads, b). The IVC is dilated and a small complex effusion is present.
Ashley Davidoff MD TheCommonvein.net 135783cL 193Lu
Irregular
51-year-old female smoker with a history of COPD asthma and pulmonary hypertension presents with progressive dyspnea. Axial CT through the upper lung fields shows extensive changes of centrilobular emphysema and an expanded group of secondary lobules noted in the right upper lobe Path confirmed a diagnosis of DIP
Ashley Davidoff MD TheCommonVein.net 252Lu 135963c
Nodular
Small Airway Disease and Nodular Thickening of the Interlobular Septum -Right Upper Lobe
Active TB
CT in the axial plane shows extensive small airway disease dominant in the right upper lobe characterized by innumerable, ground glass micronodules, centrilobular nodules (teal blue arrowheads) and nodular thickening of the interlobular septa likely reflecting lymphatic involvement (red arrowheads)
Ashley Davidoff MD TheCommonVein.net 135825cL 192Lu
Sarcoidosis Interlobular and Intralobular Nodules
SARCOIDOSIS, ACTIVE – ALVEOLAR FORM
SARCOIDOSIS, ACTIVE – ALVEOLAR FORM
48-year-old previously well presented with dyspnea and initial CXR showed an infiltrate at the right base, and clinically resolved. He presented a year later with right chest pain and low grade ever and the CXR showed patchy opacities in the LUL and in the RLL
A subsequent CT showed LUL nodular opacities and subpleural rim of consolidation in the LUL and more prominently at both lung bases, associated with significant mediastinal adenopathy. Lymphovascular nodularity was noted in the bronchovascular bundles as well as in the interlobular septa, consistent with sarcoidosis
CXR and CT 4 years later showed almost complete resolution of the parenchymal findings and the CT findings except for minimal reticulation and scarring in the subpleural regions
Ashley Davidoff MD
Sarcoidosis End Stage Fibrotic
This cross sectional series of 3 CT images shows end stage sarcoidosis characterised by marked thickening along the lymphovascular bundles. The first image in the upper left shows marked thickening of the interlobular septa caused by granulomatous changes along the lymphatics. Courtesy Priscilla Slanetz MD. 31866c

Ashley Davidoff MD thecommonvein.net 134901-lungs UIP
Calcified Nodular
CALCIFICATION ALONG LYMPHOVASCULAR BUNDLES (red arrows)
INACTIVE SECONDARY TB WITH EXTENSIVE PARENCHYMAL AND LYMPHOVASCULAR INVOLVEMENT
48-year-old male with history of TB presents with back pain
AP view of the spine shows complex lesion in the right apex characterized by fibronodular opacities. There are scattered calcifications throughout the lungs but some are centered around the lymphatics, including the interlobular septa and centrilobular region
Ashley Davidoff MD TheCommonVein.net
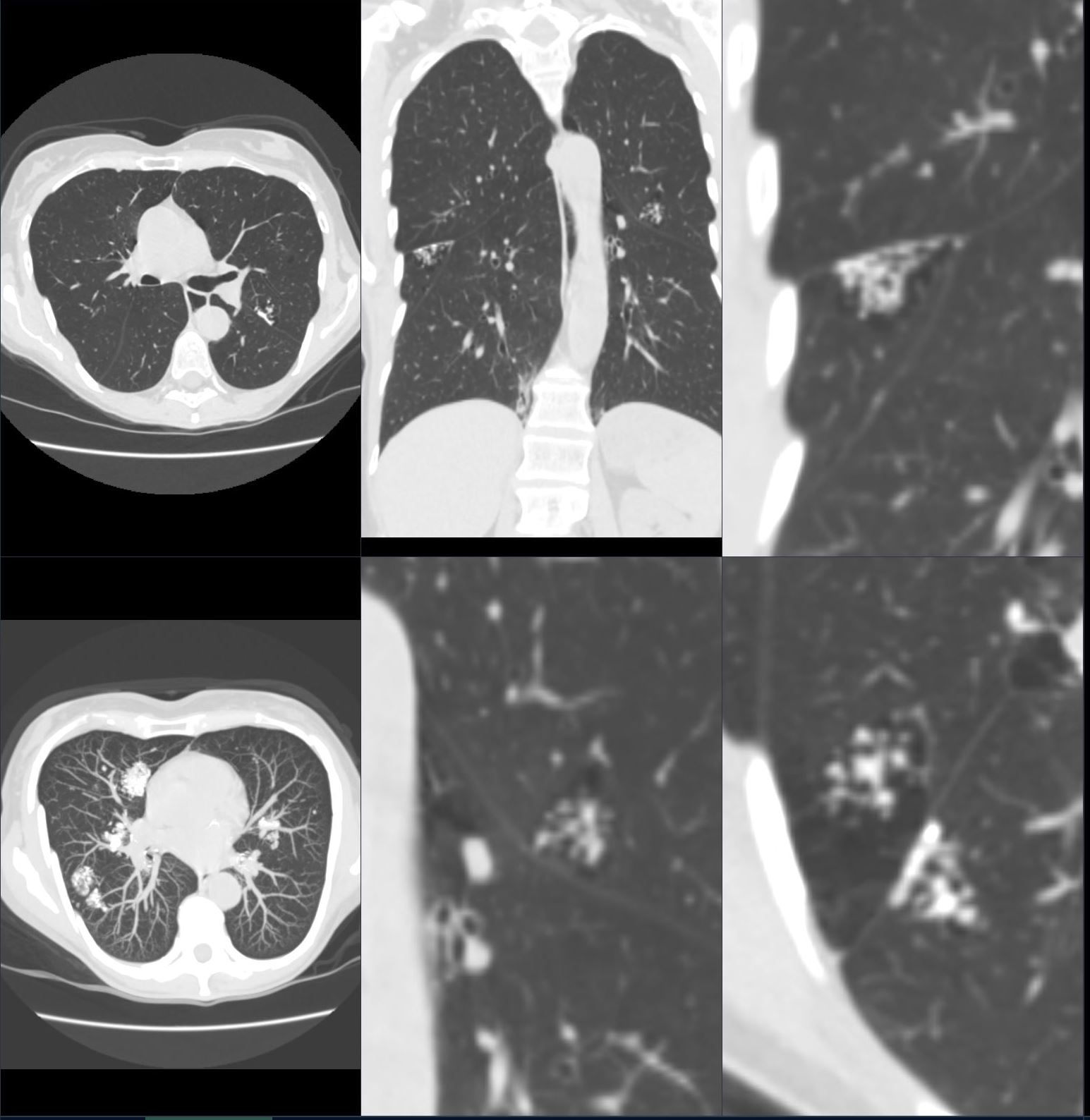
Lymphangitis Carcinomatosis
67-year-old man with prior history of bladder cancer. CT scan in the axial plane shows a large right upper lobe lung mass. Posterior to the mass, the interlobular septa are thickened.. These findings suggest lymphangitis carcinomatosis. Peribronchial thickening of the apical segmental airway may be due either to lymphangitis or chronic bronchitis There is background evidence of centrilobular emphysema, dominant in both upper lobes giving an internal comparison of the normal vs abnormal size of the interlobular septa
Ashley Davidoff MD TheCommonVein.net 32285c 243Lu

67-year-old man with prior history of bladder cancer. CT scan in the axial plane inferior to the lung mass shows extensive irregular thickening of the interlobular septa magnified in the right lower panel. These findings reflect lymphangitis carcinomatosis. There is background evidence of centrilobular emphysema, dominant in both upper lobes. A magnified view in the right lower panel offers an internal comparison of the abnormal vs the normal size and shape of the interlobular septa
Ashley Davidoff MD TheCommonVein.net 32287c 243Lu
Adenocarcinoma of Left Lung with
Coarsened Septal Thickening LUL
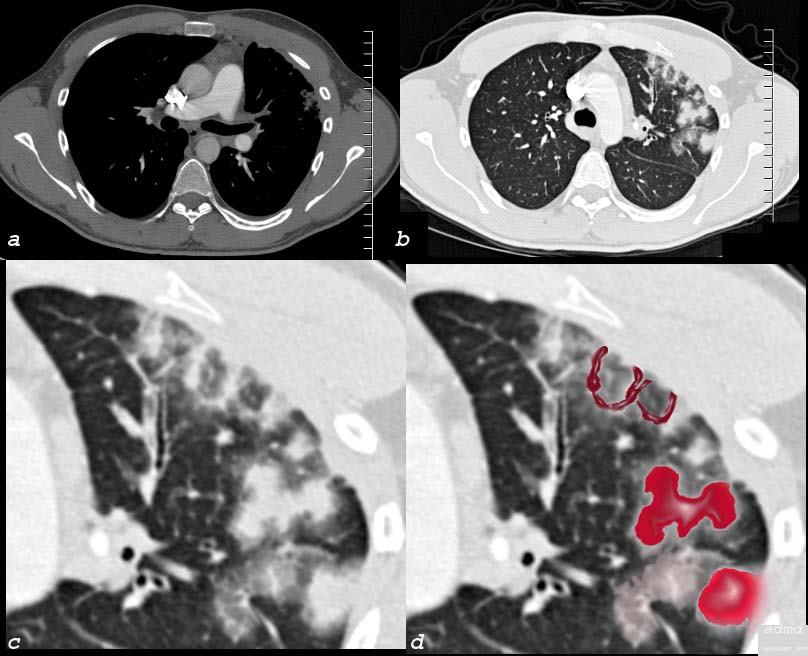
50 year old female with primary adenocarcinoma with the primary lesion presenting as pneumonic consolidation of the left lower lobe, and diffuse reticulonodular changes bilaterally
Image b is a magnified view of the left upper lobe and shows nodular thickening of the interlobular septa representing lymphatic spread along the lymphovascular bundles (pink oval)
The right lung shows interlobular septal thickening centrilobular nodules, and nodular thickening of the minor fissure
These findings are consistent with the diagnosis of lymphangitis carcinomatosa
Ashley Davidoff MD TheCommonVein.net 158Lu 131023c01L
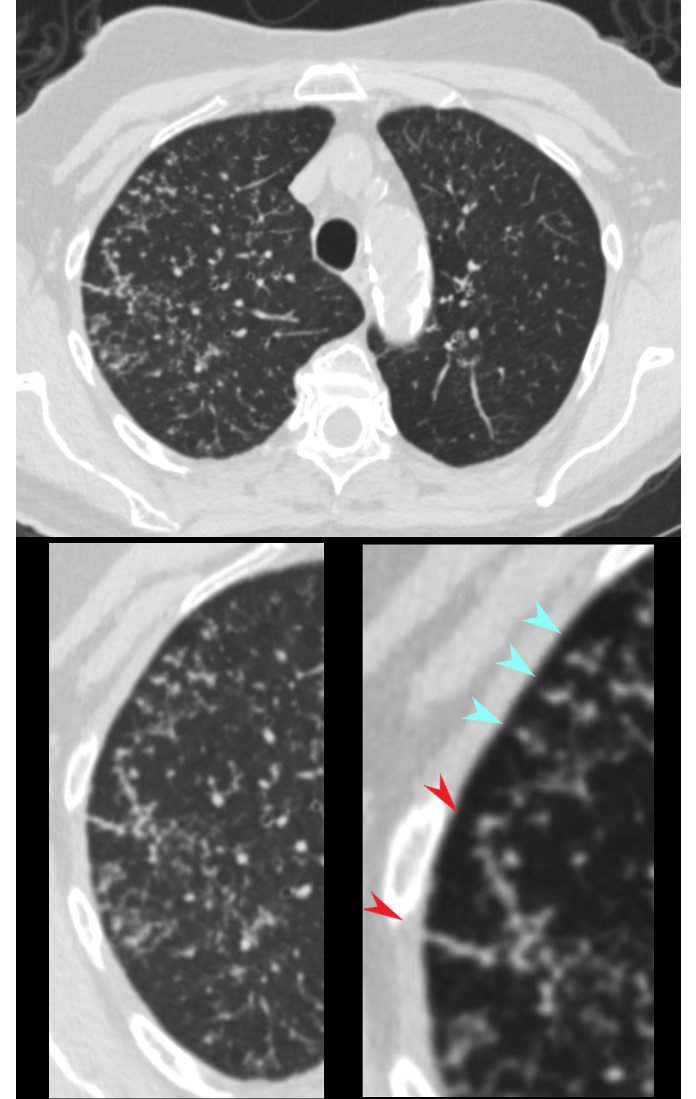
Primary Head and Neck Cancer and Lymphangitis
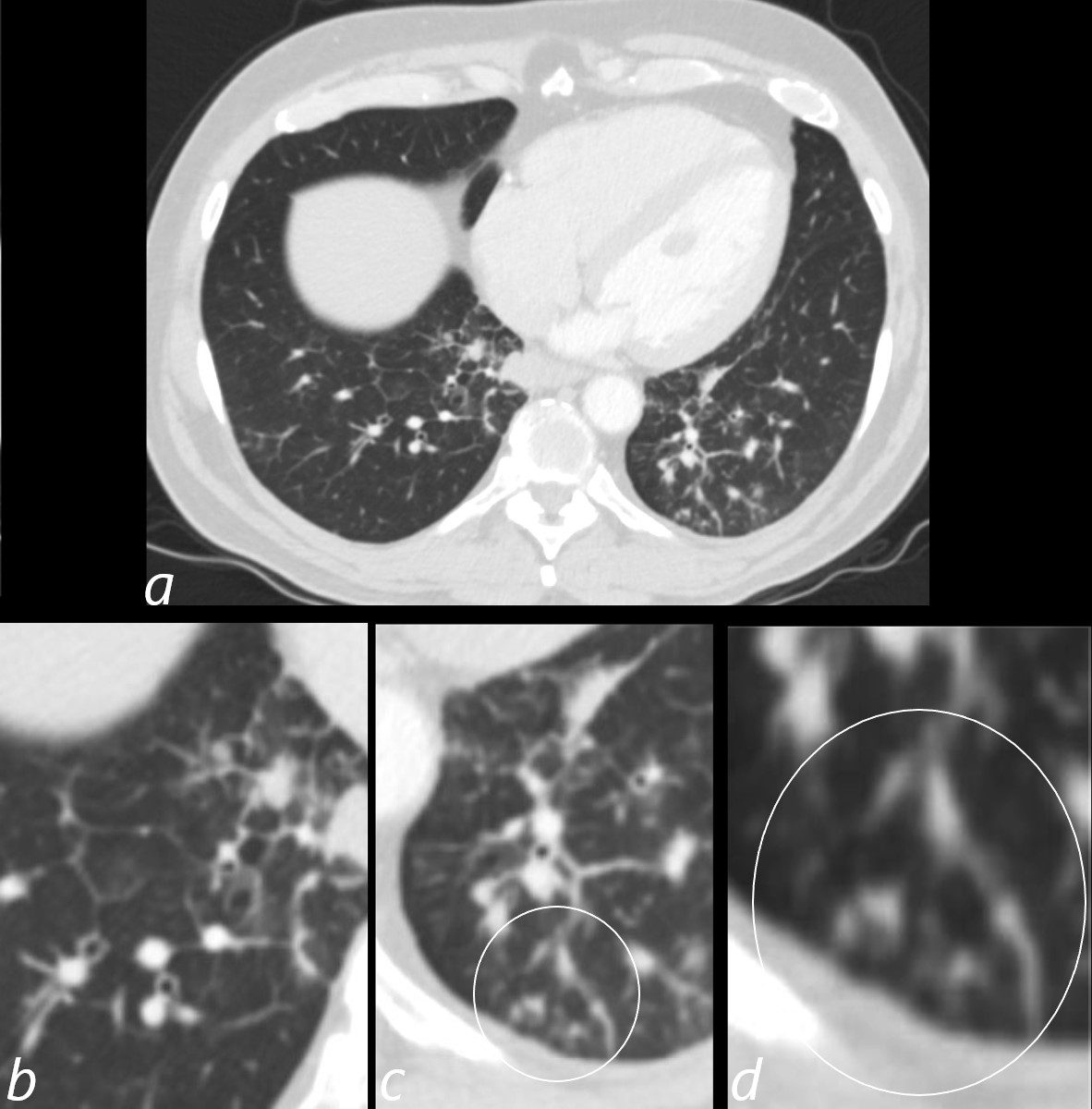
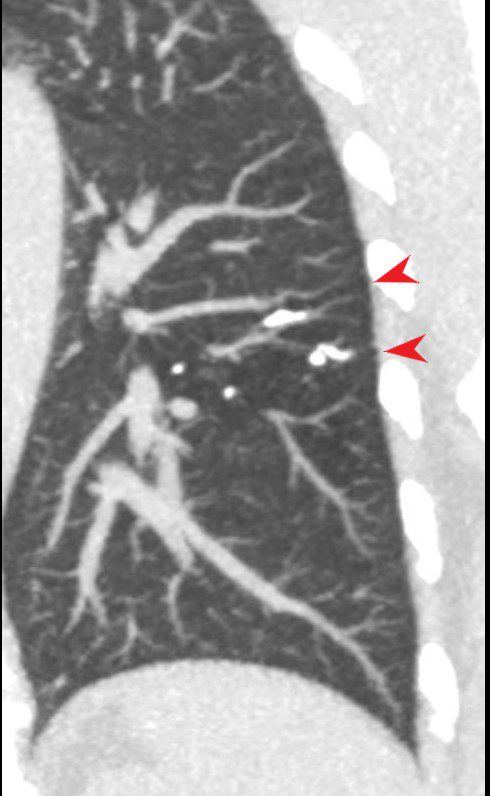
3 months later the patient presented with chest pain and a cough. CT of the chest in the axial plane shows new bilateral lower lobar regions of irregular interlobular septal thickening noted in the right lower lobe a, magnified in b). Ringed in image c and d are 2 side by side secondary lobules with irregular septal thickening centrilobular nodules and other intralobular nodules likely reflecting lymphatic involvement.
Given the changes in the right upper lobe these findings likely reflect lymphangitis carcinomatosa
Ashley Davidoff MD TheCommonVein.net 013Lu 136062cL
LIP
Post Ablation
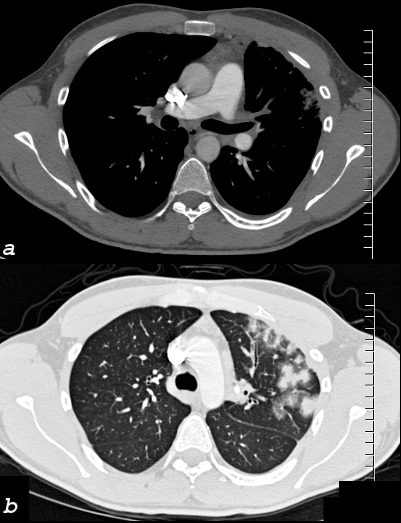
26 year old male who presents with shortness of breath a few months following RFA ablation for atrial fibrillation. Image a shows the left upper lobe thrombosed and the left lower vein contrast filled
Image b (the lung windows) shows thickening of the interlobular septa and secondary lobules distended with material, porobably representing blood.
following male SOB s/p RFA ablation for atrial fibrillation lung pulmonary let upper lobe pulmonary vein thrombosed secondary lobule interlobular septa are thickened secondary lobule destroyed dx pulmonary vein thrombosis secondary to radiofrequency ablation therapy iatrogenic CTscan Courtesy Ashley Davidoff MD Scott Tsai MD key words
ground glass changes pulmonary infarction venous infarction
TheCommonVein.net 75413c02
Reticulation results from thickening of the interlobular or intralobular septa and appears as several linear opacities that resemble a mesh or a net on HRCT scans.7 The presence of reticulation is indicative of interstitial lung disease.7 (Hansell DM, Bankier AA, MacMahon H, et al. Fleischner Society: glossary of terms for thoracic imaging. Radiology. 2008;246:697-722.)
Radiology Rounds
- Subpleural reticulation
- typically in a peripheral subpleural distribution
- located ≤1 cm from the pleura
- normal aging
- can be accompanied by subpleural cysts,
- independent of smoking history
- UIP
- bilateral basilar subpleural reticulation,
- traction bronchiectasis,
- architectural distortion and
- honeycombing
- normal aging
- UIP reticulation

UIP 05
reticulation subpleural
Case courtesy of Royal Melbourne Hospital Respiratory, Radiopaedia.orgUIP and Reticular Pattern
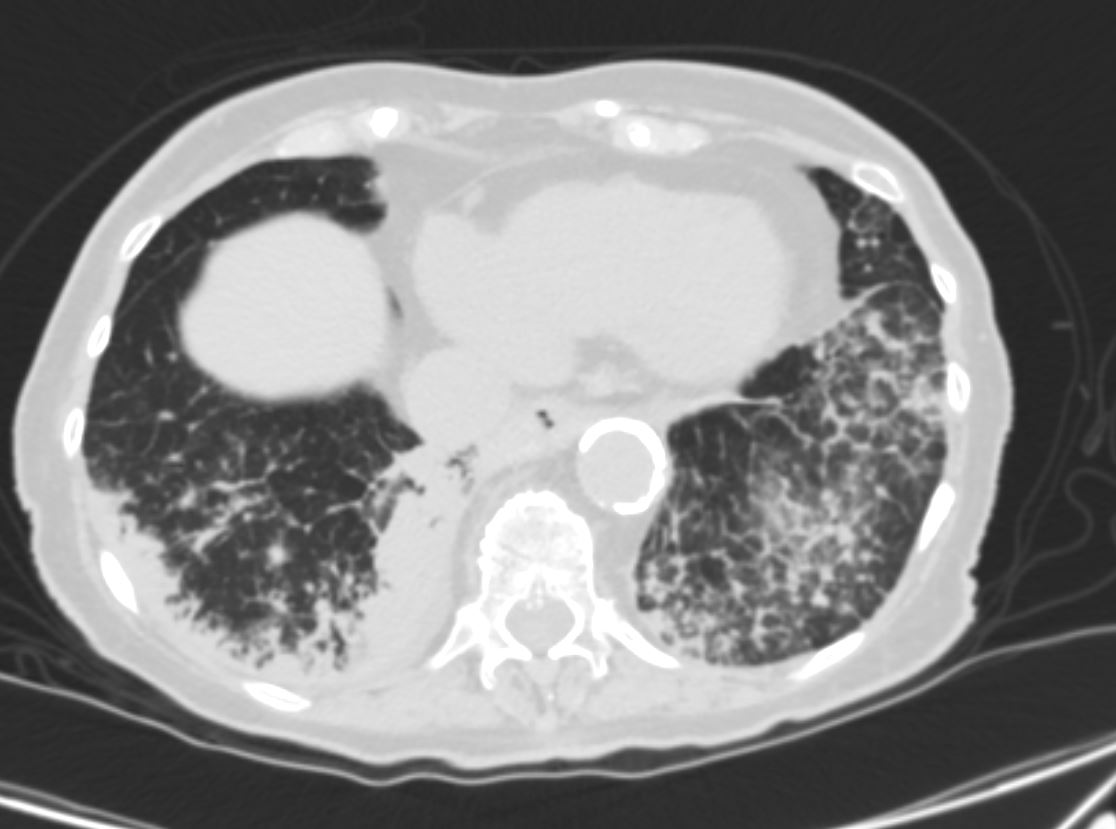
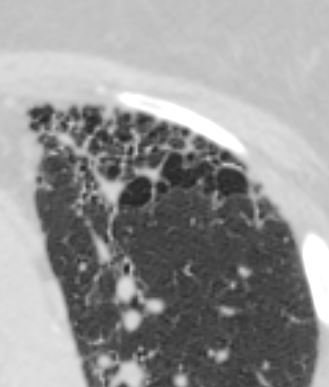
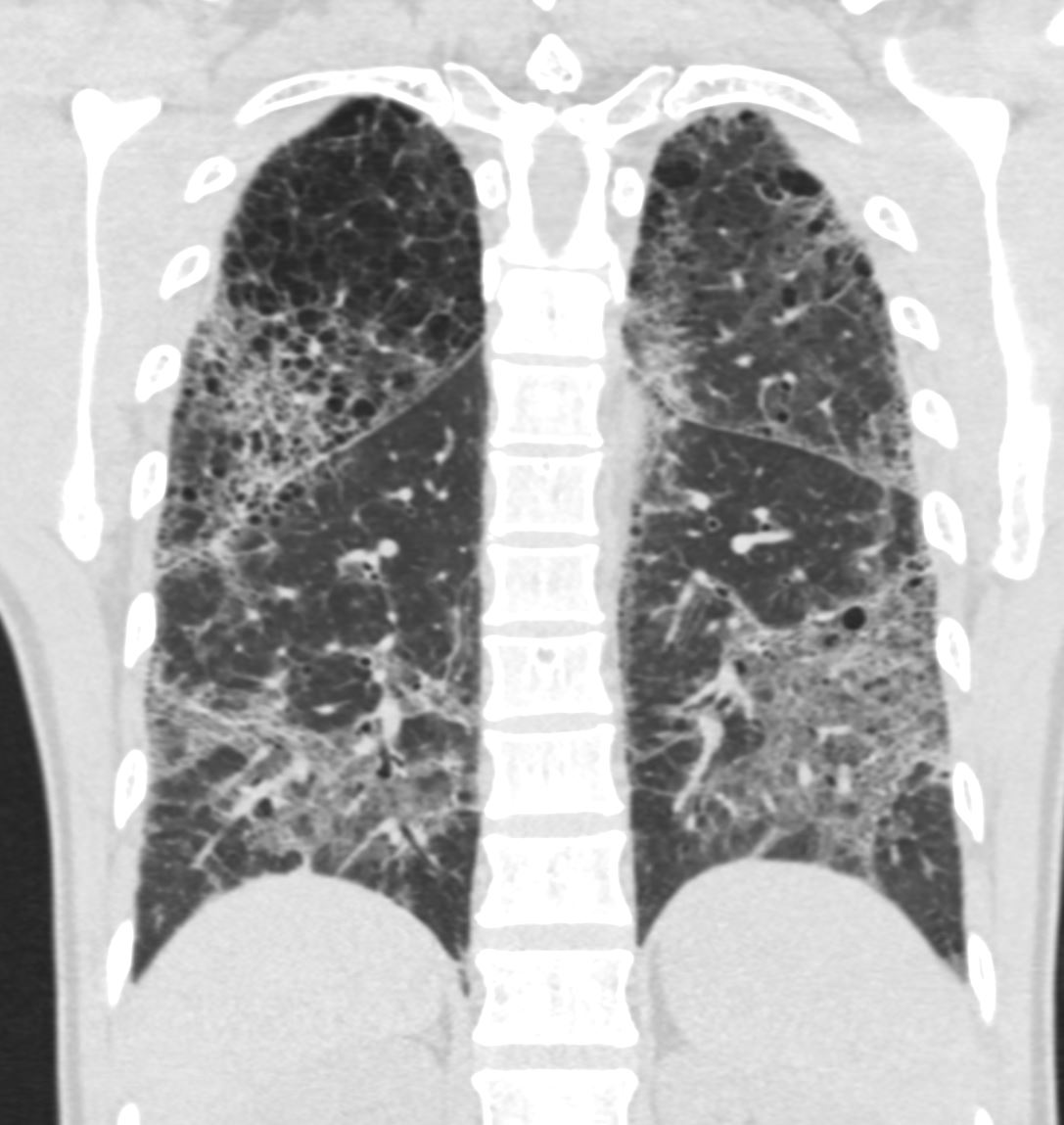
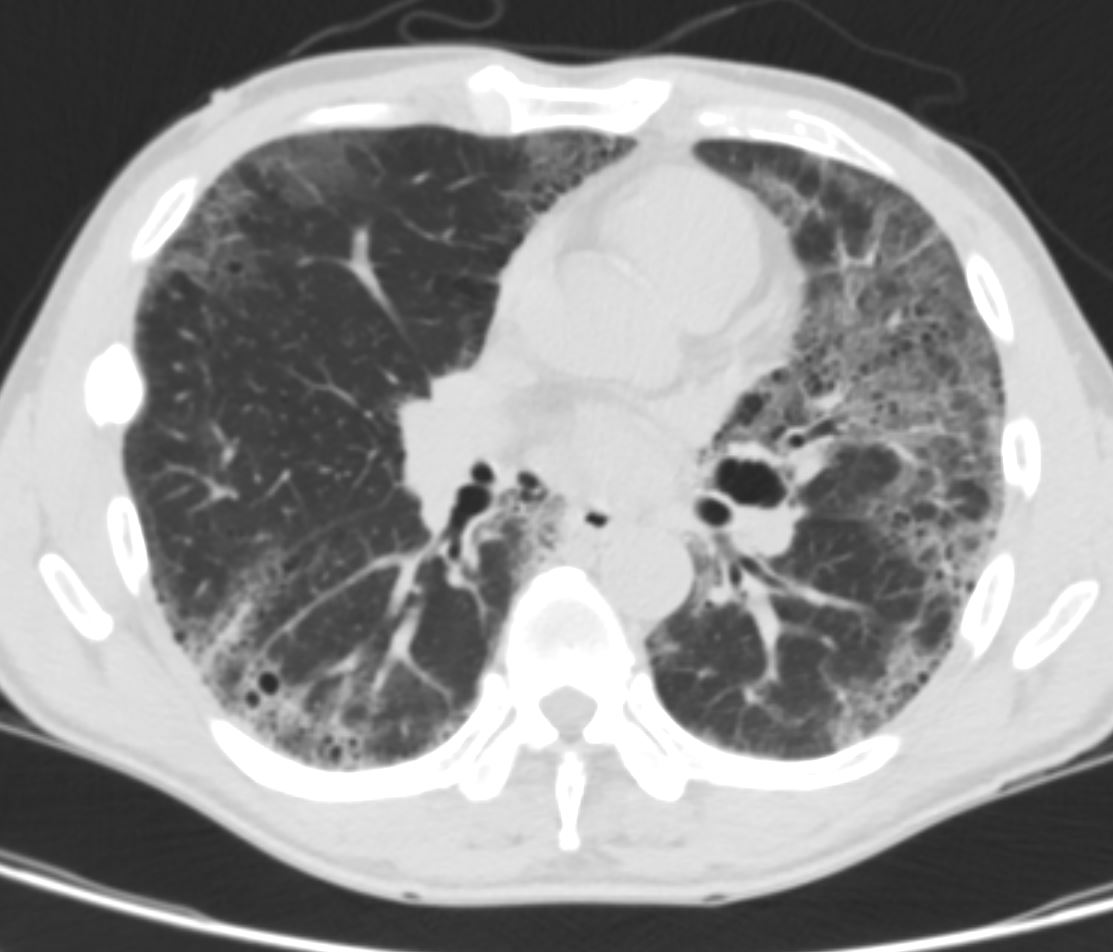
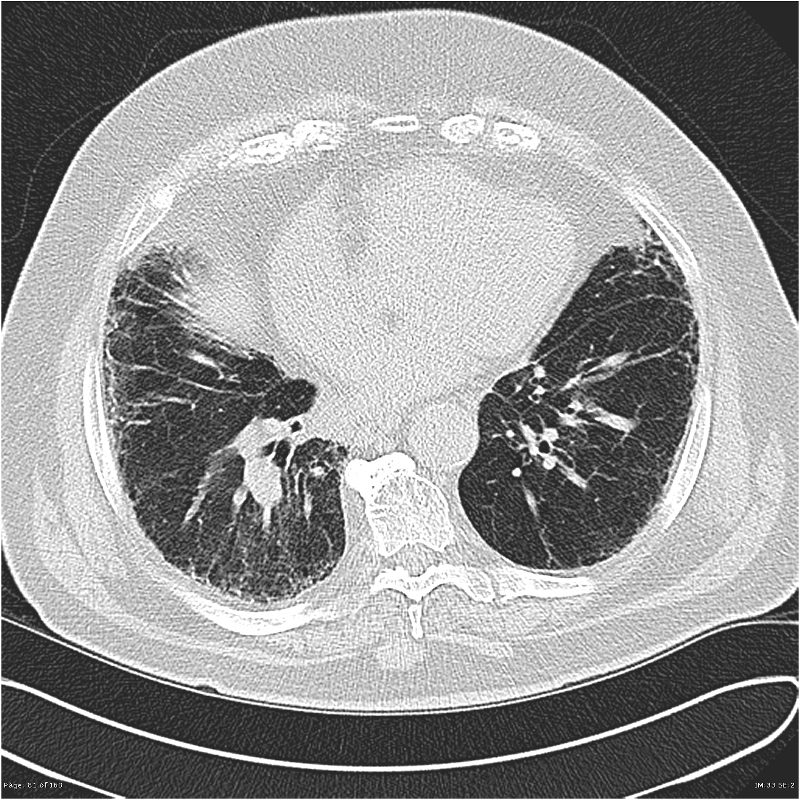
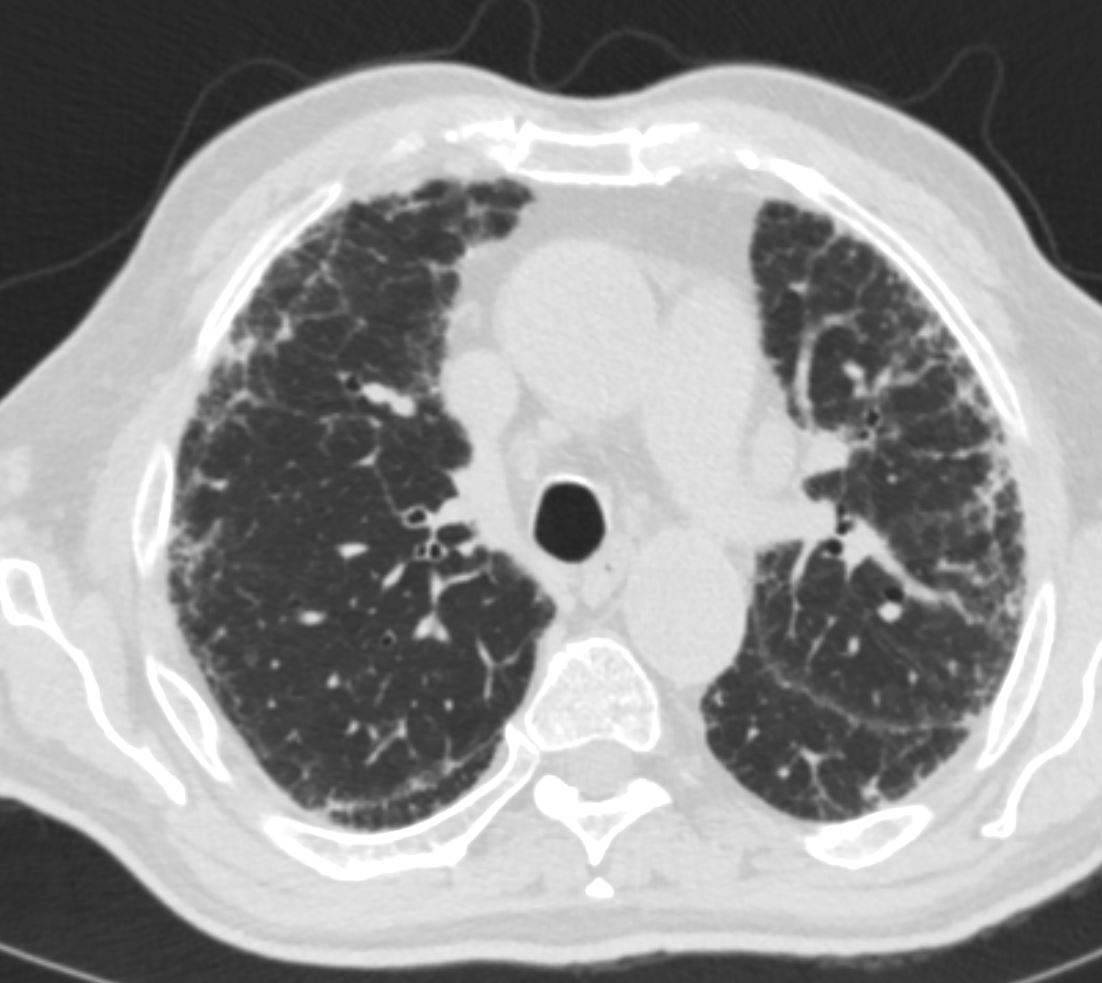
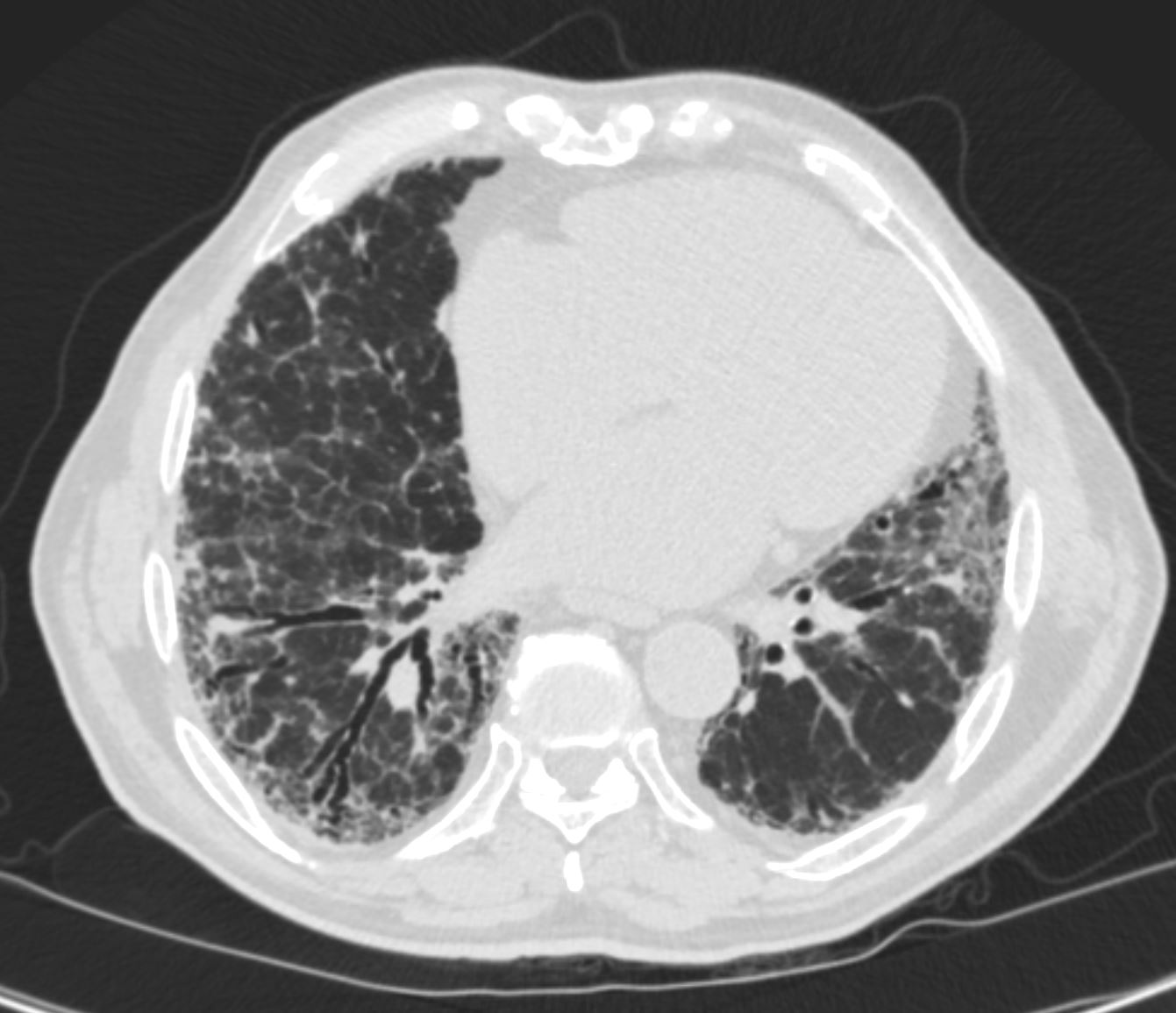
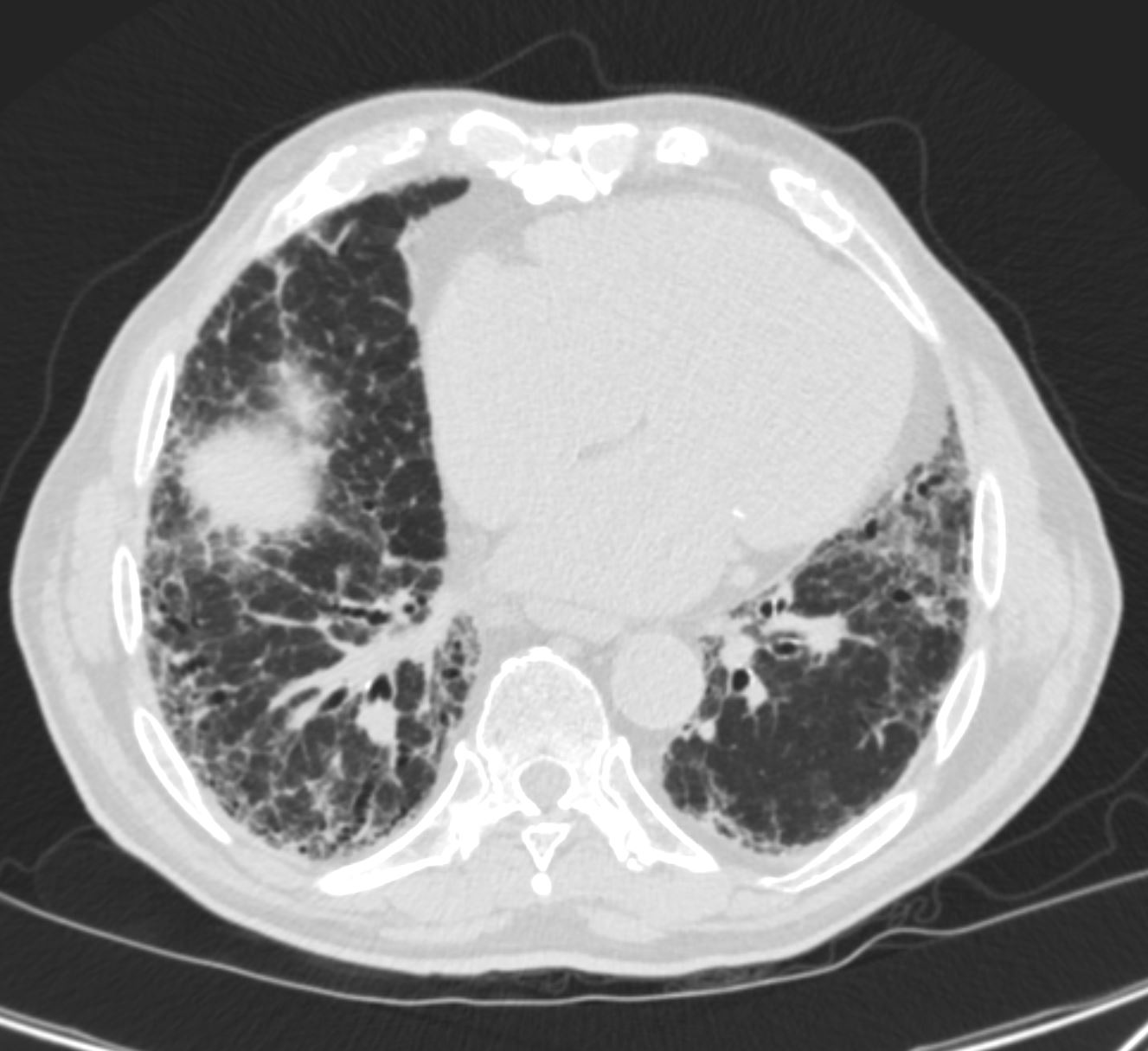
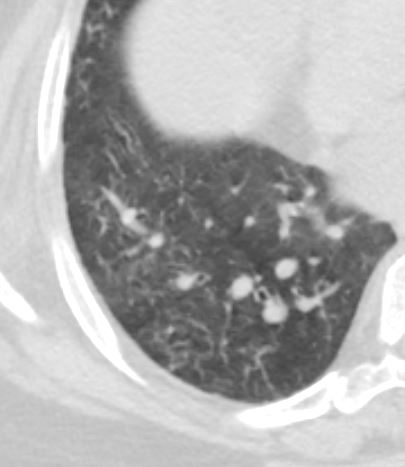
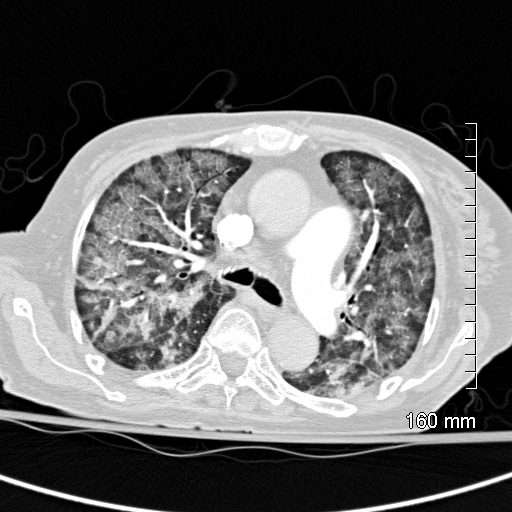
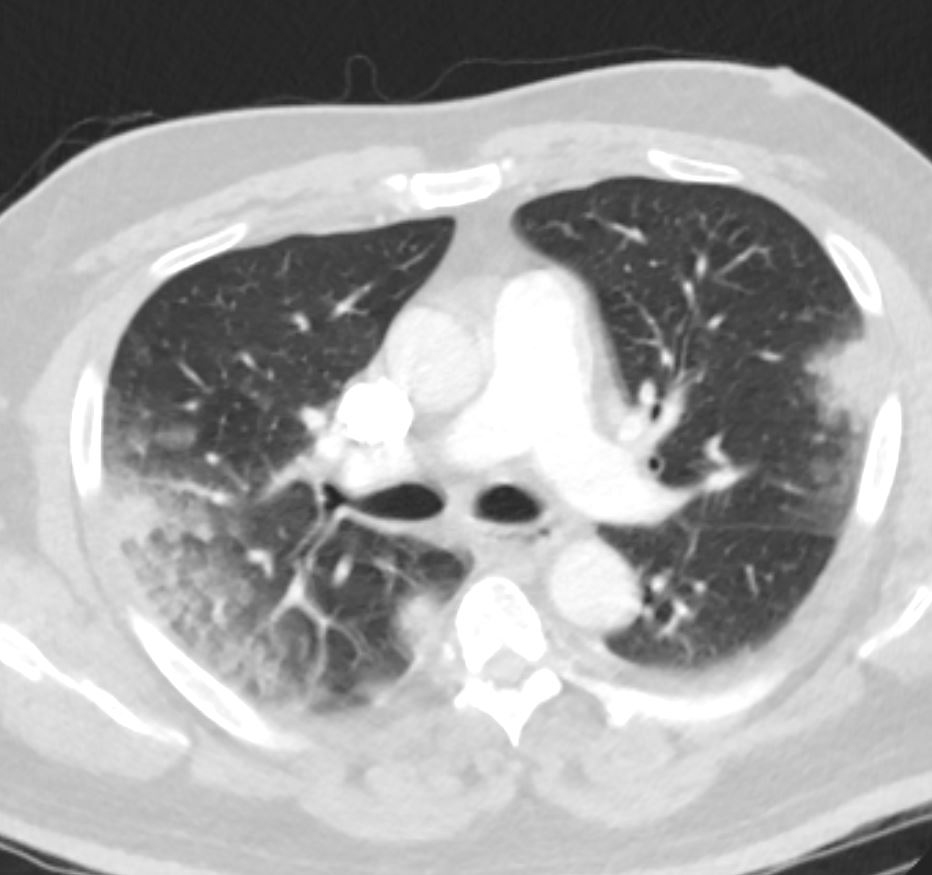
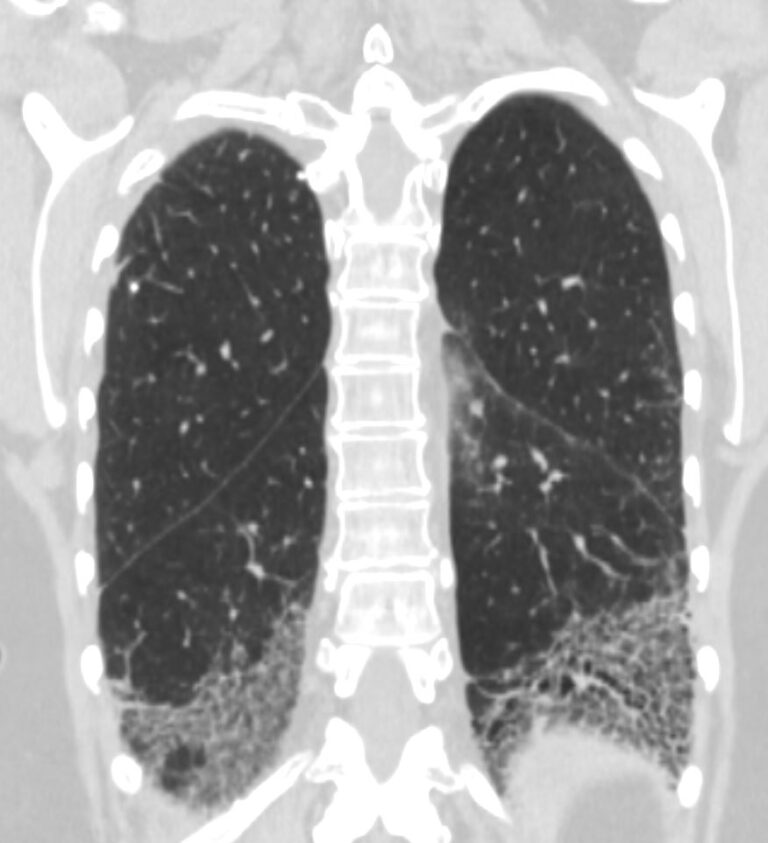
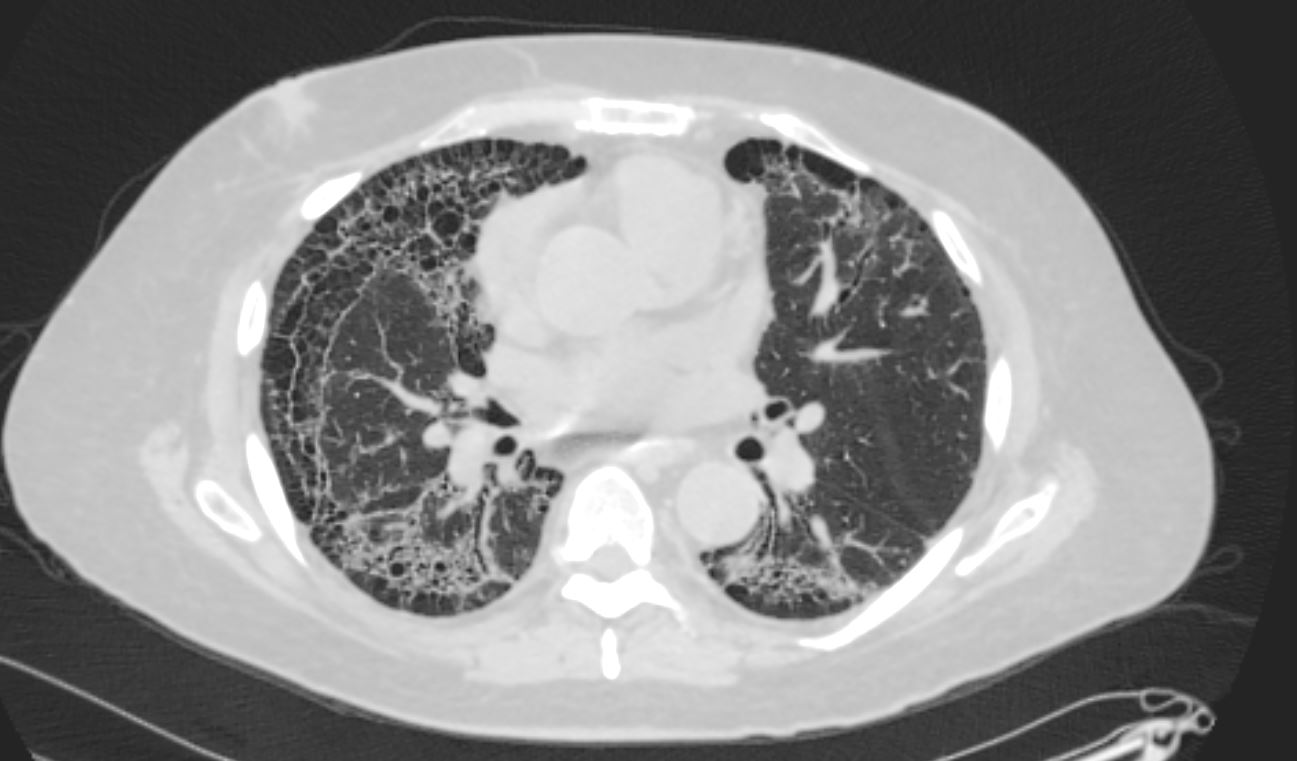
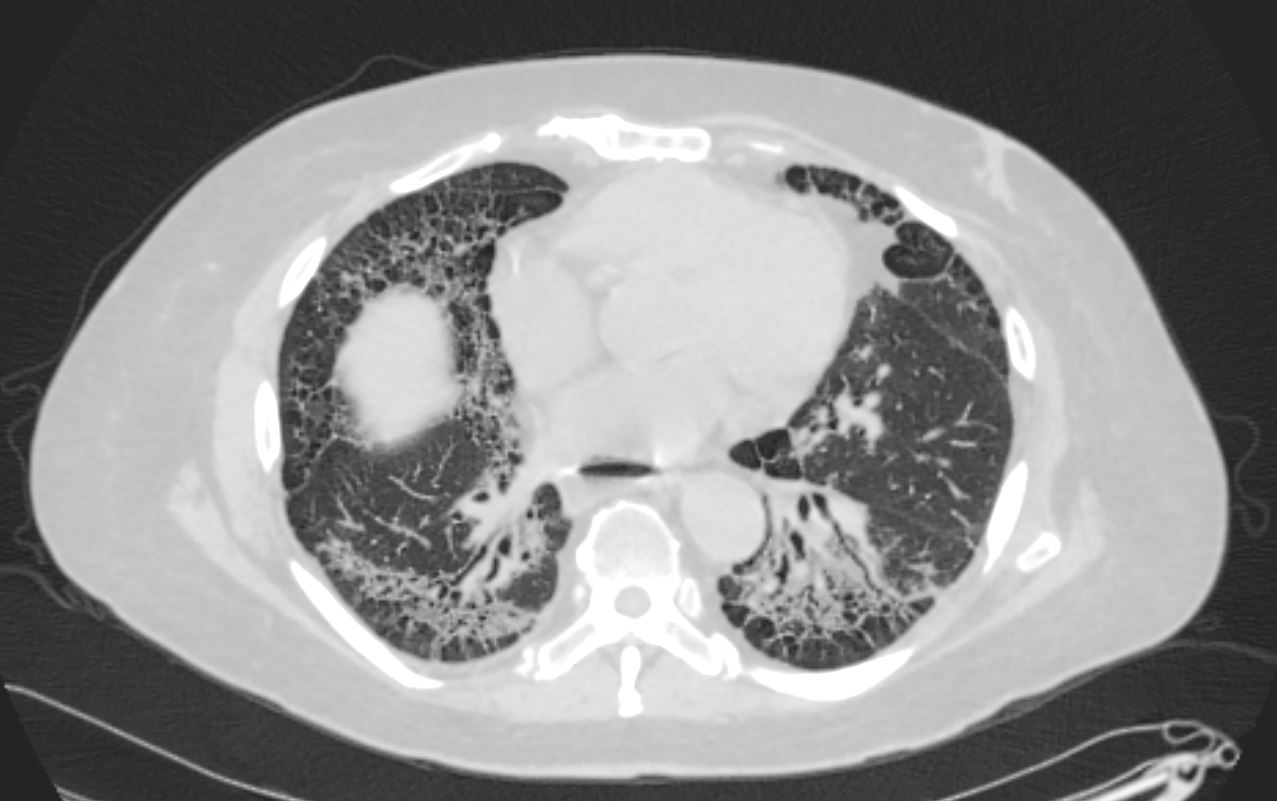
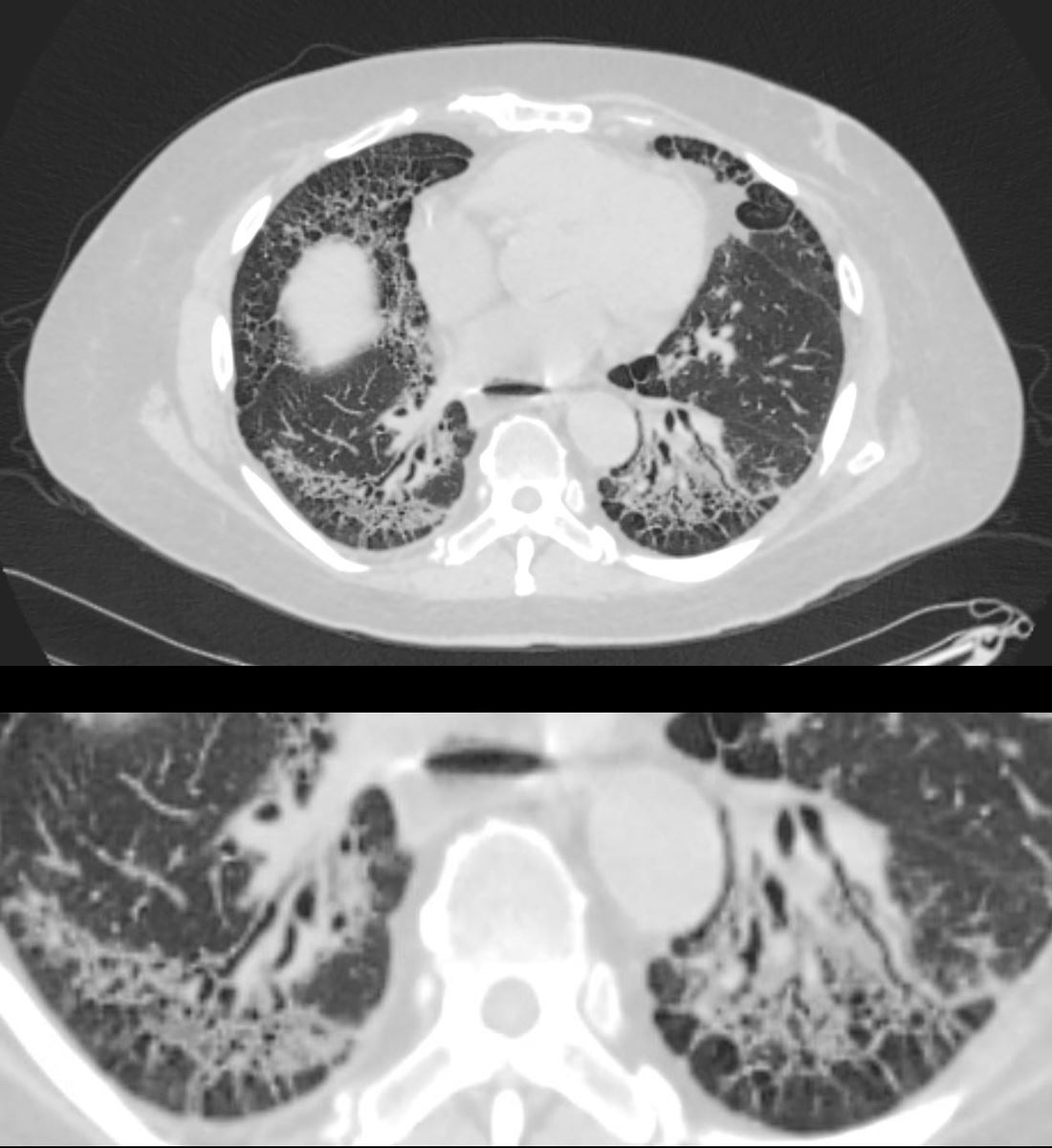
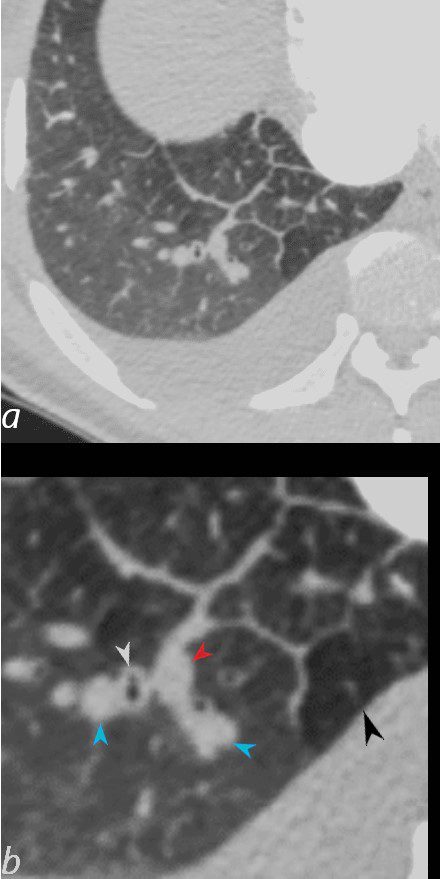
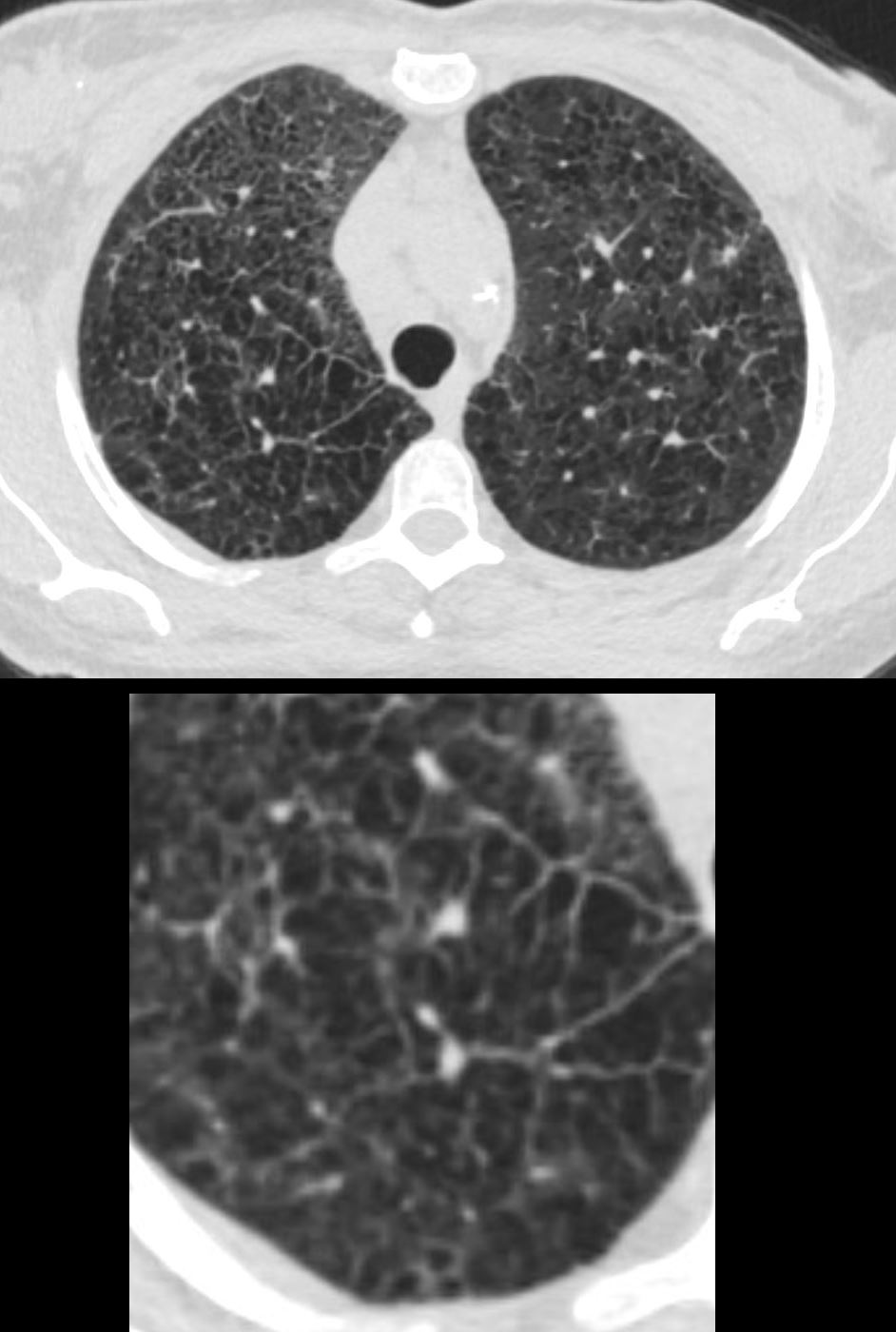
70 year old male with UIP and CHF showing extensive dominantly bibasilar and peripheral reticulation
CXR UIP and Reticular Pattern
70 year old male with UIP showing extensive dominantly bibasilar and peripheral reticulation
Ashley Davidoff MD TheCommonVein.net
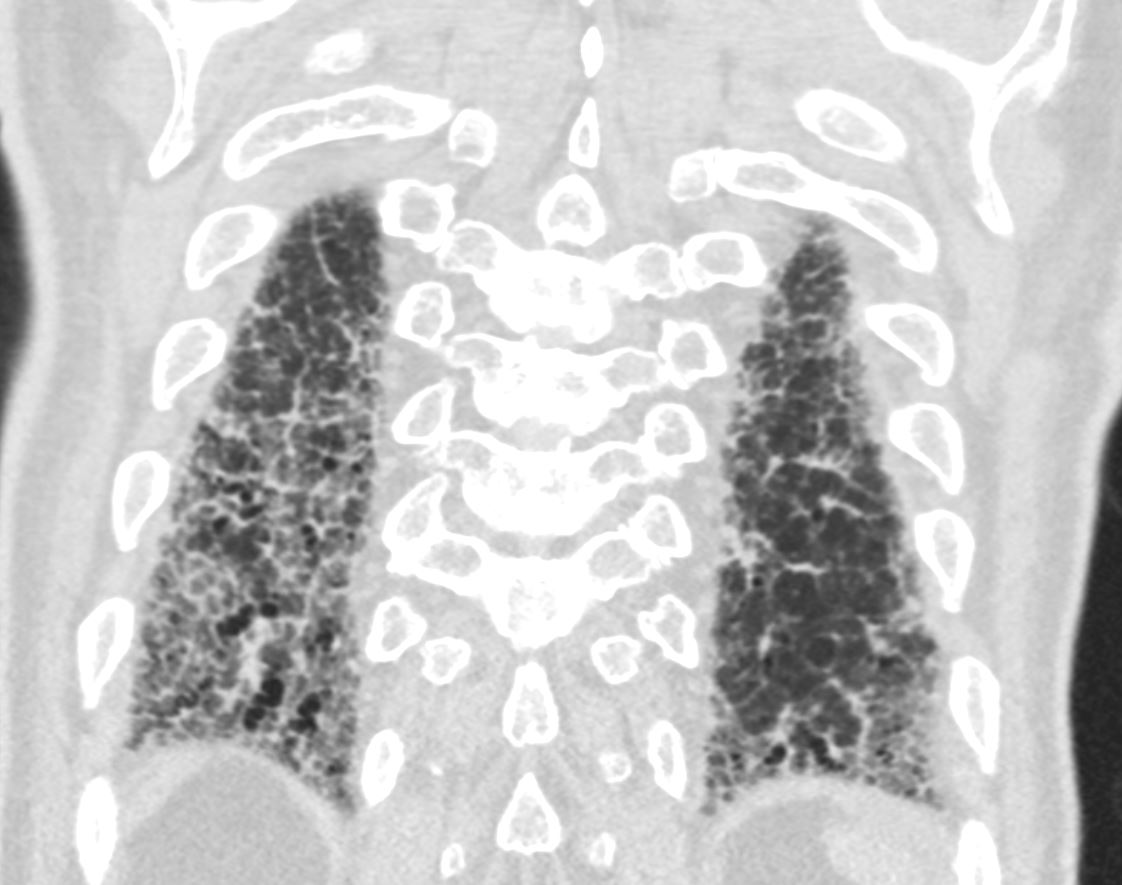
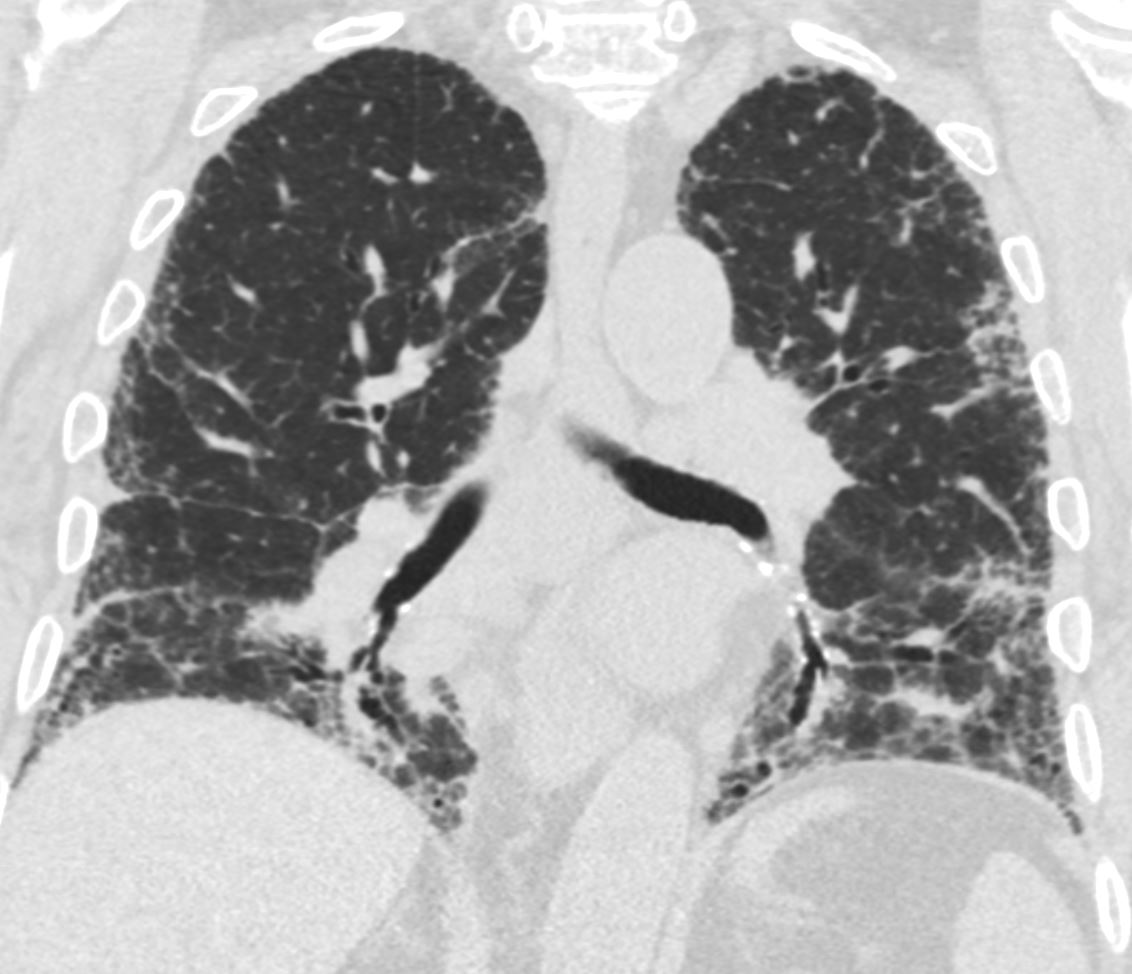
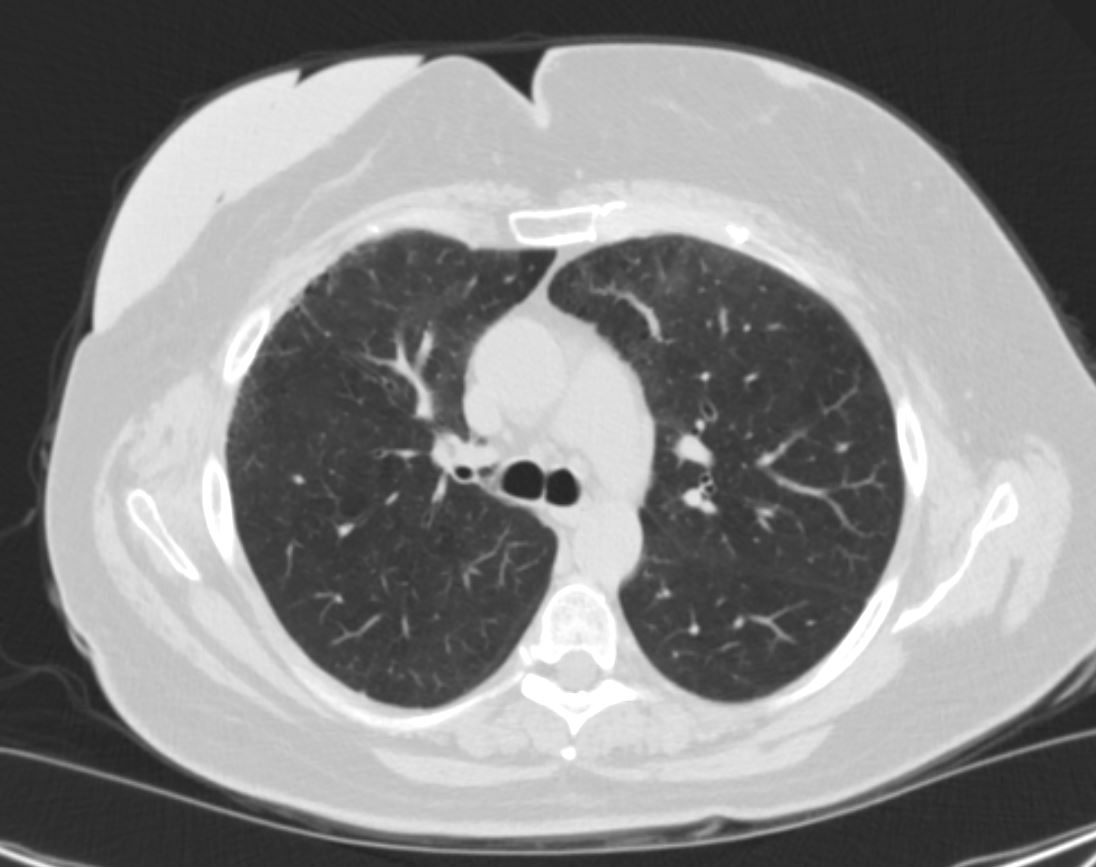
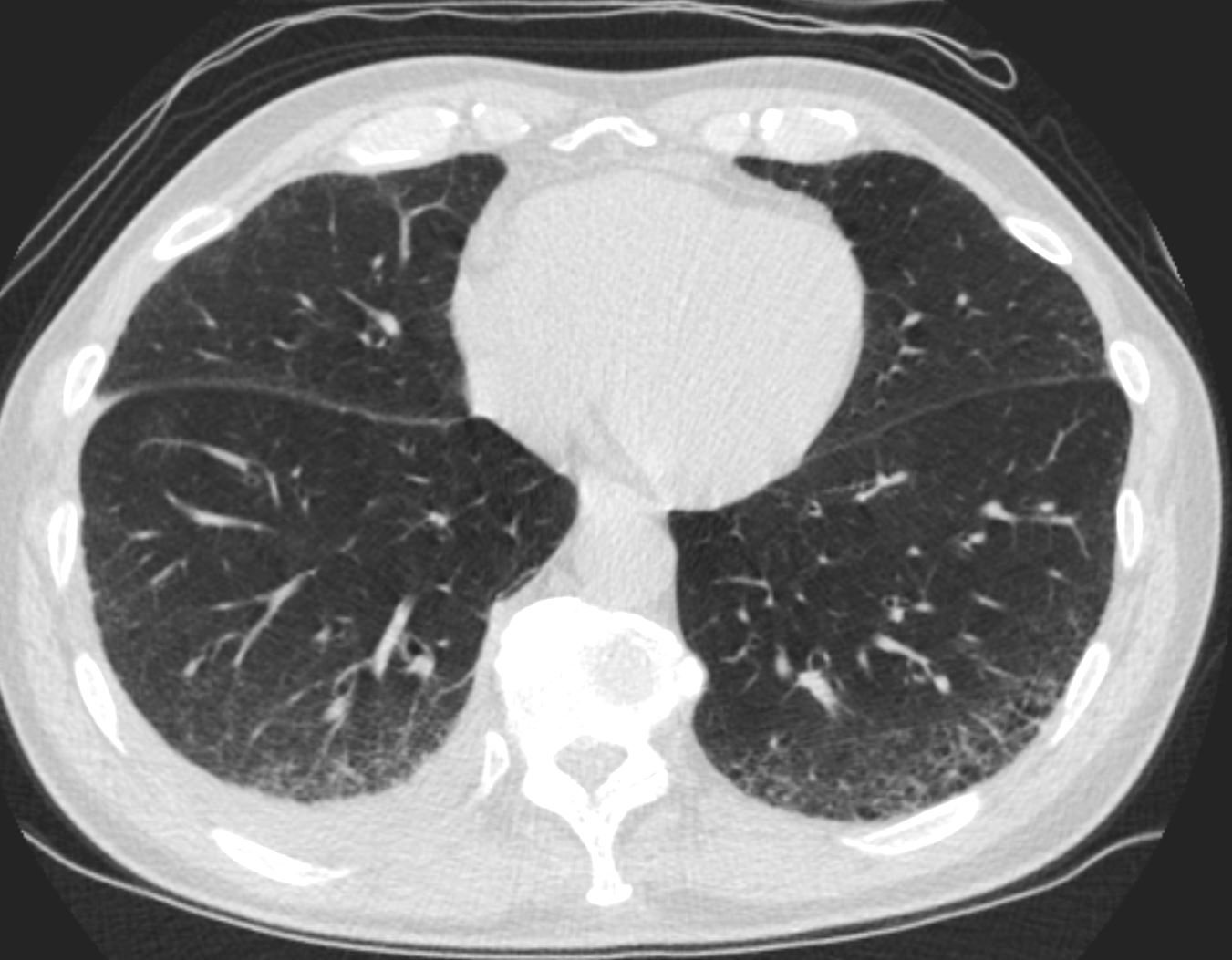
CT UIP and Reticular Pattern Thickened Interlobular Septa
70 year old male with UIP showing extensive dominantly bibasilar and peripheral reticulation
Ashley Davidoff MD TheCommonVein.net uip-004
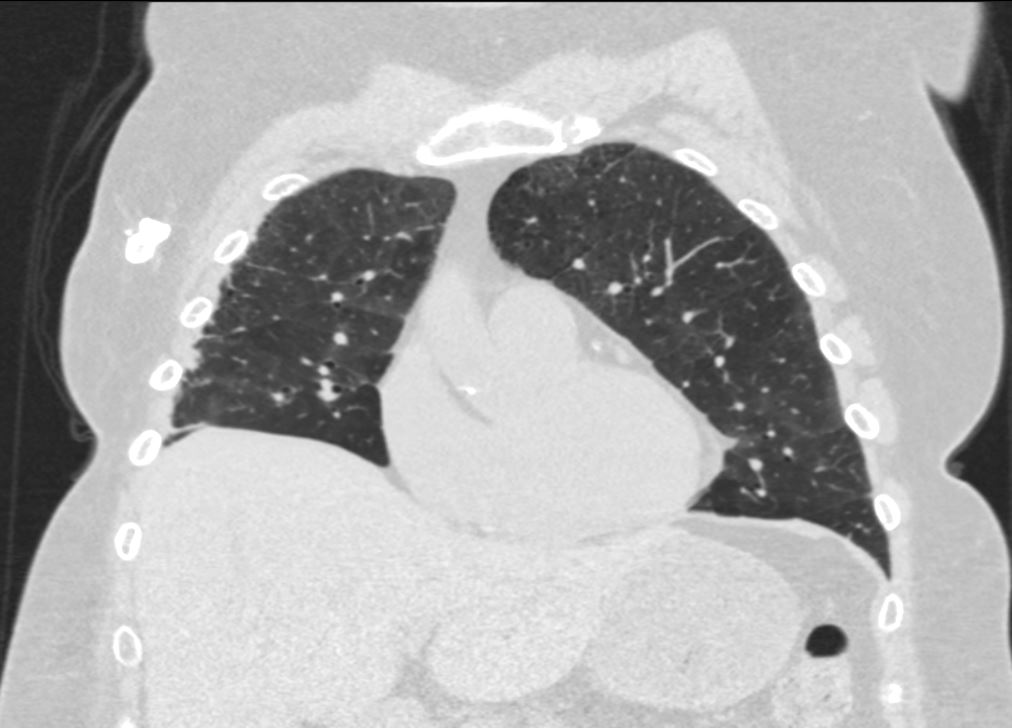
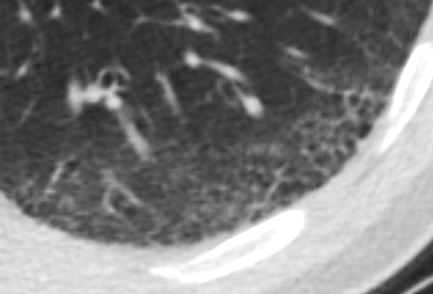
CT UIP and Reticular Pattern
70 year old male with UIP showing extensive dominantly bibasilar and peripheral reticulation
Ashley Davidoff MD TheCommonVein.net uip-003
CT UIP and Reticular Pattern
70 year old male with UIP showing extensive dominantly bibasilar and peripheral reticulation
Ashley Davidoff MD TheCommonVein.net uip-002
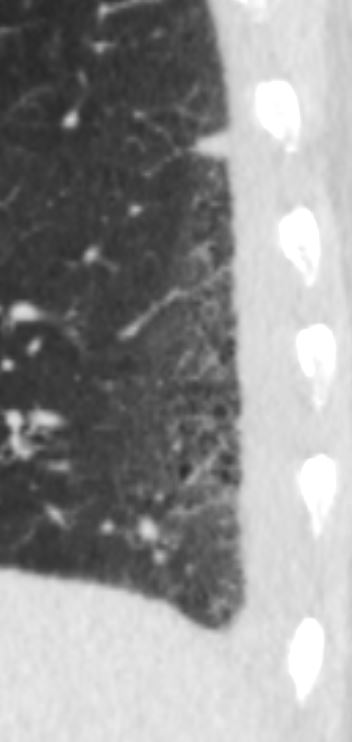
CT UIP and Reticular Pattern
70 year old male with UIP showing extensive dominantly bibasilar and peripheral reticulation
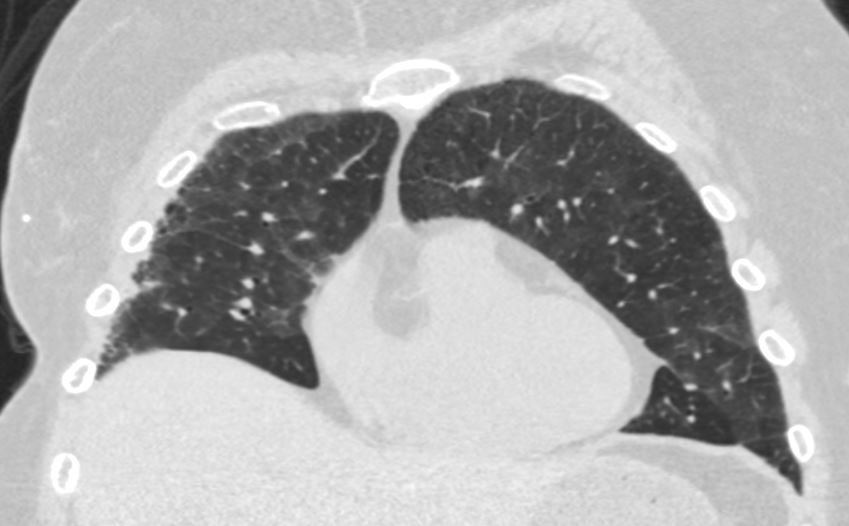
Ashley Davidoff MD TheCommonVein.net uip-005
CT UIP and Reticular Pattern
70 year old male with UIP showing extensive dominantly bibasilar and peripheral reticulation
Ashley Davidoff MD TheCommonVein.net uip-006
CT UIP and Reticular Pattern
70 year old male with UIP showing extensive dominantly bibasilar and peripheral reticulation
Ashley Davidoff MD TheCommonVein.net uip-007
CT UIP and Reticular Pattern
70 year old male with UIP showing extensive dominantly bibasilar and peripheral reticulation
Ashley Davidoff MD TheCommonVein.net uip-008Reticular Changes Caused by Fibrosis of the Interlobular Septa
Combined Pulmonary Fibrosis and Emphysema

Ashley DavidoffMD TheCommonVein.net combined pulmonary fibrosis and emphysema 002
Ashley DavidoffMD TheCommonVein.net combined pulmonary fibrosis and emphysema 000b
Ashley DavidoffMD TheCommonVein.net combined pulmonary fibrosis and emphysema 000c

Ashley DavidoffMD TheCommonVein.net combined pulmonary fibrosis and emphysema 003
Ashley DavidoffMD TheCommonVein.net combined pulmonary fibrosis and emphysema 004
-
Post COVID 19
-

Reticular fibrosis post COVID
Ashley Davidoff MD TheCommonVein.net - Diffuse Reticular Lung Disease
- PCP HIV
-

PCP Pneumonia
46 year old female with HIV presents with dyspnea. CXR scan shows a diffuse reticular pattern with suggestion of upper lobe predominance
Ashley Davidoff MD TheCommonVein.net 30755c
PCP Pneumonia
48 year old male with HIV presents with dyspnea. CT scan shows a reticular pattern within ground glass background, dominantly in the lower lobes, and affecting the right lower lobe more than the left
Ashley Davidoff MD TheCommonVein.net 30755cReticular Changes Post XRT


Reticular Changes Post XRT
Ashley Davidoff MD
TheCommonVein.net
Reticular Changes Post XRT
Ashley Davidoff MD
TheCommonVein.net